Abstract
Purpose
Combination therapy with aprepitant, serotonin receptor antagonist, and steroids improves the complete response rate of both acute and delayed chemotherapy-induced nausea and vomiting (CINV). However, it is not known whether ramosetron is suitable for administration in combination with aprepitant. Therefore, we conducted a multicenter, open-label, prospective, phase II study in order to assess the efficacy and tolerability of combination therapy with ramosetron, aprepitant, and dexamethasone (RAD) for prevention of cisplatin-based CINV in chemotherapy-naïve patients with solid cancers.
Materials and Methods
Forty-one patients with various solid cancers (31 male and 10 female; median age, 59 years) who received treatment with highly emetogenic chemotherapy (median cisplatin dose, 70 mg/m2; range 50 to 75 mg/m2) were enrolled in this study. Oral aprepitant (125 mg on day 1; 80 mg on days 2 and 3), intravenous ramosetron (0.6 mg on day 1), and oral dexamethasone (12 mg on day 1; 8 mg on days 2-4) were administered for prevention of CINV.
Results
The complete response (no emesisand retching and no rescue medication) rate was 94.9% in the acute period (24 hours post-chemotherapy), 92.3% in the delayed period (24-120 hours post-chemotherapy), and 92.3% in the overall period (0-120 hours). The absolute complete response (complete response plus no nausea) rate was 74.4% in the acute period, 51.3% in the delayed period, and 46.2% in the overall period. There were no grade 3 or 4 toxicities related to these antiemetic combinations.
Conclusion
RAD regimen is a safe and effective antiemetic treatment for prevention of CINV in patients receiving highly emetogenic chemotherapy.
Keywords: Aprepitant, Dexamethasone, Ramosetron, Chemotherapy-induced nausea and vomiting
Introduction
Chemotherapy-induced nausea and vomiting (CINV) is one of the most unpleasant side effects for patients receiving chemotherapy. It can have a significant effect on a patient's qualify of lifeand prevent continuation of chemotherapy. The incidence and severity of CINV are affected by diverse factors, including the specific chemotherapeutic agents, the dosage of the agents, the schedule and route of administration of the agents, and individual patient variability [1-3]. Cisplatin is one of the most effective chemotherapeutic agents available for treatment of many solid tumors. However, it is also highly emetogenic, resulting in poor compliance with chemotherapy. Therefore, control of CINV by selection of a relevant antiemetic regimen is as important as the efficacy of the chemotherapy regimen.
Development of newer antiemetic agents, such as serotonin (5-HT3) receptor antagonists and neurokinin-1 (NK-1) receptor antagonists, has resulted in substantially reduced incidence and risk of CINV in patients receiving chemotherapy. In particular, a triple combination regimen consisting of a NK-1 antagonist, a 5-HT3 antagonist, and dexamethasone is recommended by key clinical guidelines groups, including the National Comprehensive Cancer Network, the European Society of Medical Oncology, and the American Society of Clinical Oncology, for prevention of acute and delayed emesis in patients receiving highly emetic intravenous chemotherapy such as cisplatin [4-6]. The excellent efficacy of this triple-drug regimen with various 5-HT3 antagonists, including ondansetron, granisetron, and palonosetron, has been reported [7-9]. However, the most effective 5-HT3 antagonist for this combination has not yet been identified.
Ramosetron, a 5-HT3 receptor antagonist developed in Japan (Yamanouchi Pharmaceutical Ltd., Tokyo, Japan), has been used widely in Asian countries for prevention of CINV. In several clinical trials, it showed equivalent efficacy and a similar safety profile when compared with ondansetron and granisetron [10-13]. However, there is currently no information with regard to whether ramosetron is as effective as other 5-HT3 receptor antagonists for the triple combination regimen. In this study, we evaluated the clinical efficacy and tolerability of a combination regimen comprising ramosetron, aprepitant (NK-1 antagonist), and dexamethasone (RAD) for prevention of CINV in chemotherapy-naïve patients with solid cancers.
Materials and Methods
1. Patient selection
This study was a multicenter, open-label, prospective, phase II clinical trial conducted for investigation of the effects of RAD on prevention of CINV. Chemotherapy-naïve patients between the ages of 15 and 75 years with any solid cancer who were scheduled to receive single day chemotherapy with 50 mg/m2 or more of cisplatin were eligible. Patients from five hospitals of Hallym University Medical Center and Keimyung University Dongsan Hospital in Korea were enrolled in this study. All patients had an Eastern Cooperative Oncology Group performance status of 0-2, adequate renal function (serum creatinine level<2.5 mg/dL or calculated creatinine clearance≥50 mL/min), adequate hepatic function (serum total bilirubin level<2 mg/dL, aspartate aminotransferase/alanine aminotransferase level of<3 times the upper normal limit, and alkaline phosphatase level<5 times the upper normal limit), and adequate marrow function (absolute neutrophil count≥1,500/µL and platelets≥100,000/µL). The primary exclusion criteria were as follows: receipt of medication (antiemetics, steroids, and benzodiazepines, etc.) that might affect study results within one week before the start of chemotherapy; symptomatic brain metastasis; gastro-intestinal obstruction or other disease that could provoke nausea and vomiting; administration of radiotherapy to the brain, abdomen, or pelvis within two weeks before the start of chemotherapy; and known allergy or severe side effects to the study drugs. All patients provided written informed consent, and the study protocol was approved by the Institutional Review Board of each institution and was registered with ClinicalTrials.gov (identifier, NCT01046461).
2. Study treatment
On day 1, all eligible patients received intravenous administration of 0.6 mg ramosetron 30 minutes before administration of chemotherapy, 125 mg aprepitant orally 1 hour before administration of chemotherapy, and 12 mg dexamethasone orally 30 minutes before administration of chemotherapy. For the next two days, the patients received 80 mg aprepitant and 8 mg dexamethasone orally in the morning. Dexamethasone was continued on day 4. Rescue antiemetics were administered at any time during the study period for vomiting or severe nausea at the request of the patients or as recommended by the attending physicians. The type of antiemetic agent was determined by the attending physicians.
3. Assessment
The primary efficacy endpoint was complete response (CR), which was defined as no vomiting, including retching, and no administration of rescue anti-emetic treatment, to the RAD regimen from the start of chemotherapy (0 hour) until-day 5 (defined as the overall phase). The overall phase was classified into an acute phase (0-24 hours) and a delayed phase (24-120 hours). The secondary endpoints were CR in the acute phase and delayed phase, absolute CR (defined as CR plus no nausea), and severity of nauseain both phases. The severity of nausea was determined using the visual analog scale of the Multinational Association Supportive Care Cancer antiemesis tool [14]. Tolerability was assessed on the basis of clinical and laboratory adverse events that occurred after the start of treatment and within 14 days after treatment ended and were evaluated according to the Common Toxicity Criteria for Adverse Events (CTCAE) v.3.0. During the overall phase, patients were asked to record daily episodes of vomiting or retching, the degree of nausea, and the use of rescue medication in a diary.
4. Statistics
Calculation of patient sample size was based on the following assumption. The CR rate of high dose cisplatin-induced overall phase CINV is known to be approximately 55% (p0) for patients receiving ramosetron and dexamethasone [15,16]. Assuming that the addition of aprepitant to ramosetron and dexamethasone improves the CR rate by up to 75% (p1), the sample size should be 37 according to the "exact single-stage phase II designs" procedure (5% α-error and 80% power) [17]. Considering a possible dropout rate of 5%, a target sample size of 39 would be needed. Descriptive examination of demographic data and patients' characteristics was performed and the percentage of patients achieving CR was calculated.
Results
A total of 41 patients were enrolled in this study between November 2010 and February 2012. Baseline clinical characteristics of the patients are summarized in Table 1. The median age of patients was 59 years. Male patients accounted for 76% of the patient population. The most common primary tumor site was the lung (49%), followed by the stomach (15%) and genitourinary tract (10%). All patients received cisplatin and other chemotherapeutic agents, including pemetrexed, taxanes, and gemcitabine. The median dose of a single administration of cisplatin was 70 mg/m2 of the body surface area (range, 50 to 75 mg/m2).
Table 1.
Patients' clinical characteristics
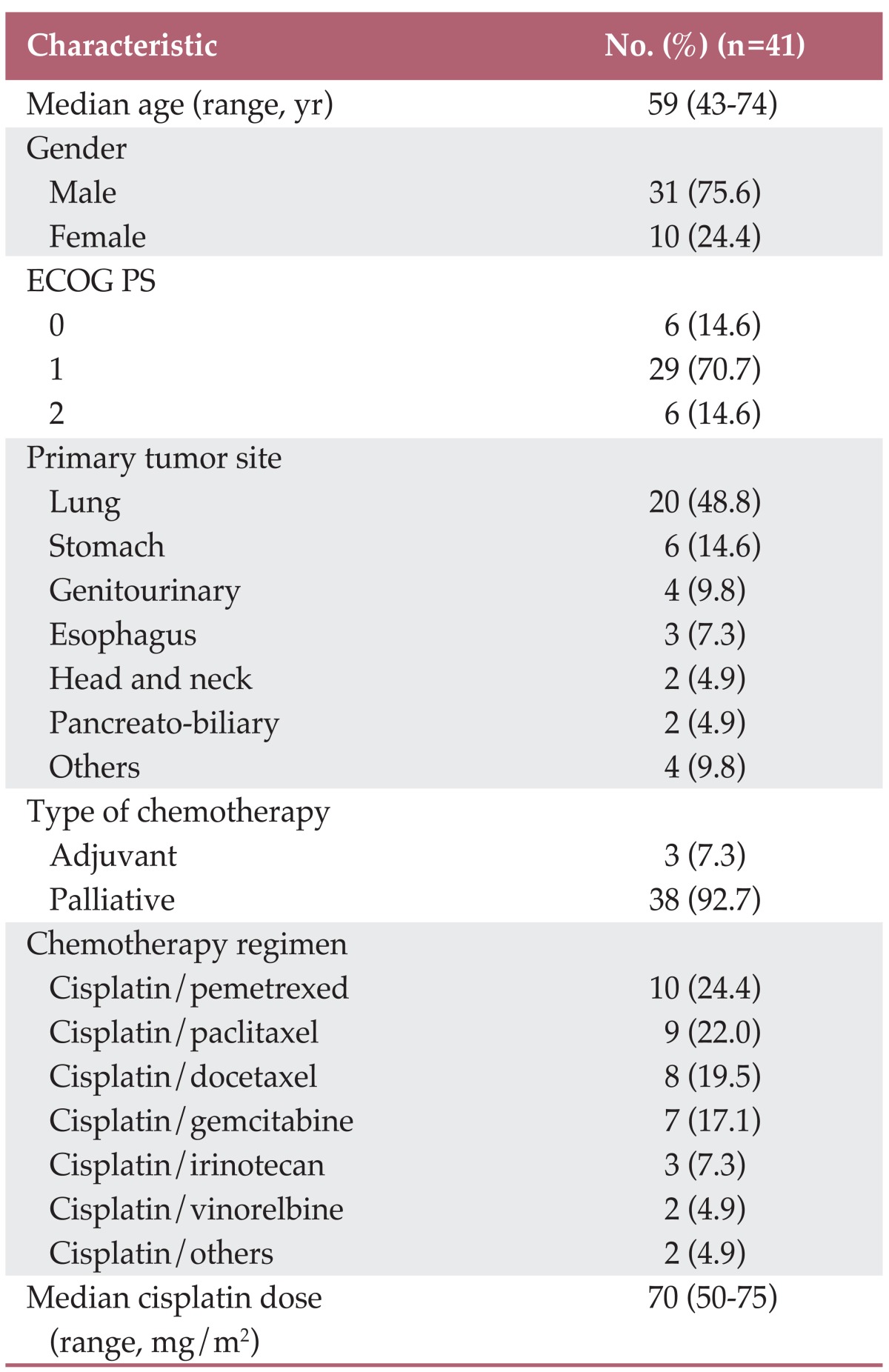
ECOG, Eastern Cooperative Oncology Group; PS, performance scale.
1. Antiemetic efficacy
Of the 41 patients, analysis for antiemetic efficacy was performed for 39 patients. Two patients were excluded from the analysis because of major study violations. One patient was not a chemotherapy-naïve patient and the other received a low dose of ramosetron. The CR rate was 92.3% in the overall phase, 94.9% in the acute phase, and 92.3% in the delayed phase (Table 2). The absolute CR rate was 46.2% in the overall phase (74.4% in the acute phase and 51.3% in the delayed phase).
Table 2.
Antiemetic efficacy (n=39)
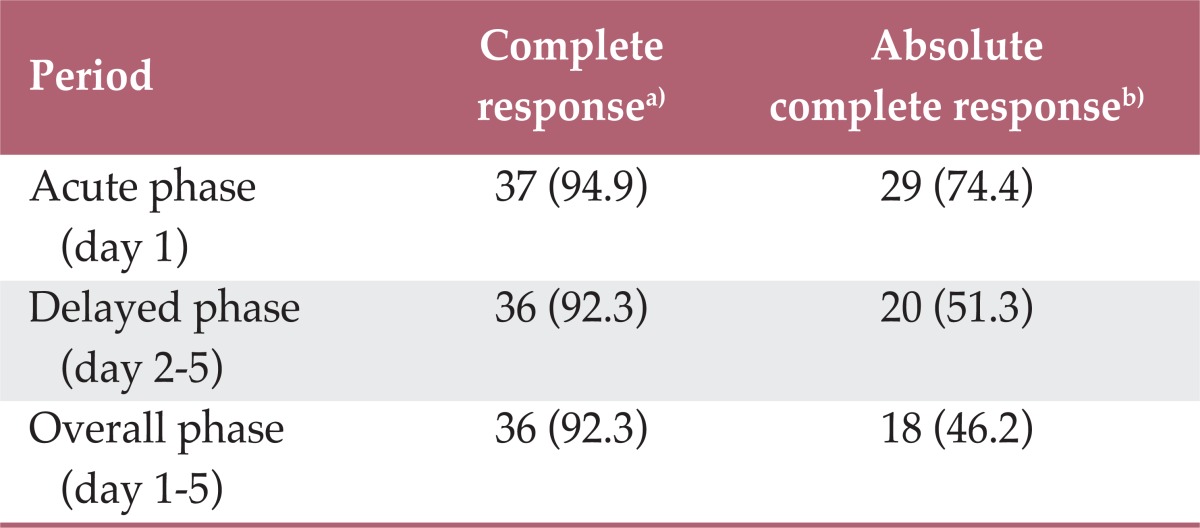
Values are presented as number (%). a)Defined as no emesis and no rescue medication, b)Defined as complete response plus no nausea
Median nausea scores during the overall, acute, and delayed phases were 2 (interquartile range [IQR], 0-4), 0 (IQR, 0-1), and 0 (IQR, 0-4), respectively. Mild nausea (score of 1-3 on the visual analogue scale) was observed in 10% of patients in the acute phase and in 13% of patients in the delayed phase (Table 3). Moderate-to-severe nausea (score of 4-10 on the visual analogue scale) was observed in 15% and 36% of patients in the acute and delayed phases, respectively.
Table 3.
Nausea visual analogue scale (n=39)
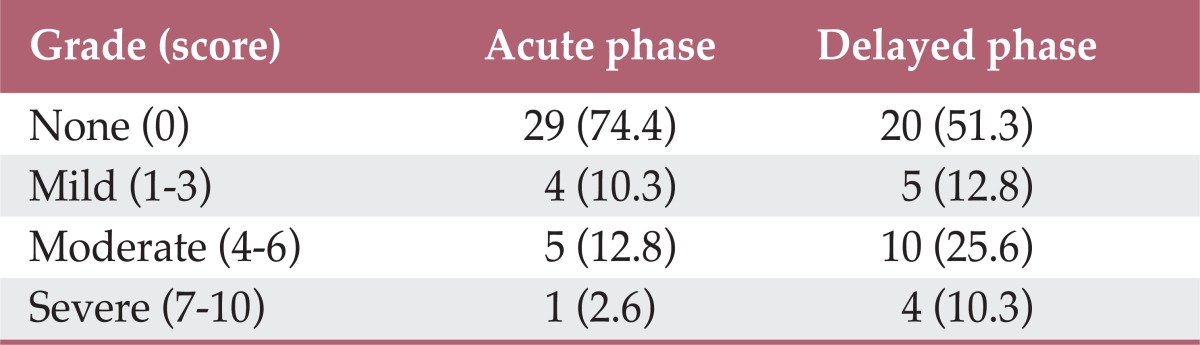
Values are presented as number (%).
2. Adverse events
There was no occurrence of additional serious adverse events associated with ramosetron. Overall adverse events according to CTCAE v.3.0 during chemotherapy are shown in Table 4. The most common grade 3/4 hematologic toxicity was neutropenia, with an incidence of 12%, followed by thrombocytopenia (10%). Regarding non-hematologic toxicities, 5% of patients experienced grade 3/4 diarrhea.
Table 4.
Adverse events according to CTCAE version 3 (n=41)
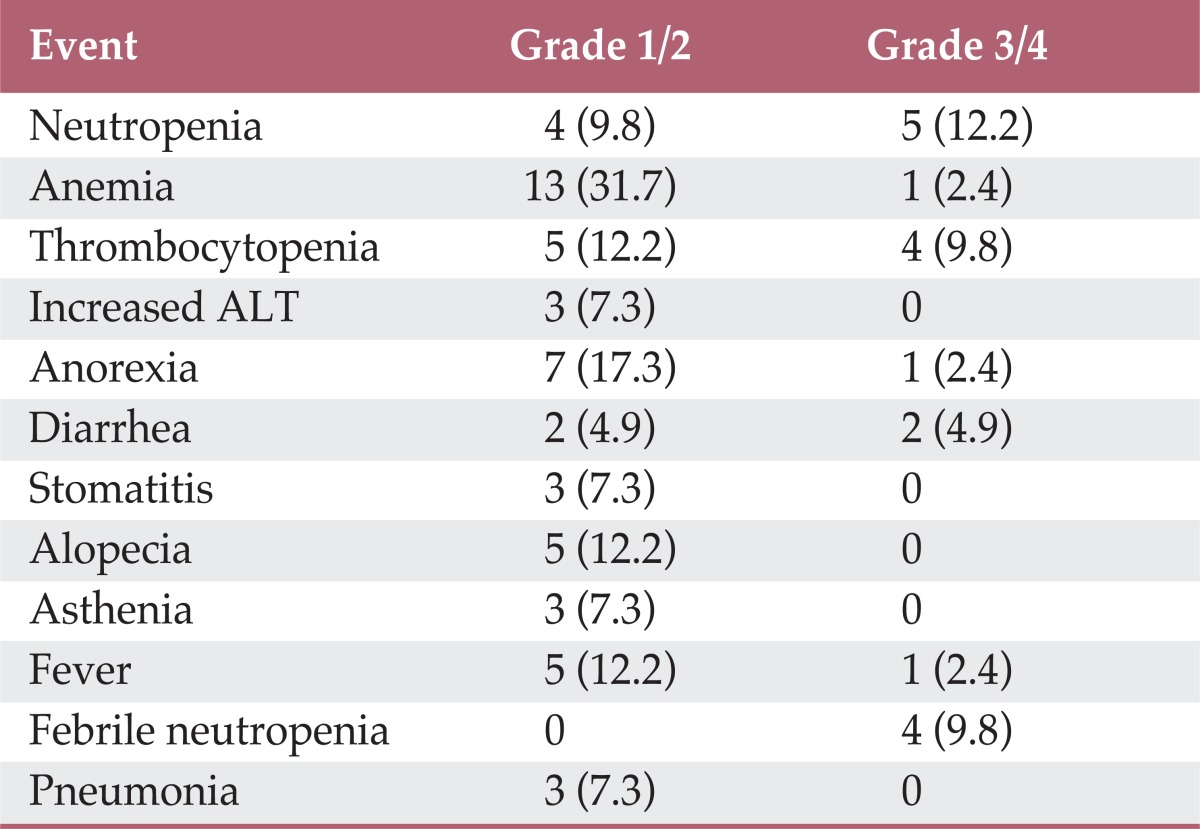
Values are presented as number (%). CTCAE, Common Toxicity Criteria for Adverse Events; ALT, alanine aminotransferase.
Discussion
In the current study, the RAD regimen showed significant efficacy for prevention ofcisplatin-induced CINV in chemonaïve cancer patients. Ninety-two percent of patients did not experience vomiting episodes, nor did they receive rescue medication for CINV during the overall phase. This CR rate is considerably high compared with that reported in other studies. The CR rates of a two-drug regimen with ramosetron plus dexamethasone for prevention of cisplatin-induced CINV were reported to range from 68% to 85% in the acute periodand from 58% to 75% in the delayed period [15,16,18]. In their study with ondansetron, Hesketh et al. [19] reported that CR rates for a triple-drug regimen of aprepitant, dexamethasone, and the 5-HT3 antagonist were 89%, 75%, and 73% in acute, delayed, and overall phases, respectively. Longo et al. [20] conducted a study evaluating a three-drug regimen with palonosetron for prevention of CINV in patients receiving highly emetogenic chemotherapy. The CR rates in the acute, delayed, and overall periods were 98%, 73%, and 70%, respectively. In another triple regimen study with palonosetron, Herrington et al. [9] reported CR rates in the acute, delayed, and overall phases of 96%, 93%, and 93%, respectively, which was comparable to our results. In our trial, the CR rate was 95% in the acute period. Only two patients experienced episodes of vomiting during the first 24 hours after initiation of chemotherapy: one was a 58-year-old male with bladder cancer receiving cisplatin plus gemcitabine chemotherapy and the other was a 54-year-old male with small cell lung cancer receiving cisplatin plus irinotecan. The CR rate in the delayed period was 92%. However, in the trial conducted by Herrington et al. [9], the proportion of patients receiving cisplatin-based chemotherapy was 55%, which was different from that observed in our study. However, in this trial, the proportion of female patients considered vulnerable to CINV was relatively low when compared with other studies.
Ramosetron belongs to a new class of selective 5-HT3 receptor antagonists. It is a tetrahydrobenzimidazole derivative, which is structurally different from ondansetron and granisetron, with more potent 5-HT3 receptor antagonizing effects than the reference compounds used in animal experiments [21,22]. In addition, because its half-life is known to be longer than that of ondansetron and granisetron [23], it can be administered once per day. Its known side effects include an elevation of hepatic transaminases, headache, diarrhea, and febrile sensation with a frequency of less than 1%. In this study, there was no occurrence of ramosetron-related serious adverse events. Although two patients (5% of cases) experienced grade 3 diarrhea, it could be considered a side effect of chemotherapeutic agents. Most adverse events were also acceptable toxicities which could be related to chemotherapy and were similar in comparison with other studies [11-13].
Aprepitant, the first NK-1 receptor antagonist to be developed, prevents binding of substance P to the NK-1 receptor forimprovement of CINV. Although the RAD regimen, ramosetron combined with aprepitant and dexamethasone, has been widely used in clinical practice in Asian countries for prevention of CINV, there are not yet any published data on this triple-drug combination.
Despite advances in control of vomiting by development of effective antiemetic agents, many patients still suffer from chemotherapy-induced nausea. In particular, delayed nausea tends to show resistance to treatment. In our study, the absolute CR rate, defined as CR plus no nausea, was 46% during the overall period. While 15% of patients experienced moderate-to-severe nausea during the acute period, 36% developed moderate-to-severe nausea during the delayed period. This result was similar to those reported byother studies. In the trial conducted by Hesketh et al. [19], 48% of patients had no nausea in the overall phase, and 9% and 25% of patients were reported to have significant nausea in the acute and delayed phases, respectively. In a recent study, Roscoe et al. [24] reported that delayed nausea could be improved by addition of dexamethasone on days 2 and 3, but not by the 5-HT3 receptor antagonist.
This study has some limitations. The patient sample size was relatively small, and the proportion of male patients was high. The effect of individual variable factors, such as alcohol consumption, chemotherapeutic agents administered in combination, and the impact of the cisplatin dose was not considered. However, to the best of our knowledge, this is the first prospectively conducted study on the efficacy of a three-drug regimen with ramosetron for prevention of CINV.
Conclusion
The results of this study showed that the RAD combination regimen is a very safe and effective antiemetic therapy for prevention of CINV in patients receiving highly emetogenic chemotherapy, although chemotherapy-induced nausea is still not completely overcome by use of this regimen. Based on the results of this study, we are currently conducting a prospective multicenter, randomized, single-blind phase III trial for comparison of RAD with ondansetron, aprepitant, and dexamethasone (NCT01536691).
Acknowledgments
This trial was supported in part by a research grant from the Investigator-Initiated Studies Program of the Merck Sharp & Dohme Corp. The opinions expressed in this paper are those of the authors and do not necessarily represent those of the Merck Sharp & Dohme Corp.
Footnotes
Conflict of interest relevant to this article was not reported.
References
- 1.Osoba D, Zee B, Pater J, Warr D, Latreille J, Kaizer L Quality of Life and Symptom Control Committees of the National Cancer Institute of Canada Clinical Trials Group. Determinants of postchemotherapy nausea and vomiting in patients with cancer. J Clin Oncol. 1997;15:116–123. doi: 10.1200/JCO.1997.15.1.116. [DOI] [PubMed] [Google Scholar]
- 2.Pollera CF, Giannarelli D. Prognostic factors influencing cisplatin-induced emesis: definition and validation of a predictive logistic model. Cancer. 1989;64:1117–1122. doi: 10.1002/1097-0142(19890901)64:5<1117::aid-cncr2820640525>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 3.Booth CM, Clemons M, Dranitsaris G, Joy A, Young S, Callaghan W, et al. Chemotherapy-induced nausea and vomiting in breast cancer patients: a prospective observational study. J Support Oncol. 2007;5:374–380. [PubMed] [Google Scholar]
- 4.National Comprehensive Cancer Network. Clinical practice guidelines in oncology: Antiemesis Version 1.2013. Fort Washington: National Comprehensive Cancer Network; 2013. [Google Scholar]
- 5.Roila F, Herrstedt J, Aapro M, Gralla RJ, Einhorn LH, Ballatori E, et al. Guideline update for MASCC and ESMO in the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting: results of the Perugia consensus conference. Ann Oncol. 2010;21(Suppl 5):v232–v243. doi: 10.1093/annonc/mdq194. [DOI] [PubMed] [Google Scholar]
- 6.Basch E, Prestrud AA, Hesketh PJ, Kris MG, Feyer PC, Somerfield MR, et al. Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2011;29:4189–4198. doi: 10.1200/JCO.2010.34.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hesketh PJ, Grunberg SM, Herrstedt J, de Wit R, Gralla RJ, Carides AD, et al. Combined data from two phase III trials of the NK1 antagonist aprepitant plus a 5HT 3 antagonist and a corticosteroid for prevention of chemotherapy-induced nausea and vomiting: effect of gender on treatment response. Support Care Cancer. 2006;14:354–360. doi: 10.1007/s00520-005-0914-4. [DOI] [PubMed] [Google Scholar]
- 8.Jordan K, Kinitz I, Voigt W, Behlendorf T, Wolf HH, Schmoll HJ. Safety and efficacy of a triple antiemetic combination with the NK-1 antagonist aprepitant in highly and moderately emetogenic multiple-day chemotherapy. Eur J Cancer. 2009;45:1184–1187. doi: 10.1016/j.ejca.2008.11.046. [DOI] [PubMed] [Google Scholar]
- 9.Herrington JD, Jaskiewicz AD, Song J. Randomized, placebo-controlled, pilot study evaluating aprepitant single dose plus palonosetron and dexamethasone for the prevention of acute and delayed chemotherapy-induced nausea and vomiting. Cancer. 2008;112:2080–2087. doi: 10.1002/cncr.23364. [DOI] [PubMed] [Google Scholar]
- 10.Koizumi W, Tanabe S, Nagaba S, Higuchi K, Nakayama N, Saigenji K, et al. A double-blind, crossover, randomized comparison of granisetron and ramosetron for the prevention of acute and delayed cisplatin-induced emesis in patients with gastrointestinal cancer: is patient preference a better primary endpoint? Chemotherapy. 2003;49:316–323. doi: 10.1159/000074533. [DOI] [PubMed] [Google Scholar]
- 11.Cheirsilpa A, Sinthusake T, Songsakkaesorn A, Visawaprasit S, Chulaka K, Changkuingdee N. Comparison of ramosetron and granisetron for the prevention of acute and delayed emesis in cisplatin-based chemotherapy: a randomized controlled trial. Jpn J Clin Oncol. 2005;35:695–699. doi: 10.1093/jjco/hyi192. [DOI] [PubMed] [Google Scholar]
- 12.Shi Y, He X, Yang S, Ai B, Zhang C, Huang D, et al. Ramosetron versus ondansetron in the prevention of chemotherapy-induced gastrointestinal side effects: a prospective randomized controlled study. Chemotherapy. 2007;53:44–50. doi: 10.1159/000098418. [DOI] [PubMed] [Google Scholar]
- 13.Kang YK, Park YH, Ryoo BY, Bang YJ, Cho KS, Shin DB, et al. Ramosetron for the prevention of cisplatin-induced acute emesis: a prospective randomized comparison with granisetron. J Int Med Res. 2002;30:220–229. doi: 10.1177/147323000203000302. [DOI] [PubMed] [Google Scholar]
- 14.Borjeson S, Clark-Snow R, Rinley R, Gralla RJ, Kris MG, Rittenberg CN. MASCC antiemesis tool (MAT) [Internet] Hillerod: Multinational Association of Supportive Care in Cancer; [cited 2009 Jun 1]. Available from: http://www.mascc.org/mc/page.do?sitePageId=88036. [Google Scholar]
- 15.Villalon A, Chan V. Multicenter, randomized trial of ramosetron plus dexamethasone versus ramosetron alone in controlling cisplatin-induced emesis. Support Care Cancer. 2004;12:58–63. doi: 10.1007/s00520-003-0528-7. [DOI] [PubMed] [Google Scholar]
- 16.Kim JH, Kim TW, Ryu MH, Chang HM, Lee SH, Lee JS, et al. A randomised crossover study comparing ramosetron plus dexamethasone with ramosetron alone in the prevention of cisplatin-induced emesis. Clin Drug Investig. 2005;25:191–197. doi: 10.2165/00044011-200525030-00005. [DOI] [PubMed] [Google Scholar]
- 17.A'Hern RP. Sample size tables for exact single-stage phase II designs. Stat Med. 2001;20:859–866. doi: 10.1002/sim.721. [DOI] [PubMed] [Google Scholar]
- 18.Voravud N, Sriuranpong V. Phase II trial of ramosetron plus dexamethasone in the prevention of cisplatin-induced nausea and vomiting. J Med Assoc Thai. 2005;88:1790–1796. [PubMed] [Google Scholar]
- 19.Hesketh PJ, Grunberg SM, Gralla RJ, Warr DG, Roila F, de Wit R, et al. The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin: the Aprepitant Protocol 052 Study Group. J Clin Oncol. 2003;21:4112–4119. doi: 10.1200/JCO.2003.01.095. [DOI] [PubMed] [Google Scholar]
- 20.Longo F, Mansueto G, Lapadula V, De Sanctis R, Quadrini S, Grande R, et al. Palonosetron plus 3-day aprepitant and dexamethasone to prevent nausea and vomiting in patients receiving highly emetogenic chemotherapy. Support Care Cancer. 2011;19:1159–1164. doi: 10.1007/s00520-010-0930-x. [DOI] [PubMed] [Google Scholar]
- 21.Miyata K, Kamato T, Yamano M, Nishida A, Ito H, Katsuyama Y, et al. Serotonin (5-HT)3 receptor blocking activities of YM 060, a novel 4,5,6,7-tetrahydrobenzimidazole derivative, and its enantiomer in anesthetized rats. J Pharmacol Exp Ther. 1991;259:815–819. [PubMed] [Google Scholar]
- 22.Miyata K, Yamano M, Kamato T, Akuzawa S. Effect of serotonin (5-HT)3-receptor antagonists YM060, YM114 (KAE-393), ondansetron and granisetron on 5-HT4 receptors and gastric emptying in rodents. Jpn J Pharmacol. 1995;69:205–214. doi: 10.1254/jjp.69.205. [DOI] [PubMed] [Google Scholar]
- 23.Nakajima M, Kanamaru M, Miura H, Takeshige T, Atsuta Y. Phase I clinical study of YM060 in healthy male volunteers: single-dose intravenous administration. Jpn J Clin Exp Med. 1994;71:2461–2468. [Google Scholar]
- 24.Roscoe JA, Heckler CE, Morrow GR, Mohile SG, Dakhil SR, Wade JL, et al. Prevention of delayed nausea: a University of Rochester Cancer Center Community Clinical Oncology Program study of patients receiving chemotherapy. J Clin Oncol. 2012;30:3389–3395. doi: 10.1200/JCO.2011.39.8123. [DOI] [PMC free article] [PubMed] [Google Scholar]


