Abstract
Outcomes of external beam radiotherapy (EBRT) in advanced medullary thyroid carcinoma (MTC) are largely unknown. Retrospective review of data from patients with MTC, diagnosed from June 1, 1970, through December 31, 2007. Overall survival and locoregional tumor control rates were calculated. Seventeen patients had adjuvant or palliative EBRT delivered to 41 sites. Six patients initially had adjuvant EBRT (median, 60.80 Gy); none had relapse in the treated area. Five patients with locoregional recurrence after surgery were treated (median, 59.40 Gy), and durable disease control was achieved in 3. Twelve patients received palliative EBRT to 29 sites of metastatic disease (median, 30.00 Gy), which provided sustained symptom relief at 45% of sites. Five- and ten-year overall survival rates were 44% and 19%, respectively. Adjuvant EBRT may be most effective for prevention of locoregional recurrence. EBRT may provide sustained control of advanced, metastatic disease in select patients.
Key words: medullary thyroid carcinoma, radiotherapy
Introduction
Medullary thyroid carcinoma (MTC) is a relatively rare malignancy that accounts for approximately 5 to 10% of thyroid cancers.1,2 Derived from the calcitonin-producing parafollicular cells, it arises sporadically in the majority of cases (80%) but also can occur in the context of multiple endocrine neoplasia syndromes.1,2
Appropriate initial treatment for MTC has long been considered to be total thyroidectomy and nodal dissection of the central compartment of the neck because up to 80% of patients with palpable disease will have nodal metastases.3 Significant controversy remains regarding the practice of nearest neighbor compartment dissection, but preoperative ultrasonography is recommended in all cases, with the aim of identifying cervical compartments with lymphadenopathy to target for dissection.4
Radiotherapy is sometimes offered as adjuvant treatment for advanced or invasive MTC; more often, it is used in a palliative setting for management of gross residual or recurrent disease.4 However, there is a paucity of data regarding outcomes of radiotherapy,1 the practice is controversial, and considerable uncertainty remains regarding indications for its use. Historically, some have viewed MTC as a radioresistant tumor, but recent series have questioned that notion.5-11
We sought to determine the effectiveness of external beam radiotherapy (EBRT) in the management of resected, recurrent, and metastatic MTC. We reviewed a cohort of patients with MTC who received adjuvant, salvage, or palliative EBRT at our institution.
Materials and Methods
After obtaining approval from the Mayo Clinic Institutional Review Board, we performed a retrospective review of data from all patients with MTC who were treated with adjuvant, salvage, or palliative EBRT at Mayo Clinic (Rochester, Minnesota, USA). All patients were diagnosed from June 1, 1970, through December 31, 2007. In accordance with Minnesota law, all living patients had authorized review of their medical records for research purposes before the study commenced. For patients treated with postoperative EBRT immediately following surgical resection and for patients treated with EBRT for unresectable locoregional recurrence, local disease control was defined as a complete response with no physical or imaging evidence of disease. The Kaplan-Meier method was used to estimate survival using JMP statistical software (version 8.0; SAS Institute Inc, Cary, North Carolina).
Results
Patient characteristics
We identified 17 patients with MTC diagnosed during the study period. The median age at diagnosis was 48 years (range, 14-76 years). Median duration of follow-up was 3.4 years (range, 0.1-21.9 years). Adjuvant, salvage, or palliative EBRT was delivered to a total of 41 sites.
Adjuvant and salvage external beam radiotherapy
Characteristics of the 11 patients receiving postoperative EBRT (adjuvant or salvage therapy) are shown in Table 1. Six patients received initial adjuvant EBRT to the neck, with or without inclusion of the mediastinum (median adjuvant dose, 60.80 Gy; range, 55.00-70.00 Gy) (Table 2). This occurred after surgery that was deemed complete (n=2), in the setting of gross residual disease (n=2), or when the amount of residual disease after surgery was unknown (n=2). None of the 6 patients had a relapse within the treatment volume (Table 2), with a median duration of local disease control of 6.3 years (range, 1.8-21.9 years). Three patients had long-term follow-up (>5 years) with durable control of local disease. This compares favorably to a 27% recurrence rate in patients treated with surgery alone at Mayo Clinic.12
Table 1.
Characteristics of patients treated with locoregional adjuvant or salvage external beam radiotherapy (n=11).
| Characteristic | Value |
|---|---|
| Age, median (range), years* 50 (20-76) | |
| Sex | |
| Male | 8 |
| Female | 3 |
| Cancer stage* | |
| IVa | 6 |
| IVb | 1 |
| IVc | 1 |
| Unknown | 3 |
| Margins* | |
| Positive | 2 |
| Negative | 5 |
| Unknown | 4 |
| Positive lymph nodes, number* | |
| 0 | 2 |
| 1-5 | 3 |
| 6-10 | 4 |
| 11-15 | 1 |
| >15 | 1 |
| Median (range) | 6 (0-27) |
| Calcitonin level before EBRT, pg/mL | |
| Undetectable | 2 |
| ≤5000 | 6 |
| >5000 | 2 |
| Unknown | 1 |
| Median (range) | 2350 (0-200,000) |
| Mediastinum involved | |
| Yes | 4 |
| No | 6 |
| Unknown | 1 |
*Characteristic was determined at the initial surgery (i.e., at the time of diagnosis). EBRT, external beam radiotherapy.
Table 2.
Treatment history and locoregional tumor control for patients receiving postoperative adjuvant or salvage external beam radiotherapy.
| Patient | Year | Total dose, Gy | Fractions, N. | Dose/fraction, Gy | Total treatment time, days | Tumor control | Duration of control, years |
|---|---|---|---|---|---|---|---|
| Adjuvant EBR | |||||||
| 1 | 1983 | 68.04 | 35 | 1.94 | 53 | Yes | 13.6 |
| 2* | 1984 | 55.00 | ND | ND | ND | Yes | 7.9 |
| 3 | 1986 | 61.68 | 32 | 1.93 | 42 | Yes | 21.9 |
| 4 | 1988 | 59.40 | 33 | 1.80 | 52 | Yes | 2.5 |
| 5 | 2002 | 60.00 | 30 | 2.00 | 42 | Yes | 1.8 |
| 6 | 2002 | 70.00 | 35 | 2.00 | 50 | Yes | 4.6 |
| Salvage EBRT | |||||||
| 7 | 1989 | 59.40 | 33 | 1.80 | 57 | Yes | 18.8 |
| 8 | 1992 | 35.00 | 14 | 2.50 | 17 | Yes | 5.4 |
| 9 | 1994 | 45.00 | 25 | 1.80 | 35 | Yes | 3.4 |
| 10 | 2000 | 70.00 | 35 | 2.00 | 48 | NA | NA° |
| 11 | 2001 | 70.00 | 35 | 2.00 | 47 | No | NA |
EBRT, external beam radiotherapy; NA, not applicable; ND, no data.
*Treatment-specific information was not available (initial treatment was at another institution).
°Patient died of an unrelated cause 5 days after completing EBRT.
Five patients were treated with salvage EBRT for locoregional recurrence after failure of initial surgery (median dose, 59.40 Gy; range, 35.00-70.00 Gy) (Table 2). For these 5 patients, disease status at the time of EBRT was considered not amenable to complete surgical removal. Margins at time of initial surgery were negative in 4 patients and unknown in 1 patient. Durable local disease control (complete response by physical examination and imaging) was achieved in 3 of the 5 patients. One patient died of an intracranial bleed unrelated to treatment 5 days after completing EBRT. Another patient received a total dose of 70.00 Gy to the neck to treat nodal recurrence after failure of initial surgery with negative margins. This patient ultimately had recurrence in the neck 54 months after salvage EBRT.
Palliative external beam radiotherapy for metastatic disease
Six of the 11 patients treated adjuvantly or for locoregional disease subsequently had metastases that were treated with palliative EBRT (17 sites). Six patients received only palliative EBRT for distant metastases (12 sites). The median palliative dose was 30.00 Gy (range, 19.80-50.00 Gy). This treatment provided documented, sustained relief of symptoms, with tumor control at 45% of irradiated sites (Table 3).
Table 3.
Treatment history and locoregional tumor control for patients receiving palliative external beam radiotherapy.
| Patient | Year | Anatomic location | Total dose, Gy | Fractions, N. | Dose/fraction, Gy | Total treatment time, days | Tumor control | Duration of control, years |
|---|---|---|---|---|---|---|---|---|
| 2 | 1989 | Spine | 50.00 | 25 | 2.00 | 34 | Yes | 3.3 |
| 1991 | Spine | 30.00 | 10 | 3.00 | 13 | Yes | 3.4 | |
| 1992 | Femur | 30.00 | 10 | 3.00 | 13 | No | NA | |
| 1992 | Femur | 30.00 | 10 | 3.00 | 13 | No | NA | |
| 1992 | Rib | 30.00 | 15 | 2.00 | 20 | No | NA | |
| 1992 | Spine | 28.80 | 16 | 1.80 | 16 | No | NA | |
| 1992 | Spine | 28.80 | 16 | 1.80 | 21 | No | NA | |
| 1992 | Humerus | 30.00 | 10 | 3.00 | 17 | No | NA | |
| 1992 | Humerus | 30.00 | 10 | 3.00 | 17 | No | NA | |
| 3 | 1994 | Ileum | 30.00 | 10 | 3.00 | 14 | Yes | 6.2 |
| 4 | 1989 | Spine | 30.00 | 10 | 3.00 | 10 | No | NA |
| 8 | 1992 | Orbit | 32.63* | 11* | 2.63* | 14 | Yes | 4.7 |
| 9 | 1994 | Mediastinum | 19.80 | 11 | 1.80 | 12 | No | NA |
| 10 | 1999 | Femur | 20.00 | 4 | 5.00 | 4 | Yes | 1.4 |
| 1999 | Shoulder | 30.00 | 10 | 3.00 | 13 | No | NA | |
| 1999 | Spine | 30.00 | 10 | 3.00 | 13 | No | NA | |
| 2000 | Shoulder | 20.00 | 5 | 4.00 | 6 | No | NA | |
| 12 | 2002 | Mediastinum | 30.00 | 10 | 3.00 | 11 | Yes | 4.7 |
| 2002 | Nodes | 25.00 | 10 | 2.50 | 14 | Yes | 3.8 | |
| 13 | 1976 | Skull | 20.00 | 8 | 2.50 | 11 | Yes | 0.9 |
| 14 | 1984 | Hip | 30.00 | 12 | 2.50 | 15 | Yes | 1.6 |
| 15 | 1989 | Spine | 40.00 | 20 | 2.00 | 28 | Yes | 2.7 |
| 1990 | Spine | 36.00 | 12 | 3.00 | 15 | Yes | 2.7 | |
| 1993 | Spine | 30.60 | 17 | 1.80 | 16 | No | NA | |
| 1993 | Spine | 36.00 | 12 | 3.00 | 12 | No | NA | |
| 16 | 1991 | Spine | 30.00 | 10 | 3.00 | 11 | Yes | NA |
| 1993 | Spine | 24.00 | 12 | 2.00 | 15 | No | NA | |
| 1993 | Brain | 30.00 | 12 | 2.50 | 12 | No | NA | |
| 17 | 2004 | Skull | 30.00 | 10 | 3.00 | 11 | Yes | 0.3 |
EBRT, external beam radiotherapy; NA, not applicable.
*Patient 8 received palliative radiotherapy to the right orbit using a single right lateral beam. The intended dose was 33.00 Gy in 11 fractions. For the first fraction, the patient received 3.00 Gy using an 18-MV photon beam prescribed to a depth of 3.2 cm. The patient’s subsequent treatment (10 fractions, 3.00 Gy per fraction) was delivered using a 6-MV photon beam to a depth of 1.5 cm. The contribution to this final prescription depth (1.5 cm) from the first fraction was 2.63 Gy. The table shows the total dose delivered to the final prescription point during this course of treatment (32.63 Gy in 11 fractions).
Survival
A Kaplan-Meier curve of overall survival (OS) is shown in Figure 1. The 5-year and 10-year OS rates were 44% and 19%, respectively. The median survival was 48 months. For the 6 patients treated with postoperative EBRT after the initial diagnosis or for salvage of locoregional recurrence (without evidence of distant metastasis at the time of EBRT), the median OS was also 48 months.
Figure 1.
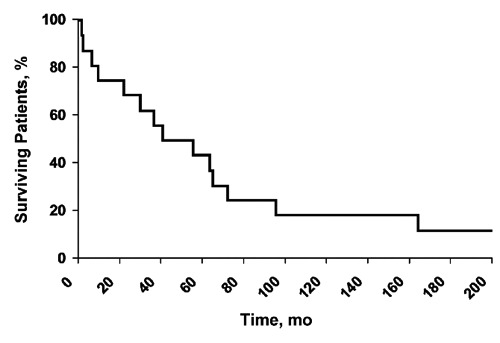
Overall survival of patients with medullary thyroid carcinoma who received external beam radiotherapy (n=17).
Discussion
In the setting of clinically apparent MTC, clinicians often recommend a total thyroidectomy with central neck dissection and either image-guided or prophylactic lateral neck dissection.1,4 Patients with locoregionally advanced disease have high risk of recurrence after surgery for MTC, as do patients with locally invasive or incompletely resected disease. Only a minority of patients with lymph node-positive disease has undetectable calcitonin levels after surgery with curative intent,13 and locoregional recurrence affects up to half of patients with locally advanced or node-positive disease.14 Grozinsky-Glasberg et al.15 reported that patients with elevated calcitonin or evidence of distant metastasis had worse OS, and patients with cervical metastasis had higher risk of recurrence. Although controversial, MTC treatment guidelines from the American Thyroid Association advocate postoperative EBRT for patients with gross residual disease after the maximal amount of safely removable disease has been resected.4 In addition, these guidelines recommend consideration of adjuvant EBRT for patients with microscopically positive margins, as well as for patients with detectable calcitonin after surgery (but no metastasis), to combat extranodal spread. However, others have questioned the efficacy of treating MTC with EBRT because they consider MTC to be relatively radioresistant.5,6 Because of the paucity of data, controversy abounds. Although some earlier reports described the limited response of MTC to EBRT, new data on the efficacy in the adjuvant setting are now emerging.7-11 Brierley et al.9 reported that patients at risk of locoregional recurrence (i.e., microscopic residual disease, extraglandular spread, or lymph node metastasis) who received radiotherapy had an 86% locoregional relapse-free survival rate after 10 years; patients who did not receive such therapy had a 52% rate. In a study of patients with lymph node disease reported by Chow et al.,10 4 of 4 had locoregional control after adjuvant EBRT, whereas 1 of 3 who did not undergo treatment had locoregional control. Fife et al.7 described 51 patients treated from 1960 through 1992. The percentage of patients without local recurrence 5 years after EBRT was 100% for patients with negative margins, 65% for patients with microscopically positive margins, and 24% for patients with gross disease. A later report from the same institution described the effect of EBRT in patients with elevated calcitonin but no clinical evidence of disease after surgery;16 they concluded that EBRT improved the local relapse rate (29% vs 59%) without any effect on survival. Despite an earlier report from MD Anderson questioning the value of EBRT in the management of MTC,6 a more recent report confirmed that postoperative EBRT could effectively achieve locoregional control.11 In that study, 34 patients (10 with recurrent disease) with stage IVa through IVc disease were treated with a median dose of 60 Gy; the locoregional relapse-free survival rate was 87%. Three patients with gross residual disease had effective control with EBRT.
The current analysis further supports the growing body of data on the efficacy of adjuvant EBRT after initial surgery and salvage EBRT after disease recurrence. We studied 11 patients who received adjuvant or salvage EBRT for advanced-stage disease, yet only 1 had locoregional relapse during follow-up. Five of the 11 patients had follow-up greater than 5 years, which underscores the durability of control achieved with postoperative EBRT. It was not uncommon, however, for patients to eventually have metastatic disease develop outside the treatment volume. Five of the 11 patients had distant metastasis at time of EBRT. Of the other 6 patients, 3 eventually received EBRT for palliation of metastatic disease.
Chemotherapy has historically shown little efficacy in MTC, and unlike differentiated thyroid cancer; radioiodine has not affected disease outcomes. Clinical trials of MTC are examining the effects of several systemic agents, including tyrosine kinase inhibitors and other novel agents,1 and preliminary results are promising. Until such agents enter routine clinical practice, however, local palliative therapies, most prominently EBRT, remain important tools in the management of metastatic disease.11 Furthermore, EBRT offers the opportunity to manage symptoms in patients with distant spread of disease. In our experience, EBRT was not as effective in this setting, although many patients benefitted from improved symptom intensity and durable control of tumor growth at treated metastatic sites. Our study was limited by the inherent challenges of its retrospective design and by the lack of adequate, consistent documentation of symptoms such as pain over the almost 40-year study period. We did not attempt to evaluate any association between calcitonin levels and outcome, although this has been extensively studied elsewhere.15,17 We also did not have sufficient data to identify risk factors associated with locoregional failure, which could be used to better identify the patients who might benefit most from postoperative EBRT. Toxicity information was not consistently recorded in our patient group, but others have observed the relatively low toxicity of EBRT in the adjuvant or salvage setting; Schwartz et al.11 observed chronic morbidity from radiotherapy in only 9% of patients.
Patients with MTC potentially may survive for several years, even after development of metastatic disease (the 5-year OS in our patient cohort was 44%). With such longevity, locoregional control is important for improving quality of life. Some clinicians at our institution have raised concern about the possibility of postoperative EBRT making future surgical interventions more difficult. However, adjuvant EBRT may have the benefit of obviating the need for further locoregional surgical interventions, especially in high-risk patients. In our patients, adjuvant EBRT after the initial surgery effectively eliminated the need for subsequent surgery. Thus, continued recommendations for EBRT seem justified. Patients with high-risk features (e.g., extensive positive lymph nodes, extrathyroidal extension, gross residual disease, and microscopically positive surgical margins) should be considered for adjuvant EBRT, and patients with metastatic disease causing symptoms should be considered for palliative EBRT.
Conclusions
Medullary thyroid carcinoma appears to be a radiosensitive tumor. EBRT may be most effective in the adjuvant setting for the prevention of locoregional recurrence, but it may also have a role in providing durable and sustained control of locoregionally advanced or metastatic disease (or both) in select patients.
Acknowledgements
This paper was presented as a poster at the World Congress on Thyroid Cancer, Toronto, Canada, August 6-10, 2009.
References
- 1.Sippel RS, Kunnimalaiyaan M, Chen H.Current management of medullary thyroid cancer. Oncologist 2008;13:539-47 [DOI] [PubMed] [Google Scholar]
- 2.Jimenez C, Hu MI, Gagel RF.Management of medullary thyroid carcinoma. Endocrinol Metab Clin North Am 2008;37:481-96 [DOI] [PubMed] [Google Scholar]
- 3.Moley JF, DeBenedetti MK.Patterns of nodal metastases in palpable medullary thyroid carcinoma: recommendations for extent of node dissection. Ann Surg 1999;229:880-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kloos RT, Eng C, Evans DB, et al. American Thyroid Association Guidelines Task Force. Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid 2009;19:565-612 [DOI] [PubMed] [Google Scholar]
- 5.Williams CR, Brewer DB.Medullary carcinoma of the thyroid. Br J Surg 1969;56:437-43 [DOI] [PubMed] [Google Scholar]
- 6.Samaan NA, Schultz PN, Hickey RC.Medullary thyroid carcinoma: prognosis of familial versus sporadic disease and the role of radiotherapy. J Clin Endocrinol Metab 1988;67:801-5 [DOI] [PubMed] [Google Scholar]
- 7.Fife KM, Bower M, Harmer CL.Medullary thyroid cancer: the role of radiotherapy in local control. Eur J Surg Oncol 1996;22:588-91 [DOI] [PubMed] [Google Scholar]
- 8.Peixoto Callejo I, Americo Brito J, Zagalo CM, Rosa Santos J.Medullary thyroid carcinoma: multivariate analysis of prognostic factors influencing survival. Clin Transl Oncol 2006;8:435-43 [DOI] [PubMed] [Google Scholar]
- 9.Brierley J, Tsang R, Simpson WJ, et al. Medullary thyroid cancer: analyses of survival and prognostic factors and the role of radiation therapy in local control. Thyroid 1996;6:305-10 [DOI] [PubMed] [Google Scholar]
- 10.Chow SM, Chan JK, Tiu SC, et al. Medullary thyroid carcinoma in Hong Kong Chinese patients. Hong Kong Med J 2005;11:251-8 [PubMed] [Google Scholar]
- 11.Schwartz DL, Rana V, Shaw S, et al. Postoperative radiotherapy for advanced medullary thyroid cancer: local disease control in the modern era. Head Neck 2008;30:883-8 [DOI] [PubMed] [Google Scholar]
- 12.Boostrom SY, Grant CS, Thompson GB, et al. Need for a revised staging consensus in medullary thyroid carcinoma. Arch Surg 2009;144:663-9 [DOI] [PubMed] [Google Scholar]
- 13.Scollo C, Baudin E, Travagli JP, et al. Rationale for central and bilateral lymph node dissection in sporadic and hereditary medullary thyroid cancer. J Clin Endocrinol Metab 2003;88:2070-5 [DOI] [PubMed] [Google Scholar]
- 14.de Groot JW, Links TP, Sluiter WJ, et al. Locoregional control in patients with palpable medullary thyroid cancer: results of standardized compartment-oriented surgery. Head Neck 2007;29:857-63 [DOI] [PubMed] [Google Scholar]
- 15.Grozinsky-Glasberg S, Benbassat CA, Tsvetov G, et al. Medullary thyroid cancer: a retrospective analysis of a cohort treated at a single tertiary care center between 1970 and 2005. Thyroid 2007;17:549-56 [DOI] [PubMed] [Google Scholar]
- 16.Fersht N, Vini L, A’Hern R, Harmer C.The role of radiotherapy in the management of elevated calcitonin after surgery for medullary thyroid cancer. Thyroid 2001;11:1161-8 [DOI] [PubMed] [Google Scholar]
- 17.Rendl G, Manzl M, Hitzl W, et al. Long-term prognosis of medullary thyroid carcinoma. Clin Endocrinol (Oxf) 2008;69:497-505 [DOI] [PubMed] [Google Scholar]


