Abstract
Lymphoepithelioma-like carcinoma of the skin (LELCS) is a rare and poorly differentiated variant of squamous cell carcinoma. The lesion is histologically identical to undifferentiated nasopharyngeal carcinoma (lymphoepithelioma), but with Epstein-Barr virus involvement documented rarely. The first case of LELCS was described in 1988 by Swanson et al. and since there has been less than a total of 60 cases documented. This case review discusses a 87 year old man who presented to his primary care physician with a 2.5 cm solitary ulcerated nodular lesion on his right chest for two weeks. The patient ultimately had the lesion excised and sent for histological examination. The microscopic examination, ancillary studies used and differential diagnosis considered are discussed in detail in the following report. This case review aims to provide insight and approach to a rare cutaneous neoplasm, with the conclusions supporting a theory that LELCS is a separate entity from lymphoepithelioma.
Key words: lymphoepithelioma-like carcinoma of the skin, lymphoepithelioma, inflamed carcinoma
Case Report
Clinical history
A 87-year old male presented to his family physician with a two week history of a skin lesion on his right anterior chest. On physical exam, particular emphasis was on head and neck assessment. On inspection of the head and neck there were no gross abnormalities including asymmetry, swelling, discoloration and or trauma. Major lymph nodes were identified symmetrically on both sides of the neck. All cranial nerves were tested to be within normal limits of functioning. The oropharynx was visualized to be without obvious lesions or deformity. On examination of the chest, a solitary 2.5 cm light brown ulcerated polyploid growth was seen. The surrounding epidermis was without erythema or hemorrhage. No telangiectatic vessels were seen grossly.
During the course of getting worked up for possible metastatic disease, a head/neck CT was performed. The results of this scan were essentially normal anatomy without any obvious lesion present (including nasopharynx). The lesion was removed with the clinical diagnosis of an epidermal carcinoma. Since the excision the patient was been in good medical health with no recurrent tumor or distant metastatic spread.
Microscopic examination
Histopathology on low power showed an unremarkable epidermal surface, with no ulceration or dysplastic changes (Figure 1A). The architecture of the lesion was that of scattered nests of tumor cells with diffuse lymphocytic infiltrate between epithelial nests. On higher power examination (Figure 1B), the biphasic nature of the lesion became more apparent. The tumor cells were mainly polygonal in shape with an eosinophilic cytoplasm, containing vesicular nuclei, prominent atypia, numerous mitosis, diffuse lymphoplasmacytic infiltrate surrounding the epithelial nests and an infiltrating tumor margin. Histological features that may suggest a more aggressive form of LELCS such as involved surgical margins, lymphvascular and or perineural invasion were all negative on examination.1
Figure 1.
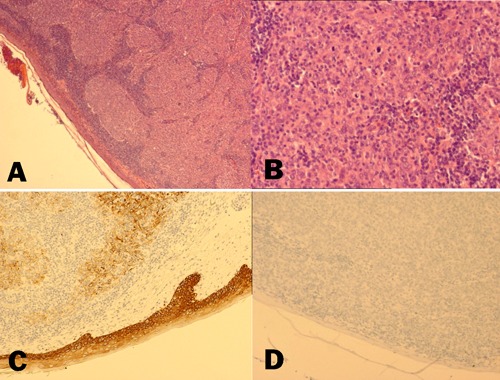
A) Hematoxylin & Eosin, 40×; B) Hematoxylin & Eosin, 200×; C) CK5/6, 100×; D) Epstein-Barr Virus, 100×.
Immunohistochemical (IHC) studies showed that the tumor cells were diffusely positively for epithelial differentiation (AE1/AE3 and EMA) and more specifically squamous cell involvement with CK5/6 (Figure 1C). Lymphoid cell markers (LCA, CD3 & CD20) were also helpful in identifying reactive nature of the surrounding lymphoid cells, while remaining negative for the epithelial tumor nests. Melanoma markers (S-100 & HMB45) and neuroendocrine markers (Chromogranin, Synaptophysin & CD56) were also negative for tumor cell involvement. The tumor cells also reacted negativity with Epstein-Barr virus (EBV) (Figure 1D). The full immunohistochemistry panel is summarized in Table 1.
Table 1.
Immunohistochemistry panel.
| Stain | Result |
|---|---|
| AE1/AE3 | + |
| CAM 5.2 | + |
| CK5/6 | + |
| EMA | + |
| HMWCK (34BE12) | + |
| CK7 | + |
| CK18 | + |
| CK19 | + |
| CK20 | * |
| CD3 | * |
| LCA | * |
| CD20 | - |
| CD56 | - |
| Chromogranin | - |
| Synaptophysin | - |
| S100 | - |
| HMB45 | - |
| EBV | - |
+ represents positive for tumor cells; * represents positive for lymphoid cells, negative for tumor cells; - represents negative for tumor cells.
The clinical history of unremarkable head and neck examination with supporting radiology correlate the theory that this lesion was a different entity from the nasopharyngeal counterpart. Therefore hematoxylin and eosin (H&E), immunohistochemistry (IHC) and clinical history were all consistent with the diagnosis of lymphoepithelioma – like carcinoma of the skin (LELCS).
Discussion
LELCS is defined as a rare and poorly differentiated variant of squamous cell carcinoma, with prominent reactive inflammatory infiltrate mimicking undifferentiated nasopharyngeal carcinoma (lymphoepthelioma). Historically, majority of cases of lymphoepithelioma were found to have a relationship with Epstein-Barr virus (EBV), while LELCS neoplasms were not.2,3 A literature review revealed only one documented case of EBV-positive LELCS.4 This distinction is what often differentiates LELCS from lymphoeptheliomatous tumors of the nasopharynx.
Clinically both tumors most often present in the head and neck region as an enlarging erythematous nodular lesion, however, there have been reports from numerous other sites with similar tumors including the gastrointestinal tract, genitourinary tract and reproductive organs.5-7 LELCS is a slow indolent growing epithelial neoplasm with moderate tendency to metastasize.8 The size of the lesion varies among locations and reports, however the majority average between 2 to 3 cm in diameter. These tumors affect mainly elderly patients with equal distribution among males and females.
The differential diagnosis with LELCS is rather extensive including metastatic disease from nasopharyngeal carcinoma, lymphoma, poorly differentiated inflamed carcinoma, Merkel cell carcinoma and melanoma. Lymphoepithelioma is histologically identical to LELCS, and therefore needs to be ruled out clinically with imaging and history. This often includes CT scan of the chest with nasopharyngeal swabs. As previously stated the skin tumors have only been reactive for EBV-encoded RNA in one documented case.4,9-11 Poorly differentiated inflamed carcinoma’s, are often in the differential diagnosis due to the similar histological appearance as well. Poorly differentiated inflamed carcinomas in contrast have areas of well differentiated carcinoma or overlying carcinoma in situ. With dense lymphoid infiltrate, lymphoma is often considered, however the latter does not present with an epithelial component. In contrast to this case, Merkel cell carcinoma would react positivity with neuroendocrine markers. Melanoma can be excluded by careful histological examination that lack residual melanocytes, and overlying melanoma in situ component. As well immunohistochemistry should show negativity for melanocytic markers including S100, Melan-A and HMB-45.
The microscopic examination has a dermal infiltrate of predominately lymphoid cells associated with enlarged, atypical epithelioid cells. The epithelioid cells may form small nests or clusters of tumor cells often being difficult to discern due to the heavy lymphoid infiltrate. On high magnification examination, the atypical cells show enlarged nuclei and prominent nucleoli, with vesicular chromatin. In some cases focal overlying SCC in situ may be identified.
Immunohistochemical profile is a critical aspect in the diagnosis of LELCS. The atypical epithelioid cells should be positive for cytokeratins, especially high molecular weight cytokeratins such as CK5/6 and CK903.12 Other positive markers include p63 and EMA (over 90% accuracy). Lymphoid markers, particularly T-cell markers, will highlight the dense background of lymphoid infiltrate.13 The other markers generally used are relevant to the individual clinical history and presentation of the patient.
LELCS is treated similarly to invasive SCC with wide local surgical excision being the standard of care with radiation reserved for tumor reoccurrence or lymph node involvement.1,14 Currently, LELCS is classified as a variant of SCC with intermediate malignant potential. Few cases of recurrence are reported, however, most patients enjoyed long term survival with no recurrence.
The association between lymphoepithelioma and EBV has been documented in several studies.9-11 There have been a total of 25 reports that correlate the theory that EBV involvement supports the diagnosis of lymphoepithelioma. EBV associated lymphoepithelioma has been documented in lungs, thymus, salivary glands and gastrointestinal tract. However, LELCS have been documented to have much higher variability in terms of anatomical location.
Conclusions
In conclusion, LELCS is a rare poorly differentiated variant of SCC with distinct pathogenesis differing from undifferentiated nasopharyngeal carcinoma. Standard morphology is often misleading and needs to be correlated with ancillary studies and full clinical history. The clinical work up includes head and body CT scans and extensive ENT examination to rule out metastatic disease. Despite similar histological presentations, the two diseases are treated with very different approaches. Lymphoepithelioma is treated with supervoltage radiotherapy, while LELCS is treated with surgical excision for non-aggressive forms. Additionally, this case highlights the rationalization that making the distinction between lymphoepithelioma and LELCS is crucial to patient care.
References
- 1.Gille TM, Miles EF, Mitchell AO, et al. Lymphoepithelioma-like carcinoma of the skin treated with wide local excision and chemoradiation therapy: a case report and review of the literature. Case Rep Oncol Med 2012;2012:241816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gulley ML, Amin MB, Nicholls JM, et al. Epstein-Barr virus is detected in undifferentiated nasopharyngeal carcinoma but not in lymphoepithelioma-like carcinoma of the urinary bladder. Hum Pathol 1995;26:1207-14 [DOI] [PubMed] [Google Scholar]
- 3.Iezzoni JC, Gaffey MJ, Weiss LM.The role of Epstein-Barr virus in lymphoepithelioma-like carcinomas. Am J Clin Pathol 1995;103:308-15 [DOI] [PubMed] [Google Scholar]
- 4.Aoki R, Mitsui H, Harada K, et al. A case of lymphoepithelioma-like carcinoma of the skin associated with Epstein-Barr virus infection. J Am Acad Dermatol 2010;62:681-4 [DOI] [PubMed] [Google Scholar]
- 5.Pittaluga S, Loke SL, So KC, et al. Clonal Epstein-Barr virus in lymphoepitheliomalike carcinoma of the stomach: demonstration of viral genome by in situ hybridization and Southern blot analysis. Mod Pathol 1992;5:661-4 [PubMed] [Google Scholar]
- 6.Pantelides NM, Ivaz SL, Falconer A, et al. Lymphoepithelioma-like carcinoma of the urinary bladder: A case report and review of systemic treatment options. Urol Ann 2012;4:45-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernando LR, Pilar SM, Carmen B, Lucia H.Lymphoepithelioma-like carcinoma of the uterine cervix. A case report studied by in situ hybridization and polymerase chain reaction for Epstein-Barr Virus. Arch Pathol Lab Med 2000;124:746-7 [DOI] [PubMed] [Google Scholar]
- 8.Cavalieri S, Feliciani C, Massi G, et al. Lymphoepithelioma-like carcinoma of the skin. Int J. of Immunopathol Pharmacol 2004;20:851-4 [DOI] [PubMed] [Google Scholar]
- 9.Carr KA, Bulengo-Ransby SM, Weiss LM, NIckoloff BJ.Lymphoepithelioma like carcinoma of the skin. A case report with immunophenotypic analysis and in situ hybridization for Epstein-Barr viral genome. Am J Surg Pathol 1992;16:1252. [PubMed] [Google Scholar]
- 10.Gillum PS, Morgan MB, Naylor MF.Absence of Epstein-Barr virus in lymphoepthelioma like carcinoma of the skin. Am J Dermatopathol 1996;18:478-82 [DOI] [PubMed] [Google Scholar]
- 11.Leung EYF, Yik YH, Chan JKC.Lack of demonstrable EBV in Asian lymphoepithelioma - like carcinoma of the skin. Am J Surg Pathol 1995;19:974-6 [DOI] [PubMed] [Google Scholar]
- 12.Requena L, Yus ES, Jimenez E.Lymphoepithelioma – like carcinoma of the skin. A light microscopic and immunohistochemical study. J Cutan Pathol 1994:21:541-8 [DOI] [PubMed] [Google Scholar]
- 13.Okamura JM, Barr RJ.Cutaneous lymphoepithelial neoplasms. Adv Dermatol 1997;12:227-94 [PubMed] [Google Scholar]


