Abstract
The study systematically reviews the hypnosis apps available via iTunes that were compatible with iPhone or iPad. Of 1455 apps identified on iTunes, 407 met inclusion criteria and were further reviewed. Most common hypnosis app targets were: weight loss (23%), boosting self-esteem (20%), and relaxation/stress reduction (19%). 83% of apps delivered hypnosis via audio track, and 37% allowed tailoring. Less than 14% of apps reported disclaimers. None of the apps reported having been tested for efficacy, and none reported being evidence-based. Although apps have the potential to enhance hypnosis delivery, it seems as though technology has raced ahead of the supporting science. Recommendations from clinical researchers and policy makers are needed to inform responsible hypnosis app development and use.
Smartphones and mobile devices have become ubiquitous, and with the rapid advances in technology, the types and numbers of healthcare and wellness applications (apps) that are available for consumers on these devices have increased to a great extent (Kailas, Chong, & Watanabe, 2010). According to the 2012 Consumer Health Apps Report, the number of consumer health apps in the Apple Store has increased from 2,993 in February 2010 to 13,619 in April 2012.
In particular, there has been a recent proliferation of hypnosis apps. Hypnosis has been used increasingly for healthcare and wellness purposes (Hartman & Zimberoff, 2011; Montgomery, David, Winkel, Silverstein, & Bovbjerg, 2002; Montgomery, Bovbjerg, Schnur et al., 2007; Montgomery, Schnur, & Kravits, 2012) and there is initial work indicating that Internet-based hypnosis interventions may be effective for a variety of outcomes, such as sleep, fatigue, mood, and quality of life (Farrell-Carnahan, Ritterband, & Bailey, 2010).
Apps have the potential to make hypnosis interventions more available and accessible to the public. However, there has been no review of the quality or content of these hypnosis apps. Additionally, little is known about the types of hypnosis apps that are available, their purpose, the features they contain and the degrees to which the available hypnosis apps incorporate evidence-based practices. Therefore, our objective in this study was to systematically review hypnosis apps available via iTunes that were compatible with iPhone or iPad.
Methods
A list of hypnosis applications was collected on June 22, 2012, using the Power Search function of iTunes version 10.6, available for download at www.apple.com/itunes. The following search terms were used separately: “hypnosis”; “hypnotherapy”; “hypnotic”; “hypnotize” (Montgomery, David, Winkel, Silverstein, & Bovbjerg, 2002). The search included apps compatible with both iPad and iPhone.
Data for the review was extrapolated from the apps’ description on iTunes. iTunes app descriptions typically included: an overall summary of the app, a list of app’s features, users’ ratings; customer reviews, and selected screenshots of the app. Apps that included basic and deluxe versions were counted as separate apps, as they could differ in their features. Each app description was reviewed by two independent raters (MS and SJM) to determine whether the app met inclusion criteria. Inclusion criteria were: 1) the app description mentioned the use of hypnosis, hypnotherapy or the user being hypnotized; 2) hypnosis targeted a symptom/problem/quality of life and was not solely for entertainment; 3) the app description was in English; and, 4) hypnosis had a written or oral verbal component (i.e., rather than just images or sounds).
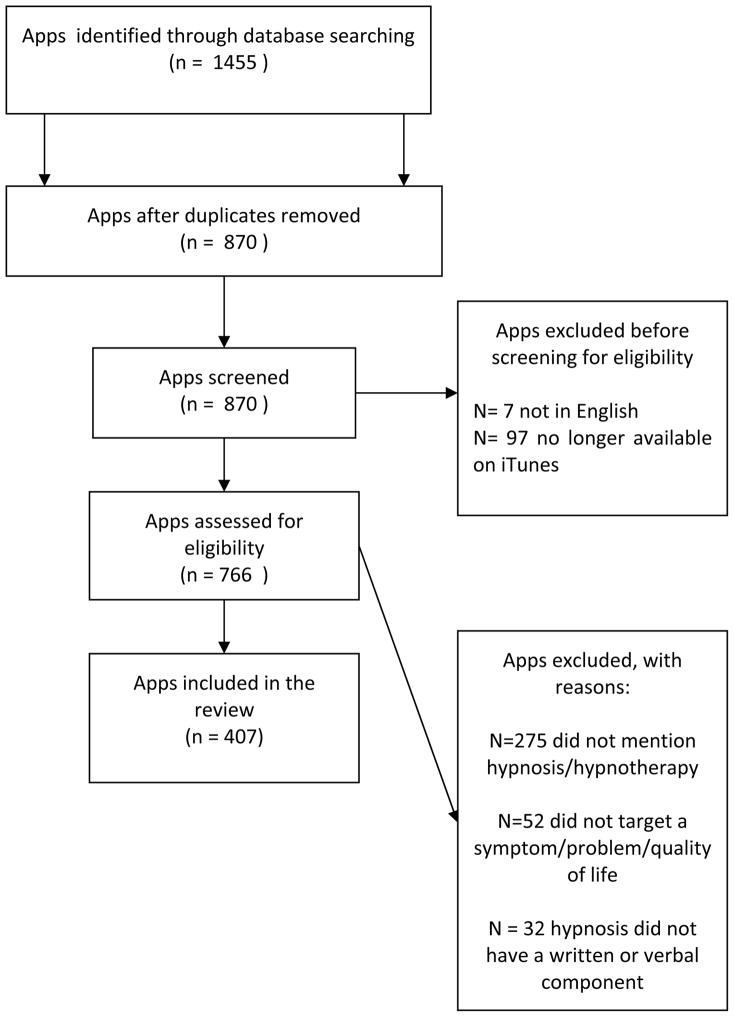
Out of 1455 apps identified using the key terms listed above, 575 were duplicates. The remaining 870 were screened independently by two of the authors (MS and SJM) to determine whether they met the inclusion criteria. During the one month review process (June 22, 2012 –July 22, 2012), 97 apps were removed from the list because they were no longer available on iTunes store, a common problem in studies investigating apps (Abroms, Padmanabhan, Thaweethai, & Phillips, 2011). Seven apps were excluded for not being in English.
Based on the inclusion criteria, the number of eligible apps was reduced from 870 to 407. Figure 1 details the reasons for exclusion. The inter-rater reliability between the authors reviewing the apps was .86, indicating strong agreement (Landis & Koch, 1977). Any discrepancies were discussed (with JBS and GHM) with reference to the original description until consensus was reached.
Figure 1.
PRISMA 2009 Flow Diagram
Data abstraction and app characteristics
The remaining 407 apps were reviewed by two authors (MS and KG), who completed a standardized data abstraction form. The data abstraction form included: (1) title of the app; (2) purpose of hypnosis; (3) hypnosis mode of delivery; (4) hypnosis app features; (5) licensure and/or trainings of the hypnotist/app developer; (6) disclaimers; (7) efficacy studies for the app; (8) whether the app was based on an existing theory; (9) price; (10) ratings from the users.
Data was abstracted and then compared by two authors (MS and KG); any lack of consensus was discussed with JBS and GHM until consensus was reached.
Results
Hypnosis app goals
Hypnosis apps were intended to help users achieve a variety of goals. The most common hypnosis app goals were: weight loss (22.60%) (k=92), boosting self-esteem (20.30%) (k=83), and relaxation/stress reduction (19.90%) (k=81) (see Table 1 for summary of these results).
Table 1.
Hypnosis app goals
| Hypnosis app goal | Frequencies | |
|---|---|---|
| % | k (number of apps) | |
| Weight loss | 22.60% | 92 |
| Increase self-esteem/confidence | 20.39% | 83 |
| Relaxation and stress reduction | 19.90% | 81 |
| Sleep improvement | 14.00% | 57 |
| Smoking cessation | 12.28% | 50 |
| Studying goals (e.g., facilitate learning, memory, organization) | 9.58% | 39 |
| Attracting others (e.g., facilitating romantic relationships) | 6.87% | 28 |
| Attracting financial success | 5.65% | 23 |
| Phobias | 5.65% | 23 |
| Happiness/feeling good | 5.40% | 22 |
| Improving the experience of pregnancy/ giving birth | 2.45% | 10 |
| Anger | 2.45% | 10 |
| Sport performance | 2.21% | 9 |
| Communication skills | 2.21% | 9 |
| Other (e.g., nail biting; depression; guilt; Irritable Bowel Syndrome; fatigue; migraines; preparing for job interviews) | < 2.00% | 8 |
Note: The frequencies add to more than 100% since one app could have multiple purposes
Hypnosis app features and mode of delivery
Eighty-three percent (k=337) of apps delivered hypnosis via audio track (i.e., a recorded audio hypnosis script). Thirteen percent (k=54) of the apps delivered hypnosis using visual means (i.e., reading the text of a hypnosis script), while the rest of the apps (4%, k=16) delivered hypnosis by both audio track and visual means.
Thirty-seven percent (k=151) of apps allowed users to tailor hypnosis by: 1) combining hypnosis audio tracks with other stimuli [23.83% (k=97) (e.g., soothing music or relaxing landscapes)]; 2) choosing the ending of the hypnosis session [17.93% (k=73) (e.g., falling asleep versus alertness)]; and, 3) choosing session length (9.82%) (k=40). Other less frequent ways to tailor the hypnosis apps included: customizing suggestions (k=6) or being able to choose a female or male voice (k=3). Apps could allow more than one way of tailoring.
Self-described professional title/training of the hypnotist/app developer
As for professional title of the hypnotist/app developer, 7.12% (k=29) of the apps mentioned the hypnotist being a “doctor”, with no specific information about the field.
In terms of hypnotist training, 34.64% (k=141) reported that the hypnotist was trained and/or certified in hypnosis or hypnotherapy. Specific training experiences were highly varied in their descriptions, and attempting to categorize and evaluate training experiences was beyond the scope of the present work.
Disclaimers
Fourteen percent (k=57) of the apps had disclaimers included in their description. Of these 57, 35.08% (k=20) specified that the app is not meant to substitute for a licensed professional and that it is advised to consult a professional for the problem in question; 29.82% (k=17) specified that is not advisable to use the app while driving or operating heavy machinery; 24.56% (k=14) specified that no dramatic result or magical solution should be expected from the hypnosis app, and 7.01% (k=4) mentioned that the developers are not licensed professionals.
Science and theory behind the apps
None of the 407 apps reported having been tested for efficacy, and none reported being evidence-based. Forty-eight percent (k=194) of the apps mentioned a theory guiding the use of hypnosis in the app description. Of these 194, 39.17% (k=76) mentioned hypnosis functioning by affecting the subconscious mind; 30.92% (k=60) mentioned neuro-linguistic programming; 16.49% (k=32) mentioned hypnosis functioning via relaxation and suggestions, and the rest (13.40%, k=26) used a number of other explanations for hypnosis (e.g., indicating that hypnosis works by changing cell memories, changing the DNA, changing theta waves).
Users’ rating and price
Ratings of the apps ranged from 1 to 5 stars, in increments of .5, with higher star ratings reflecting greater user satisfaction. Of the 144 (35.38%) apps which were rated, 8.33% (k=12) received ratings between 2–3 stars, 52.08% (k=75) received ratings between 3 and 4 stars and 13.9% (k=57) apps received between 4–5 stars.
Thirteen percent (k=53) of the apps were free. 13.75% (k=56) cost $0.99 cents; 34.15% (n=139) cost between $1.99–3.99; 32.67% (k=133) cost between $4.99–6.99 and 6.38% (k=26) cost over $7.99, with the most expensive one being $19.99.
Relationships among apps’ characteristics
We explored the relationships among the apps’ characteristics and, in particular, we were interested in qualifications and training of the hypnotist.
There was a significant association between self-described professional title (i.e., doctor) and training, indicating that the apps developed by “doctors” were more likely to report training and certifications, χ2 (1, 407) = 11.55, p = .001.
Results also showed a significant association between self-described professional title and the use of disclaimers. Apps developed by “doctors” were more likely to include disclaimers, χ2 (1, 407) = 4.86, p = .027.
There was also a significant association between inclusion of theory in the app description and mention of hypnotist training. Apps that reported theory were more likely to report the training of the hypnotist, χ2 (1, 407) = 5.11, p = .027.
Lastly, we explored the relationships among the other app characteristics such as tailoring, theory, and price. Results indicated that apps which allowed tailoring were more expensive, r(405) = −.17, p =.001, as were the apps which included theory, r (405) = −.10, p =.031, and those with higher user ratings, r(142) = .16, p = .047. There was an inverse association between price and the use of disclaimers, with the use of disclaimers being associated with less expensive apps, r(405) = −.11, p =.021.
Discussion
We reviewed the content of 407 hypnosis apps that were available through iTunes in June-July 2012 to determine their goal, the features they contain and the degree to which the available hypnosis apps incorporate evidence-based practices. Below, we will review and discuss the findings, and present our recommendations for future, responsible, evidence-based hypnosis app development.
Hypnosis app goals
Our findings indicate that hypnosis apps have been developed to help users achieve a variety of goals, ranging from improving health behaviors (e.g., weight loss, smoking cessation) to encouraging financial success. There is evidence that hypnosis is effective in treating some of the goals that the hypnosis apps where intended for such as distress (Schnur, Kafer, Marcus, & Montgomery, 2008; Schnur, Bovbjerg, David et al., 2008), weight loss (Kirsch, 1996), and pain management (Holroyd, 1996; Milling, Kirsch, Allen, & Reutenauer, 2002; Montgomery, DuHamel, & Redd, 2000). However, there is no empirical evidence to support many of the intended hypnosis targets, such as attracting a romantic partner. This is a serious concern for apps developed for a psychotherapeutic purpose. At best, apps not supported by empirical evidence are misleading, at worst, unethical. Although enthusiasm for using the app format to deliver hypnosis is understandable, it is misleading to present hypnosis apps as a panacea.
Recommendation #1
It is our recommendation that future hypnosis apps be based on empirical evidence, indicating that hypnosis is effective for the proposed goal, which has been published in a peer-reviewed journal.
Hypnosis app features and mode of delivery
Delivering hypnosis in an app format has many unique benefits as compared to face-to-face hypnosis. For example, apps are available at anytime, anywhere, and are not dependent on the schedule of a hypnotist or traveling to an office. Additionally, although many hypnotists tailor aspects of hypnosis as part of clinical practice (e.g., imagery, speed, volume), a single clinician cannot or does not typically allow for some types of tailoring permitted by apps (e.g., gender of hypnotist, background images (e.g., choosing to watch various scenes on video while listening to the hypnosis). However, it should be noted that as “cool” as many of these tailoring options are, to our knowledge, there has been no empirical research on whether all tailoring options are equally effective and/or which tailoring options are best for whom.
Recommendation #2
Tailoring options should be based on empirical support for their efficacy and should be guided by a combination of patient preferences and evidence.
Self-described professional title/training of the hypnotist/app developer
As for professional title of the hypnotist/app developer, it is a concern that only a very small percentage (7%) of the apps mentioned the hypnotist having a professional title (i.e., “doctor”) and the fields were not always specified in the app descriptions. Consumers purchasing these apps are uninformed about the credentials or training of the hypnosis app developers.
Recommendation #3
Hypnosis apps intended for therapeutic purposes should be developed by licensed healthcare providers with hypnosis training and experience. If hypnosis app developers intend for their hypnosis apps to be used to achieve psychotherapeutic goals, then it is critical that hypnosis app development be within areas of competency and scope of practice.
Approximately one-third (34.6%) of app developers/hypnotists reported that they are trained or certified in hypnosis/hypnotherapy. Unfortunately, this information might be overrated in this day of age where certification and proof of training can be easily bought online with no actual effort and the consumers might not be aware of this state of affairs, and might assume that certification means adequate training. This is a serious concern as Eichel (2001) has shown that certifications can be purchased (even for cats!) over the Internet with a credit card.
Recommendation #4
Hypnosis app developers should be able to prove adequate training in hypnosis under supervision, and this training should be verifiable by consumers.
Disclaimers
On a similar note, it is also concerning that such a limited number of apps included disclaimers in their description. Disclaimers are a critical aspect of informed consent. Consumers buying an app should clearly understand the intent, limits, and potential risks and benefits of the app (APA, 2003).
Recommendation #5
Hypnosis apps should be accompanied by at minimum a disclaimer, and preferably by an implied consent document (APA, 2003; Recupero & Rainey, 2005).
Science and theory behind the apps
Perhaps the most concerning aspect of all to us, was the total lack of evidence-based (empirically tested) apps. None of the apps reported being tested for their intended purpose and none reported being based on peer-reviewed work. Additionally, the theory guiding some of the app development was scientifically unsound at best. For example, NLP has limited empirical support (Witkowski, 2010), and to our knowledge, no research study has shown thus far that hypnosis might work by changing DNA.
Recommendation #6
Hypnosis apps should be based on evidence supporting both their efficacy/effectiveness as well as their hypothesized mechanism (David & Montgomery, 2011) The gold standard would be a randomized controlled trial (RCT) supporting the efficacy of each hypnosis app.
User’s ratings and price
The availability and accessibility of apps certainly explains their appeal, with users being able to enjoy hypnosis tailored as they like, for as long as they want and at a time of their choosing for free or typically less than $5.00! Results indicated that apps which allowed tailoring or included theory were more expensive, as were the ones which received higher user ratings. It would be interesting to correlate app price and user’s ratings with app effectiveness. However, the lack of any information about app effectiveness precludes such an exploration.
Future directions
To summarize, although apps have the potential to enhance hypnosis delivery, it seems as though technology has raced ahead of the supporting science. Unfortunately, this situation leaves consumers unable to judge which hypnosis apps are most likely, based on scientific evidence, to offer them clinical benefit. We propose that one way to improve the quality of hypnosis apps, and to provide consumers with a useful selection tool would be for national and international hypnosis organizations (e.g., Division 30 of the American Psychological Association, Society for Clinical and Experimental Hypnosis) to develop an app approval process (e.g., an app “seal of approval”). Apps could be submitted for approval to professional organizations, and could be rated according to a quality checklist (see Figure 2 for a draft version of such a checklist). Apps which met all criteria could be granted an organizational “seal of approval.” This would allow hypnosis leaders to shape future app development, and could improve consumer decision-making with regard to hypnosis apps. Apps are a fascinating tool, with tremendous potential, but it is our contention that they need to be developed and tested as rigorously and carefully as any face-to-face intervention.
Figure 2.
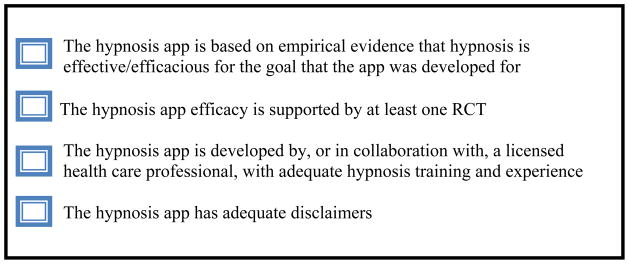
Hypnosis app quality checklist
References
- Abroms L, Padmanabhan N, Thaweethai L, Phillips T. iPhone apps for smoking cessation: A content analysis. American Journal of Preventive Medicine. 2011;40 (3):279–285. doi: 10.1016/j.amepre.2010.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association. Ethical principles of psychologists and code of conduct. 2003 http://www.apa.org/ethics/code/index.aspx.
- David D, Montgomery GH. The scientific status of psychotherapies: A new evaluative framework for evidence-based psychosocial interventions. Clinical Psychology: Science and Practice. 2011;18(2):89–99. [Google Scholar]
- Eichel SKD. Credentialing: It may not be the cat’s meow. 2011 Http://www.dreichel.com/articles/dr_zoe.htm.
- Farrell-Carnahan L, Ritterband L, Bailey E, Thorndike F, Lord H, Baum L. Feasibility and preliminary efficacy of a self-hypnosis intervention available on the web for cancer survivors with insomnia. Electronic Journal of Applied Psychology. 2010;6(2):10–23. [Google Scholar]
- Hartman D, Zimberoff D. Hypnosis and hypnotherapy in the milieu of integrative medicine: Healing the mind/body/spirit. Journal of Heart-Centered Therapies. 2011;14(1):41–75. [Google Scholar]
- Holroyd J. Hypnosis treatment of clinical pain: Understanding why hypnosis is useful. International Journal of Clinical and Experimental Hypnosis. 1996;44(1):33–51. doi: 10.1080/00207149608416066. [DOI] [PubMed] [Google Scholar]
- Kailas A, Chong CC, Watanabe F. From mobile phones to personal wellness dashboards. IEEE Pulse. 2010;1(1):57–63. doi: 10.1109/MPUL.2010.937244. [DOI] [PubMed] [Google Scholar]
- Kirsch I. Hypnotic enhancement of cognitive-behavioral weight loss treatments: Another meta-reanalysis. Journal of Consulting and Clinical Psychology. 1996;64(3):517–519. doi: 10.1037/0022-006X.64.3.517. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- Milling LS, Kirsch I, Meunier SA, Levine MR. Hypnotic analgesia and stress inoculation training: Individual and combined effects in analog treatment of experimental pain. Cognitive Therapy and Research. 2002;26(3):355–371. [Google Scholar]
- Montgomery GH, David D, Winkel G, Silverstein JH, Bovbjerg DH. The effectiveness of adjunctive hypnosis with surgical patients: A meta-analysis. Anesthesia & Analgesia. 2002;94:1639–1645. doi: 10.1097/00000539-200206000-00052. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Schnur JS, Kravits K. Hypnosis for cancer care: Over 200 years young. CA A Cancer Journal for Clinicians. 2012 doi: 10.3322/caac.21165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery GH, Bovbjerg D, Schnur J, David D, Goldfarb A, Weltz C, Schechter C, Graff-Zivin J, Tatrow K, Price D, Silverstein JH. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. Journal of National Cancer Institute. 2007;99:1304–1312. doi: 10.1093/jnci/djm106. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, DuHammel KN, Redd WH. A meta-analysis of hypnotically induced analgesia: How effective is hypnosis? International Journal of Clinical and Experimental Hypnosis. 2000;48(2):138–153. doi: 10.1080/00207140008410045. [DOI] [PubMed] [Google Scholar]
- Recupero PR, Rainey SE. Informed consent to e-therapy. American Journal of Psychotherapy. 2005;59(4):319–331. doi: 10.1176/appi.psychotherapy.2005.59.4.319. [DOI] [PubMed] [Google Scholar]
- Schnur JB, Kafer I, Marcus C, Montgomery GH. Hypnosis to manage distress related to medical procedures: A meta-analysis. Contemporary Hypnosis. 2008;25(3–4):114–128. doi: 10.1002/ch.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnur JB, Bovbjerg DH, David D, Tatrow K, Goldfarb AB, Silverstein JH, Welts CR, Montgomery GH. Hypnosis decreases surgical distress in excisional breast biopsy patients. Anesthesia & Analgesia. 2008;106(2):440–444. doi: 10.1213/ane.0b013e31815edb13. [DOI] [PubMed] [Google Scholar]
- Witkowski T. Thirty-five years of research on Neuro-Linguistic Programming. NLP research data base. State of the art or pseudoscientific decoration? Polish Psychological Bulletin. 2010;41(2):58–66. doi: 10.2478/v10059-010-0008-0. [DOI] [Google Scholar]