Summary
Background and objectives
p-Cresyl sulfate and indoxyl sulfate contribute to cardiovascular disease and progression of renal disease. Renal clearance of both solutes mainly depends on tubular secretion, and serum concentrations are widely dispersed for any given stage of CKD. From this information, it is inferred that estimated GFR is not a suitable proxy of the clearance of these solutes. Formal clearance studies have, however, not been performed to date.
Design, setting, participants, & measurements
This study analyzed renal clearances of p-cresyl sulfate and indoxyl sulfate in the Leuven CKD cohort (NCT00441623; inclusion between November of 2005 and September of 2006) and explored their relationship with estimated GFR. Multivariate linear regression models were built to evaluate contributions of estimated GFR, demographics, and generation rates to p-cresyl sulfate and indoxyl sulfate serum concentrations.
Results
Renal clearances were analyzed in 203 patients with CKD stages 1–5. Indoxyl sulfate clearances (median=17.7, interquartile range=9.4–33.2 ml/min) exceeded p-cresyl sulfate clearances (median=6.8, interquartile range=3.4–12.0 ml/min) by about threefold. A linear relationship was observed between estimated GFR and clearances of p-cresyl sulfate (R2=0.50, P<0.001) and indoxyl sulfate (R2=0.55, P<0.001). In multivariate regression, p-cresyl sulfate concentrations were associated (R2=0.75) with estimated GFR and generation rate (both P<0.001). Indoxyl sulfate concentrations were associated (R2=0.74) with estimated GFR, generation rate (both P<0.001), age (P<0.05), and sex (P<0.05).
Conclusions
Estimated GFR provides an acceptable estimate of renal clearance of p-cresyl sulfate and indoxyl sulfate. Remarkably, clearances of indoxyl sulfate exceed clearances of p-cresyl sulfate by approximately threefold, suggesting substantial differences between tubular transporter affinities and/or involvement of separate transporter systems for p-cresyl sulfate and indoxyl sulfate.
Introduction
CKD is accompanied by the accumulation of so-called uremic retention solutes. A metabolomic approach identified p-cresyl sulfate (PCS) and indoxyl sulfate (IS) among the most discriminating biomarkers of uremia (1). Several studies linked IS to progression of CKD, leading to the protein–metabolite hypothesis (2). Recently, a strong association between PCS and progression of CKD was reported (3). In addition, both PCS and IS were found to be associated with increased overall mortality and cardiovascular disease at various stages of CKD (4–8). Together, these studies and others suggest that PCS and/or IS are in the causal chain between the onset of CKD and adverse outcomes.
Glomerular filtration of PCS and IS is limited, because most of these colonic microbiome metabolites are highly (>90%) protein-bound (9). Renal excretion, thus, mainly depends on the versatile tubular transporter systems. Relevant transporters include the basolateral organic anion transporter 1 (OAT1; SLC22A6) and 3 (OAT3; SLC22A8) (10–12), the breast cancer resistance protein (BCRP), and the multidrug resistance protein 4 (MRP4) (13). Some also suggest a role for the organic anion transporting polypeptide 4C1 (OATP4C1; SLCO4C1) (14). How these molecular transporter mechanisms translate into renal clearances of PCS and IS has not been studied to date.
Early pharmacokinetic models assumed independence of glomerular clearance and tubular clearance. Because tubular plasma flow is the result of the renal blood plasma flow entering the glomeruli minus the filtered plasma flow or GFR, a more physiologic model has been developed, taking into account the dependence of tubular plasma flow and tubular clearance on glomerular filtration (15,16). In the absence of tubular secretion, the renal clearance is proportional to GFR. For solutes that undergo both glomerular filtration and tubular secretion, the renal clearance is a nonlinear function of the GFR. Protein binding, however, reduces glomerular filtration and affects tubular secretion. For solutes with a low unbound fraction, the renal clearance is then modeled as a near-linear function of the GFR (15).
Although advanced CKD stages are associated with higher median serum concentrations of both PCS and IS, individual serum concentrations for any given GFR are widely dispersed (5,7,8). One study examining associations between estimated GFR (eGFR) and serum concentrations of various uremic retention solutes showed a low coefficient of determination for both molecules (17). From this information, it was inferred that eGFR is not representative for evaluating the accumulation of uremic retention solutes that are mainly dependent of tubular secretion; this finding is in sharp contrast to the theoretical pharmacokinetic model predicting a near-linear association (15).
We studied the relationship between eGFR, serum concentrations, and renal clearances of PCS and IS in patients at various stages of CKD to test the validity of eGFR as a marker of the renal clearance of PCS and IS.
Materials and Methods
Study Population
This analysis is a secondary analysis of the Leuven Mild-to-Moderate CKD Study (clinicaltrials.gov NCT00441623; registered on February 28, 2007) (5). Prevalent CKD patients followed at the nephrology outpatient clinic of the University Hospitals Leuven who were 18 years of age or older and able to provide consent were eligible for inclusion. Patients were screened between November of 2005 and September of 2006. Data on baseline demographics and cause of kidney disease were collected at the time of informed consent. The study was performed according to the Declaration of Helsinki and approved by the ethics committee of the University Hospital Leuven. Informed consent was obtained from all patients.
Biochemical Measurements
At inclusion, blood was taken by venous puncture for measurement of creatinine (mg/dl), BUN (g/dl), PCS (µM), and IS (µM). Creatinine, BUN, and albumin were measured using standard laboratory techniques. eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) (18) and Modification of Diet in Renal Disease (MDRD) (19) Equations. We quantified PCS and IS using HPLC as described previously (20). The creatinine clearance and renal clearances of PCS and IS were calculated from 24-hour urinary collections. The fractional excretion of PCS and IS was calculated with the equation 100×(urinary solute × serum creatinine)/(serum solute × urinary creatinine)(%). Twenty-four-hour urinary collections were sampled when available at time of inclusion. Completeness was assessed using 24-hour urinary creatinine excretion. Collections were considered complete when 24-hour creatinine excretion was within 2 SDs of the mean creatinine excretion for the geographical region of this study derived from the INTERSALT study (21). Protein intake was calculated according to the formula by Maroni et al. (22) using 24-hour urinary urea nitrogen excretion and body weight (23).
Statistical Analyses
Data are expressed as mean (SD) for normally distributed variables or median (interquartile range [IQR]) for non-normally distributed variables. Differences were tested using parametric ANOVA, Kruskal–Wallis test, or chi-squared test as appropriate. Correlations were calculated by Pearson or Spearman rank correlation coefficients as indicated. For linear regression, model fit was tested by quintiles–quintiles plots and distribution analysis of studentized residuals. For analyses of reciprocal relationships, data were transformed as X=1/(1+x). For multivariate analysis, we used a stepwise approach, with Pinclude<0.20 and Pexclude>0.05. All statistical analyses were performed using SAS (version 9.1; SAS Institute, Cary, NC).
Results
Inclusion and Demographics
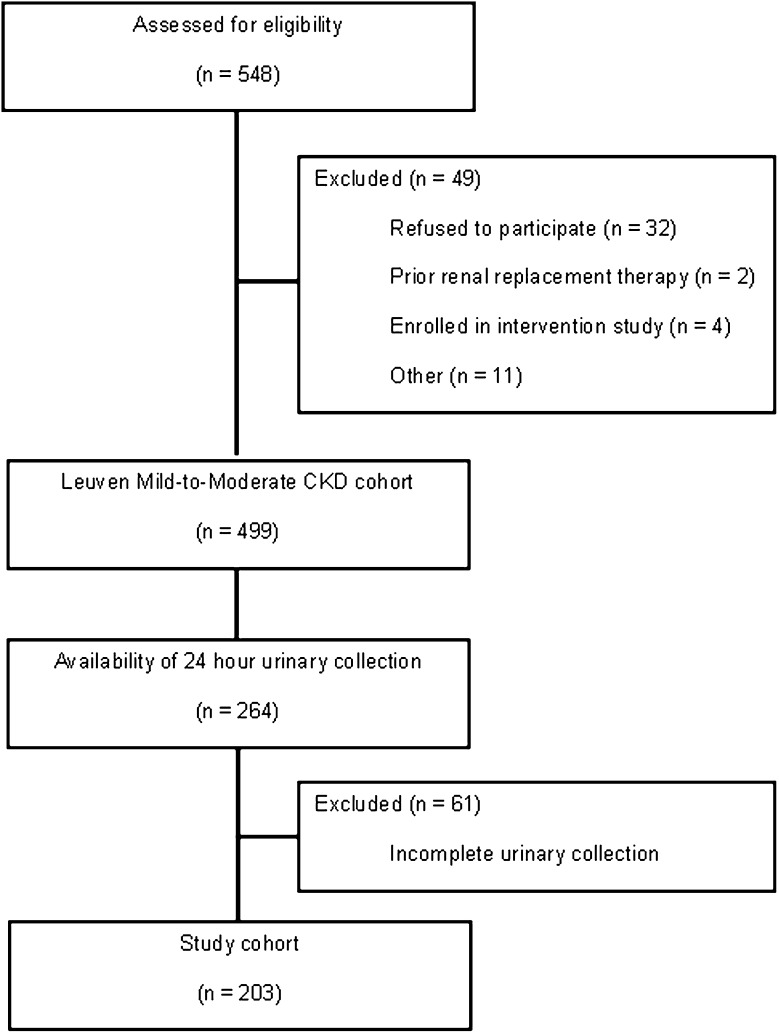
Between November of 2005 and September of 2006, 548 prevalent patients with CKD Kidney Disease Outcomes Quality Initiative stages 1–5 followed at the nephrology outpatient clinic of the University Hospitals Leuven, Belgium, were found eligible to be enrolled in the Leuven Mild-to-Moderate CKD Study; 499 patients providing informed consent were included (5). Of these patients, urinary collections were available for 264 patients. Completeness of urinary collections was assessed using 24-hour urinary creatinine excretion; 203 patients (76.9% of patients with 24-hour urinary collections) were included for analysis (Figure 1). Demographics of the study population are presented in Table 1. Apart from a small but significant age difference (P=0.01), we observed no significant differences between the current study population and the original patient cohort. With respect to CKD stage according to the CKD-EPI equation, 4.4% of patients were classified as stage 1, 18.2% of patients were classified as stage 2, 38.4% of patients were classified as stage 3, 29.1% of patients were classified as stage 4, and 9.9% of patients were classified as stage 5. When eGFR was calculated using the MDRD equation, 17.2% of patients were classified as stages 1–2, 44.8% of patients were classified as stage 3, 27.1% of patients were classified as stage 4, and 10.8% of patients were classified as stage 5. Glomerular disease was the most prevalent underlying renal disease (36.9%) followed by unknown cause (36.0%) and vascular disease (9.4%).
Figure 1.
Patient inclusion. Flow chart showing patient screening and inclusion.
Table 1.
Patient demographics
| Variable | Current Study | Leuven Mild-to-Moderate CKD Study | P Value |
|---|---|---|---|
| Patients, n | 203 | 499 | — |
| Age, yr | 60 (48–72) | 64 (50–75) | 0.01 |
| Sex, men/women (%) | 120/83 (59/41) | 274/225 (55/45) | 0.32 |
| Weight, kg | 75.5 (15.5) | 74.9 (16.0) | 0.62 |
| Body mass index, kg/m2 | 26.1 (5.4) | 26.5 (5.2) | 0.40 |
| Serum creatinine, mg/dl | 1.81 (1.30–2.49) | 1.79 (1.28–2.47) | 0.57 |
| Estimated GFR (MDRD), ml/min per 1.73 m2 | 33.8 (23.0–54.0) | 35.7 (24.6–55.3) | 0.23 |
| Estimated GFR (CKD-EPI), ml/min per 1.73 m2 | 34.3 (23.1–55.9) | 33.9 (23.0–55.1) | 0.95 |
| Serum p-cresol, µM | — | 43.6 (17.8–91.3) | — |
| Serum p-cresyl sulfate, µM | 46.4 (20.3–91.3) | — | — |
| Serum indoxyl sulfate, µM | 9.6 (5.1–18.8) | — | — |
Main demographic, clinical, and biochemical characteristics of the study population. Data are expressed as mean (SD) or median (interquartile range) as appropriate. Differences were tested using parametric ANOVA, Kruskal–Wallis test, or chi-squared test as appropriate. MDRD, Modification of Diet in Renal Disease; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration.
Serum Concentrations and eGFR
Median serum concentrations of PCS and IS were 46.4 µM (IQR=20.3–91.9) and 9.6 µM (IQR=5.0–18.9), respectively. We analyzed their relationship with eGFR (CKD-EPI and MDRD Equations) using linear regression analysis (Table 2). When eGFR was calculated using the CKD-EPI Equation, a rather low coefficient of determination was observed for both PCS (R2=0.35, P<0.001) and IS (R2=0.25, P<0.001). The same was noticed when the MDRD-derived eGFR was used. Given the reciprocal relation between serum creatinine and the GFR, we also included 1/eGFR as an independent variable. Although the coefficient of determination remained below 0.5 for PCS (R2=0.46, P<0.001) and IS (R2=0.46, P<0.001), we observed substantial increments for all solutes studied (Table 2). Slightly lower coefficients of determinations were shown when measured creatinine clearance was used instead of eGFR (data not shown).
Table 2.
Serum concentrations and eGFR
| eGFR | 1/eGFR | |||
|---|---|---|---|---|
| R2 | P | R2 | P | |
| CKD-EPI equation | ||||
| Creatinine | 0.61 | <0.001 | 0.91 | <0.001 |
| BUN | 0.55 | <0.001 | 0.61 | <0.001 |
| p-Cresyl sulfate | 0.35 | <0.001 | 0.46 | <0.001 |
| Indoxyl sulfate | 0.25 | <0.001 | 0.46 | <0.001 |
| MDRD equation | ||||
| Creatinine | 0.63 | <0.001 | 0.92 | <0.001 |
| BUN | 0.53 | <0.001 | 0.61 | <0.001 |
| p-Cresyl sulfate | 0.35 | <0.001 | 0.46 | <0.001 |
| Indoxyl sulfate | 0.26 | <0.001 | 0.46 | <0.001 |
Linear regression analysis of the relationship between eGFR or reciprocal of eGFR and serum concentrations of creatinine, BUN, p-cresyl sulfate, and indoxyl sulfate. eGFR, estimated GFR; 1/eGFR, reciprocal of eGFR; R2, coefficient of determination; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; MDRD, Modification of Diet in Renal Disease.
Renal Clearances and eGFR
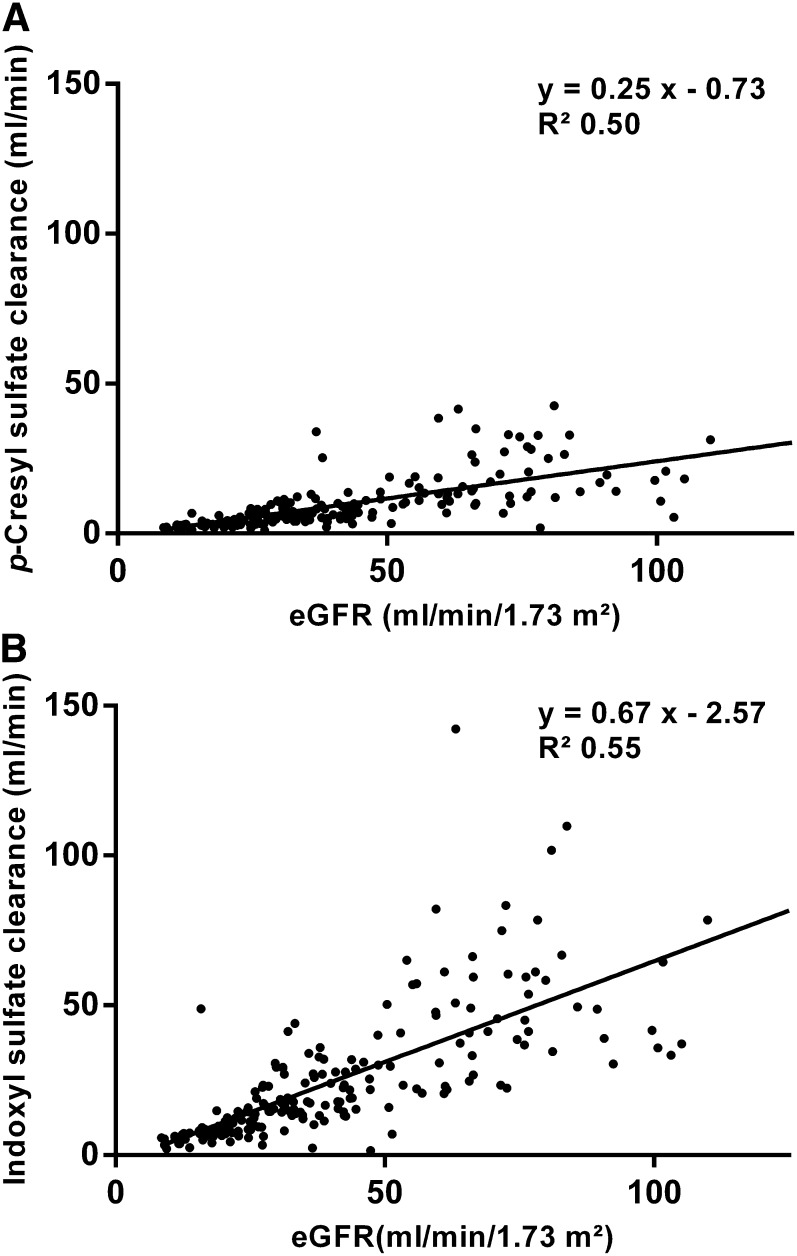
Renal clearances of PCS amounted to a median of 6.8 ml/min (IQR=3.4–12.0), whereas a median renal clearance of 17.7 ml/min was observed for IS (IQR=9.4–33.2). The relationship between eGFR and renal clearances of PCS (Figure 2A) and IS (Figure 2B) was explored using linear regression analysis. We observed a linear relationship between the eGFR (CKD-EPI Equation) and renal clearances of PCS (y=0.25x−0.73, R2=0.50, P<0.001) and IS (y=0.67x−2.57, R2=0.55, P<0.001). No major differences were noticed with the MDRD-derived eGFR (R2=0.48, P<0.001 for PCS; R2=0.55, P<0.001 for IS). Slightly higher coefficients of determination were noted when using the measured creatinine clearance instead of eGFR (R2=0.56, P<0.001 for PCS; R2=0.62, P<0.001 for IS) (Supplemental Figure 1).
Figure 2.
Estimated GFR (eGFR) and renal clearances of p-cresyl sulfate and indoxyl sulfate. Linear regression analysis of the relationship between eGFR and renal clearances of (A) p-cresyl sulfate and (B) indoxyl sulfate.
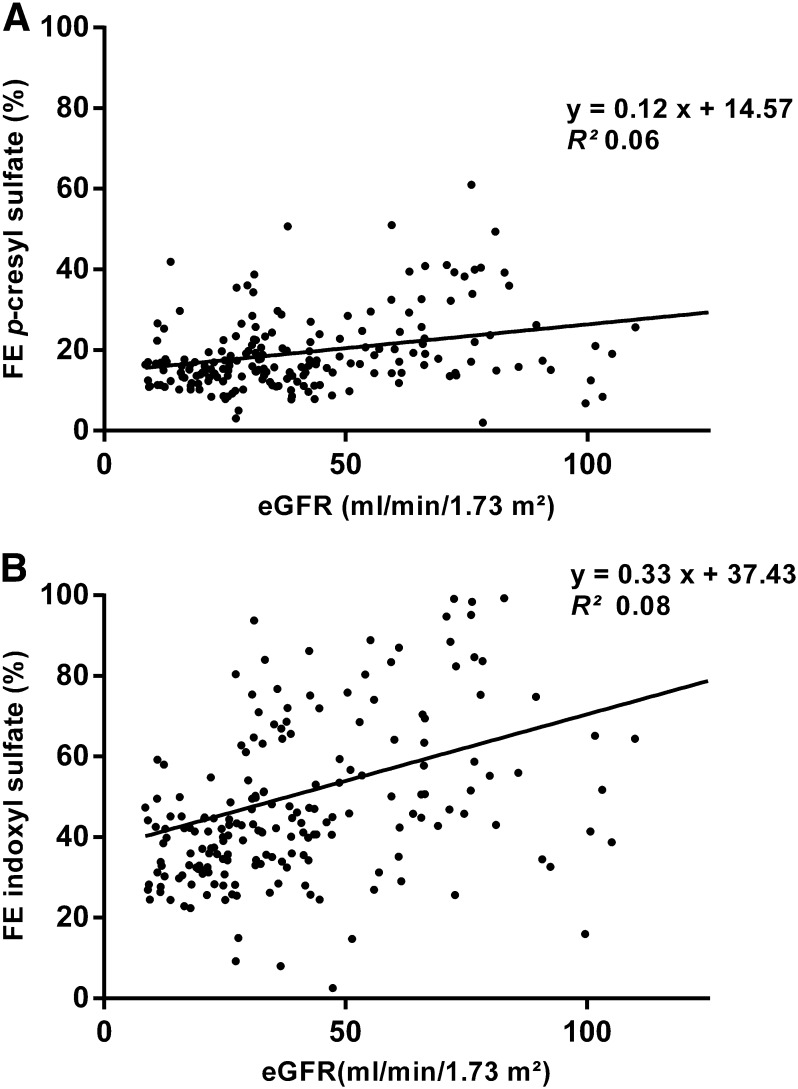
Although renal clearances of PCS and IS were clearly correlated (Spearman rank correlation coefficient=0.86, P<0.001), IS clearances exceeded PCS clearances by a median of 2.7-fold (IQR=2.2–3.2). There was no significant association between the IS clearance to PCS clearance ratio and the eGFR (Supplemental Figure 2). We then analyzed the fractional excretion of PCS (Figure 3A) and IS (Figure 3B). There was a significant but minor association between the fractional excretion of PCS (median=16.4%, IQR=13.2–22.5) and eGFR (R2=0.06, y=0.12x+14.57, P<0.001). We equally observed a significant but minor association between the fractional excretion of IS (median=43.7%, IQR=34.0%–63.2%) and the eGFR (R2=0.08, y=0.33x+37.43, P<0.001).
Figure 3.
eGFR and fractional excretion of p-cresyl sulfate and indoxyl sulfate. Linear regression analysis of the relationship between the fractional excretion (FE) of (A) p-cresyl sulfate and (B) indoxyl sulfate.
Multivariate Analysis of Serum Concentrations
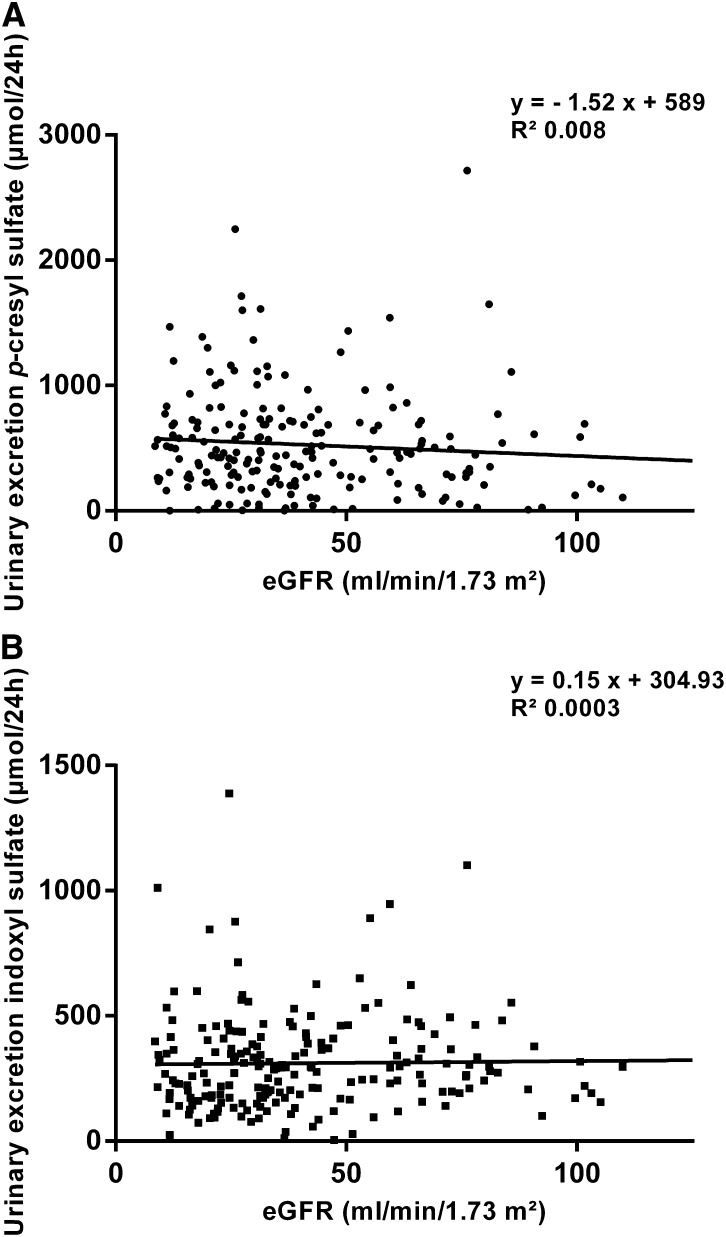
Serum concentrations of PCS were a median of 4.3-fold higher than IS (IQR=2.5–6.8). Correlation between both solutes was fairly high (Spearman rank correlation coefficient=0.75, P<0.001). To analyze factors predicting serum concentrations of both PCS and IS, we constructed multivariate models, including demographics (age, sex, length, and weight), biochemical parameters (hematocrit and albumin concentration), and 24-hour urinary excretion of PCS and IS, which under steady-state conditions, equals 24-hour intestinal absorption assuming negligible endogenous metabolism, as well as the reciprocal of eGFR as marker of kidney function (rationale described above); 24-hour urinary excretion of both PCS and IS displayed wide dispersion with higher median values of PCS (454.1 µmol, IQR=238.4–694.7) compared with IS (285.2 µmol, IQR=183.6–392.6). Although a trend was observed to higher 24-hour urinary excretion rates of PCS with higher CKD stages, there was no significant interaction between eGFR and the 24-hour urinary excretion of PCS and IS (R2=0.008, y=−1.52x+589, P=0.22 for PCS; R2=0.0003, y=0.15x+304.93, P=0.80 for IS) (Figure 4). Accounting for individual differences in protein intake, PCS but not IS 24-hour urinary excretion was significantly larger at higher CKD stages (CKD-EPI stages 1–3 versus 4–5, P=0.03 for PCS, P=0.14 for IS). Serum concentrations of PCS were associated with eGFR (P<0.001), intestinal absorption of PCS (P<0.001), and serum albumin (P<0.001; model R2=0.75, P<0.001). Serum IS concentrations were associated with eGFR (P<0.001), intestinal absorption of IS (P<0.001), age (P<0.001), and sex (P=0.05; model R2=0.74, P<0.001) (Table 3).
Figure 4.
eGFR and 24-hour urinary excretion of p-cresyl sulfate and indoxyl sulfate. Linear regression analysis of the relationship between eGFR and 24-hour urinary excretion of (A) p-cresyl sulfate and (B) indoxyl sulfate.
Table 3.
Multivariate regression analyses
| Variable | Unit | Slope (95% Confidence Interval) | P Value |
|---|---|---|---|
| Factors associated with serum p-cresyl sulfate concentrations | |||
| Serum albumin | g/dl | 21.5 (10 to 31.3) | <0.001 |
| 1/eGFR | min/ml per 1.73 m2 | 1878 (1676 to 2077) | <0.001 |
| Urinary p-cresyl sulfate excretion/24 h | µmol | 0.09 (0.07 to 0.1) | <0.001 |
| Model R2 | 0.75 | ||
| Factors associated with serum indoxyl sulfate concentrations | |||
| Sex | woman | −2.9 (−5.7 to −0.05) | 0.05 |
| Age | yr | −0.2 (−0.2 to −0.1) | <0.001 |
| 1/eGFR | min/ml per 1.73 m2 | 574 (513 to 636) | <0.001 |
| Urinary indoxyl sulfate excretion/24 h | µmol | 0.05 (0.04 to 0.05) | <0.001 |
| Model R2 | 0.74 |
1/eGFR, reciprocal of estimated GFR; R2, coefficient of determination.
Discussion
We studied the renal handling of PCS and IS in patients at various stages of CKD (excluding stage 5D). There were three key findings. (1) Renal clearances of PCS and IS are directly associated with eGFR. (2) Renal clearances of IS exceed renal clearances of PCS by nearly threefold. (3) eGFR and 24-hour urinary excretion rate (as a surrogate of 24-hour intestinal absorption rate) are both important predictors of the observed interindividual variability of serum concentrations of both PCS and IS.
Serum concentrations of the uremic retention solutes PCS and IS are associated with overall mortality (7,8), cardiovascular disease (5), and progression of CKD (3). Although advanced CKD stages are associated with higher median serum concentrations, individual serum concentrations for any given GFR are widely dispersed (5,7,8). A better understanding of the factors that predict high versus low serum concentrations is needed. A recent study by Eloot et al. (17) examining associations between eGFR and serum concentrations of various uremic retention solutes showed a low coefficient of determination for both PCS and IS. From this information, it was inferred that eGFR is not representative for evaluating the accumulation of uremic retention solutes and that eGFR is not a suitable marker for the renal handling of PCS and IS.
In our cohort, we confirmed low coefficients of determination when analyzing linear associations between eGFR and serum concentrations of PCS and IS (Table 2). Of note, a modest coefficient of determination was also observed between eGFR and serum creatinine. It should be acknowledged that the formula to calculate the GFR from urinary excretion and serum concentration implies a reciprocal relationship between the GFR and serum concentrations. Indeed, considering the reciprocal of eGFR, coefficients of determination were significantly higher for all solutes studied. We then built multivariate models to predict serum concentrations of PCS and IS. The addition of the 24-hour urinary excretion rate of either PCS or IS (as a substitute of intestinal absorption) substantially improved final models to predict serum concentrations of PCS (R2=0.75) and IS (R2=0.74), with eGFR still remaining a highly significant determinant.
We then analyzed renal clearances of PCS and IS. In line with pharmacokinetic models predicting a near-linear association between the GFR and the renal clearance of highly protein-bound solutes (15), we observed a significant direct association between eGFR and renal clearances of PCS (R2=0.50) and IS (R2=0.55). Together, these findings indicate that eGFR is an acceptable marker of the renal clearance of the protein-bound uremic retention solutes PCS and IS.
Urinary excretion of PCS and IS mainly depends on tubular secretion, because glomerular filtration of these molecules is limited because of high protein binding. Relevant transporters were recently characterized, including OAT1 (SLC22A6) and OAT3 (SLC22A8) (10–12), BCRP, and MRP4 (13). A role was also suggested for OATP4C1 (SLCO4C1) (14). The fractional excretion of both PCS and IS was significantly associated with eGFR, with lower fractional excretions being observed at more advanced CKD stages. This observation is in contrast to renal handling of other solutes (e.g., potassium and phosphorus) (24) and points to a disproportionate decline of renal clearance of both solutes compared with the GFR. It can, therefore, be hypothesized that tubular secretory mechanisms for PCS and IS become saturated at higher CKD stages, whereas the relative contribution of glomerular filtration of both solutes (unbound fraction) to total solute clearance gains importance. Although translation of experimental to clinical findings is always challenging, it can at least be estimated that basolateral uptake of IS through OAT1 (SLC22A6) becomes saturated at more advanced CKD (10). Remarkably, although renal clearances of PCS and IS were highly correlated, clearances of IS exceeded clearances of PCS by almost threefold. Theoretical modeling suggests that these findings are partly explained by higher free solute fractions of IS versus PCS (25) in addition to substantial differences between tubular transporter affinities and/or involvement of separate transporter systems for PCS and IS.
Intriguingly, 24-hour urinary excretion rates of both PCS and IS showed large interindividual variability, contributing to the observed dispersion of PCS and IS serum concentrations at different stages of CKD. Mechanisms governing these differences in intestinal absorption remain largely unknown. Both PCS and IS originate from colonic bacterial proteolytic fermentation (1,26). It is suggested that CKD goes along with a different gut microbiome (27) and favors a proteolytic fermentation pattern (28). It has already been shown that higher CKD stages are associated with increased p-cresol intestinal absorption rates (28). In our cohort, when accounting for individual differences in protein intake, intestinal absorption rate of PCS but not IS was also significantly increased at more advanced CKD stages. Our data, thus, provide additional arguments that the gut microbiome shows high interindividual variability and is modified by renal disease, and therefore, it might be a valuable target for intervention in patients with CKD.
There are limitations to our study. First, this study is a cross-sectional study in patients at various stages of CKD. This design precludes studying the effects of CKD progression on renal excretion of PCS and IS. Second, our study population mainly consists of patients of Caucasian origin. Care must be taken when extrapolating our data to other patient populations. Third, assessment of completeness of urinary collections is arbitrary. We assumed completeness of urinary collections when urinary excretion of creatinine was within 2 SDs of the mean creatinine excretion for the geographical region of this study (INTERSALT study) (21). Finally, we only modeled renal handling of total solute concentrations of PCS and IS. Because unbound solute fractions were not determined in our study, formal statements about renal clearances and serum concentrations of both free PCS and free IS cannot be made.
In conclusion, this study is the first to show clear associations between eGFR and renal clearances of PCS and IS, making eGFR an acceptable marker for the renal handling of both protein-bound solutes. Renal clearances of IS exceed renal clearances of PCS by approximately threefold, contributing to the observed lower serum concentrations of IS at different stages of CKD.
Disclosures
None.
Supplementary Material
Acknowledgments
Technical assistance by H. De Loor, M. Dekens, T. Coopmans, and G. Lemmens is greatly appreciated.
R.P. is the recipient of a fellowship of the Research Foundation—Flanders (Grant 11E9813N).
Part of this work was presented at the American Society of Nephrology Kidney Week from October 30 to November 4, 2012, in San Diego, CA.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.00300113/-/DCSupplemental.
References
- 1.Aronov PA, Luo FJ, Plummer NS, Quan Z, Holmes S, Hostetter TH, Meyer TW: Colonic contribution to uremic solutes. J Am Soc Nephrol 22: 1769–1776, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Niwa T, Nomura T, Sugiyama S, Miyazaki T, Tsukushi S, Tsutsui S: The protein metabolite hypothesis, a model for the progression of renal failure: An oral adsorbent lowers indoxyl sulfate levels in undialyzed uremic patients. Kidney Int Suppl 62: S23–S28, 1997 [PubMed] [Google Scholar]
- 3.Wu IW, Hsu KH, Lee CC, Sun CY, Hsu HJ, Tsai CJ, Tzen CY, Wang YC, Lin CY, Wu MS: p-Cresyl sulphate and indoxyl sulphate predict progression of chronic kidney disease. Nephrol Dial Transplant 26: 938–947, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bammens B, Evenepoel P, Keuleers H, Verbeke K, Vanrenterghem Y: Free serum concentrations of the protein-bound retention solute p-cresol predict mortality in hemodialysis patients. Kidney Int 69: 1081–1087, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Meijers BK, Claes K, Bammens B, de Loor H, Viaene L, Verbeke K, Kuypers D, Vanrenterghem Y, Evenepoel P: p-Cresol and cardiovascular risk in mild-to-moderate kidney disease. Clin J Am Soc Nephrol 5: 1182–1189, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meijers BK, Bammens B, De Moor B, Verbeke K, Vanrenterghem Y, Evenepoel P: Free p-cresol is associated with cardiovascular disease in hemodialysis patients. Kidney Int 73: 1174–1180, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Barreto FC, Barreto DV, Liabeuf S, Meert N, Glorieux G, Temmar M, Choukroun G, Vanholder R, Massy ZA, European Uremic Toxin Work Group (EUTox) : Serum indoxyl sulfate is associated with vascular disease and mortality in chronic kidney disease patients. Clin J Am Soc Nephrol 4: 1551–1558, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liabeuf S, Barreto DV, Barreto FC, Meert N, Glorieux G, Schepers E, Temmar M, Choukroun G, Vanholder R, Massy ZA, European Uraemic Toxin Work Group (EUTox) : Free p-cresylsulphate is a predictor of mortality in patients at different stages of chronic kidney disease. Nephrol Dial Transplant 25: 1183–1191, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Meijers BK, Bammens B, Verbeke K, Evenepoel P: A review of albumin binding in CKD. Am J Kidney Dis 51: 839–850, 2008 [DOI] [PubMed] [Google Scholar]
- 10.Deguchi T, Kusuhara H, Takadate A, Endou H, Otagiri M, Sugiyama Y: Characterization of uremic toxin transport by organic anion transporters in the kidney. Kidney Int 65: 162–174, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Deguchi T, Kouno Y, Terasaki T, Takadate A, Otagiri M: Differential contributions of rOat1 (Slc22a6) and rOat3 (Slc22a8) to the in vivo renal uptake of uremic toxins in rats. Pharm Res 22: 619–627, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Miyamoto Y, Watanabe H, Noguchi T, Kotani S, Nakajima M, Kadowaki D, Otagiri M, Maruyama T: Organic anion transporters play an important role in the uptake of p-cresyl sulfate, a uremic toxin, in the kidney. Nephrol Dial Transplant 26: 2498–2502, 2011 [DOI] [PubMed] [Google Scholar]
- 13.Mutsaers HA, van den Heuvel LP, Ringens LH, Dankers AC, Russel FG, Wetzels JF, Hoenderop JG, Masereeuw R: Uremic toxins inhibit transport by breast cancer resistance protein and multidrug resistance protein 4 at clinically relevant concentrations. PLoS One 6: e18438, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mutsaers HA, Wilmer MJ, van den Heuvel LP, Hoenderop JG, Masereeuw R: Basolateral transport of the uraemic toxin p-cresyl sulfate: Role for organic anion transporters? Nephrol Dial Transplant 26: 4149, 2011 [DOI] [PubMed] [Google Scholar]
- 15.Janků I: Physiological modelling of renal drug clearance. Eur J Clin Pharmacol 44: 513–519, 1993 [DOI] [PubMed] [Google Scholar]
- 16.Janků I, Zvára K: Quantitative analysis of drug handling by the kidney using a physiological model of renal drug clearance. Eur J Clin Pharmacol 44: 521–524, 1993 [DOI] [PubMed] [Google Scholar]
- 17.Eloot S, Schepers E, Barreto DV, Barreto FC, Liabeuf S, Van Biesen W, Verbeke F, Glorieux G, Choukroun G, Massy Z, Vanholder R: Estimated glomerular filtration rate is a poor predictor of concentration for a broad range of uremic toxins. Clin J Am Soc Nephrol 6: 1266–1273, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) : A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F, Chronic Kidney Disease Epidemiology Collaboration : Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 145: 247–254, 2006 [DOI] [PubMed] [Google Scholar]
- 20.de Loor H, Meijers BK, Meyer TW, Bammens B, Verbeke K, Dehaen W, Evenepoel P: Sodium octanoate to reverse indoxyl sulfate and p-cresyl sulfate albumin binding in uremic and normal serum during sample preparation followed by fluorescence liquid chromatography. J Chromatogr A 1216: 4684–4688, 2009 [DOI] [PubMed] [Google Scholar]
- 21.Intersalt Cooperative Research Group : Intersalt: An international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 297: 319–328, 1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maroni BJ, Steinman TI, Mitch WE: A method for estimating nitrogen intake of patients with chronic renal failure. Kidney Int 27: 58–65, 1985 [DOI] [PubMed] [Google Scholar]
- 23.Masud T, Manatunga A, Cotsonis G, Mitch WE: The precision of estimating protein intake of patients with chronic renal failure. Kidney Int 62: 1750–1756, 2002 [DOI] [PubMed] [Google Scholar]
- 24.Hayslett JP: Functional adaptation to reduction in renal mass. Physiol Rev 59: 137–164, 1979 [DOI] [PubMed] [Google Scholar]
- 25.Meijers BK, De Loor H, Bammens B, Verbeke K, Vanrenterghem Y, Evenepoel P: p-Cresyl sulfate and indoxyl sulfate in hemodialysis patients. Clin J Am Soc Nephrol 4: 1932–1938, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meyer TW, Hostetter TH: Uremic solutes from colon microbes. Kidney Int 81: 949–954, 2012 [DOI] [PubMed] [Google Scholar]
- 27.Vaziri ND, Wong J, Pahl M, Piceno YM, Yuan J, Desantis TZ, Ni Z, Nguyen TH, Andersen GL: Chronic kidney disease alters intestinal microbial flora. Kidney Int 83: 308–315, 2013 [DOI] [PubMed] [Google Scholar]
- 28.Bammens B, Verbeke K, Vanrenterghem Y, Evenepoel P: Evidence for impaired assimilation of protein in chronic renal failure. Kidney Int 64: 2196–2203, 2003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.