Summary
Background and objectives
The burden of AKI around the globe has not been systematically examined.
Design, setting, participants, & measurements
A systematic review (2004–2012) of large cohort studies was conducted to estimate the world incidence of AKI and its stages of severity and associated mortality, and to describe geographic variations according to countries, regions, and their economies. AKI definitions were reclassified according to the Kidney Disease Improving Global Outcomes (KDIGO) staging system. Random-effects model meta-analyses and meta-regressions were used to generate summary estimates and explore sources of heterogeneity.
Results
There were 312 studies identified (n=49,147,878) , primarily in hospital settings. Most studies originated from North America, Northern Europe, and Eastern Asia, from high-income countries, and from nations that spent ≥5% of the gross domestic product on total health expenditure. Among the 154 studies (n=3,585,911) that adopted a KDIGO-equivalent AKI definition, the pooled incidence rates of AKI were 21.6% in adults (95% confidence interval [95% CI], 19.3 to 24.1) and 33.7% in children (95% CI, 26.9 to 41.3). The pooled AKI-associated mortality rates were 23.9% in adults (95% CI, 22.1 to 25.7) and 13.8% in children (95% CI, 8.8 to 21.0). The AKI-associated mortality rate declined over time, and was inversely related to income of countries and percentage of gross domestic product spent on total health expenditure.
Conclusions
Using the KDIGO definition, 1 in 5 adults and 1 in 3 children worldwide experience AKI during a hospital episode of care. This analysis provides a platform to raise awareness of AKI with the public, government officials, and health care professionals.
Introduction
World Kidney Day is a joint initiative of the International Society of Nephrology and the International Federation of Kidney Foundations aimed at raising awareness of the importance of the kidneys to human health, and reducing the frequency and burden of kidney disease worldwide (1,2). Launched in 2006, World Kidney Day broadcasts a message about kidney disease to the public, government health officials, and health care providers (3). Over the last 7 years, this effort has focused on themes such as early detection of kidney disease, kidney protection measures including BP and diabetes control, and kidney organ donation. World Kidney Day 2013 focuses on AKI to raise awareness of this clinical problem, and stimulate global discussion, education, and policy development in order to improve prevention and treatment of AKI.
For many years, varying definitions of AKI have appeared in the literature, making comparisons between studies difficult. Over the last decade, however, the RIFLE (4) and the Acute Kidney Injury Network (AKIN) (5) classification and staging systems have advanced the field, allowing improved comparisons between study populations. AKI is linked to adverse outcomes and heightened resource utilization (6–9).
To date, the incidence rate of AKI around the globe has not been systematically examined. The publication of studies using the RIFLE or AKIN classification and staging systems over the past decade provides an opportunity to generate more congruent estimates on the incidence of AKI and its associated outcomes. This meta-analysis was conducted to estimate the world incidence of AKI, and to describe geographic variations according to countries, regions, and their economies. This effort hopes to raise awareness of AKI across the globe, and to provide a resource for future development of public health policies and planning of clinical trials for AKI.
Materials and Methods
Data Sources and Searches
We performed a literature search in MEDLINE (from 2004 to August 23, 2012) to identify eligible studies using the Medical Subject Headings search terms acute renal failure, acute kidney failure, acute renal insufficiency, acute kidney insufficiency, acute tubular necrosis, acute kidney injury, or acute renal injury (Supplemental Table 1). The year 2004 was selected because it corresponded to the year in which the RIFLE criteria were first published. The search was limited to human studies without language restrictions. We also searched EMBASE using similar search terms, and manually reviewed the bibliography of retrieved articles for additional relevant studies. We followed the PRISMA flow diagram for reporting of meta-analyses (10).
Study Selection
We included retrospective and prospective cohort studies (including post hoc analyses derived from clinical trials) of adults and children that reported on the incidence of AKI and its associated outcomes, including dialysis requirement, recovery of kidney function, and short-term (in-hospital)/long-term mortality. If more than one publication appeared on the same study, data from the most inclusive report were used. To improve generalizability, we only included studies of adults (age ≥18 years) and children with a minimum sample size of 500 and 50 patients, respectively. Pairs of authors initially screened the titles and abstracts of all of the electronic citations, and then retrieved and rescreened full-text articles.
Data Extraction
Due to the unanticipated large number of included articles, the data were extracted by pairs of authors. Disagreements were resolved through consensus and arbitration by a third author. Data extraction included country of origin, year of publication, study design, sample size, patient characteristics (age and sex), and clinical setting (e.g., cardiac surgery, nephrotoxins including radiocontrast exposure, critical care, trauma, heart failure, hematology/oncology, community-acquired AKI, and hospital-acquired AKI [unspecified]). We also recorded the definition of AKI and the number of patients who developed AKI, initiated dialysis, recovered kidney function, and died. Timeline for death was arbitrarily classified as <3 (inclusive of in-hospital death), 3–6, and >6 months. Although our original intent was to examine recovery of kidney function, inconsistent reporting in the studies precluded further quantitative analysis of this endpoint.
Countries were grouped within continents and world zones in accordance with the geo-scheme devised by the United Nations Statistics Division (11). Countries’ economies were assessed according to four ranges of gross national income per capita derived from the World Bank’s classification of income of economies (12,13): low (≤US$1005), lower middle (US$1006–$3975), upper middle (US$3976–$12,275), and high (≥US$12,276) income countries. Using the World Health Organization’s world health statistics, countries were also classified according to national total expenditure on health (representing the sum of general government and private health expenditures in a given year, calculated in national currency units in current prices) as a percentage of gross domestic product (GDP) (representing the value of all final goods and services produced within a nation in a given year) (14). In terms of latitude, studies were classified as originating from countries located north or south of the equator.
Harmonization of AKI Definitions
We harmonized the AKI definitions adopted in the individual studies first by classifying them according to the RIFLE (4) or AKIN (5) criteria, other biochemical/urine output/dialysis requirement-based definitions, and administrative codes for AKI derived from the International Classification of Diseases, Ninth or Tenth Revision, Clinical Modification methodology. We then reclassified studies that adopted the RIFLE (including the pediatric RIFLE) or AKIN serum creatinine-based criteria to define AKI and its stages of severity as equivalent to the latest AKI definition and staging system proposed by the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines for AKI (15) (Supplemental Table 2). These studies were grouped as having utilized a KDIGO-equivalent AKI definition. The remaining studies that defined AKI according to other criteria were analyzed separately.
Study Quality Assessment
The quality of the cohort studies was assessed independently by pairs of two authors, using the Newcastle-Ottawa scale (16), which allocates a maximum of 9 points for quality of the selection, comparability, and outcome of study populations. Study quality scores were defined arbitrarily as poor (0–3), fair (4–6), or good (7–9).
Data Synthesis and Statistical Analyses
Inter-rater agreement for the final selection of the articles and quality assessment was evaluated by calculating the weighted Cohen’s κ coefficient using the “psych” package in the R system software (version 2.14.0) (17). Random-effects model meta-analyses were conducted to generate pooled incidence rates of AKI, stages of severity, and associated mortality. Random-effects model meta-analyses were also performed to compute pooled odds ratios (ORs) for mortality in patients with AKI relative to those without AKI. For the few studies that had no mortality events in either group, we added 0.5 to the number of events and nonevents, before computing the ORs. All pooled estimates are provided with 95% confidence intervals (95% CIs). Heterogeneity was assessed using the I2 index and the Q test P value. The I2 index describes the percentage of total variation across studies due to true heterogeneity rather than chance, with a value of ≥75% indicating medium-to-high heterogeneity (18). To examine global patterns of AKI, we conducted random-effects subgroup and meta-regression analyses of AKI rates and associated mortality by geographic world regions, and patterns of country economies and latitude. We performed the meta-analyses using Comprehensive Meta-Analysis (version 2.0; Biostat, www.meta-analysis.com) and the meta-regression analyses using the “metafor” package (19) in the R system software (version 2.14.0) (17).
Results
Study Characteristics and Quality Assessment
A total of 2496 potentially relevant citations were identified and screened; 414 articles were retrieved for detailed evaluation, 312 of which fulfilled eligibility criteria (Supplemental References), representing close to 50 million patients from >40 countries worldwide (Figure 1). The inter-rater agreement weighted κ coefficient for the final selection of the articles was 0.82 (95% CI, 0.76 to 0.89). Characteristics of all 312 studies are displayed in Supplemental Tables 3 and 4, and of the 154 subset of studies that used a KDIGO-equivalent AKI definition in Table 1. In brief, there were 194 retrospective cohort studies, 109 prospective cohort studies, and 9 post hoc cohorts derived from clinical trials. All studies were published in English and publication spanned 8 years. There were 269 studies of adults, 42 studies of children, and 1 study combining adults and children. Studies of adults varied from 500 to 12,500,459 patients, and studies of children from 64 to 60,160 patients. The mean age ranged from 23 to 80 years for adults and from 0 to 13 years for children.
Figure 1.
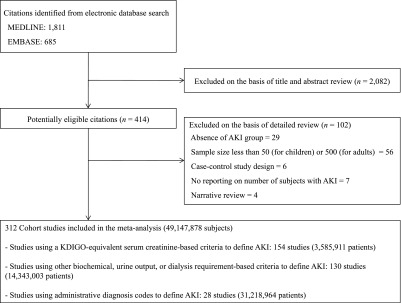
Literature search and selection. KDIGO, Kidney Disease Improving Global Outcomes.
Table 1.
Characteristics of the 154 studies that used a KDIGO-equivalent AKI definition
| All Studies | Studies of Adults | Studies of Children | |
|---|---|---|---|
| No. of studies | 154 | 130 | 24 |
| Sample size | 22,220 (95–1,126,636) | 26,240 (509–1,126,636) | 593 (95–3396) |
| Percentage of male participants | 63 (28–100) | 65 (28–100) | 56 (49–79) |
| Age of participants (yr) | 51.6 (0.0–80.3)a | 60.6 (25.5–80.3) | 4.7 (0.0–11.4)a |
| Studies by clinical setting | |||
| Community acquired | 7 (5) | 6 (5) | 1 (4) |
| Critical care | 41 (27) | 32 (25) | 9 (38) |
| Cardiac surgery | 42 (27) | 35 (27) | 7 (29) |
| Trauma | 4 (2) | 4 (3) | 0 (0) |
| Heart failure | 1 (1) | 1 (1) | 0 (0) |
| Hematology/oncology | 3 (2) | 3 (2) | 0 (0) |
| Nephrotoxins | 4 (2) | 2 (1) | 2 (8) |
| Hospital acquired, unspecified | 52 (34) | 47 (36) | 5 (21) |
| Studies by continent | |||
| Australia and New Zealand | 9 (6) | 9 (7) | 0 (0) |
| Asia | 21 (14) | 18 (14) | 3 (13) |
| Europe | 51 (33) | 45 (35) | 6 (25) |
| America | 70 (45) | 55 (42) | 15 (62) |
| Africa | 0 (0) | 0 (0) | 0 (0) |
| Multiple continents | 3 (2) | 3 (2) | 0 (0) |
| Studies by world zoneb | |||
| Australia and New Zealand | 9 (6) | 9 (7) | 0 (0) |
| Eastern Asia | 17 (11) | 15 (12) | 2 (8) |
| Western Asia | 2 (1) | 1 (1) | 1 (4) |
| Southern Asia | 2 (1) | 2 (2) | 0 (0) |
| South East Asia | 0 (0) | 0 (0) | 0 (0) |
| Eastern Europe | 2 (1) | 1 (1) | 1 (4) |
| Western Europe | 15 (10) | 13 (10) | 2 (8) |
| Northern Europe | 12 (8) | 10 (8) | 2 (8) |
| Southern Europe | 18 (11) | 17 (13) | 1 (4) |
| Multi-zone Europe | 4 (3) | 4 (3) | 0 (0) |
| North America | 64 (42) | 50 (38) | 14 (60) |
| South America | 6 (4) | 5 (3) | 1 (4) |
| North Africa | 0 (0) | 0 (0) | 0 (0) |
| Western Africa | 0 (0) | 0 (0) | 0 (0) |
| Multiple zones | 3 (2) | 3 (2) | 0 (0) |
| Studies by latitude | |||
| North | 138 (89) | 115 (88) | 23 (96) |
| South | 15 (10) | 14 (11) | 1 (4) |
| North and South | 1 (1) | 1 (1) | 0 (0) |
| Country income classificationc | |||
| Low income | 1 (1) | 1 (1) | 0 (0) |
| Lower middle income | 1 (1) | 1 (1) | 0 (0) |
| Upper middle income | 20 (13) | 16 (12) | 4 (17) |
| High income | 130 (84) | 110 (85) | 20 (83) |
| Not available | 2 (1) | 2 (1) | 0 (0) |
| Country total health expenditure (% of GDP)d | |||
| <5 | 8 (5) | 7 (5) | 1 (4) |
| 5–10 | 68 (45) | 58 (45) | 10 (42) |
| >10 | 76 (49) | 63 (48) | 13 (54) |
| Not available | 2 (1) | 2 (2) | 0 (0) |
Data are presented as the mean (range) or n (%). KDIGO, Kidney Disease Improving Global Outcomes; GDP, gross domestic product.
A zero value indicates newborns.
According to the United Nations geo-scheme classification (11).
According to the World Bank's classification of income of countries (12).
According to the World Health Organization (14).
Most studies (49.0%) originated from America (142 studies from North America and 11 studies from South America), followed by Europe (98 studies), Asia (44 studies), Australia and New Zealand (10 studies), and Africa (2 studies). The top-three world zones where studies were conducted were North America (142 studies), Northern Europe (27 studies), and Eastern Asia (26 studies).
Most studies (82.7%) originated from high-income countries (258 studies) followed by upper middle income countries (40 studies). Most studies also originated from countries that spent ≥5% of GDP on total health expenditure (286 studies).
There were 288 studies (92.3%) that originated from countries located north of the equator. There were 194 studies (62.2%) considered of good quality, 116 studies (37.3%) of fair quality, and 2 studies (0.6%) of poor quality. The weighted κ coefficient for quality assessment was 0.03 (95% CI, 0.00 to 0.14), suggesting poor inter-rater agreement.
Data Synthesis
Pooled Rate of AKI.
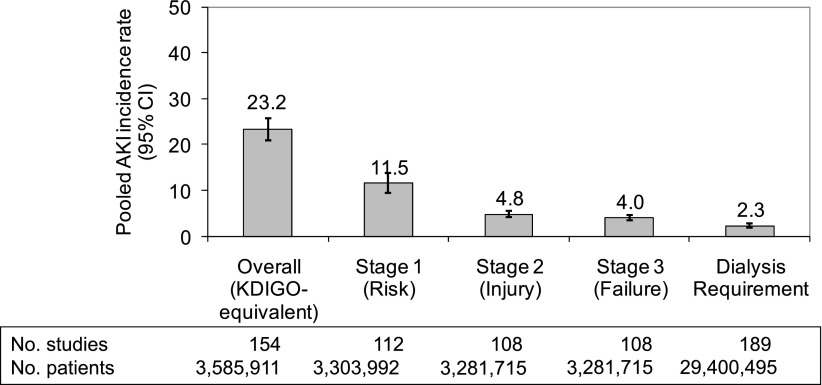
Using all 312 studies, the pooled rate of AKI was 10.7% (95% CI, 9.6 to 11.9). When restricted to the 154 studies (130 studies of adults and 24 studies of children) that used a KDIGO-equivalent AKI definition, the pooled rate of AKI was 23.2% (95% CI, 21.0 to 25.7) (Figure 2). Lower pooled AKI rates were observed in studies using other clinical criteria to define AKI (5.0%; 130 studies; 95% CI, 3.4 to 7.1) and administrative codes (2.9%; 28 studies; 95% CI, 2.3 to 3.7).
Figure 2.
Pooled incidence rate of AKI in studies that used KDIGO-equivalent serum creatinine-based AKI definition and staging system, or dialysis requirement. Some studies and patients are included in more than one category. KDIGO, Kidney Disease Improving Global Outcomes; 95% CI, 95% confidence interval.
Pooled Rate of AKI According to KDIGO Criteria, and Variability around the World.
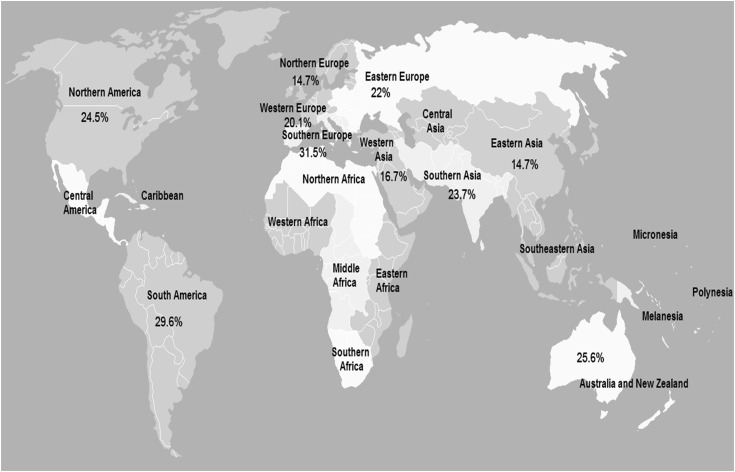
We restricted the remainder of our analyses to studies classified according to the KDIGO-equivalent AKI definition and dialysis requirement, to obtain more meaningful estimates of the disease across a wide spectrum of patient- and country-level characteristics (Table 2). In brief, the pooled rates of AKI in studies of adults and children were 21.6% (95% CI, 19.3 to 24.1) and 33.7% (95% CI, 26.9 to 41.3), respectively. Pooled rates were 11.5%, 4.8%, and 4.0% for stage 1, stage 2, and stage 3 AKI, respectively (Figure 2). The pooled rate of dialysis requirement was 2.3%. The highest pooled AKI rate was observed in critical care settings (31.7%; 95% CI, 28.6 to 35.0), followed by cardiac surgery (24.3%; 95% CI, 20.4 to 28.8). When examined according to geographic regions of the world (Figure 3) and patterns of country economies and latitude, the pooled rate of AKI appeared higher in South versus North America (29.6% versus 24.5%), Southern versus Northern Europe (31.5% versus 14.7%), and South versus Western or Eastern Asia (23.7% versus 16.7% versus 14.7%). The pooled rate was also higher in Australia and New Zealand (25.6%; 95% CI, 22.3 to 29.3).
Table 2.
Pooled incidence rate of AKI according to the KDIGO-equivalent definition
| Subgroup | Studies (n) | Patients (n) | Patients with AKI (n) | AKI Incidence Rate (%) | 95% Confidence Interval | Test for Heterogeneity | |
|---|---|---|---|---|---|---|---|
| I2 Index | Q Test P Value | ||||||
| All | 154 | 3,585,911 | 573,424 | 23.2 | 21.0 to 25.7 | 99.9 | <0.001 |
| Age category | |||||||
| Adults | 130 | 3,571,691 | 569,861 | 21.6 | 19.3 to 24.1 | 99.9 | <0.001 |
| Children | 24 | 14,220 | 3563 | 33.7 | 26.9 to 41.3 | 98.3 | <0.001 |
| Clinical setting | |||||||
| Community acquired | 7 | 548,398 | 4897 | 8.3 | 1.6 to 33.0 | 99.9 | <0.001 |
| Critical care | 41 | 888,604 | 272,580 | 31.7 | 28.6 to 35.0 | 99.9 | <0.001 |
| Cardiac surgery | 42 | 164,333 | 33,157 | 24.3 | 20.4 to 28.8 | 99.7 | <0.001 |
| Trauma | 4 | 14,947 | 2557 | 19.9 | 13.6 to 28.2 | 98.7 | <0.001 |
| Heart failure | 1 | 682 | 221 | 32.4 | 29.0 to 36.0 | — | — |
| Hematology/oncology | 3 | 2401 | 453 | 21.3 | 7.5 to 47.6 | 99.2 | <0.001 |
| Nephrotoxins | 4 | 17,786 | 1681 | 12.2 | 6.2 to 22.7 | 98.7 | <0.001 |
| Hospital acquired, unspecified | 52 | 1,948,760 | 257,878 | 20.9 | 17.2 to 25.2 | 99.9 | <0.001 |
| Continent | |||||||
| Australia and New Zealand | 9 | 523,715 | 182,405 | 25.6 | 22.3 to 29.3 | 99.9 | <0.001 |
| Asia | 21 | 286,377 | 17,358 | 15.6 | 8.7 to 26.4 | 99.9 | <0.001 |
| Europe | 51 | 918,068 | 72,390 | 23.1 | 18.0 to 29.2 | 99.9 | <0.001 |
| America | 70 | 1,847,689 | 296,655 | 24.9 | 22.1 to 27.8 | 99.9 | <0.001 |
| Multiple continents | 3 | 10,062 | 4616 | 49.4 | 22.9 to 76.3 | 99.9 | <0.001 |
| World zonea | |||||||
| Australia and New Zealand | 9 | 523,715 | 182,405 | 25.6 | 22.3 to 29.3 | 99.9 | <0.001 |
| Eastern Asia | 17 | 258,161 | 14,794 | 14.7 | 7.0 to 28.2 | 99.9 | <0.001 |
| Western Asia | 2 | 25,989 | 2006 | 16.7 | 3.3 to 54.3 | 99.3 | <0.001 |
| South Asia | 2 | 2227 | 558 | 23.7 | 7.5 to 54.4 | 99.4 | <0.001 |
| Eastern Europe | 2 | 2600 | 639 | 22.0 | 9.5 to 43.3 | 98.9 | <0.001 |
| Western Europe | 15 | 161,198 | 14,725 | 20.1 | 12.1 to 31.5 | 99.9 | <0.001 |
| Northern Europe | 12 | 607,956 | 8894 | 14.7 | 5.5 to 33.6 | 99.9 | <0.001 |
| Southern Europe | 18 | 24,080 | 6546 | 31.5 | 23.1 to 41.3 | 99.5 | <0.001 |
| Multi-zone Europe | 4 | 122,234 | 41586 | 32.5 | 28.3 to 37.0 | 99.6 | <0.001 |
| North America | 64 | 1,843,814 | 295,554 | 24.5 | 21.7 to 27.5 | 99.9 | <0.001 |
| South America | 6 | 3875 | 1101 | 29.6 | 19.1 to 42.7 | 98.3 | <0.001 |
| Multiple zones | 3 | 10,062 | 4616 | 49.4 | 22.9 to 76.3 | 99.9 | <0.001 |
| Latitude | |||||||
| North | 138 | 3,057,543 | 389,454 | 22.6 | 20.2 to 25.2 | 99.9 | <0.001 |
| South | 15 | 527,590 | 183,506 | 27.0 | 24.2 to 30.0 | 99.8 | <0.001 |
| North and South | 1 | 778 | 464 | 59.6 | 56.2 to 63.0 | — | — |
| Country income classificationb | |||||||
| Low income | 1 | 1047 | 399 | 38.1 | 35.2 to 41.1 | — | — |
| Lower middle income | 1 | 1180 | 159 | 13.5 | 11.6 to 15.5 | — | — |
| Upper middle income | 20 | 248,718 | 14,335 | 19.5 | 10.4 to 33.7 | 99.9 | <0.001 |
| High income | 130 | 3,313,430 | 553,203 | 23.8 | 21.4 to 26.4 | 99.9 | <0.001 |
| Not available | 2 | 21,536 | 5328 | 25.1 | 23.6 to 26.7 | 80.4 | 0.02 |
| Country total health expenditure (% of GDP)c | |||||||
| <5 | 8 | 222,178 | 7823 | 14.5 | 7.2 to 26.9 | 99.8 | <0.001 |
| 5–10 | 68 | 1,406,796 | 258,636 | 22.3 | 19.6 to 25.3 | 99.9 | <0.001 |
| >10 | 76 | 1,935,401 | 301,637 | 25.2 | 22.3 to 28.3 | 99.9 | <0.001 |
| Not available | 2 | 21,536 | 5328 | 25.1 | 23.6 to 26.7 | 80.4 | <0.001 |
Figure 3.
Pooled incidence rate of AKI by world zones in studies that used a KDIGO-equivalent serum creatinine-based AKI definition. Some studies and patients are included in more than one category. KDIGO, Kidney Disease Improving Global Outcomes.
The pooled rate of AKI appeared higher in studies from countries located south versus north of the equator (27.0% versus 22.6%), and from countries that spent >10% versus ≤5% GDP on total health expenditure (25.2% versus 14.5%), with a significant trend observed by meta-regression (P=0.03; Table 4). The rate of AKI declined over the span of 8 years (P<0.001; Table 4).
Table 4.
Meta-regression analyses examining the association of AKI incidence rate according to the KDIGO-equivalent definition and its associated mortality rate with aggregate study- and country-level characteristics
| Characteristic | Rate Change (%) | 95% Confidence Interval | P Value |
|---|---|---|---|
| AKI incidence rate | |||
| Country percentage GDP spent on total health expenditure (per 1% ↑) | 0.54 | 0.07 to 1.02 | 0.03 |
| Country gross national income per capita (per $10,000 ↑) | 0.18 | −0.90 to 1.27 | 0.74 |
| Year of study publication (per year ↑) | −2.02 | −2.83 to −1.22 | <0.001 |
| AKI-associated mortality rate | |||
| Country percentage GDP spent on total health expenditure (per 1% ↑) | −1.36 | −1.97 to −0.75 | <0.001 |
| Country gross national income per capita (per $10,000 ↑) | −3.43 | −4.63 to −2.23 | <0.001 |
| Year of study publication (per year ↑) | −1.46 | −2.69 to −0.24 | 0.02 |
GDP, gross domestic product.
AKI-Associated Mortality Rate.
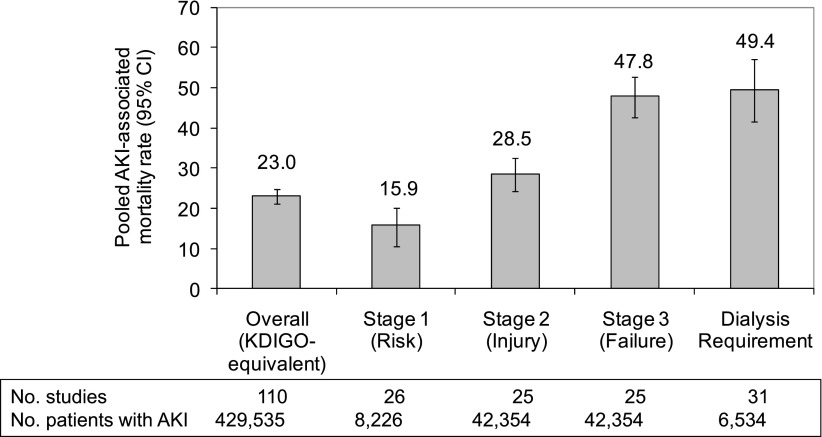
As shown in Table 3, among 110 studies (99 studies of adults and 11 studies of children) that used a KDIGO-equivalent AKI definition and assessed mortality, the pooled AKI-associated all-cause mortality rate was 23.0% (95% CI, 21.3 to 24.8) and increased with higher stages of severity (Figure 4). The pooled mortality rates were 23.9% in adults (95% CI, 22.1 to 25.7) and 13.8% in children (95% CI, 8.8 to 21.0). Meta-regression showed that the AKI-associated mortality rate declined over the span of 8 years (P=0.02), and was inversely related to the percentage of country GDP spent on total health expenditure (P<0.001) and country gross national income per capita (P<0.001) (Table 4). At <3, 3–6, and >6 months of follow-up, the pooled AKI-associated mortality rates were 22.1%, 31.5%, and 27.7%, respectively.
Table 3.
Pooled AKI-associated mortality rate in studies that adopted a KDIGO-equivalent AKI definition
| Subgroup | Studies (n) | Patients with AKI (n) | Deaths (n) | Pooled Mortality Rate | 95% Confidence Interval | Test for Heterogeneity | |
|---|---|---|---|---|---|---|---|
| I2 Index | Q Test P Value | ||||||
| All | 110 | 429,535 | 107,433 | 23.0 | 21.3 to 24.8 | 99.3 | <0.001 |
| Age category | |||||||
| Adults | 99 | 427,804 | 107,167 | 23.9 | 22.1 to 25.7 | 99.4 | <0.001 |
| Children | 11 | 1731 | 266 | 13.8 | 8.8 to 21.0 | 91.3 | <0.001 |
| Clinical setting | |||||||
| Community acquired | 5 | 4349 | 2015 | 32.8 | 20.8 to 47.5 | 98.1 | <0.001 |
| Critical care | 31 | 198,645 | 53,783 | 33.1 | 29.8 to 36.6 | 99.5 | <0.001 |
| Cardiac surgery | 23 | 21,811 | 1871 | 8.3 | 6.6 to 10.4 | 95.3 | <0.001 |
| Trauma | 3 | 2387 | 593 | 32.2 | 13.0 to 60.1 | 99.1 | <0.001 |
| Heart failure | 1 | 221 | 47 | 21.3 | 16.4 to 27.2 | — | — |
| Hematology/oncology | 2 | 278 | 76 | 25.7 | 16.1 to 38.3 | 73.9 | <0.001 |
| Nephrotoxins | 1 | 81 | 12 | 14.8 | 8.6 to 24.3 | — | — |
| Hospital acquired, unspecified | 44 | 201,763 | 49,036 | 25.7 | 22.5 to 29.1 | 99.2 | <0.001 |
| Continent | |||||||
| Australia and New Zealand | 7 | 137,116 | 33,281 | 24.4 | 23.2 to 25.6 | 93.9 | <0.001 |
| Asia | 13 | 14,718 | 4089 | 30.2 | 21.9 to 40.1 | 98.9 | <0.001 |
| Europe | 40 | 65,200 | 21,157 | 23.5 | 20.6 to 26.7 | 98.8 | <0.001 |
| America | 48 | 209,120 | 46,992 | 18.8 | 16.1 to 21.8 | 99.3 | <0.001 |
| Multiple continents | 2 | 3381 | 1914 | 49.0 | 29.3 to 69.0 | 98.6 | <0.001 |
| World zonea | |||||||
| Australia and New Zealand | 7 | 137,116 | 33,281 | 24.4 | 23.2 to 25.6 | 93.9 | <0.001 |
| Eastern Asia | 9 | 12,154 | 3688 | 36.9 | 25.7 to 49.7 | 99.2 | <0.001 |
| Western Asia | 2 | 2006 | 333 | 23.6 | 10.1 to 46.0 | 93.1 | <0.001 |
| South Asia | 2 | 558 | 68 | 13.8 | 4.6 to 34.3 | 95.2 | <0.001 |
| Eastern Europe | 2 | 639 | 111 | 21.4 | 3.6 to 66.8 | 98.8 | <0.001 |
| Western Europe | 10 | 8769 | 1951 | 21.3 | 17.4 to 25.8 | 93.3 | <0.001 |
| Northern Europe | 10 | 8712 | 1451 | 17.2 | 9.9 to 28.2 | 98.9 | <0.001 |
| Southern Europe | 14 | 5494 | 1650 | 26.3 | 19.2 to 34.9 | 97.6 | <0.001 |
| Multi-zone Europe | 4 | 41,586 | 15,994 | 38.3 | 35.9 to 40.8 | 96.2 | <0.001 |
| North America | 42 | 208,019 | 46,565 | 16.6 | 14.0 to 19.5 | 99.3 | <0.001 |
| South America | 6 | 1101 | 427 | 38.9 | 19.0 to 63.3 | 97.9 | <0.001 |
| Multiple zones | 2 | 3381 | 1914 | 49.0 | 29.3 to 69.0 | 98.6 | <0.001 |
| Latitude | |||||||
| North | 96 | 290,854 | 73,547 | 21.4 | 19.3 to 23.6 | 99.4 | <0.001 |
| South | 13 | 138,217 | 33,708 | 30.7 | 28.4 to 33.1 | 97.5 | <0.001 |
| North and South | 1 | 464 | 178 | 38.4 | 34.0 to 42.9 | — | — |
| Country income classificationb | |||||||
| Low income | 1 | 399 | 32 | 8.0 | 5.7 to 11.1 | — | — |
| Lower middle income | 1 | 159 | 36 | 22.6 | 16.8 to 29.8 | — | — |
| Upper middle income | 14 | 12,697 | 3992 | 41.4 | 30.8 to 52.9 | 98.9 | <0.001 |
| High income | 93 | 412,187 | 101,884 | 20.9 | 19.2 to 22.6 | 99.3 | <0.001 |
| Not available | 1 | 4093 | 1489 | 36.4 | 34.9 to 37.9 | — | — |
| Country total health expenditure (% of GDP)c | |||||||
| <5 | 4 | 6554 | 1571 | 36.1 | 17.3 to 60.2 | 99.2 | <0.001 |
| 5–10 | 53 | 208,689 | 57,064 | 26.6 | 24.1 to 29.3 | 99.3 | <0.001 |
| >10 | 52 | 210,199 | 47,309 | 18.4 | 15.9 to 21.2 | 99.2 | <0.001 |
| Not available | 1 | 4093 | 1489 | 36.4 | 34.9 to 37.9 | — | — |
| Duration of follow-up (mo) | |||||||
| <3 | 95 | 413,487 | 102,169 | 22.1 | 20.4 to 23.9 | 99.3 | <0.001 |
| 3–6 | 6 | 4831 | 2101 | 31.5 | 18.6 to 48.0 | 98.6 | <0.001 |
| >6 | 9 | 11,217 | 3163 | 27.7 | 22.2 to 33.9 | 97.3 | <0.001 |
Figure 4.
Pooled AKI-associated mortality rate in studies that used a KDIGO-equivalent serum creatinine-based AKI definition and staging system, or dialysis requirement. Some studies and patients are included in more than one category. KDIGO, Kidney Disease Improving Global Outcomes; 95% CI, 95% confidence interval.
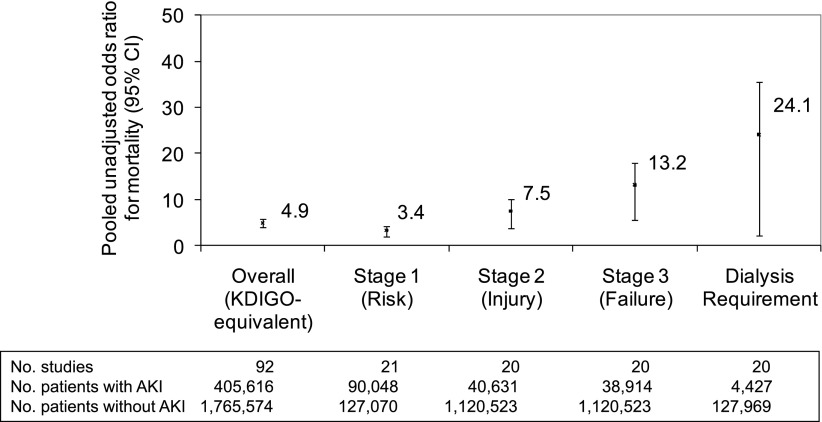
As shown in Table 5 and Figure 5, among the 92 studies that provided a comparative non-AKI group, the pooled unadjusted OR for all-cause mortality in patients with AKI was 4.95 (95% CI, 4.13 to 5.92) relative to patients without AKI. The pooled OR for stage 1–3 AKI was 3.37 (95% CI, 2.43 to 4.68), 7.52 (95% CI, 5.03 to 11.27), and 13.19 (95% CI, 8.39 to 20.76), respectively. For patients who required dialysis, the pooled OR for mortality was the highest at 24.08 (95% CI, 12.62 to 45.95). Finally, the pooled OR declined with longer duration of follow-up. Indeed, the pooled ORs for mortality in patients with AKI were 5.58, 2.25, and 2.74 at <3, 3–6, and >6 months, respectively.
Table 5.
Pooled odds ratio for mortality in patients with AKI relative to patients without AKI in studies that adopted a KDIGO-equivalent AKI definition
| Subgroup | Studies (n) | Patients with AKI (n) | Deaths (n) | Patients without AKI (n) | Deaths (n) | Pooled Odds Ratio | 95% Confidence Interval | P Value | Test for Heterogeneity | |
|---|---|---|---|---|---|---|---|---|---|---|
| I2 Index | Q Test P Value | |||||||||
| Age category | ||||||||||
| Adults | 81 | 403,880 | 98,348 | 1,760,311 | 91,915 | 4.92 | 4.07 to 5.93 | <0.001 | 99.6 | <0.001 |
| Children | 11 | 1736 | 260 | 5263 | 158 | 5.57 | 3.49 to 8.89 | <0.001 | 54.7 | <0.001 |
| Clinical setting | ||||||||||
| Community acquired | 4 | 3875 | 1,724 | 17,202 | 6978 | 2.56 | 1.31 to 5.01 | 0.01 | 95.9 | <0.001 |
| Critical care | 24 | 182,393 | 46,880 | 269,613 | 28,923 | 3.93 | 3.12 to 4.96 | <0.001 | 99.28 | <0.001 |
| Cardiac surgery | 22 | 21,402 | 1852 | 64,776 | 1118 | 6.31 | 4.81 to 8.28 | <0.001 | 87.3 | <0.001 |
| Trauma | 3 | 2387 | 593 | 11,989 | 894 | 6.62 | 1.75 to 24.99 | 0.01 | 98.9 | <0.001 |
| Heart failure | 1 | 221 | 47 | 461 | 52 | 2.13 | 1.38 to 3.27 | 0.001 | — | — |
| Hematology/oncology | 2 | 278 | 76 | 1604 | 27 | 15.50 | 8.40 to 28.60 | <0.001 | 37.5 | 0.21 |
| Nephrotoxins | 1 | 81 | 12 | 2112 | 140 | 2.45 | 1.30 to 4.63 | 0.01 | — | — |
| Hospital acquired, unspecified | 35 | 194,979 | 47,424 | 1,397,817 | 53,941 | 5.15 | 3.86 to 6.87 | <0.001 | 99.4 | <0.001 |
| Continent | ||||||||||
| Australia and New Zealand | 6 | 136,888 | 33,190 | 210,289 | 21,413 | 3.34 | 2.14 to 5.22 | < 0.001 | 99.8 | <0.001 |
| Asia | 10 | 13,702 | 3424 | 208,457 | 5374 | 8.10 | 4.78 to 13.71 | <0.001 | 98.3 | <0.001 |
| Europe | 33 | 44,525 | 13,743 | 150,667 | 10,776 | 5.21 | 4.39 to 6.18 | <0.001 | 95.0 | <0.001 |
| America | 41 | 207,120 | 46,337 | 1,194,232 | 53,832 | 4.57 | 3.30 to 6.33 | <0.001 | 99.5 | <0.001 |
| Multiple continents | 2 | 3381 | 1914 | 1929 | 678 | 2.12 | 1.42 to 3.16 | <0.001 | 82.8 | 0.02 |
| World zonea | ||||||||||
| Australia and New Zealand | 6 | 136,888 | 33,190 | 210,289 | 21,413 | 3.34 | 2.14 to 5.22 | <0.001 | 99.8 | <0.001 |
| Eastern Asia | 6 | 11,133 | 3023 | 182,810 | 5062 | 6.73 | 3.41 to 13.29 | <0.001 | 98.9 | <0.001 |
| Western Asia | 2 | 2011 | 333 | 23,978 | 303 | 9.18 | 2.95 to 28.62 | <0.001 | 87.2 | 0.01 |
| South Asia | 2 | 558 | 68 | 1669 | 9 | 49.45 | 0.57 to 4275.16 | 0.09 | 89.5 | 0.002 |
| Eastern Europe | 2 | 639 | 111 | 1961 | 131 | 6.06 | 3.896 to 9.43 | <0.001 | 36.2 | 0.21 |
| Western Europe | 9 | 4473 | 1114 | 16,732 | 955 | 6.25 | 3.93 to 9.94 | <0.001 | 90.9 | <0.001 |
| Northern Europe | 8 | 7764 | 1005 | 68,554 | 2008 | 5.70 | 3.95 to 8.24 | <0.001 | 85.6 | <0.001 |
| Southern Europe | 11 | 4639 | 1410 | 9371 | 1410 | 4.73 | 3.23 to 6.92 | <0.001 | 90.2 | <0.001 |
| Multi-zone Europe | 3 | 27,010 | 10,103 | 54,049 | 6272 | 4.34 | 2.84 to 6.64 | <0.001 | 99.2 | <0.001 |
| North America | 38 | 206,460 | 46,204 | 1,193,397 | 53,769 | 4.49 | 3.21 to 6.29 | <0.001 | 99.5 | <0.001 |
| South America | 3 | 660 | 133 | 835 | 63 | 5.64 | 2.18 to 14.62 | <0.001 | 65.6 | 0.06 |
| Multiple zones | 2 | 3381 | 1914 | 1929 | 678 | 2.12 | 1.42 to 3.16 | <0.001 | 82.8 | 0.02 |
| Latitude | ||||||||||
| North | 82 | 267,604 | 65,107 | 1,554,136 | 70,512 | 5.15 | 4.29 to 6.19 | <0.001 | 99.2 | <0.001 |
| South | 9 | 137,548 | 33,323 | 211,124 | 21,476 | 3.71 | 2.50 to 5.51 | <0.001 | 99.7 | <0.001 |
| North and South | 1 | 464 | 178 | 314 | 85 | 1.68 | 1.23 to 2.29 | 0.001 | — | — |
| Country income classificationb | ||||||||||
| Low income | 1 | 399 | 32 | 648 | 9 | 6.19 | 2.92 to 13.11 | <0.001 | — | — |
| Lower middle income | 1 | 159 | 36 | 1021 | 0 | 597.37 | 36.43 to 9796.52 | <0.001 | — | — |
| Upper middle income | 9 | 11,336 | 3064 | 181,135 | 5051 | 6.57 | 3.68 to 11.74 | <0.001 | 98.2 | <0.001 |
| High income | 80 | 389,629 | 93,987 | 1,570,079 | 85,383 | 4.73 | 3.89 to 5.75 | <0.001 | 99.6 | <0.001 |
| Not available | 1 | 4093 | 1489 | 12,691 | 1630 | 3.88 | 3.57 to 4.21 | <0.001 | — | — |
| Country total health expenditure (% of GDP)c | ||||||||||
| <5 | 3 | 6201 | 1379 | 175,079 | 4133 | 13.85 | 8.76 to 21.89 | <0.001 | 87.4 | <0.001 |
| 5–10 | 42 | 191,213 | 49,672 | 401,894 | 32,656 | 4.69 | 3.83 to 5.74 | <0.001 | 99.1 | <0.001 |
| >10 | 46 | 204,109 | 46,068 | 1,175,910 | 53,654 | 4.83 | 3.54 to 6.59 | <0.001 | 99.4 | <0.001 |
| Not available | 1 | 4093 | 1489 | 12,691 | 1630 | 3.88 | 3.57 to 4.21 | <0.001 | — | — |
| Duration of follow-up (mo) | ||||||||||
| <3 | 79 | 390,221 | 93,750 | 1,725,376 | 82,092 | 5.58 | 4.60 to 6.76 | <0.001 | 99.5 | <0.001 |
| 3–6 | 3 | 4178 | 1695 | 16,947 | 6913 | 2.25 | 1.09 to 4.68 | 0.03 | 94.8 | <0.001 |
| >6 | 10 | 11,217 | 3163 | 23,251 | 3068 | 2.74 | 2.09 to 3.58 | <0.001 | 93.9 | <0.001 |
Figure 5.
Pooled unadjusted odds ratio for all-cause mortality in patients with AKI relative to patients without AKI in studies that used a KDIGO-equivalent serum creatinine-based AKI definition and staging system, or dialysis requirement. Some studies and patients are included in more than one category. KDIGO, Kidney Disease Improving Global Outcomes; 95% CI, 95% confidence interval.
Discussion
The objective of our meta-analysis was to estimate the global incidence of AKI and to describe geographic variations according to countries, regions, and their economies. We identified a total of 312 large cohort studies representing close to 50 million patients published since 2004, the year in which the RIFLE criteria were first published. Following a process of harmonization, AKI was reclassified in 154 studies in accordance with the KDIGO AKI definition and staging system, thus allowing for more harmonious estimates. Using the KDIGO definition, 1 in 5 adults (21.6%) and 1 in 3 children (33.7%) experienced AKI worldwide. Higher rates of AKI were observed in critical care settings and after cardiac surgery, identifying these high-risk populations in urgent need for interventions. Hospital-acquired AKI, especially among the critically ill, was disproportionately represented in the literature, contrasting with community-acquired AKI, which was not. This is clearly an issue in regions located south of the equator, where AKI tends to develop in rural communities in response to infections such as gastroenteritis, malaria, leptospirosis, and hemolytic-uremic syndrome (20). These findings highlight an important knowledge gap in the published AKI literature. We observed a higher rate of AKI in children due in part to a higher representation of studies of critically ill children (38%). Pooled mortality rates were 23.9% in adults and 13.8% in children. In studies in which stages of AKI could be ascertained, patients with stage 1–3 AKI experienced 3- to 7-fold higher odds for death compared with those without AKI, consistent with previous observations (6–9).
Another important finding was the disproportionate representation of certain countries and clinical settings in the scientific literature. Nearly half of the studies were from North America, which represents only 5% of the world population (21). This contrasted with only two studies from Africa, home to 15% of the world population. Most studies originated from high-income countries (82.7%) and countries that spent ≥5% of GDP on total health expenditure (91.7%). Although AKI rates were higher in studies from countries that spent a greater percentage of GDP on total health expenditure, AKI-associated mortality rate was inversely associated with percentage of country GDP spent on total health expenditure and gross national income per capita, suggesting improved health care delivery. We found a decline in AKI rates and associated mortality over the span of 8 years. Although this might reflect improved supportive care of hospitalized patients with AKI (22), a recent analysis using administrative codes revealed an increase in the incidence of dialysis-requiring AKI over the past decade in the United States, with the number of deaths more than doubling (23). These discrepancies require further investigation.
To our knowledge, this is the first and largest meta-analysis that has systematically examined the global incidence of AKI. By imposing a large study sample size, limiting the search strategy to a more contemporaneous period representing an era of development of consensus definitions for AKI, and harmonizing the definition of AKI for consistency with the latest classification and staging system, we were able to generate more valid and generalizable pooled point estimates.
There are several important limitations, however. The pooled rates were not standardized or normalized to at-risk periods. Most studies originated from high-income countries, involving hospitalized and often critically ill patients. Assumptions were required to harmonize definitions of AKI according to one classification and staging system to generate pooled estimates, possibly introducing biases. The under-representation of studies of community-acquired AKI represents a biased sample because we imposed a large sample size for study inclusion, which likely excluded smaller reports of community-acquired AKI originating from developing countries. Although sources of study heterogeneity were explored through a broad range of subgroup and meta-regression analyses, heterogeneity remained significant across all examined subgroups. In addition, by linking study-level aggregated data to country-level geographic and economic characteristics, our analyses are susceptible to ecological inference fallacy. Higher AKI rates in studies from developed countries with a greater percentage of GDP allocated to health care expenditure may be due to ascertainment bias as a result of wider availability of laboratory testing and publication bias, because more studies are published in such regions of the world. We were also unable to assess long-term kidney-related endpoints. In a recent meta-analysis of 13 cohort studies, the pooled incidence rates of CKD and kidney failure in patients with AKI were 25.8 and 8.6 per 100 person-years, respectively (24).
Our meta-analysis carries implications for the scientific community and future development of public health policies related to AKI. Point estimates for the incidence of AKI, its stages of severity and associated mortality, including patterns of variations according to clinical settings, world geographic regions and economies should be taken into consideration during the planning, design, and execution of trials for AKI. A recent review identifies an abundance of underpowered small single-center trials in AKI (25), which may influence prematurely clinical practice. This lack of large definitive trials should galvanize the development of multinational interdisciplinary AKI trial networks, encouraging close collaborations of the academic, private, and governmental sectors to help reduce the global burden of AKI. There is also a need for more studies on AKI in less developed and lower-income countries, and in community settings, where the implementation of low-cost strategies (e.g., oral hydration for treatment of gastroenteritis) might have a large effect on preventing AKI.
In conclusion, there is a need for greater innovation in the prevention and treatment of AKI, a condition that affects 1 in 5 hospitalized patients worldwide. As World Kidney Day 2013 focuses on AKI, this analysis provides a platform to facilitate discussions among health care professionals, the public, and policy makers to raise awareness about AKI and its associated health care burden. These discussions should encourage providers to design better hospital-based health care delivery systems that focus on the prevention, early detection, and treatment of AKI, improve patient safety, and ultimately, preserve kidney health and well-being while mitigating the long-term costly burden of CKD.
Disclosures
B.L.J. serves as scientific advisor for NxStage Medical, Inc.
Supplementary Material
Acknowledgments
The following individuals are members of the 2013 Acute Kidney Injury Advisory Group of the American Society of Nephrology: Jorge Cerda (Albany Medical College, Albany, New York), Lakhmir S. Chawla (George Washington University, Washington, DC), Sarah Faubel (University of Colorado, Denver, CO), Dinna N. Cruz (University of California, San Diego, CA), Zheng Dong (Medical College of Georgia, Augusta, GA), Stuart L. Goldstein (University of Cincinnati College of Medicine, Cincinnati, OH), Benjamin D. Humphreys (Harvard Medical School, Boston, MA), Jay L. Koyner (University of Chicago, Chicago, IL), Bertrand L. Jaber (Tufts University School of Medicine, Boston, MA), Kathleen D. Liu (University of California, San Francisco, CA), Thomas D. Nolin (University of Pittsburgh, Pittsburgh, PA), Krishna R. Polu (Affymax, Palo Alto, CA), Didier Portilla (University of Arkansas College of Medicine, Little Rock, AR), Krystyna E. Rys-Sikora (National Institutes of Health, Bethesda, MD), Mark D. Okusa (University of Virginia School of Medicine, Charlottesville, VA), and Rachel N. Shaffer (American Society of Nephrology, Washington, DC).
J.C., D.N.C., and B.L.J. are members of the Acute Kidney Injury Advisory Group of the American Society of Nephrology. The opinions expressed in this manuscript are the opinions of the authors and not necessarily the opinions of their institutions or members of the American Society of Nephrology.
This work was made possible in part through an International Society of Nephrology–funded fellowship to P.S.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.00710113/-/DCSupplemental.
See related editorial, “AKI Is Around the World but Public Recognition Is Lacking,” on pages 1467–1468.
References
- 1.Collins AJ, Couser WG, Dirks JH, Kopple JD, Reiser T, Riella MC, Robinson S, Shah SV, Wilson A: World Kidney Day: An idea whose time has come. J Am Soc Nephrol 17: 600–601, 2006 [DOI] [PubMed] [Google Scholar]
- 2.World Kidney Day: Kidneys for Life. http://www.worldkidneyday.org Accessed January 05, 2013
- 3.Levey AS, Andreoli SP, DuBose T, Provenzano R, Collins AJ: Chronic kidney disease: Common, harmful, and treatable—World Kidney Day 2007. Clin J Am Soc Nephrol 2: 401–405, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup : Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8: R204–R212, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A, Acute Kidney Injury Network : Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care 11: R31, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ricci Z, Cruz D, Ronco C: The RIFLE criteria and mortality in acute kidney injury: A systematic review. Kidney Int 73: 538–546, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Thakar CV, Christianson A, Freyberg R, Almenoff P, Render ML: Incidence and outcomes of acute kidney injury in intensive care units: A Veterans Administration study. Crit Care Med 37: 2552–2558, 2009 [DOI] [PubMed] [Google Scholar]
- 8.Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL: Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int 71: 1028–1035, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Dasta JF, Kane-Gill SL, Durtschi AJ, Pathak DS, Kellum JA: Costs and outcomes of acute kidney injury (AKI) following cardiac surgery. Nephrol Dial Transplant 23: 1970–1974, 2008 [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group : Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6: e1000097, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.United Nations Statistics Division: Composition of macro geographical (continental) regions, geographical sub-regions, and selected economic and other groupings. Available at: http://millenniumindicators.un.org/unsd/methods/m49/m49regin.htm Accessed April 20, 2013
- 12.The World Bank: How we classify countries. Available at: http://data.worldbank.org/about/country-classifications Accessed April 20, 2013
- 13.The World Bank: World Development Indicators database. Gross national income per capita 2011, Atlas method and PPP. Available at: http://databank.worldbank.org/databank/download/GNIPC.pdf Accessed April 15, 2013
- 14.World Health Organization: World Health Statistics 2012. Available at: http://www.who.int/gho/publications/world_health_statistics/2012/en/index.html Accessed April 20, 2013
- 15.Kidney Disease Improving Global Outcomes (KDIGO): KDIGO clinical practice guideline for acute kidney injury. Kidney Int 2: 1–138, 2012 [DOI] [PubMed] [Google Scholar]
- 16.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P: The Newcastle-Ottawa Scale for assessing the quality of nonrandomized studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Accessed April 20, 2013
- 17.R Development Core Team: R: A language and environment for statistical computing. Available at: http://www.R-project.org Accessed April 10, 2013
- 18.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J: Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 11: 193–206, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Viechtbauer W: Conducting meta-analyses in R with the metafor package. J Stat Softw 36: 1–48, 2010 [Google Scholar]
- 20.Cerdá J, Bagga A, Kher V, Chakravarthi RM: The contrasting characteristics of acute kidney injury in developed and developing countries. Nat Clin Pract Nephrol 4: 138–153, 2008 [DOI] [PubMed] [Google Scholar]
- 21.United Nations, Department of Economic and Social Affairs, Population Division: World Population Prospects: The 2008 Revision. Available at: http://www.un.org/esa/population/publications/wpp2008/wpp2008_highlights.pdf Accessed April 20, 2013
- 22.Erickson SE, Martin GS, Davis JL, Matthay MA, Eisner MD, NIH NHLBI ARDS Network : Recent trends in acute lung injury mortality: 1996-2005. Crit Care Med 37: 1574–1579, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsu RK, McCulloch CE, Dudley RA, Lo LJ, Hsu CY: Temporal changes in incidence of dialysis-requiring AKI. J Am Soc Nephrol 24: 37–42, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coca SG, Singanamala S, Parikh CR: Chronic kidney disease after acute kidney injury: A systematic review and meta-analysis. Kidney Int 81: 442–448, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Faubel S, Chawla LS, Chertow GM, Goldstein SL, Jaber BL, Liu KD, Acute Kidney Injury Advisory Group of the American Society of Nephrology : Ongoing clinical trials in AKI. Clin J Am Soc Nephrol 7: 861–873, 2012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.