Summary
The National Institute of Diabetes and Digestive and Kidney Diseases-supported Kidney Research National Dialogue (KRND) asked the scientific community to formulate and prioritize research objectives that would improve our understanding of kidney function and disease. Several high-priority objectives for diabetic nephropathy were identified in data and sample collection, hypothesis generation, hypothesis testing, and translation promotion. The lack of readily available human samples linked to comprehensive phenotypic, clinical, and demographic data remains a significant obstacle. With data and biological samples in place, several possibilities exist for using new technologies to develop hypotheses. Testing novel disease mechanisms with state-of-the-art tools should continue to be the foundation of the investigative community. Research must be translated to improve diagnosis and treatment of people. The objectives identified by the KRND provide the research community with future opportunities for improving the prevention, diagnosis, and treatment of diabetic nephropathy.
Kidney disease is a significant medical and public health problem (1). The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) recently asked the community to identify research objectives that, if addressed, would improve our understanding of basic kidney function and aid in the prevention, treatment, and reversal of kidney disease. The Kidney Research National Dialogue (KRND) welcomed all interested parties to submit, discuss, and prioritize ideas via an interactive website. During the past 2 years, 1600 participants posted almost 300 ideas covering all areas of kidney disease.
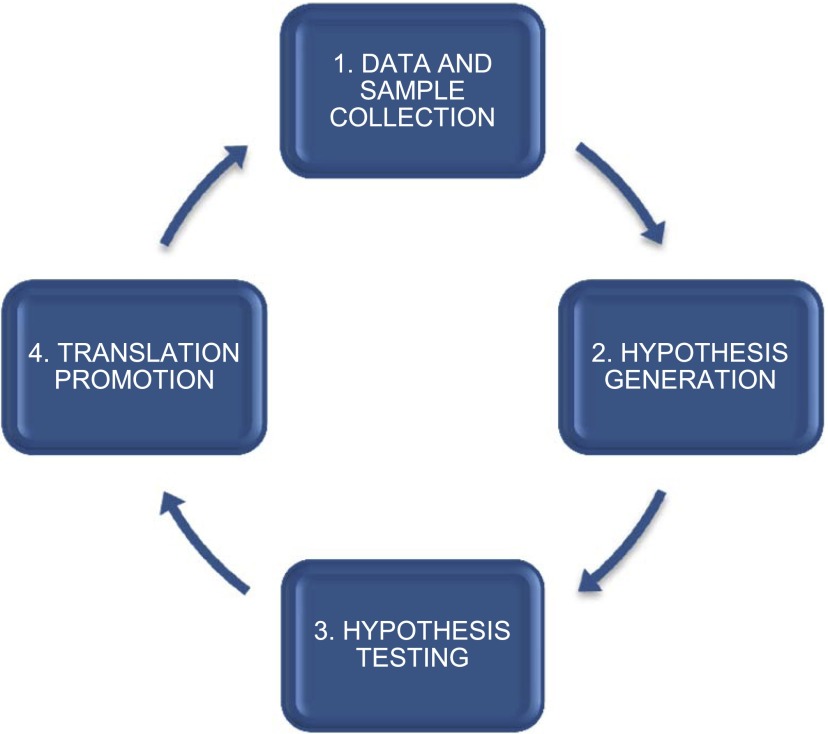
Diabetic nephropathy (DN) is the largest single cause of ESRD in the United States and accounts for nearly 44% of the >115,000 newly affected individuals requiring dialysis each year (1). People with DN do poorly on dialysis, with high rates of infection, access failure, and cardiovascular complications. Of all the long-term complications of diabetes, nephropathy imposes the highest costs in terms of both dollars and human suffering. Despite aggressive management, the risk for ESRD in DN remains high. New management strategies and therapies are needed. The KRND identified several research objectives for DN that fall into four categories (Figure 1).
Figure 1.
Categories of research objectives indentified by the Kidney Research National Dialogue.
Data and Sample Collection
Lack of readily available human samples linked to comprehensive phenotypic, clinical, and demographic data remains a significant obstacle. The community proposed several ideas to encourage the collection of these resources for discovery science in DN.
Establish a Network of Biorepositories of Well Characterized Human Samples
A large amount of material (including DNA, urine, serum, and immortalized cells) is in storage from multiple clinical trials and genetic studies. Coordination of access to these samples should be initiated.
Collaborate with Large Health Organizations
Major efforts should be made to preconsent and obtain clinical data and biologic samples (including tissues) from people at risk for DN beginning early in the course of illness, taking advantage of large, coordinated care systems with electronic medical records. Correlation of assay results from these samples with longitudinal data are essential and would allow investigators to more fully understand the heterogeneity of clinical DN and identify patterns of disease that might otherwise be missed.
Partner with Transplant Surgeons and Urologists Who Perform Nephrectomies
Tissue samples from people who have kidneys removed for trauma or cancer should be retained. Samples of normal kidney tissue collected at the time of donor nephrectomy could be used as control material. Long-term follow-up of these donors and others who undergo nephrectomy would also be of considerable interest.
Leverage Ongoing and Completed Clinical Studies
Longitudinal studies of disease (e.g., Chronic Renal Insufficiency Cohort study, Diabetes Control and Complications Trial, Epidemiology of Diabetes Interventions and Complications Study) provide a rich source of material coupled with comprehensive phenotyping. Immediate efforts should be made to consent individuals so that data and samples from these and future studies are available to the wider research community. Complication rates from kidney biopsies are low (2), thereby enhancing the practicability of people undergoing biopsies for research purposes.
Hypotheses Generation
With comprehensive data and biological samples in place, several possibilities exist for using new technologies to develop hypotheses.
Define Key Genetic and Epigenetic Risk Factors
Metabolic control alone does not fully predict an individual’s risk for diabetic complications (3). Identifying variants is a critical step in determining causality and defining the genetic and epigenetic architecture of human DN. Many of the ideas discussed in the KRND identify corollary issues to this fundamental objective, and there was strong support for using unbiased mapping strategies to achieve this goal.
Determine Molecular Pathways
The abundance of molecular pathways affected by diabetes presents not only the challenge of understanding complex interactions but also the opportunity of providing multiple and potentially complementary targets for drug development that can be tested using trial designs that are more representative of real-life clinical practice. Continued research into the underlying pathogenic mechanisms mediating diabetic complications should be highly encouraged.
Analyze the Efficacy of Systems Biology to Discover New Pathways and Targets
Systems biology aims to define the underlying regulatory principles in complex human diseases. Appropriate tools are needed to integrate genotyping information, RNA expression, promoter analysis, proteome expression, and metabolome profiles. This knowledge needs to be applied to clinical diabetes through better access and techniques for understanding human pathobiology.
Hypothesis Testing
Pursuing novel disease mechanisms with state-of-the-art tools should continue to be the foundation of our investigative community.
Create “Humanized” Mice
Although mouse models have many advantages, the human phenotype is difficult to faithfully replicate using candidate gene approaches. Future work should focus on developing “humanized” mice, in which loci associated with human diabetic complications are knocked in. The technology for recapitulating these human variants in mice will be one of the few options for direct functional testing in mammals (4).
Define a Role for Nonmammalian Systems
Nonmammalian model organisms are underused. These simple organisms permit ease of genetic manipulation, rapid throughput, genome-wide screens, and precise measurement of phenotypes (5). More should be done with large-scale screens that require establishing congruencies between model organisms and mammals.
Develop Novel Technologies
There is an expectation that imaging, systems biology, and bioinformatics will identify new areas of clinical relevance in DN. If that happens, scientists will require new levels of training and robust collaborations.
Translation Promotion
The community provided several ideas to enhance diagnosis and treatment of DN.
Develop Biomarkers
The lack of robust and dynamic biomarkers for molecular classification, risk stratification, morphologic prediction, and alternative outcomes is a major gap in the field, contributing to the high cost and long duration of clinical trials. Discovery of biomarkers that are sensitive to the rate of disease progression would allow rapid screening of potential therapeutics and preselection of clinical trial participants.
Identify New Ways to Foster Translation
Mechanisms should be established to support development of drugs and biologics that will not be pursued by industry. The expansion of existing preclinical programs and the establishment of clinical trial networks would allow potential therapies to be developed and tested in early phase I and II trials that could lead to phase III trials.
Analyze How “Omic” Medicine May Alter Patient Care
Personalized medicine is limited by the number of therapies and the “omic” approaches used to identify people who would be responsive to a particular therapy. Nevertheless, work in this area could have significant potential for identifying new therapeutic targets and improved applications of existing therapies.
Conclusion
Research efforts over the past several years generally relied on candidate approaches, predicated on individual hypotheses and often tested exclusively in cell culture or animal models. Although these efforts led to interesting biology, more progress needs to be made in understanding key mechanisms in human DN. Progress toward this end is hampered by the relative paucity of longitudinally phenotyped individuals and biologic samples to provide the necessary resources to stimulate innovative clinical, translational, and basic research. In oncology, by contrast, the ubiquitous availability of tissue has fueled substantial advances in understanding molecular pathogenesis and developing new therapies. The KRND proposes to discover critical candidates, identify regulatory pathways, generate novel models for preclinical work, and develop biomarkers with clinical utility so DN outcomes can be improved.
Disclosures
Dr. Breyer is an employee of Eli Lilly. The remaining coauthors had no disclosures to provide.
Supplementary Material
Acknowledgments
The KRND was developed and implemented by NIDDK/ Division of Kidney, Urologic, and Hematologic Diseases staff and was directed by Dr. Krystyna Rys-Sikora. The DN topic was facilitated by Drs. Chris Ketchum and Mike Flessner. Visit the KRND (http://www2.niddk.nih.gov/KUH/KUHHome/) or the NIDDK-supported Diabetic Complications Consortium (http://www.diacomp.org/) for full details or to post comments about this review.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03640413/-/DCSupplemental.
References
- 1.U.S. Renal Data System : USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012 [Google Scholar]
- 2.Jiang SH, Karpe KM, Talaulikar GS: Safety and predictors of complications of renal biopsy in the outpatient setting. Clin Nephrol 76: 464–469, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Costacou T, Chang Y, Ferrell RE, Orchard TJ: Identifying genetic susceptibilities to diabetes-related complications among individuals at low risk of complications: An application of tree-structured survival analysis. Am J Epidemiol 164: 862–872, 2006 [DOI] [PubMed] [Google Scholar]
- 4.Devoy A, Bunton-Stasyshyn RKA, Tybulewicz VLJ, Smith AJH, Fisher EMC: Genomically humanized mice: technologies and promises. Nat Rev Genet 13: 14–20, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ragvin A, Moro E, Fredman D, Navratilova P, Drivenes O, Engström PG, Alonso ME, de la Calle Mustienes E, Gómez Skarmeta JL, Tavares MJ, Casares F, Manzanares M, van Heyningen V, Molven A, Njølstad PR, Argenton F, Lenhard B, Becker TS: Long-range gene regulation links genomic type 2 diabetes and obesity risk regions to HHEX, SOX4, and IRX3. Proc Natl Acad Sci U S A 107: 775–780, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.