Abstract
The aim of this study was to use magnetic resonance imaging (MRI) to classify the morphological changes and remodeling of the right ventricle (RV) that occur in different clinical situations and that have an impact on RV function. Most literature has traditionally focused on the left ventricle (LV) and as a result, few studies analyze RV behavior and remodeling. The study evaluated all cardiac MRI performed at our center from 2008 to 2010. We retrospectively identified 159 patients who had some sign of right ventricular dysfunction (RVD) based on MRI findings. We classified patients according to a combination of criteria for RVD and the presence of left ventricle dysfunction (LVD). We considered RVD as any of the following abnormalities: i) depressed RV function; ii) RV dilatation; iii) RV hypertrophy. LVD was considered when there was atrial dilatation, LV hypertrophy, LV dilatation and/or depressed LV function. We obtained 6 pathophysiological patterns: RV pressure overload (1.9%), RV volume overload (15.7%), RV volume overload + LVD (32.7%), depressed RV function + LVD (42.1%), mixed RV overload + LVD (6.9%) and other (0.6%). The most frequent etiology was congenital heart disease (33.3%), followed by idiopathic dilated cardiomyopathy (18.2%), left valvular disease (17.6%), ischemic heart disease (15%), pulmonary disease (9.8%), and other (6.1%). This study helps to classify the different patterns that RV can adopt in different clinical situations and can, therefore, help us to understand the RV pathophysiology.
Key words: right ventricle, congenital heart disease, magnetic resonance imaging
Introduction
Most of the scientific evidence in cardiology has traditionally focused on the left ventricle (LV). This is due to the major systemic impact when this ventricle fails and the difficulty in assessing right ventricle (RV) function correctly with the classic techniques. As a result, there are few studies focusing on the analysis of RV behavior and remodeling. This has led prestigious scientific societies to strongly recommend the development of research lines focusing on the analysis of the changes occurring in the RV in different clinical situations.1
Until a few years ago, knowledge of the LV was extrapolated to the RV, assuming its pathophysiology was similar. However, this approach has been revealed to be incorrect and lacking a scientific basis. The main differences with the LV are that the RV is not ellipsoidal (half-moon shape), it functions in a state of low pressure and high flow, and pumps blood to a vascular bed with a high capacitance.2-3 These characteristics make the structure and function of the RV, as well as the behavior and phenotypic patterns it is capable of adopting under different stress situations, different from those of the LV.
Part of our current lack of knowledge about the RV has been due to the lack of suitable techniques for its study. Ultrasound study of the RV is limited by its location and shape, so it was not until the introduction of cardiac magnetic resonance imaging (MRI) that it could be analyzed properly. Its better spatial resolution has allowed the RV to be studied properly and with its own parameters, leaving behind the measurements based on the LV and becoming the reference imaging technique for its study.4,5
The aim of this study was to use MRI to classify the morphological changes and remodeling of the RV that occur in the different clinical scenarios that have impact on this ventricle.
Materials and Methods
This was a descriptive study evaluating all cardiac MRI exams performed at our center from 31st January 2008 to December 2010. This hospital serves a population of 250,000 inhabitants. In addition, it is the reference hospital for heart surgery for 1,000,000 inhabitants, and the reference hospital for heart transplant, heart-lung transplant and complex adult congenital heart disease for approximately 4,600,000 inhabitants.
The study was approved by the clinical research ethics committee of our hospital.
Of the 2824 cardiac MRI exams performed, we retrospectively identified 159 patients who had some sign of right ventricular dysfunction (RVD).
We considered RVD as any of the following abnormalities: i) depressed RV function (RV ejection fraction <50%), considered severely depressed if ejection fraction (EF) was <35%; ii) RV dilatation (RV indexed end-diastolic volume >106 mL/m2 in men and >92 mL/m2 in women);6 iii) RV hypertrophy: iv) wall diameter >6 mm in any right ventricular segment.
Left ventricular dysfunction (LVD) was considered to be present when there was at least one of the following criteria: i) atrial dilatation (>40 mm); ii) LV hypertrophy (≥13 mm in men and ≥12 mm in women); iii) LV dilatation (LV indexed end-diastolic volume >105 mL/m2); iv) depressed LV function (EF<50%).
We classified patients according to a combination of criteria for RVD and the presence of LVD.
The etiology of heart disease was established by individualized review of patient medical records. The results of the MRI studies were confirmed independently by 2 specialists in cardiac MRI. When the differences between the two evaluators implied a change in pattern, evaluation by a third expert was requested to reach a consensus.
Magnetic resonance imaging technique
Cardiac MRI was performed on a Magnetom Avanto® Syngo MR 2004V scanner (Siemens AG, Germany). All scans included a baseline module plus another module for calculation of volumes. Optional modules were added as necessary.
Baseline module
This was performed in the strict axial and coronal planes. Anatomical sequences consisted of axial HASTE and True-FISP images, coronal HASTE and oblique sagittal True-FISP images. Functional sequences consisted of cine True-FISP images in 2, 3 and 4 chamber views and short axis sequences, with a thickness of 7 mm, spacing of 3 mm and from base to apex.
Calculation of volumes
Functional sequences were true fast imaging steady state free precession sequences (True-FISP): repetition time/echo time 2.8/1.2 ms, flip angle 58°, matrix 256x256, field of view 320x270 mm, slice thickness 8 mm, obtained in 2, 3 and 4 chamber long axis views and short axis sequences, spacing of 3 mm and from base to apex.
In all modules, electrocardiographic synchronization was retrospective with a minimum of 20 phases/cycle and a minimum temporal resolution of 25 ms.
To calculate inter and intra-observer agreement, 11 patients of the study sample were randomly selected and reassessed and the following values were obtained: FEVI (CIC 0.92; CI: 0.8-0.9), FEVD (CIC 0.7; CI: 0.3-0.9), VTDVI (CIC 0.83. CI: 0.5-0.9), VTDVD (CIC 0.72 CI: 0.4-0.9), the presence of right ventricle hypertrophy (Kappa 0.5, P=0.05) and impaired right ventricle wall motion (Kappa 0.8, P<0.01).
Results
Mean patient age was 48±21 years, and 65.4% were men.
After reviewing the 159 MRI images, we obtained 6 phenotypic patterns (Table 1). Figures 1-5 show the different phenotypic patterns that can be adopted by the RV on remodeling.
Table 1.
Differential characteristics of the different patterns.
| Pathophysiological patterns of right ventricle dysfunction | Characteristics | |||
|---|---|---|---|---|
| M-S depression | RV dilatation | RV hypertrophy | LVD | |
| RV pressure overload | No | No | Yes | No |
| RV volume overload | No/Yes | Yes | No | No |
| RV volume overload + LVD | No/Yes | Yes | No | Yes |
| Depressed RV function + LVD | No/Yes | No | No | Yes |
| Mixed RV overload + LVD | No/Yes | Yes | Yes | Yes |
| Other | No | No | Yes | Yes |
LVD, left ventricular dysfunction; RV, right ventricle; LV, left ventricle; RVH, right ventricular hypertrophy, M-S, moderate-severely depressed RV function.
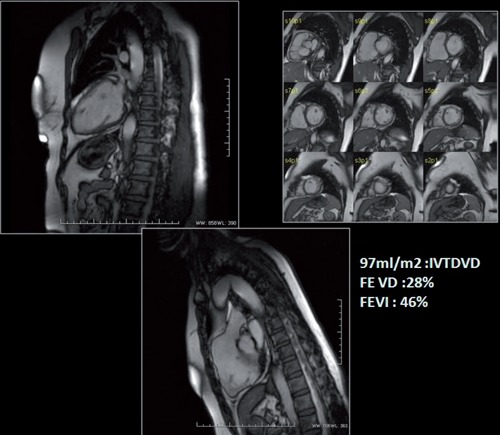
Figure 1.
True fast imaging with steady-state precession sequence in two chamber (top left), short axis (top right), and right ventricle outflow tract (bottom) in a patient with a biventricular dilated cardiomyopathy.
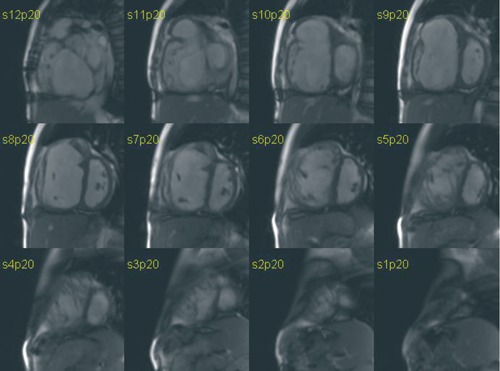
Figure 2.
True fast imaging with steady-state precession sequence (from right to left) in short axis orientation at medium level during diastole and systole in a patient with a hypertrophic cardiomyopathy.
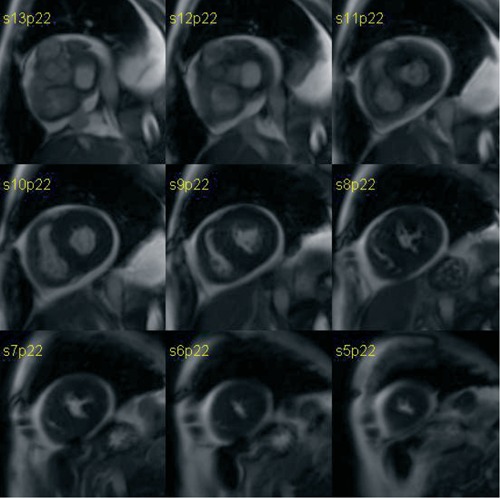
Figure 3.
True fast imaging with steady-state precession sequence (A-D) of short axis in a patient with tetralogy of Fallot. The patient has a mild left ventricle dysfunction due to the alteration of the septal contractility as a consequence of the right ventricle volume overload.
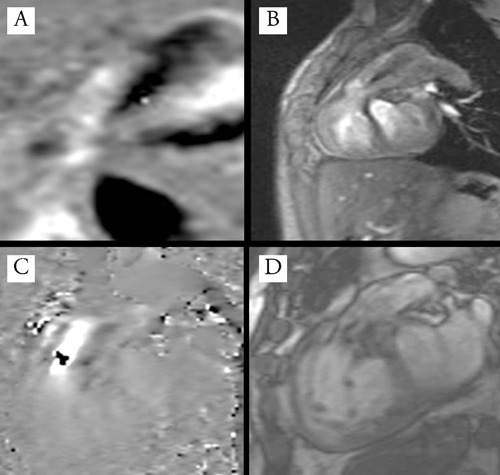
Figure 4.
True fast imaging with steady-state precession sequence in short axis orientation at medium level during diastole (right) and sistole (left) in a patient with pressure and volume right ventricle overload. Top right: biventricular function analysis and pulmonary insufficiency quantification in the same patient with the software Qmass and Qflow of Medis™. Bottom: phase contrast sequences at the pulmonary valve level in the same patient. Here we observe the severe pulmonary insufficiency.
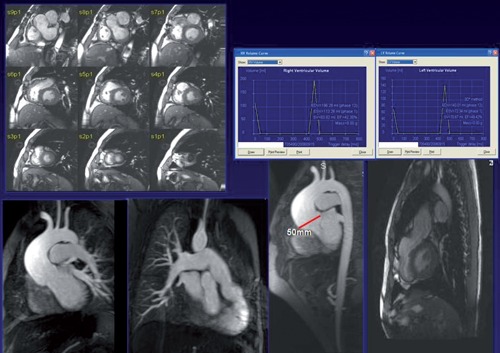
Figure 5.
Top: flash 3D angiographic sequences with MPR reconstructions at right ventricular outflow tract level. We observe the severe infundibular stenosis. Bottom: true fast imaging with steady-state precession sequence at the same level. Here we observe the infundibular hypertrophy in the right ventricle as a consequence of the pressure overload.
The most frequent etiology was congenital heart disease (33.3%), followed by idiopathic dilated cardiomyopathy (Figure 1) (18.2%), left valvular disease (17.6%), ischemic heart disease (15%), pulmonary disease (9.8%), and other (6.1%) such as biventricular hypertrophic cardiomyopathy (Figure 2). Among congenital heart diseases, and over the total percentage, 18.2% were tetralogy of Fallot (Figure 3) (TOF), 4.4% were pulmonary insufficiency not associated with tetralogy of Fallot, and 10.7% were other causes, such as pulmonary stenosis + pulmonary insufficiency (Figure 4) or isolated pulmonary stenosis (Figure 5). Frequencies and etiologies of the patterns are shown in Table 2.
Table 2.
Prevalence of patterns and causal etiologies.
| Pathophysiological patterns of right ventricle dysfunction | Frequency | Etiologies (number of cases) |
|---|---|---|
| RV pressure overload | 3 (1.9%) | PS (1); TGV (1); PHT (1) |
| RV volume overload | 25 (15.7%) | Operated TOF + PI (16): Non-TOF PI (2); PS-PI (2); Interatrial shunt (3); PHT (2) |
| RV volume overload + LVD | 52 (32.7%) | Left valvular disease (18); IDCM (10); TOF + PI (8); Non-TOF PI (4); Ischemic (5); Other (7) |
| Depressed RV function + LVD | 67 (42.1%) | Ischemic (19); IDCM (18); Valvular disease. Left (10); Right congenital (4); Pulmonary (4); Other (12) |
| Mixed RV overload + LVD | 11 (6.9%) | PS (5); Operated PS + severe PI (3); Other congenital (2); Pulmonary (1) |
| Other | 1 (0.6%) | Biventricular HCM (1) |
RV, right ventricle; LVD, left ventricular dysfunction; RVH, right ventricular hypertrophy; PS, pulmonary stenosis; TGV, transposition of the great vessels; PHT, pulmonary hypertension; TOF, tetralogy of Fallot; PI, pulmonary insufficiency; IDCM, idiopathic dilated cardiomyopathy; HCM, hypertrophic cardiomyopathy.
More than 70% of the cases of RVD were found to be concentrated in two patterns. These were patterns 3 and 4, corresponding to RV volume overload + LVD and depressed RV function + LVD. Quantitative results of MRI scans can be seen in Table 3 and in Figure 6.
Table 3.
Ejection fraction and ventricular volumes in the patterns studied.
| Pattern | RVEF (%) |
RVIEDV (mL) |
RVIESV (mL) |
LVEF (%) |
LVIEDV (mL) |
LVIESV (mL) |
|---|---|---|---|---|---|---|
| 1 | 59.5±14.2 | 85.2±19.9 | 36.0±17.4 | 69.8±2.9 | 65.5±8.2 | 19.8±3.9 |
| 2 | 47.0±10.9 | 138.4±31.4 | 71.9±16.9 | 63.1±3.7 | 69.0±13.4 | 25.6±6.2 |
| 3 | 36.2±14.2 | 140.3±29.5 | 89.0±24.4 | 45.4±17.3 | 111.6±50.1 | 66.9±49.1 |
| 4 | 38.9±9.1 | 69.6±19.5 | 42.8±14.6 | 38.8±15.9 | 112.5±48.4 | 73.5±45.7 |
| 5 | 47.2±14.1 | 165.8±59.2 | 89.4±48.0 | 59.6±8.4 | 96.7±29.2 | 35.8±12.2 |
Mean ± standard deviation for each parameter is shown. RVEF, right ventricular ejection fraction; RVIEDV, right ventricular indexed end-diastolic volume; RVIESV, right ventricular indexed end-systolic volume; LVEF, left ventricular ejection fraction; LVIEDV, left ventricular indexed end-diastolic volume; LVIESV, left ventricular indexed end-systolic volume.
Figure 6.
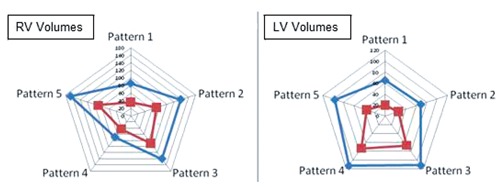
Ejection fraction and indexed volumes of both ventricles in the patterns studied. Blue: indexed end-diastolic volume. Red: indexed end-systolic volume.
Discussion
For some time now, it has been known that the RV markedly influences the course and prognosis of numerous heart diseases.7-8 However, there is still much uncertainty about the behavior of the RV under different stress situations. In the present study, we characterized for the first time the different phenotypic patterns that are adopted by the RV in different clinical situations.
In the etiological analysis of RVD, congenital heart disease (33.3%), idiopathic dilated cardiomyopathy (18.2%) and left valvular disease (17.6%) accounted for the majority of the cases. This first finding clearly differentiated the RV from the LV, where the predominant causes of LVD are the ischemic and hypertensive etiologies. This may have been influenced by the type of population served by the hospital and in which MRI is performed.
Pattern 1 or pressure overload is uncommon (1.9%). It is characterized by normal or slightly depressed RV function with RV hypertrophy (RVH). In our series, we observed only 3 cases: one patient with an operated transposition of the great arteries with conduit stenosis, one with pulmonary stenosis (PS), and another with primary pulmonary artery hypertension. In all 3 cases, isolated pressure overload (without pulmonary insufficiency) was the cause of RVH, which in itself is regarded as a sign of systolic dysfunction of the RV.9 RVH is an adaptive mechanism to increased afterload, but the RV is unable to maintain this situation for very long,10 so the RV eventually succumbs, depresses its systolic function and begins to dilate, which makes pattern 1 uncommon.
The second pattern has been named volume overload, and is characterized by a dilated RV. Its etiology was congenital in more than 90% of the cases, mainly pulmonary insufficiency (PI), either primary or secondary to previous congenital heart disease surgery, especially TOF. We observed 2 cases of pulmonary hypertension (PH) due to a pulmonary cause and 2 cases of double pulmonary aortic lesion. We considered that these cases were caused by a pattern 1 in which the RV had succumbed, dilated and reduced RV free wall thickness.11 Other etiologies such as interatrial shunts or severe PIs without a PS phase may present directly with this pattern.
A differential feature of this pattern versus pattern 3 is the absence of LVD. LV function may remain intact in patients with TOF for years, but eventually becomes depressed. In advanced phases, LVD is due to evident changes in LV geometry as a result of RV dilatation,12 but in early phases, this dysfunction seems to be more related with the muscular band shared by both ventricles, especially at the level of the apex.13 Other factors that promote LVD are the number of reoperations and late surgical repair.14 Finally, we consider that the degree of depression of LV function depends on time since onset of the heart condition.
Pattern 3 or volume overload plus LVD is the second most frequent pattern (32.7%). Its chief characteristic is dilatation of the RV and LVD of any type. Etiologies are divided almost equally between left and right origin. In both ventricles, the predominant etiologies in this pattern are valvular (mitral insufficiency and PI) and dilated cardiomyopathies with biventricular dysfunction. As occurs in the previous pattern, LV function can be more or less depressed depending on disease duration. In the case of left valvular disease, LVD would be the consequence of PH caused by increased pulmonary capillary pressure and the mechanisms involved in ventricular interdependence. LV dysfunction from right valvular disease would thus be the consequence of ventricular interdependence, to which surgery should be added in some cases.15,16 In idiopathic dilated cardiomyopathy, in addition to the described mechanisms, intrinsic dysfunction of the RV due to underlying disease would be added.
The characteristics of this pattern lead one to think that it is not a direct pattern in many cases, but rather it may be the result of progression from others. Thus, we consider that most TOFs with PI from pattern 3 originate from progression of pattern 2, with significant alteration of RV geometry causing alteration of the LV.
The most frequent phenotypic pattern (42.1%) was pattern 4 or depressed biventricular function. Depressed LV function occurs in a context of a normal sized RV with LVD. Unlike the LV, when depression of RV function occurs because of a disease intrinsic to the ventricle itself, it is usually preceded by prior dilatation. In contrast, this pattern, present in many etiologies, predominates in depressed function of left origin: ischemic heart disease, left valvular disease, idiopathic dilated cardiomyopathies and pulmonary disease. The mechanisms of ventricular interdependence are key to this pattern16 and are related to the muscle fibers shared by both ventricles,13 involvement of the interventricular septum, distortion of ventricular geometry and alterations in pericardial distensibility.16 In the absence of RV dilatation, only contraction of the septum can maintain the hemodynamic stability of the RV;17 therefore, septal involvement by a left cause negatively impacts the RV. In cases of ischemic etiology, it should be added that the RVD may be directly affected by the ischemia itself, despite it being less vulnerable to ischemia due to its lower oxygen consumption.18
Unlike pattern 3, patients with pattern 4 with left valvular disease do not present RV dilatation. We think this is due in these cases to the fact that RV may not be able to adapt to this overload and responds directly by depressing its function without prior dilatation. The pathophysiology of patients with pulmonary etiology in this group is different. In these cases, LVD would be mainly due to PH, with LVD appearing as a consequence of chronic hypoxia.19
It is unlikely that pattern 4 is due to progression from other patterns. This is because this is no dilatation of the RV, but only depression of its function. This excludes the majority of congenital heart diseases with right ventricular dysfunction, as these are usually associated with valvular disease and thus with pressure or volume overload, which finally leads to RV dilatation.
Pattern 5 has been called mixed overload, as there is co-existing biventricular dysfunction (in different degrees depending on disease duration), dilatation and RVH. It is an uncommon pattern (6.9%), which in all cases except one was due to congenital heart diseases, specifically TOFs operated on for severe PS and with residual pulmonary vein insufficiency (PVI). In these cases, RVH had not returned totally, a condition that occurs particularly when corrective surgery is performed at advanced age.20 Dilatation, as in pattern 2, would be the result of postoperative PVI, so common in patients operated on for TOF. LVD would have as its cause the surgical intervention, postoperative alteration of the septum and distortion of LV geometry as a result of RV dilatation.
From the perspective of pattern progression, pattern 5 would be formed mainly by pattern 1 patients with progression in whom RVH had not returned. This pattern is the one with the most increased end-diastolic and end-systolic volumes.
This study has the limitations intrinsic to retrospective descriptive studies and the bias resulting from the cases being from a reference hospital in congenital heart disease surgery. In our hospital, cardiac MRI is a highly accessible technique and of routine use in hemodynamically stable patients. The request for the MRI was at the discretion of the treating physician. Another bias to be noted is that cases with left valvular disease are underrepresented in our sample, since there is the clinical attitude that MIR is of little help in its diagnosis and so is rarely used in clinical decision-making.
This study helps us to understand how the RV remodels and adopts different phenotypic patterns in the different heart diseases that can affect its function. Therefore, we think it is highly useful from the diagnostic and clinical perspective.
Conclusions
This is the first study to classify the different patterns that the RV can adopt in different clinical scenarios. Thus, we have identified up to 6 different patterns depending on the type of RV dysfunction and the co-existence of LV disease.
None of the patterns is composed of a single etiology, but by several pathological entities that equally affect the RV. On the other hand, the patterns identified are not static, since progression of the underlying diseases causes a flow between patterns, which thus exhibit a dynamic pathophysiology and behavior.
This classification by phenotypic patterns helps us to better understand the response and remodeling of the RV in different heart diseases, and provides new knowledge of the mode of response and behavior of this ventricle.
References
- 1.Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation 2008;117:1436–48 [DOI] [PubMed] [Google Scholar]
- 2.Dell’Italia LJ. The right ventricle: anatomy, physiology, and clinical importance. Curr Probl Cardiol 1991;16:653–720 [DOI] [PubMed] [Google Scholar]
- 3.Sugeng L, Mor-Avi V, Weinert L, et al. Multimodality comparison of quantitative volumetric analysis of the right ventricle. JACC Cardiovasc Imag 2010;3:10–8 [DOI] [PubMed] [Google Scholar]
- 4.Boxt LM. Radiology of the right ventricle. Radiol Clin North Am 1999;37:379–400 [DOI] [PubMed] [Google Scholar]
- 5.Puchalski MD, Williams RV, Askovich B, et al. Assessment of right ventricular size and function: echo versus magnetic resonance imaging. Congenit Heart Dis 2007;2:27–31 [DOI] [PubMed] [Google Scholar]
- 6.Maceira AM, Prasad SK, Khan M, Pennell DJ. Reference right ventricular systolic and diastolic function normalized to age, gender and body surface area from steady-state free precession cardiovascular magnetic resonance. Eur Heart J 2006;27:2879–88 [DOI] [PubMed] [Google Scholar]
- 7.Ghio S, Gavazzi A, Campana C, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol 2001;37:183–8 [DOI] [PubMed] [Google Scholar]
- 8.Meluzín J, Spinarová L, Dusek L, et al. Prognostic importance of the right ventricular function assessed by Doppler tissue imaging. Eur J Echocardiogr 2003;4:262–71 [DOI] [PubMed] [Google Scholar]
- 9.Tulevski II, Hirsch A, Dodge-Khatami A, et al. Effect of pulmonary valve regurgitation on right ventricular function in patients with chronic right ventricular pressure overload. Am J Cardiol 2003;92:113–6 [DOI] [PubMed] [Google Scholar]
- 10.Bogaard HJ, Abe K, Vonk Noordegraaf A, Voelkel NF. The right ventricle under pressure: cellular and molecular mechanisms of right-heart failure in pulmonary hypertension. Chest 2009;135:794–804 [DOI] [PubMed] [Google Scholar]
- 11.Mitsuno M, Nakano S, Shimazaki Y, et al. Fate of right ventricular hypertrophy in tetralogy of Fallot after corrective surgery. Am J Cardiol 1993;72:694–8 [DOI] [PubMed] [Google Scholar]
- 12.Walker RE, Moran AM, Gauvreau K, Colan SD. Evidence of adverse ventricular interdependence in patients with atrial septal defects. Am J Cardiol 2004;93:1374–7 [DOI] [PubMed] [Google Scholar]
- 13.Torrent-Guasp F. Structure and function of the heart. Rev Esp Cardiol 1998;51:91–102 [DOI] [PubMed] [Google Scholar]
- 14.Broberg CS, Aboulhosn J, Mongeon FP, et al. Prevalence of left ventricular systolic dysfunction in adults with repaired tetralogy of fallot. Am J Cardiol 2011;107:1215–20 [DOI] [PubMed] [Google Scholar]
- 15.Chin KM, Kim NH, Rubin LJ. The right ventricle in pulmonary hypertension. Coron Artery Dis 2005;16:13–8 [DOI] [PubMed] [Google Scholar]
- 16.Santamore WP, Dell’Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis 1998;40:289–308 [DOI] [PubMed] [Google Scholar]
- 17.Hoffman D, Sisto D, Frater RW, Nikolic SD. Left-to-right ventricular interaction with a noncontracting right ventricle. J Thorac Cardiovasc Surg 1994;107:1496–502 [PubMed] [Google Scholar]
- 18.Haupt HM, Hutchins GM, Moore GW. Right ventricular infarction: role of the moderator band artery in determining infarct size. Circulation 1983;67:1268–72 [DOI] [PubMed] [Google Scholar]
- 19.Flu WJ, van Gestel YR, van Kuijk JP, et al. Co-existence of COPD and left ventricular dysfunction invascular surgery patients. Respir Med 2010;104:690–6 [DOI] [PubMed] [Google Scholar]
- 20.Perloff JK. Development and regression of increased ventricular mass. Am J Cardiol 1982;50:605–11 [DOI] [PubMed] [Google Scholar]


