Abstract
OBJECTIVES
In patients with lung cancer, endosonography has emerged as a minimally invasive method to obtain cytological proof of mediastinal lymph nodes, suspicious for metastases on imaging. In case of a negative result, it is currently recommended that a cervical mediastinoscopy be performed additionally. However, in daily practice, a second procedure is often regarded superfluous. The goal of our study was to assess the additional value of a cervical mediastinoscopy, after a negative result of endosonography, in routine clinical practice.
METHODS
In a retrospective cohort study, the records of 147 consecutive patients with an indication for mediastinal lymph node staging and a negative result of endosonography were analysed. As a subsequent procedure, 124 patients underwent a cervical mediastinoscopy and 23 patients were scheduled for an intended curative resection directly. The negative predictive value (NPV) for both diagnostic procedures was determined, as well as the number of patients who needed to undergo a mediastinoscopy to find one false-negative result of endosonography (number needed to treat (NNT)). Clinical data of patients with a false-negative endosonography were analysed.
RESULTS
When using cervical mediastinoscopy as the gold standard, the NPV for endosonography was 88.7%, resulting in a NNT of 8.8 patients. For patients with fluoro-2-deoxyglucose positron emission tomography positive mediastinal lymph nodes, the NNT was 6.1. Overall, a futile thoracotomy could be prevented in 50% of patients by an additional mediastinoscopy. A representative lymph node aspirate, containing adequate numbers of lymphocytes, did not exclude metastases.
CONCLUSIONS
In patients with a high probability of mediastinal metastases, based on imaging, and negative endosonography, cervical mediastinoscopy should not be omitted, not even when the aspirate seems representative.
Keywords: Lung cancer, Mediastinal staging, Endosonography, Mediastinoscopy
INTRODUCTION
In patients with lung cancer, precise clinical staging is mandatory to provide appropriate therapy. In the absence of distant metastases, mediastinal lymph node staging is essential to select patients for an intended curative treatment. Assessment of the mediastinum is primarily based on a combination of computed tomography (CT) scan and 18fluoro-2-deoxyglucose positron emission tomography (18FDG-PET). However, despite an improved accuracy of these imaging modalities over the last decade [1], invasive staging remains necessary in case of mediastinal lymph node enlargement, PET positive mediastinal and/or hilar lymph nodes and/or a centrally located tumour [2, 3]. For a long time, cervical mediastinoscopy has been considered the gold standard in mediastinal staging, given the high negative predictive value (NPV) if well performed [4]. During the last decade, oesophageal ultrasound-guided fine needle aspiration (EUS-FNA) followed by endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has emerged as a minimally invasive alternative, reducing the need for a cervical mediastinoscopy as a first-line staging procedure. Especially by combining both techniques, nearly all mediastinal lymph node stations are accessible, thus making it possible to perform cytological analysis of mediastinal lymph nodes considered suspicious on imaging. When, nevertheless, the result of endoscopic staging appears negative, a subsequent mediastinoscopy is currently recommended to exclude mediastinal lymph node metastases in patients with clinical suspicion [2]. But, since the sensitivity of EBUS-FNA seems to exceed that of mediastinoscopy [5, 6], the need for surgical confirmation may be diminished. Accordingly, in daily practice an additional mediastinoscopy is often regarded as overdone. However, recently only the combination of endosonography followed by mediastinoscopy was shown to be more accurate in mediastinal nodal staging than mediastinoscopy alone, reducing the rate of futile thoracotomies by more than half. Yet, 11 patients had to undergo a cervical mediastinoscopy to find one positive result after negative endosonography [7].
The goal of our study was to assess the additional value of a cervical mediastinoscopy in patients with suspected or proven non-small-cell lung cancer, after a negative result of endosonographic mediastinal staging, in routine clinical practice.
MATERIALS AND METHODS
In a retrospective cohort study, medical records of 147 consecutive patients with suspected or proven non-small-cell lung cancer and a negative result of combined endosonographic mediastinal staging between January 2009 and August 2012 were analysed.
All patients were clinically staged based on a diagnostic CT scan of the chest and upper abdomen, followed by an integrated PET/CT scan, according to the current Dutch guidelines.
When there was no sign of distant metastasis, endoscopic mediastinal lymph node staging was performed in case of enlarged and/or FDG-PET positive hilar and/or mediastinal lymph nodes, and/or a centrally located tumour. Lymph nodes with a short axis >1 cm were considered enlarged, and a tumour was considered central if located in the inner 1/3 of the lung parenchyma on a transverse image on CT scan. Since patients were referred from different hospitals, lymph nodes were considered FDG-PET positive, when clearly stated in the report of nuclear medicine of the referring hospital. In case of only a mild increased uptake by hilar and/or mediastinal lymph nodes and thus a dubious suspicion, FDG-PET was considered negative.
Endosonographic mediastinal staging, with the availability of both EUS-FNA and EBUS-TBNA, using Pentax EG3870UTK and EB1970UK scopes (Pentax Medical, Hamburg, Germany/Tokyo, Japan) in combination with a Hitachi EUB 7000HV ultrasound scanner (Hitachi Medical Corp., Japan), was performed as an outdoor clinic procedure under conscious sedation. All procedures were performed by two experienced pulmonologists. The choice for one or both modalities was made by the performing pulmonologist, based on the location and side of the primary tumour, as well as the location of the suspicious mediastinal lymph nodes. Although sometimes aspirated, lymph nodes <5 mm were regarded as unsuitable for assessment. In all patients, FNA was performed using 22G needles (Medi-Globe and Cook). Rapid on site evaluation (rose) was available in all cases to assess the yield of the procedure and was performed by an analyst of the department of pathology. The definitive diagnosis was based on cytological and immunocytochemical analysis of the obtained slides and cell-block specimens.
After a negative result of endosonography with regard to the mediastinal lymph nodes, 124 patients were scheduled for a cervical mediastinoscopy and 23 patients directly underwent an intended curative resection. In these patients, mediastinoscopy was omitted due to patient factors (laryngectomy, previous cervical radiotherapy and struma).
A cervical mediastinoscopy was performed using a video-mediastinoscope (Karl Storz GmbH, Tuttlingen, Germany) in all patients. Performance was based on the recommendations of the European Society of Thoracic Surgeons (ESTS) [2], with multiple biopsies taken of at least the lower paratracheal lymph nodes on both sides, as well as the subcarinal lymph nodes, regardless of their size.
In case of a thoracotomy, a complete resection was performed according to the definition of the International Union Against Cancer (UICC), including a lymph node dissection of at least three mediastinal stations, always including the subcarinal station [8].
The NPV of endosonography was calculated, using cervical mediastinoscopy as the gold standard, as well as using the combination of cervical mediastinoscopy and, when performed, thoracotomy as the gold standard. The NPV of mediastinoscopy was calculated using thoracotomy as the gold standard. Furthermore, the number of patients who had to undergo a subsequent mediastinoscopy to detect one false-negative result of endosonography (number needed to treat (NNT)) was determined. The analysis was based on an intention to treat.
Finally, clinical data of patients with a false-negative result of endosonography were analysed. Statistical analyses were performed using the SPSS 18.0 statistical software (SPSS, Inc., Chicago, IL, USA).
RESULTS
Imaging
Of all the 147 patients included in this study with an indication for invasive mediastinal staging, the tumour was located centrally in 52 patients (35%). In 80 patients (54%), lymph nodes in at least one station appeared to be enlarged on CT scan and FDG-PET demonstrated positive lymph nodes in 96 patients (65%): hilar lymph nodes only in 38 patients, mediastinal lymph nodes only in 21 patients and both in 37 patients.
Endosonography
As a result of these findings on imaging studies, patients were scheduled for endoscopic mediastinal staging. An EBUS-TBNA was performed in 88 patients (60%), an EUS-FNA in 29 patients (20%) and both modalities were used in 30 patients (20%).
In 147 patients, a total of 259 lymph nodes were aspirated (mean of 1.8, range 0–5). In 124 patients, both mediastinal and hilar lymph nodes were examined, with a mean of 1.5 (range 1–4) mediastinal lymph nodes aspirated. In 5 patients, only hilar lymph nodes were aspirated. In the remaining 18 patients, no aspiration was performed.
In addition to the aspirated lymph nodes, 231 lymph nodes in 147 patients (mean 1.6, range 0–4) were inspected. The size of the aspirated lymph nodes, mean 8.6 mm (range 2–23), was different from that of the inspected ones, with a mean size of 5.2 mm (range 1.8–40) (P < 0.001). When aspirated, on average 2.5 samples (range 1–6) per lymph node were taken. In 109 of 124 patients, the yield of at least one mediastinal lymph node was considered representative by pathology, based on the relative amount of lymphocytes present in at least one aspirate.
Cervical mediastinoscopy
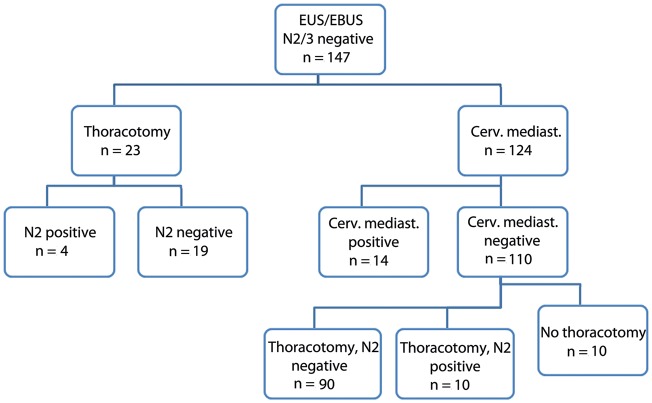
As a next-step procedure, 124 patients underwent a cervical mediastinoscopy, while in 23 patients a thoracotomy was performed directly (Fig. 1).
Figure 1:
Flow chart of patients with suspected locally advanced lung cancer, after tumour negative mediastinal endosonography, n = 147 patients.
Assessment of the mediastinum by mediastinoscopy was in accordance with the recommendations of the ESTS in 98.5% of patients. The mean number of mediastinal lymph node stations biopsied was 4.0 (range 1–5, standard deviation 0.69). In 77 patients 4 stations were biopsied, in 26 patients 5 stations, in 19 patients 3 stations, in 1 patient 2 stations and in the remaining patient 1 station.
Mediastinoscopy demonstrated positive lymph nodes in 14 of 124 patients (11%), revealing positive ipsilateral (N2) nodes in 11 patients and positive contralateral (N3) nodes in 3 patients (Table 1). Of 4 patients with only positive intrapulmonary lymph nodes found by endosonography, mediastinoscopy was positive in 1.
Table 1:
Upstaging based on lymph node involvement, n = 147 patients
| After endosonography (n = 147 patients) | After cervical mediastinoscopy (n = 124 patientsa) | After thoracotomy (n = 123 patientsb) | |
|---|---|---|---|
| N0/N1 | 147 | 110 | 109 |
| N2 | – | 11 | 14 |
| N3 | – | 3 | – |
aTwenty-three patients did not undergo a cervical mediastinoscopy.
bTwenty-four patients did not undergo a thoracotomy (14 patients because of a positive mediastinoscopy).
Thoracotomy
In 100 of the remaining 110 patients, an intended curative resection was performed, including a mediastinal lymph node dissection of at least three mediastinal stations. Ten patients did not undergo a resection: in 6 patients because of poor condition or patient preference for a different therapy, in 2 patients because of an irresectable tumour and in the last 2 patients the suspected tumour was proved to be a benign lesion. Despite endosonography followed by cervical mediastinoscopy, unexpected mediastinal lymph node metastases were found in 10 of 100 patients (10%) who had undergone a resection.
In 23 patients, mediastinoscopy was not performed. In 4 of these patients, mediastinal lymph node metastases were detected by thoracotomy.
Predictive value
Using only the result of cervical mediastinoscopy as the gold standard, the NPV for endosonography was 88.7%. When using both cervical mediastinoscopy and/or thoracotomy as the gold standard, this NPV was 80.9%.
For a cervical mediastinoscopy, with a thoracotomy as the gold standard, the NPV was 90%, although the sensitivity was only 58% in this cohort with a prevalence of N2 disease of 21%.
Since mediastinoscopy was positive in 14 of 124 patients, the NNT was 8.8 patients.
When only patients with a high probability of mediastinal metastases were considered, based on FDG-PET positive mediastinal lymph nodes in contrast to only hilar suspicion or a central tumour, mediastinoscopy was positive in 9 of 55 patients, resulting in a NNT of 6.1 patients (Table 2).
Table 2:
Reliability of endosonography and cervical mediastinoscopy in mediastinal staging
| NPV | NNT | |
|---|---|---|
| All patients (n = 147) | ||
| Endosonography (n = 147) | ||
| CM gold standard | 88.7% | 8.8 |
| CM and/or thoracotomy gold standard | 80.9% | |
| Cervical mediastinoscopy (n = 124) | ||
| Thoracotomy gold standard | 90% | 10 |
| High probability based on FDG-PETa (n = 55) | ||
| Endosonography (n = 55) | ||
| CM golden standard | 83.6% | 6.1 |
aPatients with 18FDG-PET positive mediastinal lymph nodes.
CM: cervical mediastinoscopy; NPV: negative predictive value; NNT: number needed to treat, to find one false-negative result of the diagnostic procedure.
By adding cervical mediastinoscopy to the clinical workup, in this series a futile thoracotomy could be prevented in 14 of 28 patients (50%).
Analysis of false-negative endosonography
In 28 patients, the result of mediastinal staging by endosonography was false-negative. Of these patients, mediastinal lymph nodes were enlarged on CT scan in 15 patients and 21 patients demonstrated positive lymph nodes on FDG-PET (mediastinal lymph nodes in 12 patients and hilar nodes only in 9 patients). Five patients had to undergo invasive mediastinal staging because of a centrally located tumour.
In 4 patients, no lymph nodes were aspirated during endosonography. In the remaining 24 patients, 39 mediastinal stations were investigated (average 1.6, range 1–3), in combination with 9 intrapulmonary lymph node stations. After cytopathological analysis, the yield of endosonography was considered representative (i.e. containing mature as well as immature lymphocytes), in 25 of 39 investigated mediastinal lymph node stations. In 18 of 24 patients the yield of at least one mediastinal station was considered representative.
In 14 of 28 patients, the false-negative result of endosonography was identified by mediastinoscopy. In these patients, the mean number of mediastinal lymph node stations aspirated by endosonography was 1.5 (range 0–3), compared with 3.9 (range 1–5) biopsied by mediastinoscopy. The lower paratracheal lymph nodes (Station 4) were responsible for most of the failures of endosonography, followed by the subcarinal lymph nodes (Station 7) and upper paratracheal lymph nodes (Station 2) (Table 3). In 2 patients 2 mediastinal stations were positive by mediastinoscopy and 3 stations in another 2 patients.
Table 3:
False-negative mediastinal endosonography: analysis of lymph node stations, n = 28 patients
| Mediastinal lymph node station | Positive by cervical mediastinoscopy (n = 14 patients) | Positive by thoracotomy, no cervical mediastinoscopy (n = 4 patients) | Positive by thoracotomy, despite cervical mediastinoscopy (n = 10 patients) | Total FN result endosonography (n = 28 patients) |
|---|---|---|---|---|
| 2 R | 2 | – | – | 2 |
| 2 L | 2 | – | – | 2 |
| 4 R | 7 | 1 | 4 | 12 |
| 4 L | 5 | – | 1 | 6 |
| 5 | – | 1 | 3 | 4 |
| 6 | – | – | – | – |
| 7 | 4 | 1 | 2 | 7 |
| 8 | – | – | 1 | 1 |
| 9 | – | 1 | – | 1 |
R: right; L: left; FN: false-negative.
In 7 of these 14 patients, metastases were found in lymph node stations despite assessment by endosonography, and in only 1 of them the yield was considered not representative by the pathologist. In 5 patients, metastases appeared in lymph node stations not examined by endosonography; in the remaining 2 patients, no lymph nodes had been aspirated (Table 4).
Table 4:
False-negative mediastinal endosonography: analysis of yield of endosonography, n = 28 patients
| Detected by cervical mediastinoscopy (n = 14 patients) | Detected by thoracotomy (n = 14 patients) | Total | |
|---|---|---|---|
| Metastasis in: aspirated LN station and representative | 6 | 3 | 9 |
| Metastasis in: aspirated LN station, not representative | 1 | 3 | 4 |
| Metastasis in: non-aspirated LN station | 5 | 6 | 11 |
| No LN station aspirated | 2 | 2 | 4 |
| Total | 14 | 14 | 28 |
LN: lymph node.
In the remaining 14 of 28 patients unexpected N2 disease was found by thoracotomy: in 10 patients after negative results of both endosonography and cervical mediastinoscopy and in 4 patients after negative endosonography only. Also in this group of patients, endosonography failed most frequently in the lower paratracheal lymph nodes (Station 4), followed by the subaortic lymph nodes (Station 5) and subcarinal lymph nodes (Station 7) (Table 3). In 2 patients, no lymph node aspirates were taken during endosonography; in 6 patients, metastases were found in lymph node stations also aspirated by endosonography, with a representative yield in 3 of them. In the remaining 6 patients, metastases were found by thoracotomy in lymph node stations not aspirated during endosonography (Table 4).
In 10 of these 14 patients also mediastinoscopy was false-negative. In 3 patients, because of positive subaortic and in 1 patient because of a positive paraoesophageal lymph node, both being out of reach for a cervical approach. In 6 patients, lymph node stations were positive despite a biopsy at the time of mediastinoscopy.
DISCUSSION
Treatment planning in patients with a non-small-cell lung carcinoma depends on strict and reliable staging. Especially the mediastinal lymph nodes are crucial in determining the contribution and sequence of treatment modalities. For this, EUS- and EBUS-FNA have proved their value and are attractive methods, because of their minimally invasive character [7]. But it is unclear whether a negative result has to be double checked by a cervical mediastinoscopy, being the gold standard in clinical staging. The goal of this study was to assess the additional value of a mediastinoscopy after a negative result of endosonography in patients with suspected or proven lung cancer in our routine clinical practice. This study shows that the NPV for endoscopic staging was 80.9%, considering surgical staging by cervical mediastinoscopy and/or thoracotomy as the gold standard, and 90% for a cervical mediastinoscopy. But more importantly, we found that in every 8.8 patients 1 futile thoracotomy could be avoided by performing an additional mediastinoscopy. This reduced the number of futile thoracotomies by 50%.
Comparable studies, publishing results of both techniques, are limited. In a recent study of patients with a high clinical suspicion of nodal disease who underwent EBUS-TBNA followed by mediastinoscopy, the NNT was 3.6 patients [9]. The ASTER trial, a randomized controlled trial comparing mediastinoscopy with combined endoscopic staging followed by mediastinoscopy, demonstrated a NNT of 11 patients [7]. In a prospective trial, performing both EBUS-TBNA and mediastinoscopy under general anaesthesia in all patients, similar results were achieved for both techniques, suggesting that mediastinoscopy could be replaced by endobronchial staging [10].
These differences in NNT may be explained by patient selection and performance of either technique. It is, therefore, important to determine factors that may identify patients who benefit most from an additional mediastinoscopy after negative endosonopraphy.
First, the probability of mediastinal metastases. Based on the criteria of the European Society of Thoracic Surgeons [2], all patients in our study had an elevated risk of mediastinal metastases, necessitating invasive staging. In a subanalysis of the ASTER trial, according to the risk of mediastinal metastases, no additional value of a mediastinoscopy was demonstrated in patients with a normal mediastinum based on CT and PET imaging, since the pretest probability was already low. However, in patients with an abnormal mediastinum, a number of 7 patients who needed an additional mediastinoscopy to avoid one futile thoracotomy was found [11]. In our study, the prevalence of mediastinal metastases, after a negative result of endosonography, was still 19% and overall we found a NNT of 8.8 patients, to make an additional mediastinoscopy valuable. Yet, in patients with an abnormal mediastinum, thus by excluding patients with only a centrally located tumour or clinical suspicion because of only hilar lymph nodes, this number dropped to 6.1 patients.
Secondly, the completeness of endoscopic staging. Combined endosonography has the advantage that nearly all mediastinal lymph node stations are accessible and the diagnostic yield of the combination of EUS-FNA and EBUS-TBNA is probably higher than that of either technique alone [12]. Nevertheless, in our study, both endoscopic modalities were used in only 20% of patients and the mean number of aspirated mediastinal lymph nodes was 1.5. In contrast to a complete mediastinal investigation, in daily practice performance of endosonography seems to be guided by suspicion on imaging, with regard to both the technique and subsequent aspiration of lymph nodes, and should therefore be classified as selective sampling [13]. For mediastinoscopy, minimal requirements to ensure a high NPV have been defined [2]. Yet, the yield is dependent on the experience of the surgeon and the thoroughness of the mediastinal assessment, as illustrated when more extensive surgical procedures are performed, which demonstrate an even higher NPV [14, 15].
However, these procedures are not widely used. In this series on average four mediastinal lymph node stations were biopsied. When a comparable examination of the mediastinum is performed by endosonography, equivalent reliability may be achieved [10, 16]. However, performance of endosonography is not only dependent on the operator, but also strongly influenced by the condition, and, in particular, comfort of the patient. From this aspect, performance under general anaesthesia creates ideal conditions for endosonography, in contrast to conscious sedation, allowing a more complete examination of the mediastinum, but diminishes one of the advantages of endosonography in an outdoor clinical setting. Furthermore, in our study the false-negative result of endosonography is not only explained by an incomplete examination, since in 7 patients, lymph nodes also aspirated during endosonography appeared positive by mediastinoscopy and in another 6 patients by thoracotomy.
Thus, thirdly, representativeness of the yield of endosonography is an important aspect in determining the need for a mediastinoscopy. A representative sample is supposed to contain lymphocytes in various stages of differentiation, and is a prerequisite for a reliable procedure [17], but also when this criterion was met, we found metastases in aspirated lymph node stations in 9 of 28 patients with a false-negative endosonography. This indicates a sampling error, probably as a result of aspiration of a negative lymph node in an otherwise positive lymph node station, or even negative lymphoid tissue in a positive lymph node due to micrometastases. Furthermore, also by pathological assessment micrometastases may be missed in a representative aspirate. The same is possible for a mediastinoscopy, but less likely, since the yield of a mediastinoscopy in terms of the amount of tissue, if well performed, is huge in comparison with the yield of endosonography and pathological assessment is based on histology instead of cytology. For instance, the chance to detect isolated tumour cells in, or micrometastases near the marginal sinus of a lymph node, is higher in a histological biopsy than in a FNA specimen.
Finally, in assessing the need for an additional mediastinoscopy, the consequence of minimal mediastinal disease is another consideration. Since patients with mediastinal lymph node involvement form a heterogeneous group, using endosonography to rule out multilevel or bulky N2 disease and accept the possibility of minimal residual disease only found by thoracotomy may be an option. Surgical treatment, then followed by adjuvant chemo- and radiotherapy in case of unexpected minimal N2 disease, can be an alternative to induction- or even definitive chemo-radiotherapy for these patients with minimal mediastinal involvement.
The retrospective nature of this study is a limitation when comparing the potential reliability of endosonography and mediastinoscopy in mediastinal nodal staging, but makes it possible to compare the performance of those two techniques in daily practice. Considering additional diagnostic procedures in the workup of patients with lung cancer, the burden for the patient should be balanced against the benefit, and therefore, local expertise in and performance of each technique are important aspects to take into account.
In conclusion, in patients with non-small-cell lung cancer and an indication for mediastinal staging, performing a cervical mediastinoscopy after a negative result of endosonography reduced the number of futile thoracotomies by 50%. Overall, on average 8.8 patients had to undergo an additional mediastinoscopy to find one false-negative result of endosonography, but when only patients with suspicious mediastinal lymph nodes on FDG-PET are taken into account, this NNT diminished to 6.1 patients.
Thus, in patients with a high probability of mediastinal metastases, a cervical mediastinoscopy should not be omitted after a negative result of endosonography, not even when the aspirate seems representative, based on the presence of an adequate number and maturation of lymphocytes.
Conflict of interest: none declared.
REFERENCES
- 1.Silvestri GA, Gould MK, Margolis ML, Tanoue LT, McCrory D, Toloza E, et al. Noninvasive staging of non-small cell lung cancer: ACCP evidenced-based clinical practice guidelines (2nd edition) Chest. 2007;132:178S–201. doi: 10.1378/chest.07-1360. [DOI] [PubMed] [Google Scholar]
- 2.De Leyn P, Lardinois D, van Schil PE, Rami-Porta R, Passlick B, Zielinski M, et al. ESTS guidelines for preoperative lymph node staging for non-small cell lung cancer. Eur J Cardiothorac Surg. 2007;32:1–8. doi: 10.1016/j.ejcts.2007.01.075. [DOI] [PubMed] [Google Scholar]
- 3.Darling GE, Maziak DE, Inculet RI, Gulenchyn KY, Driedger AA, Ung YC, et al. Positron emission tomography-computed tomography compared with invasive mediastinal staging in non-small cell lung cancer: results of mediastinal staging in the early lung positron emission tomography trial. J Thorac Oncol. 2011;6:1367–72. doi: 10.1097/JTO.0b013e318220c912. [DOI] [PubMed] [Google Scholar]
- 4.Anraku M, Miyata R, Compeau C, Shargall Y. Video-assisted mediastinoscopy compared with conventional mediastinoscopy: are we doing better? Ann Thorac Surg. 2010;89:1577–81. doi: 10.1016/j.athoracsur.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Gu P, Zhao YZ, Jiang LY, Zhang W, Xin Y, Han BH. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: a systematic review and meta-analysis. Eur J Cancer. 2009;45:1389–96. doi: 10.1016/j.ejca.2008.11.043. [DOI] [PubMed] [Google Scholar]
- 6.Varela-Lema L, Fernandez-Villar A, Ruano-Ravina A. Effectiveness and safety of endobronchial ultrasound-transbronchial needle aspiration: a systematic review. Eur Respir J. 2009;33:1156–64. doi: 10.1183/09031936.00097908. [DOI] [PubMed] [Google Scholar]
- 7.Annema JT, Meerbeeck van JP, Rintoul RC, Dooms C, Deschepper E, Dekkers OM, et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer. a randomized trial. JAMA. 2010;304:2245–52. doi: 10.1001/jama.2010.1705. [DOI] [PubMed] [Google Scholar]
- 8.Sobin LH. UICC International Union Against Cancer. TNM Classification of Malignant Tumours. 7th edn. Wiley-Blackwell, Hoboken NJ; 2009. [Google Scholar]
- 9.Defranchi SA, Edell ES, Daniels CE, Prakash UB, Swanson KL, Utz JP, et al. Mediastinoscopy in patients with lung cancer and negative endobronchial ultrasound guided needle aspiration. Ann Thorac Surg. 2010;90:1753–58. doi: 10.1016/j.athoracsur.2010.06.052. [DOI] [PubMed] [Google Scholar]
- 10.Yasufuku K, Pierre A, Darling G, de Perrot M, Waddell T, Johnston M, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg. 2011;142:1393–400. doi: 10.1016/j.jtcvs.2011.08.037. [DOI] [PubMed] [Google Scholar]
- 11.Tournoy KG, Keller SM, Annema JT. Mediastinal staging of lung cancer: novel concepts. Lancet Oncol. 2012;13:e221–9. doi: 10.1016/S1470-2045(11)70407-7. [DOI] [PubMed] [Google Scholar]
- 12.Szlubowski A, Zielinski M, Soja J, Annema JT, Sośnicki W, Jakubiak M, et al. A combined approach of endobronchial and endoscopic ultrasound-guided needle aspiration in the radiologically normal mediastinum in non-small-cell lung cancer staging—a prospective trial. Eur J Cardiothorac Surg. 2010;37:1175–9. doi: 10.1016/j.ejcts.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 13.Detterbeck F, Puchalski J, Rubinowitz A, Cheng D. Classification of the thoroughness of mediastinal staging of lung cancer. Chest. 2010;137:436–42. doi: 10.1378/chest.09-1378. [DOI] [PubMed] [Google Scholar]
- 14.Zielinski M, Szlubowski A, Kolodziej M, Orzechowski S, Laczynska E, Pankowski J, et al. Comparison of endobronchial ultrasound and/or endoesophageal ultrasound with transcervical extended mediastinal lymphadenectomy for staging and restaging of non-small-cell lung cancer. J Thorac Oncol. 2013;8:630–6. doi: 10.1097/JTO.0b013e318287c0ce. [DOI] [PubMed] [Google Scholar]
- 15.Witte B, Hürtgen M. Video-assisted mediastinoscopic lymphadenectomy (VAMLA) J Thorac Oncol. 2007;2:367–9. doi: 10.1097/01.JTO.0000263725.89512.d7. [DOI] [PubMed] [Google Scholar]
- 16.Sanz-Santos J, Andreo F, Castellà E, Llatjós M, de Castro PL, Astudillo J, et al. Representativeness of nodal sampling with endobronchial ultrasonography in non-small-cell lung cancer staging. Ultrasound Med Biol. 2012;1:62–8. doi: 10.1016/j.ultrasmedbio.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Nayak A, Sugrue C, Koenig S, Wasserman PG, Hoda S, Morgenstern NJ. Endobronchial ultrasound-guided transbronchial needle aspirate (EBUS-TBNA): a proposal for on-site adequacy criteria. Diagn Cytopathol. 2012;40:128–37. doi: 10.1002/dc.21517. [DOI] [PubMed] [Google Scholar]