Abstract
OBJECTIVES
Delirium after cardiac surgery is a problem with consequences for patients and healthcare. Preventive strategies from known risk factors may reduce the incidence and severity of delirium. The present aim was to explore risk factors behind delirium in older patients undergoing cardiac surgery with cardiopulmonary bypass.
METHODS
Patients (≥70 years) scheduled for routine cardiac surgery were included (n = 142). The patients were assessed and monitored pre-/postoperatively, and delirium was diagnosed from repeated assessments with the Mini-Mental State Examination and the Organic Brain Syndrome Scale, using the DSM-IV-TR criteria. Variables were analysed by uni-/multivariable logistic regression, including both preoperative variables (predisposing) and those extracted during surgery and in the early postoperative period (precipitating).
RESULTS
Delirium was diagnosed in 78 patients (54.9%). Delirium was independently associated with both predisposing and precipitating factors (P-value, odds ratio, upper/lower confidence interval): age (0.036, 1.1, 1.0/1.2), diabetes (0.032, 3.5, 1.1/11.0), gastritis/ulcer problems (0.050, 4.0, 1.0/16.1), volume load during operation (0.001, 2.8, 1.5/5.1), ventilator time in ICU (0.042, 1.2, 1.0/1.4), highest temperature recorded in ICU (0.044, 2.2, 1.0/4.8) and sodium concentration in ICU (0.038, 1.2, 1.0/1.4).
CONCLUSIONS
Delirium was common among older patients undergoing cardiac surgery. Both predisposing and precipitating factors contributed to delirium. When combined, the predictive strength of the model improved. Preventive strategies may be considered, in particular among the precipitating factors. Of interest, delirium was strongly associated with an increased volume load during surgery.
Keywords: Delirium, Cardiac surgery, Risk factors
INTRODUCTION
Neurological complications after cardiac surgery remain an intriguing issue with a complex background. Delirium is a neuropsychiatric syndrome, which found its place in cardiac surgery from the early beginning of cardiopulmonary bypass (CPB) described as postcardiotomy delirium [1]. In more recent years, brain damage after cardiac surgery has been described in terms of stroke and neurocognitive decline, with reference to Type-I and Type-II injury, respectively [2]. Delirium is probably the most common symptom of Type-II injuries. The distinction between delirium and the former nomenclature has not yet been clarified [3].
Postoperative delirium is a clinical reality being common after all types of surgery. Delirium is described as fluctuations in cognition and attention. By definition it is assumed to express an underlying cause and is often transient [4]. The reported incidence of delirium after cardiac surgery varies, exemplified by 8–52% [5–7]. The condition is more common among old patients [8]. The span in incidence between studies may partly reflect various means for how delirium has been screened and diagnosed. Delirium is a psychiatric syndrome that hides various types of pre-existing (predisposing), inflicted brain injuries and side-effects of the medical management (precipitating). Advanced age, previous cerebrovascular disease and diabetes exemplify the commonly referred predisposing risk factors [5]. Suggested precipitating factors are: ventilator time [5], postoperative infections and prolonged operating time [8]. The subdivision of risk factors has a purpose. Predisposing factors may be used for risk evaluation prior to surgery, whereas precipitating factors may be considered for improving the clinical care and avoiding delirium.
This study aimed at identifying potential predisposing and precipitating risk factors behind delirium in consecutive patients, 70 years and older undergoing cardiac surgery.
MATERIALS AND METHODS
Subjects
Patients (≥70 years) scheduled for routine cardiac surgery with planned use of CPB were included. All patients were operated on at the Cardiothoracic Surgery Department, Umeå University Hospital, Sweden, in between February and October 2009. During this period, 199 patients were eligible for inclusion. The exclusions criteria were: acute procedures, planned deep hypothermic arrest, known psychiatric disease, severe communication difficulties and severe vision or hearing problems (n = 6). Also, 15 patients were lost due to administrative reasons, resulting in 178 patients, who were approached. Of these 153 patients gave oral and written consent to participate. Eleven patients did not complete the study protocol due to various reasons leaving 142 patients, who were reviewed for analysis. The 36 patients lost for analysis did not differ from the analysed cohort in terms of gender, age and procedural type. The study was approved by the ethics review board of the medical faculty at Umeå University Hospital (Dnr 08-169M).
Operative procedures and anaesthesia
The patients were premedicated with oral acetaminophen, oxicodone and zopiclone, routinely 2 h before anaesthetic induction. Intramuscular morphine and in a few cases ketobemidone or morfine-scopolamine was administered 30 min before arriving into the operation theatre. General anaesthesia was induced with intravenously propofol and fentanyl, supplemented with small doses of midazolam when required. Tracheal intubation was performed after administration of pancuronium. Muscle relaxation was not reversed. Anaesthesia was maintained with additional fentanyl and isoflurane in air/oxygen. Antibiotic prophylaxis was given routinely until the first postoperative morning. Blood pressure was controlled with phenylephrine or norepinephrine. The requirement of blood transfusion and infusions was assessed from haemodynamics monitoring, urine output, blood-gas measurements and from echocardiographic findings. Surgery was performed according to standard methods including cardioplegic arrest at aortic cross clamping. In coronary procedures, a partial aortic clamp was applied for the suturing of proximal anastomoses. In open-heart procedures, carbon dioxide was flushed over the wound for de-airing purposes. Aortic calcifications were mainly assessed by palpation only or by ultrasound. During CPB, alpha-stat conditions were applied. Propofol infusion was initiated at CPB weaning to be continued until extubation in the intensive care unit (ICU). Extubation occurred when the patient was circulatory and respiratory stable. Postoperative pain relief during hospitalization generally encountered oral paracetamol and oxycodone and if necessary intravenously ketobemidone.
Data collection, assessments and variable definitions
A protocol for data entry was designed in chronology with the ward sequence. Medical, social and functional data were collected by interviewing the patient on admission. Additional data were retrieved from medical records and from the local clinical database.
Variables were separated into predisposing and precipitating (Tables 1 and 2). The predisposing variables were defined as those registered in advance of surgery. In brief, diabetes included childhood and adult types, regardless of insulin requirement. History of cerebrovascular disease included any type of documented stroke or transient ischaemic accident. In general, the predisposing variables included any type of reported or documented ongoing condition of clinical relevance. The precipitating variables described intraoperative and early postoperative observations. The temporal relationship vs delirium onset was considered for causality. The variable volume load during operation was the sum of infused volumes administered in the operating theatre. The variable included: CPB prime with mannitol added, crystalloid cardioplegic solutions and infusions from the anaesthetic management. Blood transfusions were separately analysed and not included in the variable volume load. The term blood transfusions included erythrocytes, plasma or platelets used. Preoperative infusions were generally not given. Infusions during surgery and CPB were of crystalloid type. Crystalloid and colloid infusions administered postoperatively in the ICU were not monitored in this study.
Table 1.
Preoperative variables
| Parameter | All patients (n = 142) | Control (n = 64) | Delirium (n = 78) | Univariate |
|---|---|---|---|---|
| Mean ± SD (%) | Mean ± SD (%) | Mean ± SD (%) | P-value | |
| Preoperative | ||||
| Age (years) | 76.6 ± 4.4 | 75.9 ± 4.2 | 77.2 ± 4.5 | 0.092a |
| Gender (female) | 35.2 | 40.6 | 30.8 | 0.22b |
| Length (m) | 169.1 ± 9.2 | 168.3 ± 9.0 | 169.8 ± 9.4 | 0.32 |
| Weight (kg) | 75.7 ± 13.5 | 72.3 ± 11.8 | 78.4 ± 14.3 | 0.009a |
| BMI | 26.4 ± 4.2 | 25.5 ± 4.0 | 27.1 ± 4.2 | 0.031c |
| NRS pain (0–10) | 1.8 ± 2.1 | 1.4 ± 1.8 | 2.2 ± 2.2 | 0.030a |
| MMSE score (0–30) | 27.0 ± 2.6 | 27.3 ± 2.2 | 26.7 ± 2.9 | 0.18 |
| GDS-15 score (0–15) | 2.5 ± 2.2 | 2.3 ± 2.2 | 2.7 ± 2.2 | 0.26 |
| Type of living (own house) | 56.3 | 62.5 | 51.3 | 0.18 |
| Living condition (single) | 38.7 | 37.5 | 39.7 | 0.78 |
| Tobacco use (active) | 7.7 | 7.8 | 7.7 | 0.98 |
| Hypertension (yes) | 83.8 | 85.9 | 82.1 | 0.53 |
| NYHA (Class IV) | 17.6 | 12.5 | 21.8 | 0.15 |
| Angina (unstable) | 29.8 | 29.7 | 29.9 | 0.98 |
| Platelet inhibitor use (yes) | 82.4 | 87.5 | 78.2 | 0.15 |
| Congestive heart failure (yes) | 21.8 | 17.2 | 25.6 | 0.23 |
| Myocardial infarction (previous) | 40.4 | 42.2 | 39.0 | 0.70 |
| Main stem stenosis (yes) | 21.4 | 23.8 | 19.5 | 0.54 |
| Vessel disease (0–3) | 2.0 ± 1.2 | 2.0 ± 1.2 | 2.0 ± 1.2 | 0.86 |
| Left ventricular function (reduced) | 32.4 | 26.6 | 37.2 | 0.18 |
| Previous cardiac surgery (yes) | 5.7 | 6.3 | 5.1 | 0.76 |
| Previous PCI (yes) | 14.8 | 10.9 | 17.9 | 0.25 |
| Combined surgical procedure (yes) | 20.4 | 12.5 | 26.9 | 0.038a |
| Cerebrovascular history (yes) | 14.8 | 12.5 | 16.7 | 0.49 |
| Sleeping disorder (yes) | 31.0 | 31.3 | 30.8 | 0.95 |
| Pulmonary disease (yes) | 10.6 | 10.9 | 10.3 | 0.90 |
| Diabetes (yes) | 16.2 | 9.4 | 21.8 | 0.052a |
| Renal disease (yes) | 3.5 | 3.1 | 3.8 | 0.82 |
| Reumatic disease (yes) | 5.6 | 3.1 | 7.7 | 0.26 |
| Prostatic disease (yes) | 22.5 | 20.3 | 24.4 | 0.57 |
| Urogenital disease (yes) | 31.0 | 28.1 | 33.3 | 0.50 |
| Gastritis/peptic ulcer (yes) | 12.0 | 6.3 | 16.7 | 0.067a |
| Thyroid disorder (yes) | 7.0 | 3.1 | 10.3 | 0.12 |
| Malignant disease (yes) | 3.5 | 4.7 | 2.6 | 0.50 |
| Infectious disease (yes) | 11.3 | 7.8 | 14.1 | 0.24 |
| SAP (mmHg) | 139.4 ± 20.8 | 140.2 ± 21.0 | 138.7 ± 20.8 | 0.66 |
| DAP (mmHg) | 75.1 ± 10.3 | 76.0 ± 9.9 | 74.3 ± 10.6 | 0.32 |
| Pulse rate (beats/min) | 68.9 ± 13.1 | 69.8 ± 11.9 | 68.1 ± 14.1 | 0.43 |
| Pulse type (not SR) | 7.8 | 9.4 | 6.5 | 0.53 |
| Temperature (°C) | 36.5 ± 0.3 | 36.5 ± 0.3 | 36.4 ± 0.3 | 0.42 |
| Oxygen saturation peripheral (%) | 96.7 ± 2.0 | 97.0 ± 1.6 | 96.4 ± 2.3 | 0.053a |
| Sodium concentration (mmol/l) | 139.5 ± 2.4 | 139.3 ± 2.3 | 139.7 ± 2.5 | 0.33 |
| Potassium concentration (mmol/l) | 4.29 ± 0.30 | 4.27 ± 0.27 | 4.30 ± 0.32 | 0.57 |
| Albumin concentration (g/l) | 42.3 ± 3.6 | 42.3 ± 3.9 | 42.3 ± 3.4 | 0.91 |
| Creatinine concentration (µmol/l) | 84.8 ± 19.8 | 85.9 ± 19.6 | 83.9 ± 20.1 | 0.56 |
| Leucocyte count (109/l) | 7.03 ± 1.81 | 6.91 ± 1.43 | 7.13 ± 2.07 | 0.47 |
| Haemoglobin (g/l) | 135.6 ± 12.6 | 136.0 ± 11.6 | 135.3 ± 13.4 | 0.78 |
| Platelet count (109/l) | 225.6 ± 55.4 | 234.3 ± 57.2 | 218.5 ± 53.3 | 0.096a |
aDenotes those variables tested in multivariable models, with a P-value of <0.10.
bDenotes variables added at multivariable testing due to their expected principal importance rather than its statistical influence at univariate testing. The variable MMSE is shown but is not considered a covariate because of its influence on the diagnosis of delirium. Percent values or mean values ± SDs are shown.
cDenotes variables (P < 0.10) avoided in the multivariable models because of covariability against other used parameters.
BMI: body mass index; NRS: numeric rating scale of pain; MMSE: Mini-Mental State Examination; PCI: percutaneous coronary intervention; GDS: geriatric depression scale; SAP: systolic arterial blood pressure; DAP: diastolic arterial blood pressure; SR: sinus rhythm. P-values refer to univariate logistic regression analyses.
Table 2.
Operative and early postoperative variables
| Parameter | All patients (n = 142) | Control (n = 64) | Delirium (n = 78) | Univariate |
|---|---|---|---|---|
| Mean ± SD (%) | Mean ± SD (%) | Mean ± SD (%) | P-value | |
| At Operation | ||||
| Operation time (h) | 2.89 ± 0.84 | 2.70 ± 0.57 | 3.04 ± 0.99 | 0.020a |
| CPB time (h) | 1.49 ± 1.01 | 1.40 ± 1.29 | 1.56 ± 0.70 | 0.37 |
| Haemoglobin, lowest recorded (g/l) | 87.8 ± 10.7 | 86.9 ± 10.0 | 88.5 ± 11.3 | 0.37 |
| Aortic plaque (presence) | 22.4 | 16.4 | 27.4 | 0.13 |
| Lowest SAP (mmHg) | 76.5 ± 8.6 | 76.3 ± 8.0 | 76.7 ± 9.2 | 0.82 |
| Lowest DAP (mmHg) | 43.2 ± 6.5 | 43.3 ± 5.8 | 43.1 ± 7.1 | 0.86 |
| Lowest oxygen saturation (%) | 96.9 ± 2.1 | 97.2 ± 1.6 | 96.6 ± 2.4 | 0.079a |
| Arrhythmia, treatment required (yes) | 32.4 | 28.1 | 36.0 | 0.32 |
| Blood glucose >10 mM (yes) | 19.5 | 13.6 | 24.6 | 0.12 |
| Insulin infusion required (yes) | 16.7 | 9.5 | 22.7 | 0.045a |
| Tranexamic acid used (yes) | 57.9 | 54.7 | 60.5 | 0.49 |
| Adrenalin required (yes) | 10.0 | 12.5 | 7.9 | 0.37 |
| Milrinone required (yes) | 20.0 | 20.3 | 19.7 | 0.93 |
| Phenylephrine required (yes) | 22.9 | 23.4 | 22.4 | 0.88 |
| Norepinephrine required (yes) | 96.4 | 95.3 | 97.4 | 0.52 |
| Blood products required (yes) | 12.7 | 7.8 | 16.7 | 0.12 |
| Blood loss (l) | 0.46 ± 0.38 | 0.39 ± 0.30 | 0.51 ± 0.43 | 0.079a |
| Diuresis (l) | 0.79 ± 0.37 | 0.74 ± 0.40 | 0.82 ± 0.34 | 0.22 |
| Volume load, blood excluded (l) | 3.73 ± 1.05 | 3.44 ± 0.58 | 3.98 ± 1.26 | 0.003a |
| In the ICU | ||||
| ICU time (h) | 22.4 ± 19.5 | 18.2 ± 5.5 | 25.8 ± 25.4 | 0.013b |
| Ventilator time (h) | 7.42 ± 7.89 | 5.92 ± 2.01 | 8.65 ± 10.36 | 0.005a |
| Lowest SAP (mmHg) | 80.8 ± 12.6 | 80.5 ± 11.3 | 81.0 ± 13.6 | 0.80 |
| Lowest DAP (mmHg) | 42.8 ± 8.3 | 43.4 ± 8.5 | 42.3 ± 8.1 | 0.42 |
| Lowest oxygen saturation (%) | 94.7 ± 2.1 | 95.1 ± 2.1 | 94.3 ± 2.0 | 0.021a |
| Highest temperature recorded (°C) | 37.1 ± 0.5 | 37.0 ± 0.5 | 37.2 ± 0.5 | 0.068a |
| Pulse rate (beats/min) | 81.0 ± 13.4 | 80.9 ± 13.2 | 81.1 ± 13.6 | 0.95 |
| Pulse type (not SR) | 10.6 | 9.4 | 11.5 | 0.95 |
| Bleeding, recorded at 8 h (l) | 0.53 ± 0.32 | 0.51 ± 0.28 | 0.54 ± 0.36 | 0.60 |
| Haemoglobin, lowest recorded (g/l) | 95.0 ± 11.1 | 96.0 ± 11.4 | 94.2 ± 10.8 | 0.34 |
| Blood products required (yes) | 33.8 | 29.7 | 37.2 | 0.35 |
| Sodium concentration (mmol/l) | 138.1 ± 2.4 | 137.6 ± 2.4 | 138.5 ± 2.4 | 0.033a |
| Potassium concentration (mmol/l) | 4.91 ± 0.35 | 4.91 ± 0.36 | 4.92 ± 0.34 | 0.88 |
| Creatinine concentration (mg/l) | 83.0 ± 24.4 | 81.8 ± 25.9 | 84.1 ± 23.3 | 0.57 |
| Leucocyte count (109/l) | 10.9 ± 3.3 | 10.8 ± 3.5 | 11.0 ± 3.1 | 0.75 |
| Haemoglobin (g/l) | 104.0 ± 11.5 | 104.6 ± 13.2 | 103.6 ± 10.1 | 0.61 |
| Platelet count (109/l) | 162.4 ± 43.3 | 168.3 ± 41.6 | 157.6 ± 44.3 | 0.14 |
| Troponin-T (ng/l) | 0.37 ± 0.36 | 0.38 ± 0.40 | 0.37 ± 0.33 | 0.83 |
aDenotes variables tested in multivariable models, with a P-value of <0.10.
bDenotes variables (P < 0.10) avoided in the multivariable models because of covariability against other used parameters. Percent values or mean values ± SD.
CPB: cardiopulmonary bypass; SAP: systolic arterial blood pressure; DAP: diastolic arterial blood pressure; ICU: intensive care unit; SR: sinus rhythm. P-values refer to univariate logistic regression analyses.
Surgery included a variety of procedures and combinations thereof. The procedures were here separated into isolated or combined surgery, with avoidance of too small subgroups. Isolated procedures referred to either coronary artery bypasses grafting or valve replacement/repair. Both aortic and mitral valve procedures were included. All other procedures were categorized as combined. Among the combined procedures, 5 patients had simultaneous intervention of the ascending aorta. One patient became exposed to deep hypothermic arrest and remained included. Redo-cardiac procedures accounted for 8 patients.
The patients were assessed preoperatively and on Day 1 and Day 4 postoperatively. In only 1 of the 142 patients the ventilator time exceeded 24 h. This patient remained eligible for analysis although follow-up was delayed. The median length of postoperative stay was 6 days. Cognition was assessed with the Mini-Mental State Examination (MMSE). The MMSE scale is an interviewer administered scale, with a range from 0 to 30. A score of <24 indicates a notable cognitive impairment and the instrument is associated with good concurred validity [9]. In addition, the Organic Brain Syndrome Scale (OBS) was used. The first subscale of this instrument resembles the MMSE and was disregarded here. The next subscale, sensitive to confusion, is based on observations and interviews of the patient and caregivers. The scale is comprehensive, describing 34 clinical features and is rated on a scale from 0 to 3 (from lack of symptoms to strong manifestations). These features are exemplified by: diurnal cognitive fluctuations, emotional reactions, suspiciousness and delusion, hallucinations, language and speech disturbance, neurological symptoms, spatial disorientation and impaired recognition [10]. The OBS scale was performed together with the MMSE.
Delirium was diagnosed according to the DSM-IV-TR criteria [4] based on the MMSE and OBS-scale recordings. Fluctuations in cognitive status are part of these criteria. With repetitive MMSE screenings, fluctuations in cognitive status are monitored and evaluated [11]. Moreover, the OBS scale is an established instrument in these perspectives [10]. Their combined use (MMSE and OBS scale) has been found valid in previous studies regarding delirium [6, 10].
All assessments in the study were done by two trained research nurses. For delirium diagnosis, two senior experts in psycho-geriatric medicine independently analysed the two instruments vs the DSM-IV-TR criteria. Patients diagnosed with delirium were subgrouped into those with hyper-, hypoactive and mixed profiles. It was not possible to subgroup some of the delirious patients by these characteristics. Nevertheless, in this study, delirium was analysed collectively regardless of subgroup characteristics.
Additional scoring instruments were used. Pain was assessed by the Numerical Rating Scale (NRS, range 0–10, low to high pain) [12]. Depression was evaluated by the Geriatric Depression Scale (GDS)-15 with higher scores indicating more depressive symptoms [13]. Most of the underlying variables of EuroSCORE-I [14] were considered separately rather than using the score value.
Statistical methods
Extracted data were tabulated using Microsoft Excel. Variables were reviewed for normality, outliers and dependencies. For variables with obvious co-variability, one was selected on the basis of its assumed higher clinical relevance. For instance, CPB time was preferred rather than aortic cross-clamp time. Also, weight was used rather than body mass index because of its higher predictive value in the analyses. Variables were tested against delirium by means of univariate and multivariable logistic regression. Continuous variables were generally used in their numeric mode rather than being categorized. Non-conformity to linearity was considered in this respect. Also, co-linearity between variables vs delirium was reviewed and considered. In view of the surplus of information in relation to the cohort size, the inclusion to multivariable testing was restricted to variables associated with delirium and a P-value of < 0.10. Apart from this rule, gender was added for its assumed principal importance. The process followed a manual backward conditional approach, with forward testing as control. Missing data were few and accounted for only 80 of 12 698 recordings. For these, case-wise deletion was applied.
Preoperative variables were separately analyzed from those describing the intra- and early postoperative period distinguishing predisposing and precipitating risk factors. The two groups of variables were also run together in a multivariable model. The extracted independent risk factors were applied on the cohort for analysis of their explanatory strength. The probability of developing delirium was calculated and interpreted based on a cut-point of 0.50. Their accuracy was evaluated by receiver operating characteristics (ROCs).
A P-value of <0.05 was regarded as statistically significant. Numeric variables are reported as mean values and standard deviations (SDs). The Statistical Package for Social Sciences version 18 was used (IBM SPSS Statistics, IBM, Inc., Chicago, IL, USA).
RESULTS
In total, 78/142 (54.9%) of the patients were diagnosed with delirium postoperatively, based on the DSM-IV-TR criteria. Delirium was divided into subprofiles: hypoactive (n = 56/78), hyperactive (n = 4/78), mixed (n = 4/78). The remaining patients were non-classifiable (n = 14/78). Risk-factor analyses were not conducted on subgroup levels.
Patient characteristics for predisposing and precipitating variables, respectively, are given in Tables 1 and 2. These tables also describe the univariate results with respect to delirium and the variables of interest for multivariable testing are indicated to be further listed in Table 3. In multivariable logistic regression, the following predisposing variables were found independently associated with delirium: preoperative pain score on NRS, diabetes, oxygen saturation and combined surgery. These variables had about the same statistical influence (i.e. Wald) in predicting postoperative delirium. The precipitating variables were separately analysed to expose: volume load during operation, postoperative ventilator time and plasma sodium concentration in the ICU. Among these, the volume load during operation had the strongest predict influence.
Table 3.
Logistic regression analyses
| Variable (unit) | Univariate |
Multivariable |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| P-value | Wald | OR | CI low | CI high | P-value | Wald | OR | CI low | CI high | |
| Predisposing factors | ||||||||||
| Age (years) | 0.092 | 2.84 | 1.07 | 0.99 | 1.16 | |||||
| Gender (female) | 0.22 | 1.49 | 0.65 | 0.32 | 1.30 | |||||
| Weight (kg) | 0.009 | 6.76 | 1.04 | 1.01 | 1.06 | |||||
| NRS pain (0–10) | 0.030 | 4.69 | 1.21 | 1.02 | 1.43 | 0.042 | 4.12 | 1.20 | 1.01 | 1.44 |
| Diabetes (yes) | 0.052 | 3.79 | 2.69 | 0.99 | 7.31 | 0.029 | 4.78 | 3.24 | 1.13 | 9.32 |
| Gastritis/peptic ulcer (yes) | 0.067 | 3.36 | 3.00 | 0.93 | 9.71 | |||||
| Oxygen saturation peripheral (%) | 0.053 | 3.74 | 0.83 | 0.70 | 1.00 | 0.045 | 4.03 | 0.82 | 0.67 | 1.00 |
| Platelet count (109/l) | 0.096 | 2.76 | 0.99 | 0.99 | 1.00 | |||||
| Combined surgical procedure (yes) | 0.038 | 4.31 | 2.58 | 1.05 | 6.30 | 0.024 | 5.08 | 2.98 | 1.15 | 7.70 |
| Precipitating factors | ||||||||||
| At operation | ||||||||||
| Operation time (h) | 0.020 | 5.39 | 1.68 | 1.08 | 2.59 | |||||
| Lowest oxygen saturation (%) | 0.079 | 3.08 | 0.85 | 0.72 | 1.02 | |||||
| Insulin infusion required (yes) | 0.045 | 4.03 | 2.78 | 1.02 | 7.57 | |||||
| Blood loss (l) | 0.079 | 3.09 | 2.85 | 0.89 | 9.17 | |||||
| Volume load (blood excluded) (l) | 0.003 | 8.81 | 2.08 | 1.28 | 3.39 | 0.003 | 8.78 | 2.19 | 1.30 | 3.67 |
| In the ICU | ||||||||||
| Ventilator time (h) | 0.005 | 8.04 | 1.23 | 1.07 | 1.42 | 0.027 | 4.92 | 1.20 | 1.02 | 1.41 |
| Lowest oxygen saturation (%) | 0.021 | 5.31 | 0.82 | 0.69 | 0.97 | |||||
| Highest temperature recorded (°C) | 0.068 | 3.32 | 1.88 | 0.95 | 3.73 | |||||
| Sodium concentration (mmol/l) | 0.033 | 4.55 | 1.17 | 1.01 | 1.35 | 0.043 | 4.09 | 1.17 | 1.00 | 1.37 |
| Combined predisposing and precipitating factors | ||||||||||
| Age (years) | 0.036 | 4.39 | 1.10 | 1.01 | 1.21 | |||||
| Diabetes (yes) | 0.032 | 4.58 | 3.49 | 1.11 | 10.99 | |||||
| Gastritis/peptic ulcer (yes) | 0.050 | 3.83 | 4.00 | 1.00 | 16.06 | |||||
| Volume load during operating theatre (blood excluded) (l) | 0.001 | 10.71 | 2.77 | 1.51 | 5.11 | |||||
| Ventilator time in ICU (h) | 0.042 | 4.14 | 1.20 | 1.01 | 1.42 | |||||
| Highest temperature recorded in ICU (°C) | 0.044 | 4.06 | 2.23 | 1.02 | 4.85 | |||||
| Sodium concentration in ICU (mmol/l) | 0.038 | 4.30 | 1.19 | 1.01 | 1.41 | |||||
NRS: numeric rating scale of pain; ICU: intensive care unit; OR: odds ratio; CI: confidence interval ± 95%.
A somewhat different model was obtained when the predisposing and precipitating variables were collectively analysed (Table 3). In this model diabetes, ventilator time, sodium concentration and volume load during operation remained independently associated with postoperative delirium, together with age and early postoperative temperature. The variable peptic ulcer showed a borderline significance in this model. When this unexpected variable was removed, the model remained essentially unchanged with only a modest decrease in explanatory strength. The highest predictive influence in the model was obtained from the variable volume load during operation.
In Table 4, the statistical results are shown for the various models applied on the cohort. All models (e.g. predisposing, precipitating and combined) were highly significant. Nevertheless, the model based on precipitating variables gave a somewhat better explanatory strength than that based on predisposing factors. The strength increases when both predisposing and precipitating factors were collectively considered in the model. This was illustrated by the Nagelkerke R2 value explaining 34.6% of the variance. The corresponding ROC curves are shown in Fig. 1 with their areas under curve listed in Table 4.
Table 4.
Logistic models applied on cohort
| Predisposing | Precipitating | Combined | |
|---|---|---|---|
| Valid cross-matched observations (n) | 140 | 141 | 141 |
| Sensitivity to correctly predict (%) | 69.7 | 71.4 | 74.0 |
| Specificity to correctly predict (%) | 57.8 | 62.5 | 71.9 |
| Positive predictive value (%) | 66.3 | 69.6 | 76.0 |
| Negative predictive value (%) | 61.7 | 64.5 | 69.7 |
| Wald | 15.1 | 19.5 | 30.2 |
| P-value | <0.001 | <0.001 | <0.001 |
| Nagelkerke R2 | 0.156 | 0.214 | 0.346 |
| Hosmer and Lemeshow P-value | 0.998 | 0.963 | 0.803 |
| ROC area under curve | 0.695 | 0.729 | 0.802 |
ROC: receiver operating characteristic.
Figure 1.
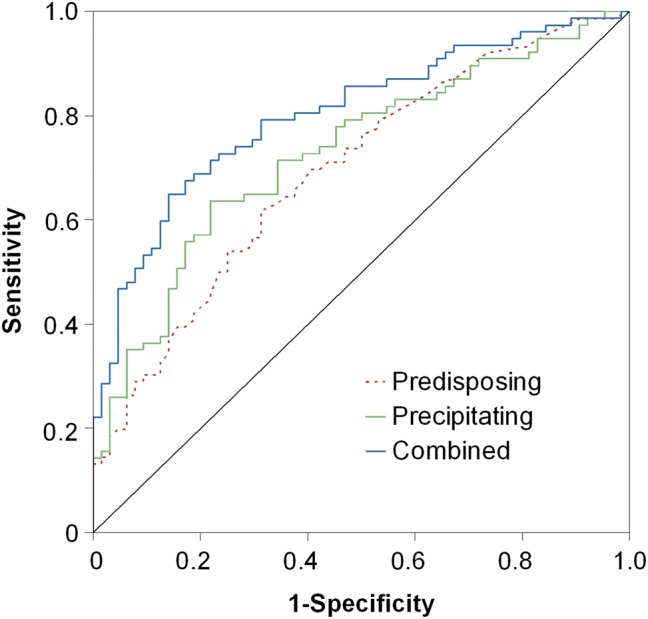
ROCs of the tested multivariable models. See text for further details.
DISCUSSION
Delirium was diagnosed in 55% of the patients, 70 years and older undergoing consecutive routine cardiac surgery. Both predisposing and precipitating factors contributed to delirium. However, when predisposing and precipitating were combined, the predictive strength of the model increased notably with more than one-third of the variance explained. In overview, our study confirmed many of the previously suggested risk factors. In addition and of great interest in our study, the variable volume load during the operation was found to be a dominant factor, not previously identified.
The incidence of delirium was higher in our report than in most other studies [7, 15–18]. Partly, this finding may reflect our careful and comprehensive cognitive testing being performed both before and repeatedly after the operation. Studies not using cognitive tests usually report a much lower incidence rate, since many patients with hypoactive delirium are likely to have escaped detection [15, 17, 18]. Also, our observational period of delirium included four postoperative days being longer than in most other studies [7, 18]. A third factor that may have contributed to our results was the selection of older patients and inclusion of surgical procedures other than isolated coronary bypass.
The variable volume load during the operation was strongly associated with postoperative delirium. This variable added together infusions administered in the operating theatre for anaesthetic and CPB purposes. Blood transfusions were separately analysed and blood products had no independent influence on delirium. On average, each patient was given 3.7 l of fluids. The difference between delirious and control patients was small in numeric terms, but the variable was associated with the highest predictive influence. Per litre of extra volume, the risk of developing delirium increased nearly 3-fold. An association between volume load and delirium has not been previously reported. However, Bucerius et al. [5] observed that patients exposed to intraoperative haemofiltration showed an increased risk of postoperative delirium. Moreover, they also reported that patients exposed to beating heart coronary bypass surgery were protected against delirium, implying a mechanistic role of CPB. This comparison must be considered with care because in their study no cognitive testing was performed and their reported incidence rate of delirium was only 8.4% [5].
A high sodium concentration in the first postoperative morning predicted delirium, independently from that of an increased volume load during surgery. The two variables showed no statistical correlation, an observation that talks against an electrolyte disturbance being the result of intraoperative infusions given. The association between sodium concentration and delirium is previously identified [19]. The interpretation regarding sodium in our study is complex because none of the patients was hypernatremic by definition. It must also be brought to mind that both intraoperative volume load and sodium concentrations in the ICU may be surrogate variables for unknown factors. Nevertheless, our study used a wide range of analysed variables which counteracts this potential error.
Additional variables with relevance to delirium were identified. In brief, diabetes increased the risk of delirium 3.5 times, which finds support in previous literature [5, 20]. Age is another well-known risk factor behind delirium [15, 18]. In our study, the risk of developing delirium increased 10% per extra year of age. Here only older patients were analysed, 70 years of age and older. Despite this restrained selection of older patients, age remained independently associated with delirium in this cohort. The selection may also explain the high incidence rate of delirium, compared with many previous studies.
Among the precipitating factors, a prolonged ventilator time was associated with delirium. This observation supports previous suggestions [15]. The risk of delirium increased ∼20% per each extra hour of ventilation. Nevertheless, the variable is complex and a prolonged ventilator time may reflect an underlying cause (e.g. comorbidities, anaesthetic managements or complications at surgery). Also, the variable is bias from local ICU routines (e.g. extubation protocols and differences between individual care givers). Moreover, some studies have reversed the causality to explain a prolonged ventilator time as a result of delirium rather than the other way around [15, 18]. An increased body temperature in the early postoperative period was associated with delirium. Our observation finds scattered support in the literature [21] and is not assumed to reflect an infectious disease, being too early after surgery. Infection is otherwise a well-known trigger of delirium [22]. In contrast to our finding, a low intraoperative body temperature has also been found relevant [16, 19]. Intraoperative temperatures were not recorded in our study. However, the cooling during CPB interferes with this issue with a low CPB temperature reflecting a complex and long-duration procedure probably being more important than the temperature as such. An unexpected finding in our study was that patients reporting gastritis and/or peptic ulcer problems had an increased risk of delirium. This observation showed a borderline significance and must be considered with caution. The multivariable model was also tested without this variable included without affecting the results notably.
This study reports the results from consecutive older patients undergoing cardiac surgery. The study was based on comprehensive assessments including cognitive testing both before and repeatedly after surgery. All assessments were performed by two trained research nurses. Similarly, a large number of variables were systematically extracted for analysis, pre-, intra- and early postoperatively. Unfortunately, pharmacological interactions were not explored. Our study is also limited from its relatively small sample size in relation to the surplus of variables analysed. Therefore, our findings should be validated in future studies. Certainly, contributing factors behind delirium are to be sought among a variety of factors beyond those tested in our study, for example, inflammatory and embolic mechanisms. Also, our results are valid only for the cohort studied of older patients during their period of hospitalization.
In conclusion, delirium was common among older patients undergoing cardiac surgery. Both predisposing and precipitating factors contributed to delirium and it is potentially possible to modify several of these factors in daily clinical practice. The strongest precipitating factor for delirium was an increased volume load during operation. An association between delirium and volume load has not been previously identified, a detail that it may be possible to investigate in a randomized study.
Funding
This work was supported by grants from the Heart Foundation of Northern Sweden; the Erik and Anne-Marie Detlof's Foundation; the Dementia foundation, the Borgerskapet in Umeå Research Foundation; the Medical Faculty at Umeå University Sweden; the University of Umeå; the County Council of Västerbotten, Sweden, and the Strategic Research Programme in Care Sciences, Sweden.
Conflict of interest: none declared.
Acknowledgements
The authors acknowledge the participants and the staff at the Cardiothoracic Surgery Department Heart Center University Hospital of Umeå, Sweden, for their cooperation in this study. The authors also appreciate Fredrik Jonsson for statistical review of our study.
REFERENCES
- 1.Blachy PH, Starr A. Post-cardiotomy delirium. A J Psychiatry. 1964;121:371–5. doi: 10.1176/ajp.121.4.371. [DOI] [PubMed] [Google Scholar]
- 2.Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med. 1996;335:1857–63. doi: 10.1056/NEJM199612193352501. [DOI] [PubMed] [Google Scholar]
- 3.Newman MF. Open heart surgery and cognitive decline. Cleve Clin J Med. 2007;74(Suppl 1):S52–5. doi: 10.3949/ccjm.74.suppl_1.s52. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th edn. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 5.Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Falk V, et al. Predictors of delirium after cardiac surgery delirium: effect of beating-heart (off-pump) surgery. J Thorac Cardiovasc Surg. 2004;127:57–64. doi: 10.1016/s0022-5223(03)01281-9. [DOI] [PubMed] [Google Scholar]
- 6.Eriksson M, Samuelsson E, Gustafson Y, Aberg T, Engstrom KG. Delirium after coronary bypass surgery evaluated by the organic brain syndrome protocol. Scand Cardiovasc J. 2002;36:250–5. doi: 10.1080/14017430260180436. [DOI] [PubMed] [Google Scholar]
- 7.Rudolph JL, Jones RN, Levkoff SE, Rockett C, Inouye SK, Sellke FW, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119:229–36. doi: 10.1161/CIRCULATIONAHA.108.795260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koster S, Hensens AG, Schuurmans MJ, van der Palen J. Risk factors of delirium after cardiac surgery A systematic review. Eur J Cardiovasc Nurs. 2011;10:197–204. doi: 10.1016/j.ejcnurse.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 9.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Jensen E, Dehlin O, Gustafson L. A comparison between three psychogeriatric rating scales. Int J Geriatr Psychiatry. 1993;8:215–29. [Google Scholar]
- 11.O'Keeffe ST, Mulkerrin EC, Nayeem K, Varughese M, Pillay I. Use of serial Mini-Mental State Examinations to diagnose and monitor delirium in elderly hospital patients. J Am Geriatr Soc. 2005;53:867–70. doi: 10.1111/j.1532-5415.2005.53266.x. [DOI] [PubMed] [Google Scholar]
- 12.Breivik EK, Bjornsson GA, Skovlund E. A comparison of pain rating scales by sampling from clinical trial data. Clin J Pain. 2000;16:22–8. doi: 10.1097/00002508-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–73. [Google Scholar]
- 14.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16:9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 15.Norkiene I, Ringaitiene D, Misiuriene I, Samalavicius R, Bubulis R, Baublys A, et al. Incidence and precipitating factors of delirium after coronary artery bypass grafting. Scand Cardiovasc J. 2007;41:180–5. doi: 10.1080/14017430701302490. [DOI] [PubMed] [Google Scholar]
- 16.Detroyer E, Dobbels F, Verfaillie E, Meyfroidt G, Sergeant P, Milisen K. Is preoperative anxiety and depression associated with onset of delirium after cardiac surgery in older patients? A prospective cohort study. J Am Geriatr Soc. 2008;56:2278–84. doi: 10.1111/j.1532-5415.2008.02013.x. [DOI] [PubMed] [Google Scholar]
- 17.Gottesman RF, Grega MA, Bailey MM, Pham LD, Zeger SL, Baumgartner WA, et al. Delirium after coronary artery bypass graft surgery and late mortality. Ann Neurol. 2010;67:338–44. doi: 10.1002/ana.21899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stransky M, Schmidt C, Ganslmeier P, Grossmann E, Haneya A, Moritz S, et al. Hypoactive delirium after cardiac surgery as an independent risk factor for prolonged mechanical ventilation. J Cardiothorac Vasc Anesth. 2011;25:968–74. doi: 10.1053/j.jvca.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 19.Giltay EJ, Huijskes RV, Kho KH, Blansjaar BA, Rosseel PM. Psychotic symptoms in patients undergoing coronary artery bypass grafting and heart valve operation. Eur J Cardiothorac Surg. 2006;30:140–7. doi: 10.1016/j.ejcts.2006.03.056. [DOI] [PubMed] [Google Scholar]
- 20.Mu DL, Wang DX, Li LH, Shan GJ, Li J, Yu QJ, et al. High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: a prospective cohort study. Crit Care. 2010;14:R238. doi: 10.1186/cc9393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sadler PD. Incidence, degree, and duration of postcardiotomy delirium. Heart Lung. 1981;10:1084–92. [PubMed] [Google Scholar]
- 22.Laurila JV, Laakkonen ML, Tilvis RS, Pitkala KH. Predisposing and precipitating factors for delirium in a frail geriatric population. J Psychosom Res. 2008;65:249–54. doi: 10.1016/j.jpsychores.2008.05.026. [DOI] [PubMed] [Google Scholar]


