Abstract
Despite the advances in video-assisted thoracoscopic surgery (VATS), vascular reconstruction of the pulmonary artery (PA) is still infrequently performed by thoracic surgeons because of the technical difficulties and the increased operative risk during thoracoscopy. The few published reports have been performed by using 3–4 incisions. We present the first report of a pulmonary artery reconstruction procedure performed by a single-incision VATS technique. A 73-year old male patient was operated on by the thoracoscopic approach through a single 4-cm incision with no rib spreading. The postoperative recovery was uneventful.
Keywords: Thoracoscopy/video-assisted thoracoscopic surgery, Minimally invasive surgery, Pulmonary artery reconstruction, Vasculoplasty, Vascular reconstruction, Surgery/incisions/technique
INTRODUCTION
In the past two decades, video-assisted thoracoscopic surgery (VATS) has been performed with increasing frequency for lung cancer treatment. However, advanced cases are actually performed in only a few centres. Most surgeons use a 3-4 incision VATS for complex resections such as bronchial or vascular sleeves. This report describes the technique for a left upper lobectomy with vascular reconstruction by using a uniportal VATS technique.
CLINICAL SUMMARY
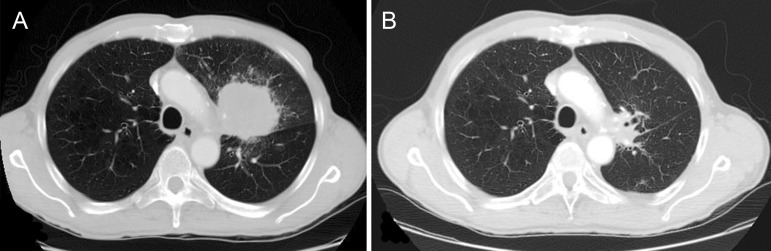
A 73-year old male, smoker, with no other comorbidities was diagnosed with a 7.2 cm left upper lobe large-cell carcinoma with vascular involvement (Fig. 1A). The patient was diagnosed with stage IIIB non-small-cell lung cancer and received cisplat-in based chemotherapy and high doses of radiotherapy (66 Gy). After showing good response (Fig. 1B), the patient was recommended for surgery.
Figure 1:
(A) CT-scan before induction treatment. (B) CT-scan after induction chemoradiotherapy.
SURGICAL TECHNIQUE
Under general anaesthesia, a VATS approach using a 5-cm single-incision was made in the fifth intercostal space with no rib spreading (no soft tissue retractor and no direct vision).
After digital palpation, a mass was confirmed in the upper lobe. Surgery was begun by dissecting and dividing the superior pulmonary vein. The fissure was divided from anterior to posterior from the hilum. The bronchus was dissected and then transected by using a TA™ stapler and a long knife. The arterial branches for the upper lobe were involved by the mass, and dissection was not possible. The main pulmonary artery (PA) and the interlobar artery were dissected to gain adequate proximal and distal vascular control. Before clamping of the PA, 5000 units of heparin were injected intravenously to prevent clotting. The main PA and interlobar artery were occluded by placement of thoracoscopic clamps. Both clamps were placed towards the anterior portion of the incision to facilitate the instrumentation for vascular reconstruction. The camera was located in the posterior part of the incision, and the instrumentation was inserted between the camera and the clamps (Fig. 2A).
Figure 2:
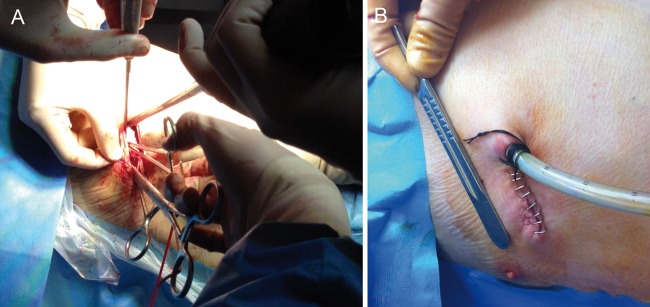
(A) Surgical image of instrumentation during vascular reconstruction. (B) Postoperative result with chest tube placed in the posterior part of the incision.
The PA was transected laterally (Supplementary Video 1) and the defects in the truncus anterior and interlobar artery were repaired by using direct, lateral, continuous 4-0 monofilament non-absorbable sutures. The sutures were tied and the air was released through one of the apical branches, which was then closed by using a vascular clip (Click aV, Grena®) (Supplementary Video 2).
Supplementary video 1:
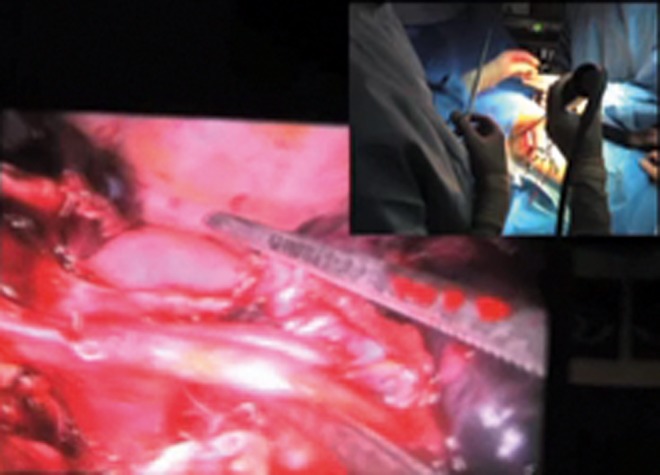
Vascular resection.
Supplementary video 2:
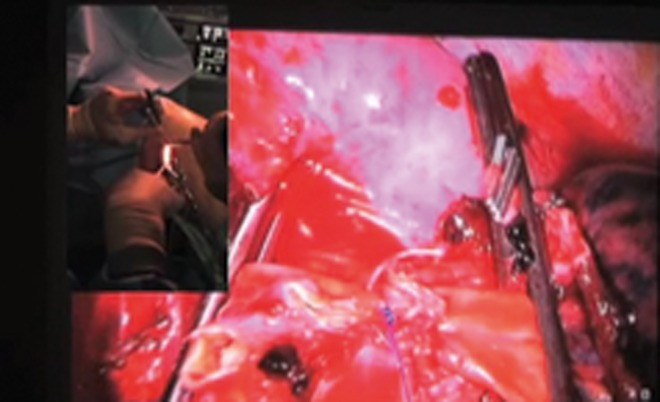
Vascular reconstruction.
The specimen was then removed in a protective bag. Systematic lymph node dissection was then performed to complete the procedure and a single chest tube was placed (Fig. 2B). Total surgery time was 230 min and estimated blood loss was 150 ml. The patient was discharged on the 14th postoperative day. The extended stay was due to a postoperative air leak.
The pathological examination revealed complete tumour regression (Junker Grade III classification) with no lymph node involvement. The patient was doing well 6 months after the operation with no signs of tumour recurrence. A control CT scan showed good calibre of the left PA with no stenosis.
DISCUSSION
Thoracoscopic major lung resection for advanced lung cancer stages is now gaining wide acceptance worldwide [1]. However, lobectomy requiring vasculoplasty remains a contraindication for the VATS approach, even for experienced thoracoscopic surgeons.
The main reason is because vascular resection and reconstruction is a complex procedure even when performed by thoracotomy. The fear of a vascular accident during thoracoscopy as well as the technical difficulties for an optimal vascular reconstruction are the main concerns.
With recent technical advances in VATS lobectomy (instruments and HD cameras) and the experience gained in the treatment of a large number of patients, these complex procedures can be performed by thoracoscopy. As our own experience has grown with the uniportal VATS technique, our list of contraindications to VATS has been reduced [2]. Advanced procedures such as uniportal sleeve lobectomy [3] or chest wall resection have already been published with good postoperative outcomes.
However, there are very few articles published in the literature describing thoracoscopic vascular reconstruction. The published cases are performed by using 3-4 incisions, and the additional incisions are mainly used for the insertion of vascular clamps [4].
The success in performing complex lobectomies by the uniportal approach is a result of skills and experience accumulated over time from performing many uniportal VATS surgeries [2]. The advantage of uniportal VATS surgery is that the vision is direct to the target tissue, providing a similar angle of view as for open surgery. Conventional multiport VATS triangulation creates a new optical plane with a genesis of the torsional angle that is not favourable, with standard two-dimension monitors. Another advantage of the uniportal VATS technique is that the instruments inserted parallel to the videothoracoscope mimic the chest manoeuvres performed during open surgery. These geometric uniportal VATS concepts help the vascular reconstruction in complex resections such as the one described in this article.
The use of thoracoscopic instruments with proximal and distal articulation (Scanlan International, Inc., St. Paul, MN, USA) facilitates this uniportal surgery, particularly for clamping the PA with no interference with the instrumentation used for the vascular reconstruction. That is because the clamps were placed in the anterior portion of the incision and the instrumentation was inserted above the clamps.
A lobectomy with resection and reconstruction of the PA allows patients to preserve the functioning pulmonary tissue. This is particularly important in patients receiving induction chemoradiotherapy in whom the performance of a pneumonectomy would increase the rate of postoperative complications. The presence of complete tumour regression after surgery is associated with better long-term outcomes [5].
Despite the increasing adoption of the uniportal VATS approach worldwide, the technique for advanced procedures such as vascular reconstruction should be performed only by experienced VATS surgeons.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Conflict of interest: none declared.
REFERENCES
- 1.Hennon M, Sahai RK, Yendamuri S, Tan W, Demmy TL, Nwogu C. Safety of thoracoscopic lobectomy in locally advanced lung cancer. Ann Surg Oncol. 2011;18:3732–6. doi: 10.1245/s10434-011-1834-9. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez-Rivas D, Paradela M, Fernandez R, Delgado M, Fieira E, Mendez L, et al. Uniportal video-assisted thoracoscopic lobectomy: two Years of experience. Ann Thorac Surg. 2013;95:426–32. doi: 10.1016/j.athoracsur.2012.10.070. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Rivas D, Fernandez R, Fieira E, Rellan L. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg. 2013;145:1676–7. doi: 10.1016/j.jtcvs.2013.02.052. [DOI] [PubMed] [Google Scholar]
- 4.Nakanishi R, Yamashita T, Oka S. Initial experience of video-assisted thoracic surgery lobectomy with partial removal of the pulmonary artery. Interact CardioVasc Thorac Surg. 2008;7:996–1000. doi: 10.1510/icvts.2008.184564. [DOI] [PubMed] [Google Scholar]
- 5.Maurizi G, D'Andrilli A, Anile M, Ciccone AM, Ibrahim M, Venuta F, et al. Sleeve lobectomy compared with pneumonectomy after induction therapy for non-small-cell lung cancer. J Thorac Oncol. 2013;8:637–43. doi: 10.1097/JTO.0b013e318286d145. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.