Abstract
Objective
This 15-year follow-up assessed the effects of a preventive intervention for divorced families, the New Beginnings Program (NBP), versus a literature control condition (LC).
Method
Mothers and their 9-to-12-year olds (N= 240 families) participated in the trial. Young adults (YAs) reported on their mental health and substance-related disorders, mental health and substance use problems, and substance use. Mothers reported on YA's mental health and substance use problems. Disorders were assessed over the past 9 years (since previous follow-up) and 15 years (since program entry). Alcohol and marijuana use, other substance use and polydrug use, and mental health problems and substance use problems were assessed over the past month, past year and past six months, respectively.
Results
YAs in NBP had a lower incidence of internalizing disorders in the past nine (7.55% versus 24.4%; Odds Ratio [OR] =.26) and 15 years (15.52% versus 34.62%; OR =.34) and a slower rate of onset of internalizing symptoms associated with disorder in the past nine (hazard ratio [HR] =.28) and 15 years (HR =.46). NBP males had a lower number of substance-related disorders in the past nine years (d=.40), less polydrug (d=.55) and other drug use (d=.61) in the past year and fewer substance use problems (d=.50) in the past six months than LC males. NBP females used more alcohol in the past month (d=.44) than LC females.
Conclusions
NBP reduced the incidence of internalizing disorders for females and males and substance-related disorders and substance use for males.
Keywords: Divorce, Prevention, Young Adults, Mental Health, Substance Use
Introduction
Although the rate of divorce in the U.S. has stabilized or decreased somewhat since the 1970s (Bramlett & Mosher, 2002; U.S. Census Bureau, 2005), it is estimated that 30 to 50% of youth in the United States will experience parental divorce in childhood or adolescence (National Center for Health Statistics, 2008). Although most youths do not experience significant adjustment problems after parental divorce (e.g., Amato, 2001; Hetherington, 1999), there is compelling evidence demonstrating that divorce confers increased risk for multiple problems in childhood and adolescence, including mental health problems and disorders (e.g., Amato, 2001; Fergusson, Horwood & Lynskey, 1994), elevations in substance use (e.g., (Eitle, 2006; Paxton, Valois, & Drane, 2007), early onset of sexual activity (Hetherington, 1999) and physical health problems (Troxel & Matthews, 2004). For a sizeable subgroup, the negative effects of parental divorce continue into adulthood. Multiple prospective studies with epidemiologic samples have shown that parental divorce is associated with substantial increases in clinical levels of mental health problems, substance abuse, mental health service use, and psychiatric hospitalization in adulthood (e.g., Afifi, Boman, Fleisher & Sareen, 2009; Kessler, Davis & Kendler,1997). Illustratively, in the National Comorbidity Study, Kessler et al. (1997) found that parental divorce was related to elevated rates of multiple mental (odds ratios [OR] range = 1.39-2.61) and substance-related (OR range=1.46-2.38) disorders, controlling for demographics including age, sex, race, and family SES. Similarly, Chase-Lansdale, Cherlin and Kiernan (1995) reported a 39% increase in the odds of being above the clinical cut-point on mental health problems at age 23 as a function of parental divorce, controlling for pre-divorce emotional problems, school achievement and SES.
Because of the high prevalence of divorce and its association with multiple problem outcomes, divorce has a considerable impact on population rates of youth and adult problems (Scott, Mason, & Chapman, 1999). The population attributable risk (PAR; the proportion of an outcome in the population due to a risk factor or percent of cases that could be prevented by removing the factor or its consequences) provides an important perspective on the public health significance of preventive interventions for this at-risk group. Illustratively, using data from a nationally representative survey of adults (Kessler, Davis, & Kendler, 1997), and controlling for demographics, prior disorders, and adversities, the PAR of parental divorce for drug dependence is 23% (OR=1.73). Given these data, the development and evaluation of interventions for youths in divorced families have clear public health significance.
To date, several randomized experimental trials of programs for either youths or parents from divorced families have shown positive short-term effects on youths’ mental health outcomes (Braver, Griffin, & Cookston, 2005; Forgatch & DeGarmo, 1999; Pedro-Carroll & Cowen, 1985; Stolberg & Garrison, 1985; Wolchik, Sandler, Weiss, & Winslow, 2007; Wolchik, et al., 2000; Wolchik, et al., 1993). Further, some studies have documented maintenance of these effects two to nine years following program completion, with a few demonstrating program effects when youths were in mid-to-late adolescence (DeGarmo & Forgatch, 2005; DeGarmo, Patterson, & Forgatch, 2004; Forgatch, Patterson, DeGarmo, & Beldavs, 2009; Pedro-Carroll, Sutton, & Wyman, 1999; Stolberg & Mahler, 1994). However, two limitations of these follow-up evaluations are notable. First, none have examined program effects on measures of onset (i.e., incidence) of mental health or substance-related disorders subsequent to participation in the intervention. Second, none examined the impact of prevention programs delivered in childhood on outcomes when the offspring are young adults. Examining the effects of prevention programs on the incidence of mental health and substance-related disorders in young adulthood is an important indicator of long-term prevention effects because it has been found that 75% of lifetime cases of such disorders have their onset by age 24 (Kessler, Berglund, Demler, Jin, & Walters, 2005). Illustratively, several of the mental disorders that are associated with parental divorce and have significant public health burden, such as depression and substance-related disorders, have a median age of onset (Burke, Burke, Regier, & Rae, 1990) and/or increase or peak in prevalence during this stage (e.g., Kessler et al., 2005). Further, research has consistently shown that young adulthood is a period when individual trajectories related to psychopathology become more firmly established so that having a mental disorder in young adulthood has implications for both concurrent and future functioning (e.g., Arnett & Tanner, 2006). For example, chronic, heavy substance use in young adulthood is associated with current and future mental health and physical health difficulties, criminal behavior and antisocial personality disorders (Arnett & Tanner, 2006).
Assessment of whether the effects of preventive interventions last into young adulthood is also interesting from a theoretical perspective. Prevention programs are designed to modify social environmental risk and protective factors as well as individual-level competencies and problems. The underlying theory is that changing these risk and protective factors will impact the development of problems and disorder at later developmental periods (Coie et al., 1993; NRC/IOM, 2009). Because 75% of mental disorders have their onset by young adulthood, testing the long-term mental health and substance use outcomes in young adulthood of a preventive intervention delivered in childhood provides a stringent test of this theoretical proposition (NCR/IOM, 2009).
This article reports on a 15-year follow-up in young adulthood of a randomized controlled trial that compared a parenting program for divorced mothers, a dual-component program consisting of the program for mothers and a child coping program, and a literature control condition that were provided when the youths were between ages 9 and 12 (Wolchik et al., 2000). The underlying conceptual model of the program is based on elements from a person-environment transactional framework and a risk and protective factor model. In transactional models, aspects of the social environment affect the development of problems and competencies in an individual, which in turn influence the social environment and development of competencies and problems at later developmental stages (e.g., Sameroff, 2000). Derived from epidemiology (Institute of Medicine, 1994), the risk and protective factor model posits that the likelihood of mental health problems is affected by exposure to risk factors and the availability of protective resources. Cummings et al.'s (2000) “cascading pathway model” integrates these two models into a developmental framework. From this perspective, stressful events, such as divorce, can lead to an unfolding of failures to resolve developmental tasks and increase susceptibility to mental health problems and impaired competencies. Parenting is viewed as playing a central role in facilitating children's successful adaptation, and the skills and resources that are developed in successful resolution of developmental tasks, such as effective coping and academic success, are viewed as important tools when youths face challenges in subsequent developmental periods.
Prior research has shown: a) positive effects of the parenting program vs. the literature control condition on externalizing problems at posttest and 6-month follow-up (Wolchik et al., 2000), b) positive effects of the parenting program vs. the literature control condition and the dual-component condition vs. the literature control condition on multiple mental health and substance use outcomes, including mental disorder, at the six-year follow-up (Wolchik et al., 2002); and c) no difference in the effects of the parenting program and the dual-component program on mental health outcomes at posttest, 6-month or six-year follow-up (Wolchik et al., 2002; Wolchik et al., 2007; Wolchik et al., 2000). Mediational analyses indicated that improvements in mother-child relationship quality at posttest accounted for program-induced effects on increased coping efficacy and active coping as well as reduced internalizing and externalizing problems for those with high baseline risk for maladjustment at the six-year follow-up. In addition, improvements in effective discipline at posttest accounted for program-induced effects on reduced externalizing problems at the six-month follow-up and higher GPA at the six-year follow-up (Tein, Sandler, MacKinnon, & Wolchik, 2004; Zhou, Sandler, Millsap, Wolchik, & Dawson-McClure, 2008).
The current study examined program effects on the incidence of mental health and substance-related disorders; levels of internalizing, externalizing and substance use problems; and frequency of substance use 15 years after participation. Mental health and substance-related disorders were assessed in two ways. First, the incidence of disorder with onset during the nine year period since the last follow-up assessment, which occurred six years after program completion, was assessed. Developmentally, this measure represents disorders that have their onset during mid-adolescence to young adulthood. Second, the incidence of mental health and substance-related disorders with onset since program entry (i.e., during the last 15 years) was assessed. The nine-year interval was used so that program effects on incidence of disorder would be distinct from previously reported findings at the six-year follow-up (Wolchik et al., 2002); the 15-year interval was used to assess the overall effects of the program on incidence of mental health and substance-related disorders. It was hypothesized that YAs in the mother program or dual-component program would have a lower incidence of disorders than those in the literature control condition. i. Given that baseline risk moderated program effects at earlier assessments ((Wolchik, Sandler, Weiss, & Winslow, 2007; Wolchik, et al., 2002; Wolchik, et al., 2000)), with stronger effects occurring for those at higher risk at program entry, risk was examined as a moderator. Also, given the association between gender and mental health problems and substance use in young adulthood (e.g., Johnston, O'Malley, Bachman, & Schulenberg, 2008), gender was examined as a moderator.
Methods
Participants
Participants were YAs and their mothers from 240 divorced families who participated in a randomized controlled trial of a preventive intervention 15 years earlier. Of the YAs interviewed, 50% were female. Average age of YAs was 25.6 (SD=1.2, range = 24-28). Ethnicity was 88.7% Non-Hispanic White, 6.7 % Hispanic, 2.1% African-American, and 2.5% other. Educational attainment of YAs was: Less than high school – 2.6%; High school only – 22.1%; Some college – 45.4%; College graduate – 29.4%; Post-graduate – 3.1%. Of the YAs, 51% were married or living as if married. YA median annual income was in the $30,000 range (choices were $5,000 categories ranging from ≤ $5,000 to ≥ $200,000).
The primary method of recruitment for the trial involved the use of randomly selected court records of divorce decrees that involved children and were granted within two years of the intervention's start. Eighty percent of the sample was recruited in this way; the remainder responded to media advertisements. Families were first sent a letter about the study, which was followed by a phone call to assess eligibility criteria and invite mothers to participate in an in-home recruitment visit. Eligibility was assessed at pretest as well.
Eligibility criteria were: a) divorced in past two years, b) primary residential parent was female, c) at least one 9-12 year-old child resided (at least 50%) with the mother, d) neither mother nor any child was in treatment for mental health problems, e) mother had not remarried, did not plan to remarry during the program, and did not have a live-in boyfriend, f) custody was expected to remain stable, g) family resided within an hour drive of program site, h) mother and child could complete assessments in English, i) child was not learning disabled or in special education, and j) if diagnosed with attention deficit disorder, child was taking medication. The criterion of maternal residential living arrangements was selected because at the time of the trial, about 80% of children lived primarily with their mothers (Cancian & Meyer, 1998). In families with multiple children in the age range, one was randomly selected as the target child for the assessment of program effects to ensure independence of responses. Because of the preventive nature of the program and ethical concerns, families were excluded and referred for treatment if the child scored above 17 on the Children's Depression Inventory (CDI) (Kovacs, 1985), endorsed an item indicating that s/he wanted to kill herself/himself, or scored above the 97th percentile on the Externalizing Subscale [Child Behavior Checklist (CBCL); (Achenbach, 1991)].
The trial was conducted at Arizona State University (ASU) in Tempe, AZ. The study was approved by the ASU Institutional Review Board. Assessments (i.e., pretest; posttest; and 3-month, 6-month, six-year and 15-year follow-ups) were typically conducted in the participants’ homes; a few occurred at the university. Interviews for three YAs who lived abroad were conducted via skype; the items in the self-administered questionnaires were read aloud in these cases. The intervention groups were held at the university. Assessments were conducted by trained interviewers who were blind to program condition. Parents and youths older than 18 signed informed consent forms; children signed informed assent forms. Families received $45 compensation for participating in the interviews at pretest, posttest, 3-month and 6-month follow-ups. At the six-year follow-up, adolescents and parents each received $100; at the 15-year follow-up, young adults received $225 and parents received $50.
Sample size, power and precision
A sample size of 240 was selected so that small to medium effects, the magnitude of the effects found in the pilot study of the MP (Wolchik, et al., 1993), could be detected with power of ≥ .80. Hypothesis tests were conducted using 2-tailed tests with α=.05. Assuming the covariates account for 25% of the variance, power to detect small to medium (Cohen d=.32) effects of mean differences is .80 using analysis of covariance (ANCOVAs). Assuming a 30% base rate of diagnosis in LC, power is over .90 to detect an OR of 2 with logistic regression. Assuming a .25 control hazard rate, power to detect a risk ratio of .5 is .87 in survival analyses.
Measures
Mental Health Outcomes
The Diagnostic Interview Schedule IV (DIS) (Robin, et al., 2000) was administered to YAs to assess internalizing and externalizing disorders. The DIS has adequate reliability and validity (Compton & Cottler, 2000) and has been used in numerous epidemiologic studies of mental disorder (e.g., Grant et al., 2004). The presence of disorder was scored according to the DIS manual. YAs met criteria for a disorder if they endorsed the required symptoms and reported that the symptoms caused impairment (problems) in social, occupational, or other areas of functioning. Disorders were classified as internalizing or externalizing based on the consensus of three doctoral-level clinicians.
As noted earlier, the incidence of disorder was assessed over two periods of time, past 9 years and past 15 years. To assess program effects on disorders that were distinct from those reported at the six-year follow-up, dichotomous disorder scores were created based on whether criteria for any externalizing disorder, any internalizing disorder and any internalizing or externalizing disorder were met with symptom onset in the past nine years using the standard DIS methods for dating onset (Robin et al., 2000). To ensure that the disorders reported on the DIS with onset in the last nine years were new disorders rather than continuations of disorders reported at the six-year follow-up, scores on the C-DIS at the six-year follow-up were also examined to check that disorders dated as having their onset in the past nine years were not present when youth were interviewed at the six-year follow-up (Wolchik, et al., 2002) [Diagnostic Interview Schedule for Children, C-DIS (algorithm version J; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000)]. None of the disorders with onset during the last nine years represented the continuation of a disorder that was reported at the six-year follow-up. To assess overall effects of the program on incidence of disorder, the same scores as above were calculated with the time frame being since program entry (during the last 15 years).
To assess recent mental health problems, the internalizing problems and externalizing problems subscales of Adult Self Report (ASR; YA;(Achenbach & Rescorla, 2003) and Adult Behavior Checklist (ABCL; mother; (Achenbach & Rescorla, 2003) were used. These scales, which assess mental health problems in the past six months, have adequate reliability and validity (Achenbach & Rescorla, 2003). Alphas for internalizing problems were .90 and .92 for YA and mother reports, respectively; alphas for externalizing problems were .84 and .92 for YA and mother reports, respectively. Mother and YA scores were standardized and then averaged.
Substance Use Outcomes
A dichotomous disorder score for presence of any substance-related disorder and a continuous score for number of substance-related disorders with symptom onset in the last nine years were assessed using the standard DIS method for dating onset. As with mental health disorders, scores on the C-DIS at the six-year follow-up were also examined to check that disorders dated as having their onset in the past nine years were not present when youth were interviewed at the six-year follow-up. None of the substance-related disorders reported on the DIS with onset during the last nine years represented a continuation of a disorder reported at the six-year follow-up. Scores for any substance-related disorder and number of substance-related disorders during the last 15 years were assessed using the standard DIS methods for dating onset.
Age of onset of regular drinking was derived from the DIS. Items from the Monitoring the Future Scale (MTF) (Johnston, O'Malley, & Bachman, 1993) were used to assess alcohol use and marijuana use in the past month (1=0 occasions; 7=40 or more) and other drug use (i.e., mean of ratings for 13 drugs other than alcohol and marijuana; 1=0 occasions; 7=40 or more) and polydrug use (count of different drugs used) in the past year. The MTF has adequate internal consistency reliability and validity (Johnston, et al., 1993). To maximize validity, MTF items were self-administered (Gribble, Miller, Rogers, & Turner, 1999). Substance use problems in the past six months were assessed by standardizing and averaging mother (ABCL) and YA (ASR) reports. Achenbach and Rescorla (2003) note that alpha is not applicable for this subscale. Binge drinking was measured using an adaptation of an item from the Quantity and Frequency of Alcohol and Drugs Scale (Sher, Walitzer, Wood, & Brent, 1991) that assessed the frequency of binge drinking in the past year (1= less than five times; 2=more than 5 times but less than once a month; 3= 1-3 times a month, 4=1-2 times a week, 5=3-5 times a week, 6= every day). This item is highly similar to those typically used to define binge drinking behavior (Johnston, O'Malley, Bachman, & Schulenberg, 2011).
Covariates
Baseline risk, internalizing problems and self-esteem were used as covariates in all analyses. Risk, as defined by (Dawson-McClure, Sandler, Wolchik, and Millsap, (2004), was a composite score (i.e., equally-weighted sum of standardized scores) of: a) mother and child reports of child externalizing problems at baseline [the 33-item externalizing subscale of Child Behavior Checklist (CBCL; Achenbach,1991; alpha=.86) for parent report; the 27-item Divorce Adjustment Project Externalizing Scale (Program for Prevention Research, 1985; alpha=.87) for child report] and b) environmental stressors (i.e., a multicomponent measure of interparental conflict, negative life events that occurred to the child, maternal distress, missed visits with the non-custodial father, current per capita annual income). This composite risk measure had been found to predict child mental health problems in the control group of the randomized trial of NBP at the six-year follow-up and to moderate the NBP's effects on internalizing problems, externalizing problems, substance use, mental disorder and competence at the six-year follow-up, such that stronger intervention effects were found for youth at higher risk at program entry (Dawson-McClure et al., 2004). Accordingly, we included the risk measure as a covariate and examined whether risk interacted with NBP's effects at the 15-year follow-up. The inclusion of internalizing problems and self-esteem was based on results of analyses comparing non-respondents and respondents at the 15-year follow-up on 16 baseline variables (Jurs & Glass, 1971), which showed no significant attrition × group interactions but two significant main attrition effects. On average, respondents had significantly lower self-esteem (20.45 vs. 21.53; p < .03) and higher levels of internalizing problems (−.06 vs. −.30; p < .03) than non-respondents. Pretest internalizing problems was a composite of standardized scores on the CBCL internalizing subscale (alpha=.87, mother report), the CDI (alpha=.87, child report) and Revised Children's Manifest Anxiety Scale (Reynolds & Richmond, 1978) (alpha=.90, child report). Pretest self-esteem was assessed with the Self-Perception Profile for Children (Harter, 1985) (alpha=.71, child report).
Intervention and Control Conditions
Intervention Conditions
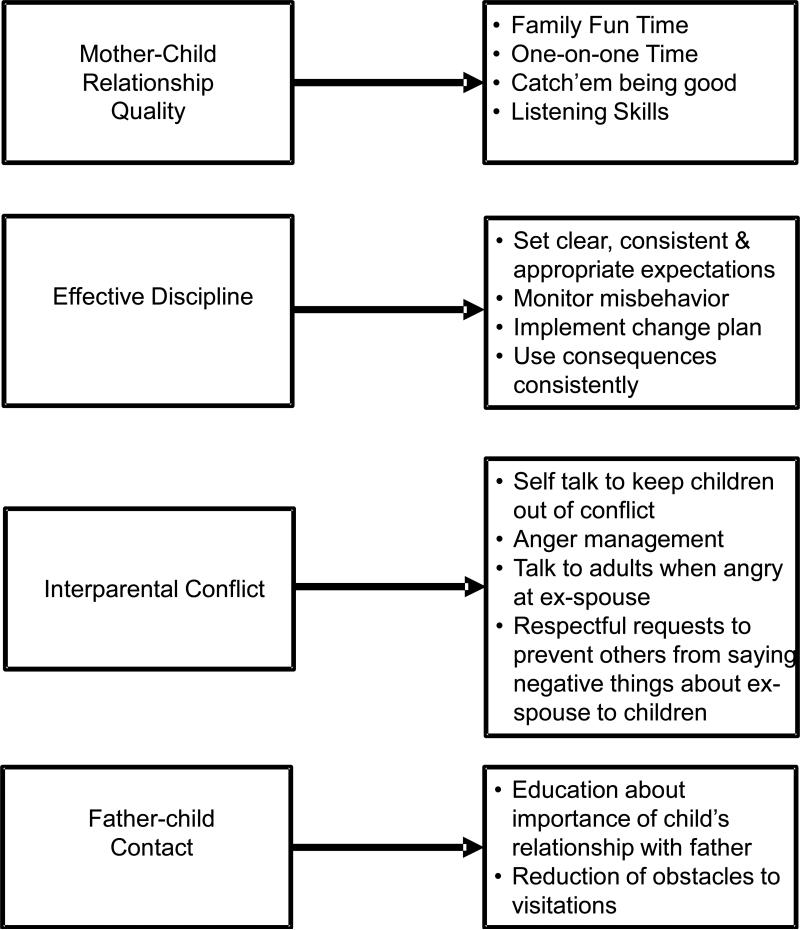
The mother program consisted of 11 group sessions (1.75-hours each) that focused on four family processes that had been shown to predict children's post-divorce adjustment problems and could potentially be changed by working with mothers (Wolchik et al., 2000). The program taught skills to improve mother-child relationship quality and effective discipline, decrease barriers to father-child contact and reduce children's exposure to interparental conflict. Clinical methods, based on social learning and cognitive behavioral theories, were derived from intervention research (e.g., relationship quality: Guerney, Coufal, & Vogelsong, [1981]; discipline: Patterson, [1976]; anger management: Novaco [1975]). The specific skills that were taught in the program are provided in Figure 1. Based on Marlatt and Gordon's (1985) work, maintenance strategies included leaders providing many opportunities for parents to practice and get feedback on program skills and to address problems with their use, giving parents handouts on skills and forms to track use of the skills after the program, and leaders attributing change to maternal efforts. The highly structured program used active learning methods, videotaped modeling and role plays. Homework assignments focused on practicing the program skills. Two individual sessions were held; one focused on ways to increase use of the program skills; the other focused on ways to increase use of the program skills and ways to decrease barriers to father-child contact. There were 18 mother groups (9 in the mother program condition and 9 in the dual-component condition); average group size was 9 (range 8-10).
Figure 1.
Risk and Protective Factors and Change Strategies Mother Program
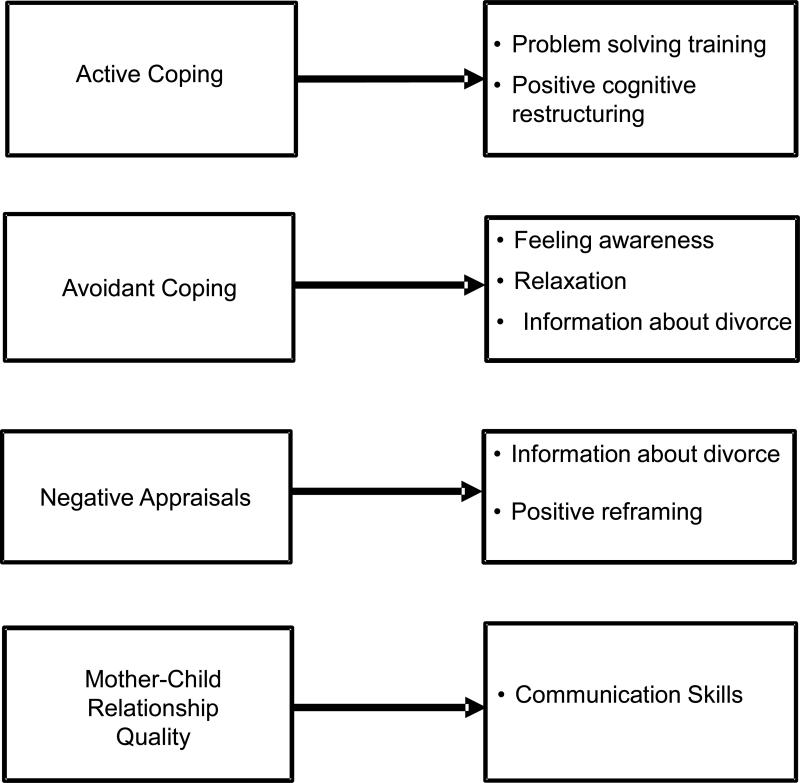
In the dual-component program, mothers participated in the mother program and children participated concurrently in an 11-session group program. The child program targeted active coping, avoidant coping, threat appraisals of divorce stressors, and mother-child relationship quality. The change strategies, based on social learning and social cognitive theory, were derived from intervention research (e.g., coping and appraisals: Pedro-Carroll & Cowen [1985]; relationship quality: Guerney et al. [1981]). The dual-component program included one conjoint group session in which mothers and children practiced listening/communication skills. The specific skills that were taught in the program are provided in Figure 2. Didactic presentations, videotapes, leader modeling, role plays and engaging games were used to teach the program skills. Homework involved practicing the program skills. There were nine child groups with an average group size of 9 (range 9-10). For more information about the programs, see Wolchik et al. (2000; 2007).
Figure 2.
Risk and Protective Factors and Change Strategies Child Program
Each group was led by two Master's-level clinicians (13 leaders for mother groups; 9 for child groups). The leaders used highly detailed session manuals to deliver the groups. Extensive training (30 hours prior to the start of the program and 1.5 hours per week during delivery) and weekly supervision (1.5 hour per week) were provided by doctoral-level clinicians. Prior to delivery of each session, leaders were required to score 90% on a quiz of the content of the session. Average scores were 97% (SD=3%) and 98% (SD=1%) for leaders in the mother and child groups, respectively.
Control condition
In the literature control condition (LC), mothers and children received three books each about children's divorce adjustment and a syllabus to guide their reading. Books were mailed to families at one-month intervals.
Random Assignment
After completion of the pretest, families were randomly assigned to one of three conditions: mother, dual-component or LC. Randomization was conducted by project staff other than the investigators and interviewers. A computer-generated algorithm developed by a researcher not involved in the trial was used to assign families to condition. Randomization was conducted within the evening availability pool (Tuesday vs. Thursday) because some families could attend on only one of the two nights the groups were offered.
Masking
Interviewers were given no information about families’ program condition. To reduce the likelihood that interviewers would learn about the condition, at the beginning of the interview, participants were asked not to discuss their program. After the assessment was complete, interviewers completed a question about knowledge of the participant's intervention condition. At the 15-year follow-up, 95% (mother interviewers) and 96% (YA interviewers) were blind to assignment.
Data Analytic Approach
Given the lack of differences between the mother and dual-component programs in prior evaluations (Wolchik, et al., 2007; Wolchik, et al., 2002; Wolchik, et al., 2000), preliminary analyses comparing these two conditions on all outcome measures at the 15-year follow-up were conducted using logistic regression for dichotomous outcome variables and ANCOVAs for continuous outcomes. The two conditions differed on 4% of the comparisons. Because fewer differences than would be expected by chance were found, these conditions were combined and labeled the New Beginnings Program (NBP). Intervention effects were evaluated by comparing the NBP and LC.
Baseline equivalence of the NBP and LC on demographic and child functioning variables was tested using χ2 (categorical) or t-statistics (continuous). Attrition analyses (Jurs & Glass, 1971) [analyses of variance (continuous); χ2 test or logistic regression (dichotomous)] were conducted to examine whether attrition rates differed across condition and whether attrition or attrition × intervention effects were related to baseline demographic or child functioning variables.
Intervention effects were examined with logistic regression (dichotomous), ANCOVAs (continuous), and Cox proportional hazards survival analysis (i.e., onset of drinking, onset of internalizing symptoms for those who developed an internalizing disorder; onset of externalizing symptoms for those who developed an externalizing disorder), controlling for baseline risk. For each outcome, differential program effects were first examined across baseline risk and YA gender. If an interaction were significant, tests of simple effects were conducted. If an interaction were not significant, the analysis was re-run without the interaction term.
An intent-to-treat approach with the original 240 families was employed in all analyses except those that used DIS disorder scores (i.e., presence of internalizing disorder, presence of externalizing disorder, presence of an internalizing or externalizing disorder, presence of substance-related disorder and number of substance-related disorders) and onset of regular drinking. In the analyses of DIS scores in the last nine years (since the last follow-up), YAs who reported a disorder with any broadband symptom onset more than nine years earlier (i.e., internalizing symptom, externalizing symptom, substance use symptom), as assessed on the DIS, or who met criteria for an internalizing, externalizing, or substance-use disorder on the C-DISC at the six-year follow-up, were not included (internalizing disorder [43 excluded]; externalizing disorder [14 excluded]; substance-related disorder and number of substance-related disorders [29 excluded]). In the analyses of DIS scores since the program began (i.e., last 15 years), YAs who reported a disorder on the DIS with symptom onset prior to the beginning of the program were excluded (substance use [3 excluded]; internalizing disorders [26 excluded]; externalizing disorders [4 excluded]). In the analyses of onset of regular drinking, YAs who reported that they started drinking before the program began were excluded [4 excluded].
The rates of missing data for study variables and covariates ranged from 0% to 23% (Median = 19%). Because missingness was related to baseline self-esteem and internalizing problems, missing at random (MAR) was assumed. Mplus software (Muthén, & Muthén, 1998-2010) was employed for analyzing continuous variables, using full-information maximum likelihood estimation to handle missing data. Due to the inability of Mplus to handle missing data with categorical or count variables, SAS 9.2 (SAS Institute 2010), incorporating the multiple imputation procedure for missing data, was used for analyzing dichotomous variables and time of onset (Ake & Carpenter, 2002). Both methods are based on expectation-maximization (EM) algorithm of handling missing data and are comparable in performance (Schafer & Graham, 2002).
Because the intervention was delivered in a group format, NBP participants were nested within group. The intra-class correlations (ICCs) for binary variables were computed using Guo and Zhao's (2000) procedure. ICCs across all of the study variables for the intervention group were very low with a mean of .02 (SD = .03).
To adjust for multiple tests, the false discovery rate (Benjamini & Hochberg, 2000), which controls for the expected proportion of false positives among all significant hypotheses, was applied to the main and interaction effects separately for mental health and substance use outcomes. We interpreted effects as reliable if the FDR was ≤10% and the observed p-value met Benjamini-Hochberg's adaptive FDR criterion (Benjamini & Hochberg, 2000).
Results
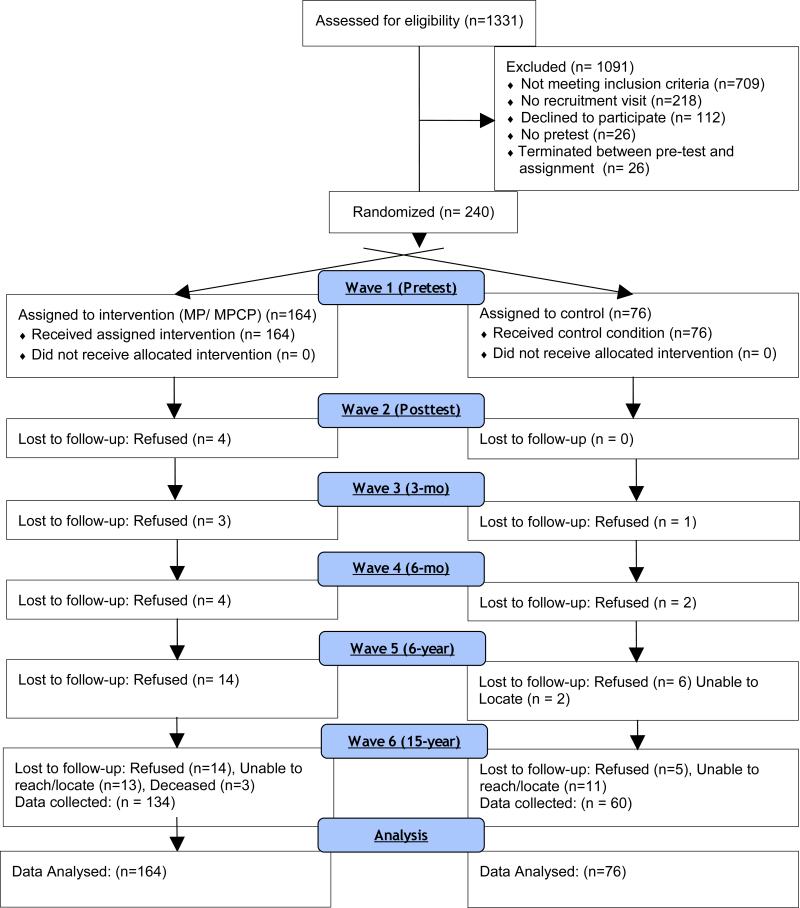
Participant flow
Figure 3 depicts the screening and enrollment process. As shown in Figure 3, of the 1,331 families contacted by phone, 709 (53%) did not meet eligibility criteria, 218 (16%) did not complete the recruitment visit, 112 (8%) declined participation, 26 (2%) did not complete the pretest, 49 (4%) were ineligible at pretest, and 26 (2%) terminated participation between pretest and random assignment to condition, which occurred after the pretest. Two hundred forty families (38% of those that were eligible) were randomly assigned to the mother program (n=81), dual-component program (n=83), or LC (n=76). In accord with intent-to-treat designs, all participants who were randomly assigned to condition were included in the analyses.
Figure 3.
Participant Flow
Families were recruited for participation in the randomized trial from 3/1992 to 12/1993. Data for this report are from the 15-year follow-up (4/2007- 1/2009), which occurred an average of 15.3 years (SD=.10) after the posttest. At the 15-year follow-up, data were collected from 89.6% of the families (194 YAs; 204 of the mothers) randomly assigned to condition. Rate of attrition at 15-year follow-up did not differ significantly across NBP (9.8%) and LC (11.8%) (χ2 [1, N=240] = .24, p=.65) conditions. Length of follow-up did not differ across condition (p = .36).
Treatment integrity
Using lists of session content areas (number of areas ranged from 7-11), independent observers rated videotapes for the degree of completion of each content area. Inter-rater reliability, assessed for a randomly selected 20% of the sessions, averaged 98%. The average rate of completion of session activities was high (2.86 [SD=0.39] for the mother groups and 3.00 [SD=0.02] for the child groups; 1=not at all and 3=completed.
Mothers attended an average of 77% (M=10.2; SD =3.56) of the 13 sessions (11 group, 2 individual). Children attended an average of 78% (M=8.55; SD =2.97) of the 11 group sessions. Attendance in the mother program did not differ significantly for the mother program (M=9.72, SD =3.53) and dual-component program conditions (M=10.33, SD =3.44) conditions (p = .28). LC participants reported reading about half the books [mothers: 3.04 (SD=.92); children: 3.22 (SD=1.01); 1=not at all, 5=whole].
Preliminary analyses
Sample representativeness was assessed by comparing the baseline demographics and child functioning variables in Table 1 across families assigned to condition (N=240) and eligible families that refused to participate but agreed to complete the pretest (N=62). Families assigned to condition reported significantly higher incomes (t=2.54, p=.01) and maternal education (t=2.73, p=.01). There were no significant differences across the NBP and LC on demographic variables and child functioning at baseline (see Table 1).
Table 1.
Demographics and Child Functioning Variables at Baseline
| Control | NBP | Difference | |
|---|---|---|---|
| Demographics | |||
| Male youth, No. (%) | 37 (48.68%) | 86 (52.44%) | p = .59 |
| Youth mean age | 10.27 (1.06) | 10.38 (1.15) | p = .59 |
| Sole maternal legal custody, No. (%) | 48 (63.16%) | 104 (63.41%) | p = .96 |
| Mother | |||
| Ethnicity, No. (%) | p = .57 | ||
| White, Non-Hispanic | 66 (88.41%) | 145 (88.68%) | |
| Hispanic | 8 (10.53%) | 10 (6.10%) | |
| Black | 1 (1.32%) | 3 (1.83%) | |
| Asian American/Pacific Islanders | 0 (0%) | 3 (0.07%) | |
| Other | 1 (1.67%) | 3 (1.83%) | |
| Education1 | 4.93 (1.10) | 5.04 (1.20) | p = .53 |
| Age, years | 36.47 (4.63) | 37.74 (4.85) | p = .06, |
| Gross income, US $ | 5.68 (2.61) | 5.88 (3.26) | p = .65 |
| Father | |||
| Ethnicity, No. (%) | p = .81 | ||
| White, Non-Hispanic | 68 (90%) | 139 (84.33%) | |
| Hispanic | 5 (6.58%) | 14 (8.54%) | |
| Black | 2 (2.63%) | 5 (3.05%) | |
| Asian American/Pacific Islanders | 0 (0%) | 2 (1.22%) | |
| Other | 1 (1.32%) | 5 (3.05%) | |
| Education | 4.62 (1.43) | 4.62 (1.56) | p = .99 |
| Age, years | 38.82(5.39) | 40.04 (5.74) | p= .12 |
| Father (ex-spouse) remarried2, No. (%) | 12 (15.79%) | 22 (13.41%) | p= .64 |
| Time since separation, months | 27.91(18.86) | 26.41 (16.45) | p = .53 |
| Time since divorce, months | 12.43 (6.39) | 12.12 (6.43) | p = .73 |
| Child Functioning Variables | |||
| Internalizing Problems – Mother + Child Report | −.050 (.71) | .023 (.78) | p = .49 |
| Externalizing Problems – Mother + Child report | −.197 (.70) | −.001 (.91) | p = .10 |
| Self-Esteem – Child Report | 20.82 (2.80) | 21.06 (6.75) | p = .76 |
Education was defined as 1=Elementary, 2=Some High School, 3=High School Graduate, 4=Technical School, 5=Some College, 6=College Graduate, 7=Graduate School.
Remarriage of mother was an exclusion criterion.
Analyses of Intervention Effects
Table 2 presents the analyses of program main effects and program × gender interaction effects. None of the program × baseline risk interaction effects had a FDR ≤.10. This table presents program effects on mental health and substance-related abuse disorders with onset in the past nine years. Thus, these results are not redundant with previously reported findings on program effects on disorder at the six-year follow-up (Wolchik et al., 2002).
Table 2.
NBP Intervention Effects at 15-year Follow-Up
| Measures | Actual Proportion (SD) / Actual Means (SD)1 | Main Effect | Program × Gender Effect | |||
|---|---|---|---|---|---|---|
| NBP (n=164) | Control (n=76) | Adjusted regression weight2(CI) [Odds Ratio (OR) or Cohen's d] | p-value (FDR p-value) | Adjusted regression weight (CI) (Cohen's d)3 | p-value (FDR p-value) | |
| Mental Health Problems | ||||||
| Composite ABCL/ASR internalizing t-Score (mean) | 55.02 (4.84) | 55.48 (5.71) | −.91 (−2.38, .56) | .23 (.28) | −1.80 (−4.75, 1.15) | .23 (.53) |
| Composite ABCL/ASR externalizing t-Score (mean) | 49.15 (9.11) | 49.00 (9.04) | −.36 (−2.83, 2.11) | .78 (.78) | −1.57 (−6.53, 3.39) | .53 (.53) |
| Internalizing disorder past 9 years (%)4 | 4.55% (2.69 ) | 16.7% (3.25) | −1.36 (−2.41, −.32) OR=.26 | .007 (.03) | .71 (−1.29, 2.71) | .37 (.53) |
| Externalizing disorder past 9 years (%)4 | 0% (0) | 3.64% (.04) | −.86 (−.96, .31) | .12 (.27) | −.74 (−2.78, 1.29) | .43 (.53) |
| Internalizing or externalizing disorder past 9 years (%)4 | 8.0% (2.71) | 19.5% (6.19) | −1.19 (−2.33, −.06) OR=.30 | .04 (.09) | −1.19 (−3.41, 1.04) | .30 (.53) |
| Substance Use | ||||||
| Age started regular drinking (mean) | 18.36 (2.30) | 18.84 (2.62) | −.47 (−1.31, .36) | .17 (.49) | 1.94 (.27, 3.61) | .22 (.28) |
| Binge drinking past year(mean) | 1.10 (1.14) | .93 (1.23) | .16 (−.14, .46) | .29 (.49) | −.64 (−1.44, .17) | .12 (.15) |
| Alcohol use past month (mean) | 3.22 (1.52) | 2.98 (1.70) | .23 (−.26, .72) | .35 (.57) | −1.12 (−2.06, −.18) d =.44 (female) | .02 (.08) |
| Marijuana use past month (mean) | 1.66 (1.53) | 1.98 (1.88) | .00 (−.47, .47) | .99 (.99) | −.27 (−1.17, .64) | .57 (.64) |
| Polydrug use past year (mean) | 1.58 (1.23) | 1.98 (1.88) | −.44 (−.88, .00) | .05 (.23) | −.88 (−1.76, .01) d =.55 (male) | .05 (.08) |
| Other drug use past year (mean) | 1.05 (.15) | 1.11 (.23) | −.06 (−.11, −.00) | .04 (.23) | −.12 (−.23, −.02) d =.61 (male) | .03 (.08) |
| Composite ABCL/ASR substance use problems t-score (mean) | 55.43 (5.18) | 55.70 (4.96) | −.95 (−2.45, .56) | .22 (.49) | −3.51 (−6.49, −.53) d =.50 (male) | .02 (.08) |
| Substance use disorder past 9 years (%)4 | 18.6% (4.13) | 15.38% (2.60) | .08 (−.78, .95) | .82 (.92) | −2.65 (−4.97, −.33) | .05 (.08) |
| Number of substance use disorders past 9 years (mean)4 | .20 (.50) | .32 (1.31) | −.11 (−.34, .13) | .38 (.57) | −.48 (−.94, −.01) d =.40 (male) | .05 (.08) |
The confidence intervals for the actual proportions (binary variables) and means (continuous variables) did not control for the baseline covariate nor reflect the FIML estimate of the intervention effect.
The intervention condition was coded as 0 (control) vs. 1 (NBP). Thus, the adjusted regression weight for the main effect is the adjusted mean difference between the two conditions.
Cohen's d was reported only for findings with FDR p ≤ .10.
Only YAs who reported a disorder with broadband symptom onset after the six-year follow-up assessment were included in these analyses (N = 197 internalizing disorder; N = 226 for externalizing disorder; N = 211 for substance-related disorder and number of substance-related disorders).
Mental Health Outcomes within past nine years
There were two significant main effects that had a FDR≤.10 and met the adaptive FDR criterion. A smaller percentage of YAs in the NBP than YAs in the LC developed an internalizing disorder in the last nine years [7.55% vs. 24.40%; p = .007; OR=.26 (95% CI .09-.72); absolute risk reduction=16.85% (95% CI, 1% to 34%)]. Also, a smaller percentage of YAs in the NBP than in LC developed either an internalizing disorder or an externalizing disorder [8.00% vs. 19.5%; p = .04; OR=.33 (95% CI, .10 to .94); absolute risk reduction= (11.50% (95% CI, 7% to 16%)]. Table 3 shows the percentage of YAs in the NBP and LC conditions who met diagnostic criteria for specific disorders. Given the limited number of cases for most disorders, we were able to analyze the data for major depression only. The NBP significantly reduced the onset of major depression relative to the LC (χ2[1] = 3.85, p = .04).
Table 3.
Percentage of YA's Meeting Criteria for Disorders1
| NBP – Past 9 Years % (n) | LC – Past 9 Years % (n) | NBP – Past 15 Years % (n) | LC – Past 15 Years % (n) | |
|---|---|---|---|---|
| Internalizing | ||||
| Major Depressive episode2 | 16.5(15) | 24.4 (10) | 18.4 (23) | 28.8 (17) |
| Bipolar/ Manic episode | 0 (0) | 2.3 (1) | 1.5 (2) | 3.3 (2) |
| Panic disorder | 0.8 (1) | 0 (0) | 1.5 (2) | 0 (0) |
| Generalized anxiety disorder | 4.0 (4) | 0 (0) | 4.5 (6) | 0 (0) |
| OCD (compulsive) | 0 (0) | 0 (0) | 0.8 (1) | 1.7 (1) |
| Specific phobia | 0 (0) | 3.8 (2) | 0.8 (1) | 5.5 (3) |
| Social phobia | 0 (0) | 0 (0) | 1.5 (2) | 3.4 (2) |
| PTSD | 0 (0) | 12.5 (5) | 0.8 (1) | 11.9 (7) |
| Eating disorder | 0 (0) | 0 (0) | 1.6 (2) | 0 (0) |
| Externalizing | ||||
| Conduct disorder | 0 (0) | 0 (0) | 3.4 (4) | 1.9 (1) |
| Attention deficit disorder | 0 (0) | 5.0 (2) | 0 (0) | 3.5 (2) |
| Antisocial personality disorder | 0 (0) | 0 (0) | 3.7 (5) | 6.7 (4) |
| Substance Use3 | ||||
| Nicotine | 5.2 (6) | 7.5 (4) | 6.7 (9) | 6.7 (4) |
| Alcohol | 22.4 (24) | 17.6 (9) | 23.7 (31) | 23.3 (14) |
| Drug | 5.7 (6) | 5.8 (3) | 9.9 (13) | 6.7 (4) |
These percentages are based on the 194 YAs who participated in Wave 6 (15 year follow-up). YAs with onset of symptoms associated with the specific disorder (e.g., depressive symptoms) prior to the program were excluded from the “Past 15 Years” calculations and YAs with onset of symptoms associated with the specific disorder prior to Wave 5 (6 year follow-up) were excluded from the “Past 9 Years” calculations.
For ease of presentation, several diagnostic categories were combined. Major Depressive episode includes major depressive disorder single and recurrent episode, Bipolar/Manic Episode includes manic episode, hypomania, and bipolar I and II (single and recurrent), Eating disorder includes anorexia and bulimia, Nicotine includes nicotine withdrawal and dependence, Alcohol includes alcohol withdrawal, dependence, and abuse, and Drug includes drug withdrawal, dependence and abuse.
A program x gender effect occurred for substance use disorder. Males in the NBP had fewer substance abuse disorders than those in the LC.
The results of the survival analysis show that, compared to YAs in the LC, the rate of onset of internalizing symptoms during the past nine years for YAs in the NBP who developed an internalizing disorder decreased by 72% [hazard ratio (HR) =.28 (95% CI .10-.74); p = .01]. Figure 4 shows the hazard functions for the NBP and LC conditions.
Figure 4.
Cumulative proportion of onset of symptoms for an internalizing disorder since program entry. LC = Literature control condition; NBP = New Beginnings Program condition. For the NBP condition, there was no onset of symptoms for new cases of internalizing disorder after 12 years from program entry and for the LC condition there was no onset of symptoms for new cases of internalizing disorder after 13 years from program entry. The shaded grey area represents time since the six-year follow-up and shows onset of new internalizing disorder during this time period.
There were no significant program effects on internalizing or externalizing problems in the past six months. Analyses conducted separately for mother and YA report of internalizing problems and externalizing problems(i.e., ABCL/ASR) in the past six months showed a similar pattern of findings (i.e., program effects were non-significant). None of the program by gender interaction effects was significant.
Substance Use Outcomes within the past nine years
There were six significant program x gender effects that had a FDR ≤ .10 and met the adaptive FDR criterion. Post-hoc analyses within gender found that males in the NBP had a lower number of substance-related disorders in the past nine years (adjusted means = −.06 vs. .29; p = .05; Cohen d=.40) than males in the LC. Also, males in the NBP reported less polydrug use (adjusted means = 2.88 v. 3.80; p =.05; Cohen d=.55) and other drug use in the past year (adjusted means = 1.10 vs. 1.24; p =.03; Cohen d=.61) and fewer substance use problems (composite of ABCL/ASR scores) in the last six months (adjusted means = 54.28 vs. 56.99; p = .02; Cohen d=.50) than those in the LC. Analyses conducted separately for mother and YA reports of substance use problems in the last six months (i.e., ABCL/ASR) showed a similar pattern of effects as the analysis that used the composite score; the program × gender interaction was marginally significant for YA report and significant for mother report. The direction of the simple effects tests was consistent with that for the composite variable. The program × gender interaction for substance-related disorder was significant but the simple effects tests comparing NBP and LC for males and females did not reach p ≤ .05. Unexpectedly, females in the NBP reported more alcohol use in the past month than those in the LC (adjusted means = 3.86 vs. 3.13; p = .02; Cohen d=.44). The difference across condition on this variable for males was non-significant.
Mental health and substance–related disorder since program entry (past 15 years)
To examine program effects on disorders that occurred any time after the program began rather than on disorders with onset between the six-year and 15-year follow-up, additional analyses were conducted on the DIS variables. The results were similar to those for onset of disorder in the past nine years. A smaller percentage of YAs in the NBP than YAs in the LC developed an internalizing disorder in the last 15 years [15.52% vs. 34.62%; p = .006; OR=.34 (95% CI, .16 to .73); absolute risk reduction=19.10% (95% CI, 3% to 35%)]. In addition, a smaller percentage of YAs in the NBP than in the LC developed either an internalizing disorder or an externalizing disorder in the last 15 years [25.20% vs. 38.89%; p = .05; OR=.50 (95% CI, .24 to .99); absolute risk reduction= (13.69% (95% CI, 4% to 23%)].The program × gender interaction on number of substance-related disorders was marginally significant (p = .08).
Table 3 presents the percentages of YAs who met criteria for specific disorders in the NBP and LC conditions. As can be seen, the program effect on internalizing disorders is primarily due to the effect to reduce the incidence of major depressive disorders.
The results of the survival analysis showed that, compared to YAs in the LC, the rate of onset of internalizing symptoms for YAs in the NBP who developed an internalizing disorder in the past 15 years decreased by 54% (HR =.46 [95% CI .24-.96]; p = .01. Figure 4 shows the hazard functions across intervention conditions since the beginning of the program.
Discussion
This is the first study to examine the effects of a preventive intervention for divorced families provided in childhood on the incidence of mental health and substance-related disorders and problems in young adulthood. The internal validity of these findings is enhanced by the randomized design, very high levels of fidelity of implementation of the program, high level of retention of participants in the 15-year follow-up, use of an intent-to-treat data analysis approach and use of the false discovery method to protect against alpha inflation.
The results indicated that the NBP reduced the likelihood of onset of an internalizing disorder in the nine-year period between the previous and current follow-up which spanned from mid-to-late adolescence to young adulthood, and slowed the rate at which an internalizing disorder developed. Further, for males, the program reduced the number of substance-related disorders between adolescence and young adulthood and several aspects of substance use, including frequency of use of several types of substances during the last year and substance use problems in the last six months. However, for females, program participation led to an increase on one of the nine measures of substance use, alcohol use in the last month.
The analyses showed significant program effects for both males and females on the incidence and rate of onset of internalizing disorders. Three times more young adults in the LC experienced the onset of an internalizing disorder since the follow-up in adolescence than those in the NBP (24.40% vs. 7.55%), with most of the disorders being major depression. In addition, since the follow-up in adolescence, for those who developed an internalizing disorder, the rate of developing an internalizing disorders in the LC was about three and half times faster (earlier onset) than in the NBP (HR = .28). Further, using the interval from program entry to the current follow-up, about two times more young adults in the LC than in NBP experienced the onset of an internalizing disorder (34.62% vs. 15.52%) and these disorders developed about two times faster for those in the LC versus NBP condition (HR =.46). It is important to note that most of the effect on internalizing disorder appears to be accounted for by a reduction in major depression (i.e., 18.4% NBP vs. 28.8% LC for onset since program initiation). There was no evidence that the intervention produced effects on anxiety disorders. It is notable that the rate of depression in the NBP group is similar to the lifetime prevalence of major depression reported in a nationally representative sample of 19 to 29 year olds (15.4%; Kessler et al., 2005), while the rate of depression is substantially higher in the LC group.
These findings augment the limited research on the long-term effects of prevention programs provided in childhood. Previous research has found preventive effects on outcomes such as felony arrests, incarceration, high risk sexual behaviors, marijuana use, and depressive symptoms in adulthood (Campbell, Ramey, Pungello, Sparling & Miller-Johnson, 2010; Lonczak, Abbott, Hawkins, Kosterman & Catalano, 2002; Reynolds et al., 2007; Schweinhart & Weikart, 1997). To our knowledge, this is the first study to find long-term program effects on the incidence of major depression from mid-to-late adolescence to young adulthood. Preventing the onset of mental disorders at this point in development is important because young adulthood is a time when key choices are made in multiple life spheres (Schulenberg, Sameroff, & Cicchetti, 2004) and mental health problems during this period can have serious, long-lasting consequences (Arnett & Tanner, 2006).
The enduring impact of the NBP is noteworthy given its length (11 weeks). Most studies that have assessed young adults who were involved in preventive programs during childhood (e.g., Lonczak et al., 2002; Reynolds et al., 2007; Schweinhart & Weikart, 1997) have evaluated much lengthier programs (e.g., 9 months to 6 years). Although Sandler and colleagues (2011) review of 46 parenting-focused prevention programs found evidence of effects lasting a year or longer, the maintenance of program effects into adulthood has been examined for very few programs (Sandler, Schoenfelder, Wolchik, & MacKinnon, 2011). The current results underscore the need to conduct long-term follow-ups to test whether other relatively brief, parenting-focused preventive interventions have effects that last into adulthood.
In contrast to the findings at the six-year follow-up, which showed positive program effects on frequency of substance use for males and females who were at high risk of developing problems at program entry (Wolchik et al., 2002), in the current follow-up, positive program effects occurred for males only. This interactive effect may be related to the higher risk for males to develop substance use problems in young adulthood (Chilcoat & Breslau, 1996; Johnston, et al., 2008; NSDUH Series H-34, DHHS Publication No. SMA 08-4343). Of the program effects on substance use measures, the one with the clearest clinical significance is the reduction in the number of substance-related disorders with onset between mid-to-late adolescence and young adulthood. These findings are encouraging, given estimates that the economic cost of substance abuse exceed $484 billion per year and more than 2 million Americans die each year due to substance use (Hanson & Li, 2003). Additional follow-up of this sample is needed to assess whether the program effects on substance use and substance-related disorders for males are sustained later in development.
Although females in the NBP reported using more alcohol in the last month than those in the LC, the significance of this finding is mitigated by the level of drinking reported in both the NBP and LC groups. Females in both the NBP and LC reported drinking between three and five drinks in the past month, an amount not likely to have clinical significance. Nevertheless, future follow-ups should assess whether this unexpected effect persists and whether program participation predicts problematic substance use outcomes later in development for females.
Preliminary analyses showed very few differences between the two active conditions and thus they were combined and compared to the LC. The absence of long-term additive effects of the child coping component is consistent with the findings at earlier assessments (Wolchik et al., 2000; 2002; 2007). It is important to note that this study examined the additive effects of the child program and did not compare the child program to a control condition. Other researchers have found positive effects for child-focused interventions up to two years after participation (e.g., Pedro-Carroll, 1999), so the lack of additive effects of the child coping component in the current study should not be interpreted to indicate that coping programs are ineffective for this population. The most obvious explanation of the lack of an additive effect in the current study is related to the absence of a differential program effect at posttest on the central target of this component, coping (Wolchik et al., 2000). Possible explanations for the lack of effects on coping include an overreliance on didactic presentation and/or insufficient opportunity for children to practice the more adaptive coping efforts. Alternatively, given Stolberg and Mahler's (2004) findings that adding a parent component to a child coping program did not result in additive effects, it is possible that intervening with either the parent or child is sufficient to reduce the risks associated with divorce. Although the long-term effects of child-focused programs have not been assessed, offering child-focused as well as parent-focused programs could be important, particularly for families in which the parents do not have the time for or interest in participating in a program.
The public health implications of findings on the prevention of major depression and substance-related disorders are encouraging. However, caution is recommended in interpreting the practical implications of the current findings. This university-based trial included extensive supervision and intensive monitoring of implementation. Research is needed to demonstrate that similar effects can be achieved when the program is implemented under real-world conditions as a community service. Also, research is needed to address several limitations of this study. First, the sample was primarily Non-Hispanic White. Research using ethnically diverse samples is vital given that by 2023, ethnic minorities will comprise more than half of U.S. youths (America's Children, 2011). Second, the sample consisted of families in which children lived primarily with their mothers, the living arrangement that characterized the majority of divorced families when the trial was conducted. Given that fathers now play a greater role in post-divorce parenting (Fabricius, Braver, Diaz, & Velez, 2010), it is important to assess the program effects when delivered to fathers, as well as to mothers who are not primary residential parents. Third, few families in the sample lived at or below the poverty level. Research is needed to evaluate the generalizability of this intervention across such high-risk groups. Fourth, using a randomized controlled trial, the purpose of this study was to evaluate the long-term effects of a program that targeted a specific set of family and individual process, which had been consistently shown to be associated with children's post-divorce adjustment and were potentially modifiable by a relatively brief intervention. Similar studies should be conducted to assess the long-term effects of programs that focus on other potential mediators of children's post-divorce adjustment, such as the quality of fathers’ parenting. We are in the process of conducting an effectiveness trial to address several of these limitations in which we are testing the parenting program with a heterogeneous sample of both residential and non-residential fathers and mothers when delivered by community providers under real-world conditions.
There are other potentially fruitful research questions. It will be important to identify the program components that account for the NBP's long-term effects. Studies have shown that program-induced improvements in parenting accounted for program effects on a wide range of mental health problems at earlier waves including higher coping efficacy, improved academic performance, as well as reduced mental health and substance use problems (Tein et al., 2004; Sigal, Wolchik, Tein, & Sandler, 2012; Velez, Wolchik, Tein & Sandler, 2011; Zhou et al., 2008). Parallel analyses are needed to assess the developmental pathways by which the changes induced by the program in adolescence led to reductions in major depression and substance-related disorders in young adulthood. Given research that demonstrates significant continuity in development (Bardone, Moffitt, Caspi, Dickson, Stanton & Silva, 1998; Capaldi & Stoolmiller, 1999), these analyses should include attention to youths’ mental health functioning at earlier assessments as well as the family and individual processes targeted in the program. Conducting a cost-benefit analysis is another important direction for future research. Further, it will be important to examine whether the benefits of the program are found in other areas of adaptation in young adulthood (e.g., romantic relationships) and to reassess the sample to see whether the effects observed in young adulthood are maintained in future developmental periods.
Acknowledgments
This research was funded by the National Institute of Mental Health (5R01MH071707; 5P30MH068685, 5P30MH039246). Trial Registration: clinicaltrials.gov Identifier: NCT01407120. We thank Philip G. Poirier and Linda Sandler for their support throughout this project; the mothers and young adults for their participation; Monique Nuno, Toni Genalo, and Michele McConnaughay for their assistance with data collection and management; the interviewers for their commitment and dedication to this project; and Janna LeRoy for her technical assistance. We also thank the group leaders and graduate students for their assistance with implementing the programs.
Footnotes
Sharlene A. Wolchik, Irwin N. Sandler and Michele M. Porter declare the following competing financial interest: Partnership in Family Transitions – Programs That Work LLC, which trains and supports providers to deliver the New Beginnings Program.
Contributor Information
Sharlene A. Wolchik, Department of Psychology, Arizona State University.
Irwin N. Sandler, Department of Psychology, Arizona State University.
Jenn-Yun Tein, Department of Psychology, Arizona State University..
Nicole E. Mahrer, Department of Psychology, Arizona State University.
Roger E. Millsap, Department of Psychology, Arizona State University.
Emily Winslow, Department of Psychology, Arizona State University..
Clorinda Vélez, Department of Psychology, Swarthmore College..
Michele M. Porter, Department of Psychology, Arizona State University.
Linda J. Luecken, Department of Psychology, Arizona State University.
Amanda Reed, Department of Psychology, Arizona State University..
References
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA adult forms & profiles. University of Vermont, Research Center for Children, Youth & Families; Burlington, VT: 2003. [Google Scholar]
- Afifi TO, Boman J, Fleisher W, Sareen J. The relationship between child abuse, parental divorce, and lifetime mental disorders and suicidality in a nationally representative adult sample. Child Abuse & Neglect. 2009;33(3):139–147. doi: 10.1016/j.chiabu.2008.12.009. doi:10.1016/j.chiabu.2008.12.009. [DOI] [PubMed] [Google Scholar]
- Ake CF, Carpenter AL. Survival analysis with PHREG: Using MI and MIANALYZE to accommodate missing data; Paper presented at the 10th Annual Western Users of SAS Software, Inc. Users Group Conference; Cary, NC. SAS institute Inc.; 2002. Retrieved from http://www.caloxy.com/papers/47-ImputedPHREG.pdf. [Google Scholar]
- Amato PR. Children of divorce in the 1990s: An update of the Amato and Keith (1991) meta-analysis. Journal of Family Psychology. 2001;15:355–370. doi: 10.1037//0893-3200.15.3.355. doi:10.1037/0893-3200.15.3.355. [DOI] [PubMed] [Google Scholar]
- America's Children . Key national indicators of well-being. Federal Interagency Forum on Child and Family Statistics; Washington, DC: 2011. [Google Scholar]
- Arnett JJ, Tanner JL, editors. Emerging adults in American: Coming of age in the 21st century. American psychological Association; Washington, DC: 2006. [Google Scholar]
- Bardone AM, Moffitt TE, Caspi A, Dickson N, Stanton WR, Silva PA. Adult physical health outcomes of adolescent girls with conduct disorder, depression, and anxiety. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:594–601. doi: 10.1097/00004583-199806000-00009. doi:10.1097/00004583-199806000-00009. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. On the adaptive control of the false discovery rate in multiple testing with independent statistics. Journal of Educational and Behavioral Statistics. 2000;25:60–83. doi:10.3102/10769986025001060. [Google Scholar]
- Bramlett MD, Mosher WD. Cohabitation, Marriage, Divorce and Remarriage in the United States. Vital Health Statistics, Series 23, Number 2. National Center for Health Statistics; Hyattsville, MD: 2002. [PubMed] [Google Scholar]
- Braver SL, Griffin WA, Cookston JT. Prevention programs for divorced non-resident fathers. Family Court Review. 2005;43:81–96. doi:10.1111/j.1744-1617.2005.00009.x. [Google Scholar]
- Burke KC, Burke JD, Regier DA, Rae DS. Age at onset of selected mental disorders in five community populations. Archives of General Psychiatry. 1990;47:511–518. doi: 10.1001/archpsyc.1990.01810180011002. doi:10.1001/archpsyc.1990.01810180011002. [DOI] [PubMed] [Google Scholar]
- Campbell FA, Ramey CT, Pungello E, Sparling J, Miller-Johnson S. Early childhood education: Young adult outcomes from the Abecedarian Project. Applied Developmental Science. 2002;6:42–57. doi:10.1207/s1532480xads0601_05. [Google Scholar]
- Cancian M, Meyer D. Who gets custody? Demography. 1998;35:147–157. doi:10.2307/3004048. [PubMed] [Google Scholar]
- Capaldi DM, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. Prediction to young-adult adjustment. Development and Psychopathology. 1999;11:59–84. doi: 10.1017/s0954579499001959. doi:10.1017/S0954579499001959. [DOI] [PubMed] [Google Scholar]
- Chase-Lansdale PL, Cherlin AJ, Kiernan KK. The long-term effects of parental divorce on the mental health of young adults: A developmental perspective. Child Development. 1995;66:1614–1634. doi:10.2307/1131900. [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Alcohol disorders in young adulthood: Effects of transitions into adult roles. Journal of Health and Social Behavior. 1996;37:339–349. doi:10.2307/2137261. [PubMed] [Google Scholar]
- Coie JD, Watt NF, West SG, Hawkins JD, Asarnow JR, Markman HJ, Ramey SL, Shure MB, Long B. The science of prevention: A conceptual framework and some directions for a national research program. American Psychologist. 1993;48:1013–1022. doi: 10.1037//0003-066x.48.10.1013. doi:10.1037/0003-066x.48.10.1013. [DOI] [PubMed] [Google Scholar]
- Compton WM, Cottler LB. The Comprehensive Handbook of Psychological Assessment, Volume 2: Personality Assessment. In: Hersen M, Segal MJ, editors. The diagnostic interview schedule. John Wiley & Sons, Inc.; New York: 2000. [Google Scholar]
- Cummings EM, Davies PT, Campbell SB. Developmental Psychopathology and Family Process: Theory, Research, and Clinical Implications. The Guilford Press; New York: 2000. New directions in the study of parenting and child development. pp. 200–250. [Google Scholar]
- Dawson-McClure SR, Sandler IN, Wolchik SA, Millsap RE. Risk as a moderator of the effects of prevention programs for children from divorced families: A six-year longitudinal study. Journal of Abnormal Child Psychology. 2004;32:175–190. doi: 10.1023/b:jacp.0000019769.75578.79. doi:0091-0627/04/0400-0175/0. [DOI] [PubMed] [Google Scholar]
- DeGarmo DS, Forgatch MS. Early development of delinquency within divorced families: evaluating a randomized preventive intervention trial. Developmental Science. 2005;8:229–239. doi: 10.1111/j.1467-7687.2005.00412.x. doi:10.1111/j.1467-7687.2005.00412.x. [DOI] [PubMed] [Google Scholar]
- DeGarmo DS, Patterson GR, Forgatch MS. How do outcomes in a specified parent training intervention maintain or wane over time? Prevention Science. 2004;5:73–89. doi: 10.1023/b:prev.0000023078.30191.e0. doi:10.1023/B:PREV.0000023078.30191.e0. [DOI] [PubMed] [Google Scholar]
- Eitle D. Parental gender, single-parent families, and delinquency: Exploring the moderating influence of race/ethnicity. Social Science Research. 2006;35:727–748. doi:10.1016/j.ssresearch.2005.06.003. [Google Scholar]
- Fabricius WV, Braver SL, Diaz P, Velez CE. Custody and parenting time: Links to family relationships and well-being after divorce. In: Lamb ME, editor. The role of the father in child development. 5th ed. John Wiley & Sons; Hoboken, NJ: 2010. pp. 201–240. [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT. Parental separation, adolescent psychopathology, and problem behaviors. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:1122–1131. doi: 10.1097/00004583-199410000-00008. doi:10.1097/00004583-199410000-00008. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, DeGarmo DS. Parenting through change: An effective prevention program for single mothers. Journal of Consulting & Clinical Psychology. 1999;67:711–724. doi: 10.1037//0022-006x.67.5.711. doi:10.1037/0022-006X.67.5.711. [DOI] [PubMed] [Google Scholar]
- Forgatch MS, Patterson GR, DeGarmo DS, Beldavs ZG. Testing the Oregon delinquency model with 9-year follow-up of the Oregon Divorce Study. Development and Psychopathology. 2009;21:637–660. doi: 10.1017/S0954579409000340. doi:doi:10.1017/S0954579409000340. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. doi:10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Gribble JN, Miller HG, Rogers SM, Turner CF. Interview mode and measurement of sexual behaviors: Methodological issues. Journal of Sex Research. 1999;36:16–24. doi: 10.1080/00224499909551963. doi:10.1080/00224499909551963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerney BG, Coufal J, Vogelsong E. Relationship enhancement versus a traditional approach to therapeutic/preventative/enrichment parent-adolescent programs. Journal of Consulting and Clinical Psychology. 1981;49:927–939. doi: 10.1037//0022-006x.49.6.927. doi:10.1037/0022-006x.49.6.927. [DOI] [PubMed] [Google Scholar]
- Guo G, Zhao H. Multilevel modeling for binary data. Annual Review of Sociology. 2000;26:441–462. doi:10.1146/annurev.soc.26.1.441. [Google Scholar]
- Hanson GR, Li T. Public health implications of excessive alcohol consumption. Journal of the American Medical Association. 2003;289:1031–1032. doi: 10.1001/jama.289.8.1031. doi:10.1001/jama.289.8.1031. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for the Self-Perception Profile of Children (Revision of the Perceived Competence Scale for Children) University of Denver, CO.; 1985. Unpublished manuscript. [Google Scholar]
- Heffler S, Smith S, Keehan S, Clemens MK, Zezza M, Truffer C. Health Affairs. Advance online publication; 2004. Health Spending projections through 2013. doi:10.1377/hlthaff.w4.79. [DOI] [PubMed] [Google Scholar]
- Hetherington EM. Social capital and the development of youth from nondivorced, divorced and remarried families. In: Laursen B, Collins WA, editors. Relationships as developmental contexts: Vol 30. The Minnesota symposia on child psychology. Lawrence Erlbaum; Mahwah, NJ: 1999. pp. 177–209. [Google Scholar]
- Institute of Medicine . Reducing risks for mental disorders: Frontiers for preventive intervention research. National Academy Press; Washington, DC: 1994. [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG. Smoking, drinking and illicit drug use among American secondary school students, college students, and young adults, 1975-1991. National Institute on Drug Abuse; Rockvile, MD: 1993. NIH Publication No. 93-3481. [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. National Institute on Drug Abuse; Bethesda, MD: 2008. Monitoring the future national survey results on drug use, 1975–2007. Vol. 2 College students and adults ages 19-45. (NIH Publication No. 08-6418B) [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Institute for Social Research, The University of Michigan; Ann Arbor, MI: 2011. Monitoring the Future national survey results on drug use, 1975-2010. Volume I: Secondary school students and Monitoring the Future national survey results on drug use, 1975-2010. Volume II: College students and adults ages 19-50. [Google Scholar]
- Jurs DG, Glass GV. The effect of experimental mortality on the internal and external validity of the randomized comparative experiment. Journal of Experimental Education. 1971;40:62–66. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. doi:10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. doi:10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the U.S. National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. doi:10.1017/S0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The Children's Depression Inventory (CDI). Psychopharmacology Bulletin. 1985;21:995–999. [PubMed] [Google Scholar]
- Lonczak HS, Abbott RD, Hawkins JD, Kosterman R, Catalano RF. Effects of the Seattle Social Development Project on sexual behavior, pregnancy, birth, and sexually transmitted disease outcomes by age 21 years. Archives of Pediatrics & Adolescent Medicine. 2002;156:438–447. doi: 10.1001/archpedi.156.5.438. doi:10.1001/archpedi.156.5.438. [DOI] [PubMed] [Google Scholar]
- Luppa M, Heinrich S, Angermeyer MC, König H-H, Riedel-Heller SG. Cost-of-illness studies of depression: A systematic review. Journal of Affective Disorders. 2007;98(1–2):29–43. doi: 10.1016/j.jad.2006.07.017. doi:10.1016/j.jad.2006.07.017. [DOI] [PubMed] [Google Scholar]
- Maas CJM, Hox JJ. Sufficient Sample Sizes for Multilevel Modeling. Methodology: European Journal of Research Methods for the Behavioral and Social Sciences. 2005;1(3):86–92. doi:10.1027/1614-2241.1.3.86. [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: maintenance strategies in the treatment of addictive behaviors. Guilford Press; New York, NY: 1985. [Google Scholar]
- Muñoz RF, Beardslee WR, Leykin Y. Major depression can be prevented. American Psychologist. 2012;67:285–295. doi: 10.1037/a0027666. doi:10.1037/a0027666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide: The comprehensive modeling program for applied researchers. 5th ed. Muthén & Muthén; Los Angeles, CA: 1998-2010. [Google Scholar]
- National Center for Health Statistics Marriage and divorce. 2008 Retrieved from http://www.cdc.gov/nchs/fastats/divorce.htm.
- National Research Council and Institute of Medicine . Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Committee on the Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults: Research Advances and Promising Interventions. In: O'Connell Mary Ellen, Boat Thomas, Warner Kenneth E., editors. Board on Children, Youth, and Families, Division of Behavioral and Social Sciences and Education. National Academics Press; Washington, D.C.: 2009. [PubMed] [Google Scholar]
- Novaco RA. Anger control: the development and evaluation of an experimental treatment. D.C. Heath; Lexinton, MA: 1975. [Google Scholar]
- Patterson GR. Parents and teachers as change agents: a social learning approach. In: Olson D, editor. Treating relationships. Graphic Press; Lake Mills, IA: 1976. pp. 189–215. [Google Scholar]
- Paxton R, Valois R, Drane J. Is there a relationship between family structure and substance use among public middle school students? Journal of Child and Family Studies. 2007;16:593–605. doi:10.1007/s10826-006-9109-y. [Google Scholar]
- Pedro-Carroll JL, Cowen EL. The Children of Divorce Intervention Program: An investigation of the efficacy of a school-based prevention program. Journal of Consulting and Clinical Psychology. 1985;53:603–611. doi: 10.1037//0022-006x.53.5.603. doi:10.1037/0022-006x.53.5.603. [DOI] [PubMed] [Google Scholar]
- Pedro-Carroll JL, Sutton SE, Wyman PA. A two-year follow-up evaluation of a preventive intervention for young children of divorce. School Psychology Review. 1999;28:467–476. [Google Scholar]
- Program for Prevention Research . The divorce adjustment project externalizing scale. Arizona State University; 1985. Unpublished manual. [Google Scholar]
- Reynolds AJ, Temple JA, Ou S-R, Robertson DL, Mersky JP, Topitzes JW, Niles MD. Effects of a school-based, early childhood intervention on adult health and well-being: A 19-year follow-up of low-income families. Archives of Pediatrics & Adolescent Medicine. 2007;161:730–739. doi: 10.1001/archpedi.161.8.730. doi:10.1001/archpedi.161.8.730. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of Children's Manifest Anxiety. Journal of Abnormal Child Psychology. 1978;6:271–280. doi: 10.1007/BF00919131. doi:10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Robin LN, Cottler LB, Bucholz KK, Compton WM, North CS, Rourke KM. Diagnostic Interview Schedule for the DSM-IV (DIS-IV) Washington University; St. Louis MO: 2000. Available from http://epi.wustl.edu/DIS/DIShome.htm. [Google Scholar]
- Sameroff AJ. Developmental systems and psychopathology. Development and Psychopathology. 2000;12:297–312. doi: 10.1017/s0954579400003035. doi:10.1017/S0954579400003035. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Schoenfelder E, Wolchik SA, MacKinnon DP. Long-term impact of prevention programs to promote effective parenting: Lasting effects but uncertain processess. Annual Review of Psychology. 2011;62:299–329. doi: 10.1146/annurev.psych.121208.131619. doi:10.1146/annurev.psych.121208.131619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute . SAS/STAT® 9.22 User's Guide. SAS Institute Inc.; Cary, NC: 2010. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. doi:10.1037/1082-989x.7.2.147. [PubMed] [Google Scholar]
- Schulenberg JE, Sameroff A, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and Psychopathology. 2004;16:799–806. doi: 10.1017/s0954579404040015. doi:doi:10.1017/S0954579404040015. [DOI] [PubMed] [Google Scholar]
- Schweinhart LJ, Weikart DP. The High/Scope preschool curriculum comparison study through age 23. Early Childhood Research Quarterly. 1997;12:117–143. doi:10.1016/s0885-2006(97)90009-0. [Google Scholar]
- Scott KG, Mason CA, Chapman DA. The use of epidemiological methodology as a means of influencing public policy. Child Development. 1999;70:1263–1272. doi:10.1111/1467-8624.00091. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. doi:10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Walitzer KS, Wood PK, Brent EE. Characteristics of children of alcoholics: Putative risk factors, substance use and abuse, and psychopathology. Journal of Abnormal Psychology. 1991;100:427–448. doi: 10.1037//0021-843x.100.4.427. doi:10.1037/0021-843X.100.4.427. [DOI] [PubMed] [Google Scholar]
- Sigal AB, Wolchik SA, Tein JY, Sandler IN. Enhancing youth outcomes following parental divorce: A longitudinal study of the effects of the New Beginnings Program on educational and occupational goals. Journal of Clinical Child & Adolescent Psychology. 2012;41:150–165. doi: 10.1080/15374416.2012.651992. doi: 10.1080/15374416.2012.651992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolberg AL, Garrison KM. Evaluating a primary prevention program for children of divorce. American Journal of Community Psychology. 1985;13:111–124. doi: 10.1007/BF00905724. doi:10.1007/bf00905724. [DOI] [PubMed] [Google Scholar]
- Stolberg AL, Mahler J. Enhancing treatment gains in a school-based intervention for children of divorce through skill training, parental involvement, and transfer procedures. Journal of Consulting and Clinical Psychology. 1994;62:147–156. doi: 10.1037//0022-006x.62.1.147. doi:10.1037/0022-006x.62.1.147. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results From the 2007 National Survey on Drug Use and Health: National Findings. Substance Abuse and Mental Health Services Administration; Office of Applied Studies; Rockville, MD: 2008. NSDUH Series H-36, HHS Publication No. SMA 08-4343. [Google Scholar]
- Tein J-Y, Sandler IN, MacKinnon DP, Wolchik SA. How did it work? Who did it work for? Mediation and mediated moderation of a preventive intervention for children of divorce. Journal of Consulting and Clinical Psychology. 2004;72:617–624. doi: 10.1037/0022-006X.72.4.617. doi:10.1037/0022-006X.72.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA. What are the costs of marital conflict and dissolution to children's physical health? Clinical Child and Family Psychology Review. 2004;7:29–57. doi: 10.1023/b:ccfp.0000020191.73542.b0. doi:10.1023/B:CCFP.0000020191.73542.b0. [DOI] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall G, Azevedo K. Longitudinal effects of a universal family-focused intervention on growth patterns of adolescent internalizing symptoms and polysubstance use: Gender comparisons. Journal of Youth and Adolescence. 2007;36:725–740. doi:10.1007/s10964-007-9179-1. [Google Scholar]
- U.S. Census Bureau . Current Population Survey. 2004 Annual Social and Economic Supplement. U.S. Census Bureau; Washington, DC: 2005. Retrieved from http://www.census.gov/population/socdemo/hh-fam/ms2.pdf. [Google Scholar]
- U.S. Office of National Drug Control Policy . The economic costs of drug abuse in the United States, 1992-1998. Executive Office of the President; Washington, DC: 2001. [Google Scholar]
- Vélez CE, Wolchik SA, Tein JY, Sandler I. Protecting children from the consequences of divorce: A longitudinal study of the effects of parenting on children's coping processes. Child development. 2011;82:244–257. doi: 10.1111/j.1467-8624.2010.01553.x. doi: 10.1111/j.1467-8624.2010.01553.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolchik SA, Sandler I, Weiss L, Winslow EB. New Beginnings: An empirically-based program to help divorced mothers promote resilience in their children. In: Briesmeister JM, Schaefer CE, editors. Handbook of parent training: Helping parents prevent and solve problem behaviors. John Wiley & Sons; New York: 2007. pp. 25–62. [Google Scholar]
- Wolchik SA, Sandler IN, Millsap RE, Plummer BA, Greene SM, Anderson ER, Haine RA. Six-year follow-up of a randomized, controlled trial of preventive interventions for children of divorce. Journal of the American Medical Association. 2002;288:1874–1881. doi: 10.1001/jama.288.15.1874. doi:10.1001/jama.288.15.1874. [DOI] [PubMed] [Google Scholar]
- Wolchik SA, West SG, Sandler IN, Tein J-Y, Coatsworth D, Lengua L, Griffin WA. An experimental evaluation of theory-based mother and mother-child programs for children of divorce. Journal of Consulting and Clinical Psychology. 2000;68:843–856. doi:10.1037/0022-006X.68.5.843. [PubMed] [Google Scholar]
- Wolchik SA, West SG, Westover S, Sandler IN, Martin A, Lustig J, Fisher J. The children of divorce parenting intervention: Outcome evaluation of an empirically based program. American Journal of Community Psychology. 1993;21:293–331. doi: 10.1007/BF00941505. doi:10.1007/BF00941505. [DOI] [PubMed] [Google Scholar]
- Zhou Q, Sandler IN, Millsap RE, Wolchik SA, Dawson-McClure SR. Mother-child relationship quality and effective discipline as mediators of the 6-year effects of the New Beginnings Program for children from divorced families. Journal of Consulting and Clinical Psychology. 2008;76:579–594. doi: 10.1037/0022-006X.76.4.579. doi:10.1037/0022-006X.76.4.579. [DOI] [PMC free article] [PubMed] [Google Scholar]