Abstract
Mazabraud's syndrome is a rare disorder characterized by the association of single or multiple intramuscular myxomas with fibrous dysplasia. Here, we present the first case of Mazabraud's syndrome visualized on 18F-FDG PET/CT with histopathological confirmation of the myxoma. Our case demonstrates a slightly increased FDG uptake (SUVmax 2.1) within the myxomas and a moderately to highly increased tracer uptake (SUVmax 7.0) within the fibrous dysplastic lesions. The typical histological appearance of the intramuscular myxoma confirmed the radiological diagnosis. Further, we discuss the imaging findings and the histopathological features of this rare case with a review of the related literature.
Keywords: Mazabraud's syndrome, fibrous dysplasia, myxoma, fluorodeoxyglucose F18 (18F-FDG PET/CT), MRI
Mazabraud's syndrome is a rare benign disorder characterized by the association of single or multiple intramuscular myxomas with fibrous dysplasia, which can develop in a single bone (monostotic) or in multiple bones (polyostotic). Soft tissue myxomas are benign mesenchymal tumors, and fibrous dysplasia is a benign, intra-medullary, fibro-osseous lesion (1). The first case of Mazabraud's syndrome was described by Henschen (2) in 1926, and a pattern of association between fibrous dysplasia and soft tissue myxomas was presented by Mazabraud et al. (3) in 1967. Today, approximately 80 cases of Mazabraud's syndrome have been reported (4), but the appearance of the syndrome by 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) has only been described in one case (5). To our knowledge, we present here the first case of Mazabraud's syndrome visualized on 18F-FDG PET/CT with a histopathological confirmation of the myxoma. In addition, we review the clinical, imaging, and histopathological features of this rare syndrome.
Case report
A 54-year-old woman was referred to our clinic with a complaint of pain in her right gluteal region with radiation to her foot that had been present for 2 months. The pain was most pronounced during sitting and jogging, and a physiotherapist detected a mass in the proximal right semitendinosus muscle. She had no history of trauma and was otherwise healthy. However, she had a previous history of breast fibroadenomatosis, carcinoma in situ of the uterine cervix, and uterine fibroma.
Conventional X-rays of the right femur demonstrated a 9.5 × 3.3 cm intra-osseous cystic lesion with sclerotic margins at the right femoral neck in the subtrochanteric and metaphyseal region (Fig. 1a). A similar lesion was observed within the right ileum above the acetabulum (Fig. 1b). The lesions were interpreted as being consistent with fibrous dysplasia. Ultrasonography of the right gluteal region revealed a 3 × 4.2 × 4.5 cm hypoechoic soft tissue mass located in the musculature below the ischial tuberosity (not shown). There was no involvement of the adjacent bone. Moreover, the patient underwent magnetic resonance imaging (MRI) of her pelvis and right thigh with and without intravenous administration of a gadolinium-containing contrast agent. The examination showed multiple cystic and solid tumor-like lesions within the bones and muscles. The largest of the soft tissue masses was located in the proximal right adductor magnus muscle and measured 5.5 × 4.4 × 2.9 cm. Two similar lesions were observed in the proximal right adductor brevis muscle with diameters of 1.4 and 1 cm, respectively, and a lesion extending 1.3 cm was located in the rectus femoris muscle. The muscle masses showed low signal intensity on T1-weighted images and high signal intensity on T2-weighted images and short T1 inversion recovery (STIR) images. The signal intensity increased after contrast injection. Skeletal changes related to fibrous dysplasia were evident within the right ilium and in the proximal diaphysis of the right femur measuring 7 and 8 cm, respectively. The bone lesions demonstrated a slight thinning of the cortical bone but no real destruction. The bony lesions were typical of fibrous dysplasia, but the diagnosis of the soft tissue lesions was uncertain, including differentials such as soft tissue sarcoma, lymphoma, and neurofibroma (Fig. 2).
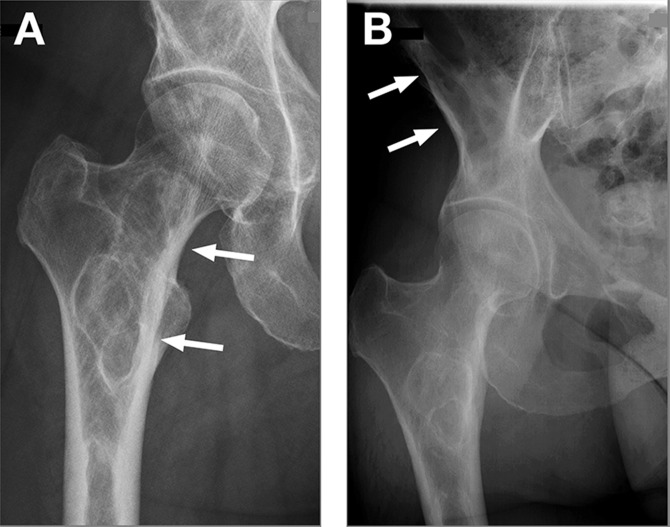
Fig. 1.
(a, b) Anteroposterior radiographs of the proximal femur and right hip showing radiolucent cystic lesions with sclerotic margins and no periosteal reaction, findings in keeping with fibrous dysplasia (straight arrows)
Fig. 2.
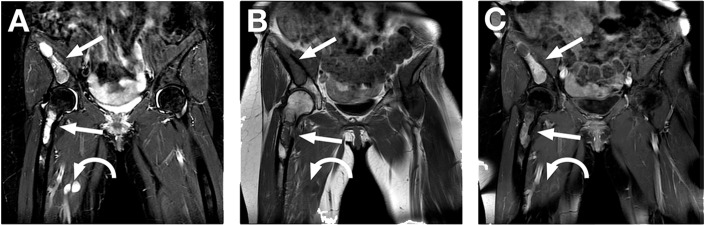
(a) Coronal STIR, (b) T1, and (c) T1-weighted with fat-sat and gadolinium (Gd) contrast agent MR images. Bony lesions with high signal on STIR, low signal on T1, and heterogeneous contrast enhancement after Gd injection (straight arrows) can be observed. Soft tissue lesions with high signal on STIR, low signal on T1, and a mixture of rim and central contrast enhancement after Gd injection (curved arrows) can also be observed
Ultimately, the patient underwent an 18F-FDG PET/CT of the neck, chest, abdomen, and thighs at our clinic. The patient received an intravenous injection of 370 MBq of 18F-FDG at rest in dimmed ambient light with minimal background noise. The patient was asked to fast for 6 h before the bolus injection of FDG (water only). One hour after the injection, the PET/CT scan was performed under standard resting condition using a 64-channel PET/CT scanner (Discovery VCT, GE Healthcare, Milwaukee, WI, USA). Images were acquired for 2.5 min in three-dimensional (3D) mode and were filtered and reconstructed using standard techniques. The examination demonstrated a slightly increased FDG uptake (standardized uptake value [SUV] max 2.1) within the solid-appearing regions of the intramuscular lesions in the right hip and thigh and the findings were interpreted as intramuscular myxomas. Moreover, we observed moderately to highly increased tracer uptake (SUVmax 7.0) within the right ilium and the proximal diaphysis of the right femur that was consistent with fibrous dysplasia. The accompanying CT findings were concordant, demonstrating multiloculated and expansive intramedullary lesions with areas of both thickening and thinning of the cortical bone but without cortical destruction. The areas with FDG-uptake on the PET/CT also showed contrast enhancement on the MRI with intravenous gadolinium (Figs. 3 and 4). The scan showed no signs of malignancy; thus, enlarged lymph nodes or FDG uptake in lymph nodes was not observed in the neck, chest, and abdomen. The spleen was of normal volume, homogeneous and without focal changes or uptake of FDG. The bone marrow had no signs of lymphomatous infiltration. Overall, the PET/CT findings were interpreted as consistent with Mazabraud's syndrome.
Fig. 3.
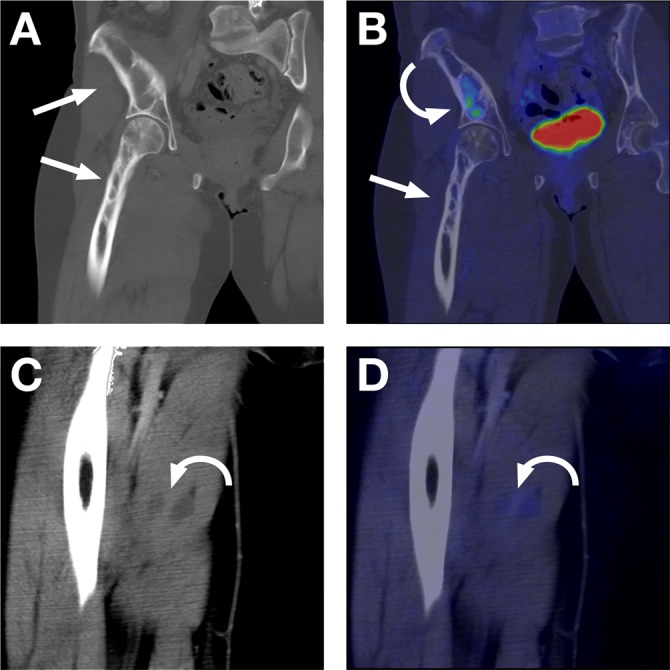
18F-FDG PET/CT. (a) Coronal CT with a bone window showing multi-loculated expansile intramedullary fibrous dysplasia lesions in the ileum and proximal part of the femur (straight arrows). (b) Fused PET/CT with increased FDG uptake (SUVmax 7.0) only in the lower region of the fibrous dysplasia lesion in the right ileum (curved arrow). Notice that the region of the fibrous dysplasia taking up the FDG corresponds to the region on the coronal MR image in Fig. 2c that is the most enhanced by the Gd contrast agent. (c) Coronal CT with a soft tissue window showing the low-density myxomas in the medial thigh muscles (curved arrow). (d) Fused PET/CT showing slightly increased FDG uptake in the myxomas (curved arrow)
Fig. 4.
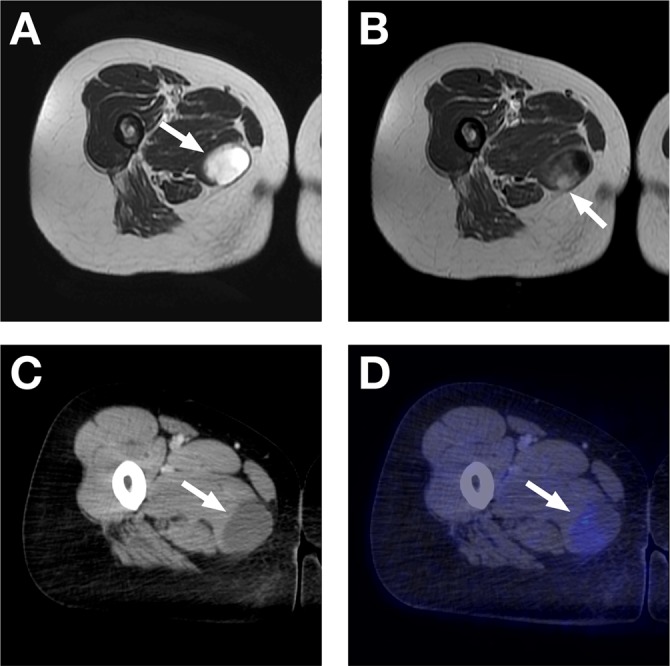
MRI and 18F-FDG PET/CT. (a) Axial T2-weighted MR image with high signal, partly cystic-appearing soft tissue lesion in the medial thigh muscle (straight arrow). (b) Axial T1-weighted MR image after intravenous Gd agent administration with contrast enhancement of the more solid-appearing region of the myxoma (straight arrow). (c) Axial CT with a soft tissue window showing the low-density, almost cystic-appearing lesion in the medial thigh muscle (straight arrow). (d) Fused PET/CT with slightly increased FDG uptake (SUV max 2.1) in the apparently more solid region of the myxoma. Notice that the region of the myxoma taking up the FDG corresponds to the Gd-enhanced region on the MRI (straight arrow)
After the scans, the intramuscular mass located in the proximal right adductor magnus muscle was excised. It had well-defined borders and measured 6 × 5 × 3 cm. Histological examination of the lesion supported the radiological diagnosis of myxoma (Fig. 5).
Fig. 5.
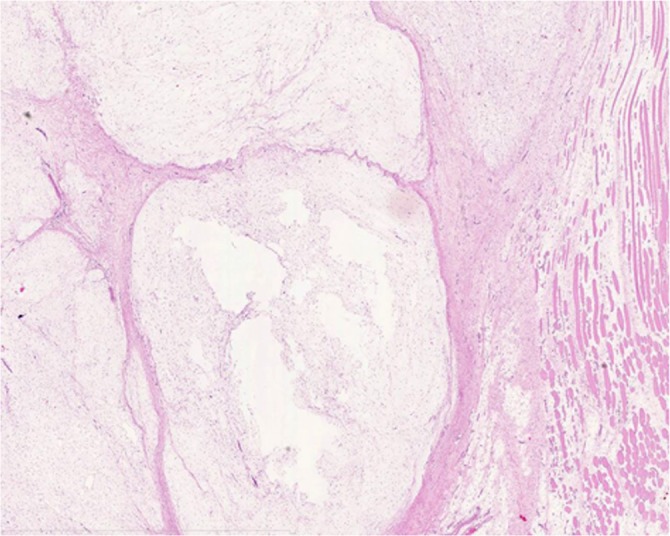
Typical histological appearance of intramuscular myxoma: well-circumscribed, paucicellular lobulated myxoid tumour with skeletal muscle involvement
Discussion
The present case of Mazabraud's syndrome is quite typical. Most patients with Mazabraud's syndrome have multiple intramuscular myxomas that tend to be located in the lower extremities with a curious predilection for the right limb. Moreover, the myxomas are most often located in the vicinity of the bone lesions (6). The syndrome is more common with the polyostotic form of fibrous dysplasia, but monostotic involvement has been reported as well. In general, the onset of fibrous dysplasia predates the appearance of the intra-muscular myxomas, and the soft-tissue lesions become apparent many years later, usually in the fifth or sixth decade of life. The disease is more frequent in women than men and patients are often asymptomatic. However, complications such as skeletal deformities, fractures and pain can occur (1, 6, 7). The etiology of Mazabraud's syndrome is unknown. The affliction is believed to be caused by a basic metabolic error of both soft and bone tissues during the initial growth period (8). A role for somatic gene mutation has been suggested, and molecular genetic analyses have shown point mutations in the GNAS-1 gene encoding a signal transduction protein that regulates the cellular cyclic adenosine monophosphate level in intramuscular myxomas (9). In the literature, three cases of gynecological tumors in patients with Mazabraud's syndrome have been reported (10). Our patient had a history of fibroadenomatosis mammae, carcinoma in situ of the uterine cervix, and uterine fibroma. However, it is difficult to know whether these tumors were part of the disease spectrum.
The image findings in our patient were in agreement with previously reported cases. On radiographs, fibrous lesions exhibit lucency with a ground glass appearance surrounded by condensed bone. The borders are well-defined, and the cortex is usually intact, but it may be thinned due to expansive nature of the lesion (7, 11). MRI of fibrous dysplasias shows homogenous low signal intensity on T1-weighted images, whereas the signal may be mixed or high on T2-weighted images. The sclerotic rim is observed as a band of low signal intensity on both T1- and T2-weighted sequences (11, 12). CT helps to indicate the extent of bone involvement and demonstrates the mild osseous expansion associated with the characteristic ground glass appearance (5, 7, 11).
Ultrasonography of myxomas demonstrates well-defined, hypoechoic masses consisting of a large number of small, fluid-filled spaces conglomerating to form a microcystic pattern (13). By MRI myxomas demonstrate a sharply defined contour. The muscle masses show low signal intensity on T1-weighted images and high signal intensity on T2-weighted images and STIR images. The signal intensity increases after intravenous injection of gadolinium contrast agent (7). CT scans of myxomas typically display a homogeneous, well-circumscribed mass with low attenuation. The appearance of Mazabraud's syndrome by 18F-FDG PET/CT, reported in one patient previously (5), was in agreement with our findings. A relatively low but not insignificant 18F-FDG uptake in the multiple intramuscular myxomas was described with a SUV range between 1.3 and 2.6. In our case, the SUVmax was 2.1. Further, increased tracer uptake within several bones affected by fibrous dysplasia was reported. The SUV range for the fibrous dysplasia lesions was between 3.3 and 19.2. Our case had a SUVmax of 7.0.
Histologically, fibrous dysplasia is characterized by the replacement of normal bone with fibrous tissue and irregular spicules of woven bone. Myxomas are relatively hypocellular with a myxoid matrix and loose reticular fibres. Collagenous and vascular structures are sparse. The cells have a stellate shape with small hyperchromatic pyknotic nuclei and scant cytoplasm (11, 14).
The treatment of Mazabraud's syndrome is dependent on the extent of the lesions. Because the myxomas are benign, conservative management is indicated. Yet, myxomas should be excised if pain or pressure symptoms develop. Simple local excision is sufficient in most cases. However, a proper histopathological investigation of the lesions should also be carried out to exclude differentials such as primary malignancy or metastatic tumour (11, 15). Fibrous dysplasia progresses slowly and has a favorable prognosis if the involvement is local. Treatment is usually conservative and aims to prevent skeletal deformity and fracture (1, 11). Bisphosphonates may be helpful in relieving pain and possibly in reconstituting lesions with normal bone (16). Surgical intervention is indicated for severe and progressive disease with persistent pain, skeletal deformity, or danger of fracture or pathological fracture (1, 11). Although Mazabraud's syndrome is benign, postoperative follow-up should be undertaken to detect other myxomas that may not yet be clinically detectable or local recurrences of myxomas after incomplete excision (17). Malignant transformation of a myxoma has not been reported (15) but six cases of malignant transformation of a fibrous dysplastic lesion into osteogenic sarcoma in patients with Mazabraud's syndrome have been reported supporting the necessity of clinical follow-up (18–23). However, the significance of osteosarcomatous transformation in Mazabraud's syndrome is unclear.
Several benign lesions such as myxolipoma, myxoid neurofibroma, and myxochondroma, as well as richly myxoid malignant tumors may show regions that resemble intramuscular myxoma. Myxoid liposarcoma, myxoid malignant fibrous histiocytoma, low grade fibromyxoid sarcoma, extraskeletal myxoid chondrosarcoma, and botryoid type rhabdomyosarcoma are some of the malignant lesions to consider on the differential diagnosis of myxoma (15). In addition, many different lesions such as enchondroma, aneurysmal bone cyst, chondrosarcoma, simple bone cyst, osteosarcoma, non-ossifying fibroma, and medullary bone infarct should be considered in the radiographic differential diagnosis of fibrous dysplasia (11).
In conclusion, radiologists need to be aware of Mazabraud's syndrome as an association of fibrous dysplasia and soft tissue myxomas in order to secure appropriate management of the patient and prevent misdiagnosis of this benign syndrome as a malignant condition.
References
- 1. van der Wal WA, Unal H, de Rooy JW, et al. Fibrous dysplasia of bone associated with soft-tissue myxomas as well as an intra-osseous myxoma in a woman with mazabraud's syndrome: A case report. J Med Case Reports 2011;5:239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Henschen F Fall von ostitis fibrosa mit multiplen tumoren in der umgebenden muskulatur. Verh Dtsch Ges Pathol 1926;21:93–7 [Google Scholar]
- 3. Mazabraud A, Semat P, Roze R Apropos of the association of fibromyxomas of the soft tissues with fibrous dysplasia of the bones. Presse Med 1967;75:2223–8 [PubMed] [Google Scholar]
- 4. Gaumetou E, Tomeno B, Anract P Mazabraud's syndrome. A case with multiple myxomas. Orthop Traumatol Surg Res 2012;98:455–60 [DOI] [PubMed] [Google Scholar]
- 5. Singnurkar A, Phancao JP, Chatha DS, et al. The appearance of mazabraud's syndrome on 18F-FDG PET/CT. Skeletal Radiol 2007;36:1085–9 [DOI] [PubMed] [Google Scholar]
- 6. Sundaram M, McDonald DJ, Merenda G Intramuscular myxoma: A rare but important association with fibrous dysplasia of bone. Am J Roentgenol 1989;153:107–8 [DOI] [PubMed] [Google Scholar]
- 7. Iwasko N, Steinbach LS, Disler D, et al. Imaging findings in mazabraud's syndrome: Seven new cases. Skeletal Radiol 2002;31:81–7 [DOI] [PubMed] [Google Scholar]
- 8. Wirth WA, Leavitt D, Enzinger FM Multiple intramuscular myxomas. another extraskeletal manifestation of fibrous dysplasia. Cancer 1971;27:1167–73 [DOI] [PubMed] [Google Scholar]
- 9. Okamoto S, Hisaoka M, Ushijima M, et al. Activating gs(alpha) mutation in intramuscular myxomas with and without fibrous dysplasia of bone. Virchows Arch 2000;437:133–7 [DOI] [PubMed] [Google Scholar]
- 10. Faivre L, Nivelon-Chevallier A, Kottler ML, et al. Mazabraud syndrome in two patients: Clinical overlap with McCune-albright syndrome. Am J Med Genet 2001;99:132–6 [DOI] [PubMed] [Google Scholar]
- 11. Kabukcuoglu F, Kabukcuoglu Y, Yilmaz B, et al. Mazabraud's syndrome: Intramuscular myxoma associated with fibrous dysplasia. Pathology & Oncology Research 2004;10:121–3 [DOI] [PubMed] [Google Scholar]
- 12. Jee WH, Choi KH, Choe BY, et al. Fibrous dysplasia: MR imaging characteristics with radiopathologic correlation. Am J Roentgenol 1996;167:1523–7 [DOI] [PubMed] [Google Scholar]
- 13. Fornage BD, Romsdahl MM Intramuscular myxoma: Sonographic appearance and sonographically guided needle biopsy. J Ultrasound Med 1994;13:91–4 [DOI] [PubMed] [Google Scholar]
- 14. Szendroi M, Rahoty P, Antal I, et al. Fibrous dysplasia associated with intramuscular myxoma (mazabraud's syndrome): A long-term follow-up of three cases. J Cancer Res Clin Oncol 1998;124:401–6 [DOI] [PubMed] [Google Scholar]
- 15. Kabukcuoglu F, Kabukcuoglu Y, Yilmaz B, et al. Mazabraud's syndrome: Intramuscular myxoma associated with fibrous dysplasia. Pathol Oncol Res 2004;10:121–3 [DOI] [PubMed] [Google Scholar]
- 16. Lane JM, Khan SN, O'Connor WJ, et al. Bisphosphonate therapy in fibrous dysplasia. Clin Orthop Relat Res 2001;382:6–12 [DOI] [PubMed] [Google Scholar]
- 17. Court-Payen M, Ingemann Jensen L, Bjerregaard B, et al. Intramuscular myxoma and fibrous dysplasia of bone–mazabraud's syndrome. A case report. Acta Radiol 1997;38:368–71 [DOI] [PubMed] [Google Scholar]
- 18. Witkin GB, Guilford WB, Siegal GP Osteogenic sarcoma and soft tissue myxoma in a patient with fibrous dysplasia and hemoglobins JBaltimore and S. Clin Orthop Relat Res 1986;204:245–52 [PubMed] [Google Scholar]
- 19. Lopez-Ben R, Pitt MJ, Jaffe KA, et al. Osteosarcoma in a patient with McCune-albright syndrome and mazabraud's syndrome. Skeletal Radiol 1999;28:522–6 [DOI] [PubMed] [Google Scholar]
- 20. Jhala DN, Eltoum I, Carroll AJ, et al. Osteosarcoma in a patient with McCune-albright syndrome and mazabraud's syndrome: A case report emphasizing the cytological and cytogenetic findings. Hum Pathol 2003;34:1354–7 [DOI] [PubMed] [Google Scholar]
- 21. Crawford EA, Brooks JS, Ogilvie CM Osteosarcoma of the proximal part of the radius in mazabraud syndrome. A case report. J Bone Joint Surg Am 2009;91:955–60 [DOI] [PubMed] [Google Scholar]
- 22. Roze R, Mazabraud A, Semat P Fibrous dysplasia of bone and myxomas of the soft tissues. localized sarcomatous degeneration. J Radiol Electrol Med Nucl 1967;48:527–36 [PubMed] [Google Scholar]
- 23. Nguyen BD, Ram PC Mazabraud's syndrome with sarcomatous transformation: Scintigraphic and radiologic imaging. Clin Nucl Med 2005;30:829–30 [DOI] [PubMed] [Google Scholar]