Abstract
Background:
Nonadherence to medication is a recognized problem and may be the most challenging aspect of treatment.
Methods:
We performed a systematic review of factors that influence adherence and the consequences of nonadherence to the patient, healthcare system and society, in patients with schizophrenia. Particular attention was given to the effect of nonadherence on hospitalization rates, as a key driver of increased costs of care. A qualitative systematic literature review was conducted using a broad search strategy using disease and adherence terms. Due to the large number of abstracts identified, article selection was based on studies with larger sample sizes published after 2001. Thirty-seven full papers were included: 15 studies on drivers and 22 on consequences, of which 12 assessed the link between nonadherence and hospitalization.
Results:
Key drivers of nonadherence included lack of insight, medication beliefs and substance abuse. Key consequences of nonadherence included greater risk of relapse, hospitalization and suicide. Factors positively related to adherence were a good therapeutic relationship with physician and perception of benefits of medication. The most frequently reported driver and consequence were lack of insight and greater risk of hospitalization respectively.
Conclusions:
Improving adherence in schizophrenia may have a considerable positive impact on patients and society. This can be achieved by focusing on the identified multitude of factors driving nonadherence.
Keywords: adherence, antipsychotics, nonadherence, schizophrenia, systematic review
Introduction
Schizophrenia is a severe form of mental illness affecting about 7 per 1000 adults globally. Although the incidence is low, the prevalence of schizophrenia is high as it is a long-term chronic illness [World Health Organization, 2011]. Antipsychotic medication plays an important role in schizophrenia treatment and symptom control. Effective management of schizophrenia requires continuous long-term treatment in order to keep symptoms under control and to prevent relapse [American Psychiatric Association, 2006]. Despite the critical importance of medication, nonadherence to prescribed drug treatments has been recognized as a problem worldwide and may be the most challenging aspect of treating patients with schizophrenia [World Health Organization, 2003]. Data from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study showed that 74% of patients had discontinued medication within 18 months due to insufficient efficacy, intolerable side effects or for other reasons [Lieberman, 2005].
Nonadherence to medication includes a range of patient behaviours, from treatment refusal to irregular use or partial change of daily medication doses. Partial adherence to medication is at least as frequent as complete nonadherence [Svestka and Bitter, 2007]. There is no single theory that explains adherence issues, but rather a range of theories with their own strengths and limitations [Weiden, 2007]. Potential factors for nonadherence may be related to disease severity, treatment characteristics or even external environmental factors such as therapeutic support [Llorca, 2008]. Adherence factors may also be unique to the characteristics of schizophrenia; factors such as cognitive impairment or lack of illness insight may play an important role. A recent retrospective database study in schizophrenia [Liu-Seifert, 2012] found that the best predictor of good adherence was a significant improvement in positive symptoms, hostility and depressive symptoms, regardless of treatment.
Nonadherence to medication has a negative impact on the course of illness resulting in relapse, rehospitalization, longer time to remission, and attempted suicide [Leucht and Heres, 2006]. A recent retrospective database study which analysed data from 861 patients in Sweden [Boden, 2011] linked nonadherence to antipsychotic medication shortly after discharge to early rehospitalization. The consequences of nonadherence contribute to the already high costs of the disease to healthcare systems [Knapp et al. 2004]. Thus, nonadherence can have a substantial negative impact on patients’ health and functioning as well as a financial impact on society. Reducing nonadherence to antipsychotic medications has the potential to reduce psychiatric morbidity and costs of care substantially. That would improve the welfare of patients with schizophrenia and reduce the use of resources for acute psychotic episodes [Byerly et al. 2007]. Therefore it is important to identify the key factors contributing to nonadherence in schizophrenia, and their consequences. In addition, assessing causes and consequences of nonadherence together may highlight the importance and complexity of adherence to medication in schizophrenia. However, we are not aware of any comprehensive review of both the causes and consequences of nonadherence in schizophrenia. Furthermore, there is a need for a review that investigates whether the data allow for a quantitative assessment of the specific link between nonadherence and hospitalization.
The objective of this study was to perform a systematic review of the factors that influence adherence in schizophrenia and of the consequences of nonadherence for the patient, healthcare system and society. Particular attention was given to the effect of nonadherence on hospitalization rates, as a key driver of increased costs of care.
Methods
A systematic literature review was conducted to include English-language manuscripts published from 2000 in OVID. Four electronic databases (MEDLINE, MEDLINE In-Process, EMBASE and the Cochrane Library) were searched to identify potentially relevant articles. Conference abstracts were not included in this review. The search combined free text and medical subject headings (MeSH) disease terms with adherence terms for psychosis or schizophrenia AND adherence or compliance or persistence. As the outcomes of interest included all factors and consequences of nonadherence, no search terms were included for specific outcomes, as this may have resulted in missing some outcomes. One search was conducted for both sets of outcomes. Thus a very broad search strategy was adopted in order to avoid missing potentially relevant information, with the identification of relevant studies per outcome (i.e. nonadherence drivers or consequences) based on abstract screening [Liberati et al. 2009].
The abstract screening for identification of relevant data was based on the following predefined criteria: populations comprising adult patients with schizophrenia and disorders with psychotic features, psychosis and schizophrenia spectrum disorders; oral antipsychotic interventions were included, and subanalysis of the impact on adherence on hospitalization rates focused on studies of oral interventions comparing once daily dosing with multiple daily dosing; studies were excluded based on comparison if they were comparing interventions or drugs which were not of interest; outcomes including factors influencing adherence rates and consequences of nonadherence; study designs including phase II or III randomized controlled trials, observational studies such as prospective and retrospective studies, cross-sectional questionnaire-based studies, economic and epidemiologic studies, meta-analyses and qualitative reviews; and a focus on studies with larger sample sizes and more recent publications (publications after 2001) due to the large expected number of studies identified.
Two research facets were assessed qualitatively: drivers of nonadherence and consequences of nonadherence. In addition, for a particular consequence of nonadherence, namely hospitalization, the feasibility of quantitative meta-analysis was assessed for the link between nonadherence and hospitalization.
Results
Study selection
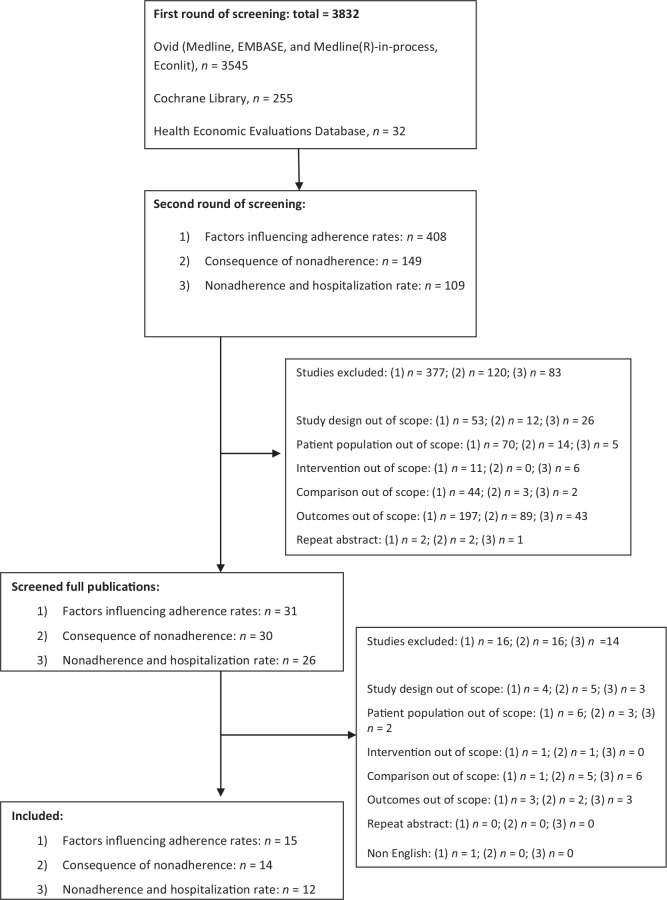
Figure 1 presents the flow chart of identified studies. The OVID search identified 3832 abstracts for screening. Due to the large number of abstracts identified and the need to answer three different research questions, the first stage of screening involved sorting the abstracts according to the three outcomes of interest: drivers of nonadherence, consequences of nonadherence, and studies on nonadherence and hospitalization rate. During this first screening, any abstracts that clearly did not match the inclusion criteria were also excluded. Thus in the second, outcome-specific, phase of screening, there were 149 potentially relevant abstracts on drivers, 408 on consequences and 109 on hospitalization due to nonadherence. There were 37 full papers included in total: 15 studies on nonadherence drivers and 22 on consequences of nonadherence, of which 12 focused on the specific link between nonadherence and hospitalization. A quantitative meta-analysis was not performed for the link between nonadherence and hospitalization, due to lack of data on comparable outcome measure. Thus, a qualitative approach was taken for all outcomes.
Figure 1.
Study selection flow diagram.
Details from the studies in this review, including study design, study population, definition of adherence and findings for key outcomes are presented in Tables 1–3.
Table 1.
Summary of findings on potential positive and negative factors influencing adherence rates.
| Author [year] | Study design | Patient population | Key potential negative factors | Key potential positive factors |
|---|---|---|---|---|
| Acosta et al. [2009] | Prospective | Schizophrenia, N=74 | Poor insight (p = 0.04), higher scores for conceptual disorganization in the PANSS items (p = 0.068) | NR |
| Ascher-Svanumet al. [2006] | Prospective | Schizophrenia, N = 1,579 | Prior poor adherence (p < 0.001), prior illicit drug use (p = 0.025), prior alcohol use (p = 0.015), prior treatment with antidepressants, and greater patient-reported, medication-related cognitive impairment (p < 0.001) | NR |
| Hudson et al. [2004] | Prospective | Schizophrenia, N = 153 | Barriers including stigma of taking medications, adverse drug reactions, forgetfulness, lack of social support (significance level NR), higher PANSS total score (p = 0.05), lower education level (p = 0.02), substance abuse (p = 0.01) | NR |
| Janssen et al. [2006] | Prospective | Schizophrenia, n = 500 (74.6%) Schizoaffective disorder, n = 110 (16.4%) Other, n = 60 (9.0%) |
Involuntary admission (p < 0.005), history of aggressive behaviour (p < 0.005), no school graduation (p < 0.005), substance disorder comorbidity (p < 0.005), not having competitive work (p < 0.005) | Switching to atypical antipsychotics (p < 0.001) |
| Linden et al. [2001] | Prospective | Schizophrenia, N = 122 | Physician’s judgment on lack of willingness of the patient to cooperate (p < 0.001), idiosyncratic assumptions (p < 0.05) | Older age (p < 0.05), longer duration of illness (p < 0.01), trust in the effectiveness of medication (significance NR), less tendency to feel responsible for their illness (significance NR) |
| Loffler et al. [2003] | Prospective | Schizophrenia, N = 307 | Subjective reasons for noncompliance include: side effects (50%), lack of acceptance of the necessity of pharmacological treatment (40%), lack of insight (27%) | Subjective reasons for compliance include: relapse prevention (88%), perceived benefit from medication (79%), positive relationship with a therapist (41%) |
| Novick et al. [2010] | Prospective | Schizophrenia, N = 6,731 | Alcohol dependence (p = 0.013) or substance abuse (p = 0.043) in a previous month, hospitalization in the last 6 months (p < 0.001) | Good prior adherence (p < 0.001), greater social activities (p < 0.001) |
| Aldebot and de Mamani [2009] | Cross-sectional (interview) | Schizophrenia/schizoaffective, N = 40 | Denial coping (p = 0.008) | NR |
| Borras et al. [2007] | Cross-sectional (interview) | Schizophrenia/other nonaffective disorders, N = 103 | Negatively influenced by spiritual belief (26%) | Positively influenced by spiritual belief (31%) |
| McCann et al. [2009] | Cross-sectional (interview) | Schizophrenia, N = 81 | Adverse events not associated with medication omission | |
| Olfson et al. [2006] | Cross-sectional (Postal survey) | 534 psychiatrists responded to the survey | Lack of awareness of mental illness (p = 0.021) | NR |
| Rettenbacher et al. [2004] | Cross-sectional (interview) | Schizophrenia, N = 61 | NR | Subjectively experienced positive effect on illness (p = 0.093) and everyday life (p = 0.072), psychiatrist inquiring medication intake (p = 0.074), more negative symptoms (p = 0.044), psychological side effects (p = 0.004) |
| Weiden et al. [2004] | Cross-sectional (postal survey) | Schizophrenia, N = 304 | Obesity (OR = 2.5; 95% CI 1.1–5.5) and subjective distress from weight gain (significance level NR) | NR |
| Valenstein et al. [2004] | Retrospective database analysis | Schizophrenia or schizoaffective disorder, N = 63,214 | Ethnicity (African-American) (OR 2.38; 95% CI 2.28–2.49), younger age < 45 (OR 1.31; 95% CI 1.25–1.37) | Atypical agent (clozapine) (p < 0.0001), switching from conventional to atypical therapy (p < 0.001) |
| Velligan et al. [2009] | Qualitative review and survey of experts | The survey involved 48 leading experts on adherence problems | Rating by experts on scale from 1 to 10: poor insight (7.2), distress associated with side effects (7.2), lack of/partial efficacy with continued symptoms (6.9), belief that the medications are no longer needed (6.7), ongoing substance use problems (6.6) | Results from literature review on positive factors include: positive therapeutic relationship, family and social support |
95% CI, 95% confidence interval; NR, not reported; OR, odds ratio; PANSS, Positive and Negative Syndrome Scale.
Table 2.
Summary of findings on consequence of non-adherence.
| Author [year] | Study design | Patient population | Key findings |
|---|---|---|---|
| Morken et al. [2008] | RCT | Schizophrenia/schizoaffective schizophreniform disorder, N = 50 | Nonadherence was associated with relapse (p = 0.000), hospital admission (p = 0.204), and having persistent psychotic symptoms (p = 0.040) Among 22 nonadherent patients on oral treatment, 11 (50%) were admitted to hospital during the 2 years |
| Ascher-Svanum et al. [2006] | Prospective | Schizophrenia/schizoaffective schizophreniform/disorder, N = 1,906 | Nonadherence associated with significantly greater risks of psychiatric hospitalization and use of emergency psychiatric services, arrests, violence, victimizations, poorer mental functioning, poorer life satisfaction, greater substance abuse and more alcohol-related problems (all p < 0.001) Nonadherence associated with greater risk of violence (nonadherent patients more than twice as likely to be more violent and more than two times more often arrested than adherent patients) |
| Rzewuska [2002] | Prospective | Schizophrenia, N = 185 | No difference in total time spent in hospital in 7 years of illness between compliant and noncompliant groups Refusal to comply correlated with frequent lack of criticism, and the presence of average to intense signs of defect and maladjustment (all p < 0.01). |
| Chen et al. [2005] | Prospective | Schizophrenia/schizoaffective schizophreniform/disorder, N = 93 | Medication nonadherence was the strongest predictor of relapse with an OR of 7.6 (p = 0.002) |
| Knapp et al. [2004] | Cross-sectional (national survey) | Resident in hospital, N = 304: schizophrenia (72%) Resident in other institutions, N = 354: schizophrenia (63.3%) |
Nonadherent patients were over 1.5 times more likely to report use of in-patient services compared with adherent patients (p = 0.054) Nonadherence was associated with almost three times increase in external service costs (p < 0.001) Patients reporting nonadherence were predicted to have excess in-patient costs of approximately £2,500 a year Predicted excess total service costs for patients reporting nonadherence is over £5,000 a year compared with total costs for adherent patients |
| Rittmannsberger et al. [2004] | Cross-sectional (interview) | Schizophrenia/schizoaffective disorder, N = 95 | Nonadherent patients were hospitalized for significantly longer periods during the year after the index episode 44.8 days (95% CI ± 58.5) versus 20.6 days (95% CI ± 27.4) (p < 0.05) |
| Eaddy et al. [2005] | Retrospective database analysis | Schizophrenia/bipolar disorder, N = 7,864 | Partially compliant patients were 49% (95% CI 29.2–71.7) more likely than compliant patients to have an inpatient hospitalisation and incurred 54.5% (p < 0.001) higher inpatient charges |
| Marcus and Olfson [2008] | Retrospective database analysis | Schizophrenia, N = 35,815 | The fraction of acute care inpatient admissions attributable to not having medication was 12.3% (95% CI 11.7–12.6) and the inpatient days attributable to not receiving medication was 13.1% (95% CI 11.7–12.6) when a 15-day gap in the prescription record was used. When a 30-day gap was used, the attributable rates changed modestly to 9.5% (95% CI 9.0–10) of hospital admissions and 10.2% (95% CI 6.8–13.7) of inpatient days. Improving the adherence to eliminate gaps in antipsychotic medication could lower the number of acute care admissions by 12.3% (95% CI 11.7–12.6) and reduce the number of treatment days by 13.1% (95% CI 9.8–16.5) resulting in a savings of $106 million (95% CI 79.0–133.0) |
| Valenstein et al. [2002] | Retrospective database analysis | Schizophrenia/schizoaffective disorder, N = 67,079 | Patients with poor adherence were 2.4 times as likely to be admitted during the study years than patients with good adherence (p < 0.001) Once admitted, patients with poor adherence had more total psychiatric inpatient days (mean of 33 days) than patients with good adherence (mean of 24 days) (p < 0.0001) |
| Byerly et al. [2007] | Qualitative review | Schizophrenia | Nonadherence was associated with exacerbation of psychotic symptoms, increased aggression, worse prognosis, increased hospital and emergency room use, and high healthcare costs |
| Leucht and Heres [2006] | Qualitative review | Schizophrenia | Nonadherent patients were at four times greater risk of suicide than those who were adherent |
| Llorca et al. [2008] | Qualitative review | Schizophrenia | Nonadherent patients were at seven times greater risk of suicide than those who were adherent |
| Svestka and Bitter [2007] | Qualitative review | Schizophrenia disorders | Out of a total of 41,754 patients, 1,020 attempted suicide and 154 were successful in their attempt The relapse after premature withdrawal from antipsychotic treatment is associated with suicidal behaviour or violence |
| Velligan et al. [2009] | Qualitative review and survey of experts | Schizophrenia | Nonadherence was associated with increased risk of relapse and suicide |
95% CI, 95% confidence interval; RCT, randomized controlled trial.
Table 3.
Results on a link between non-adherence and hospitalisation.
| Author [year] | Study design | Patient population | Definition of adherence | Key findings |
|---|---|---|---|---|
| Morken et al. [2008] | RCT | Schizophrenia/schizoaffective schizophreniform disorder, N = 50 | Good adherence was defined as less than one month without medication | Good adherence with oral antipsychotics admitted to hospital (32%) versus poor adherence (50%, p = 0.201) |
| Knapp et al. [2004] | Cross-sectional (national survey) | Resident in hospital, N = 304: schizophrenia (72%) Resident in other institutions, N = 354: schizophrenia (63.3%) |
Survey responses to two questions: ‘Do you sometimes not take your medications even though you should?’ ‘Do you sometimes take more medication/pills than the stated dose?’ | Nonadherent patients were over 1.5 times more likely to report use of inpatient services compared with adherent patients (p = 0.054) |
| Ahn et al. [2008] | Retrospective database analysis | Schizophrenia, N = 36,195 | Fully or partially adherent if MPR ≥80% Nonadherent if MPR < 80% |
Nonadherent patients were more likely to use acute hospitalization (p < 0.001), psychiatric hospitalization (p < 0.001) and ambulatory outpatient care (p = 0.025) than adherent patients |
| Eaddy et al. [2005] | Retrospective database analysis | Schizophrenia/bipolar disorder, N = 7,864 | Partly compliant if <80% Compliant if 80–125% Overly compliant if >125% |
Partially compliant patients were 49% (95% CI 29.2–71.7) more likely than compliant patients to have an inpatient hospitalization |
| Gilmer et al. [2004] | Retrospective database analysis | Schizophrenia, N = 1,619 | Nonadherent patients if CPR = 0–49% Partly adherent if CPR = 50–79% Adherent if CPR = 80–110% Excess medication fillers if CPR > 110% |
Nonadherent patients had the highest risk for psychiatric (34.9% versus 13.5%) and medical hospitalization (13.3% versus 7.0%) (p < 0.001 for both) |
| Karve et al. [2009] | Retrospective database analysis | Schizophrenia, N = 3,395 patients | PDC: same formula as MPR except values greater than 1.0 were capped or truncated at 1 | Any cause hospitalizations: cutoff value 80%, OR 0.417 (p < 0.001). Empirical evidence showed 80% as a reasonable cutoff point that stratifies adherent and nonadherent patients based on subsequent risk of hospitalization |
| Kozma et al. [2009] | Retrospective database analysis | Schizophrenia/schizoaffective disorder, N = 1,499 | % of MPR | OR of hospitalizations (<70% versus ≥70%): 0.83 (p < 0.001) |
| Laan et al. [2010] | Retrospective database analysis | Psychotic disorder, N = 477 Schizophrenia (79%) |
% of MPR | The average MPR for patients readmitted and not readmitted was 50% and 59% respectively. HR of 0.60 (95% CI 0.42–0.88) for the MPR on relapse risk |
| Law et al. [2008] | Retrospective database analysis | Schizophrenia, N = 1,191 | Medication gap days | HR of all-cause hospitalizations 1.4 (95% CI 0.99–1.98) for ≤10 days, 1.3 (0.87–1.93) for 11–30 days, 1.57 (1.23–2.01) for >30 days compared with individuals not in a gap HR of schizophrenia-related hospitalizations 1.77 (95% CI 1.16–2.71) for ≤10 days, 1.23 (0.74–2.06) for 11–30 days, 1.49 (1.09–2.02) for >30 days compared with individuals not in a gap |
| Svarstad et al. [2001] | Retrospective database analysis | Schizophrenia/schizoaffective/bipolar disorder, N = 619 | Irregular users if they had one quarter or more without a claim | Rehospitalizations (irregular users versus regular users): OR 1.99 (95% CI 1.12–3.54) (p < 0.05) |
| Valensteinet al. [2002] | Retrospective database analysis | Schizophrenia/schizoaffective disorder, N = 67,079 | Poorly adherent if MPR < 80% Good adherence if MPR from 80% to 110% Excess medication fills if MPR > 110% |
Hospitalization rate by MPR: 37.1% for MPR between 0 and 10%, 8.3% for MPR between 90% and 100%, 28.4% for MPR between 120% and >130% OR for MPR < 80%: 2.4 (p < 0.0001); OR for MPR > 110%: 3.0 (p < 0.0001) |
| Weiden et al. [2004] | Retrospective database analysis | Schizophrenia, N = 4,325 | % of MPR | OR of hospitalizations (<70% versus ≥70%): 0.87 (p < 0.001) for 10% improved compliance |
95% CI, 95% confidence interval; CPR, cumulative possession ratio; HR, hazard ratio; MPR, medication possession ratio; OR, odds ratio; PDC, proportion of days covered; RCT, randomized controlled trial.
Factors influencing adherence rates
Fifteen papers [Acosta et al. 2009; Aldebot and de Mamani 2009; Ascher-Svanum, 2006; Borras et al. 2007; Hudson et al. 2004; Janssen et al. 2006; Linden et al. 2001; Loffler et al. 2003; McCann et al. 2009; Novick et al. 2010; Olfson et al. 2006; Rettenbacher et al. 2004; Valenstein et al. 2004; Velligan et al. 2009; Weiden et al. 2004b] assessed drivers of nonadherence in schizophrenia; seven were prospective longitudinal studies [Acosta et al. 2009; Ascher-Svanum, 2006; Ascher-Svanum et al. 2006; Hudson et al. 2004; Janssen et al. 2006; Linden et al. 2001; Loffler et al. 2003; Novick et al. 2010] and six were cross-sectional studies such as interviews and surveys [Aldebot and de Mamani 2009; Borras et al. 2007; McCann et al. 2009; Olfson et al. 2006; Rettenbacher et al. 2004; Weiden et al. 2004b]. In addition, there was one retrospective database study [Valenstein et al. 2004] and one review/survey of experts [Velligan et al. 2009]. Ten of these studies [Ascher-Svanum 2006; Borras et al. 2007; Hudson et al. 2004; Janssen et al. 2006; Linden et al. 2001; Loffler et al. 2003; Novick et al. 2010; Olfson et al. 2006; Valenstein et al. 2004; Weiden et al. 2004b] included more than 100 subjects (i.e. patients or psychiatrists), and five of these studies [Ascher-Svanum 2006; Janssen et al. 2006; Novick et al. 2010; Olfson et al. 2006; Valenstein et al. 2004] included more than 500 subjects. Countries where studies were conducted included Spain [Acosta et al. 2009; Novick et al. 2010], the USA [Aldebot and de Mamani 2009; Ascher-Svanum, 2006; Hudson et al. 2004; Olfson et al. 2006; Valenstein et al. 2004; Weiden et al. 2004b], Switzerland [Borras et al. 2007], Germany [Janssen et al. 2006; Linden et al. 2001; Loffler et al. 2003], Australia [McCann et al. 2009], Denmark [Novick et al. 2010], Italy [Novick et al. 2010], Portugal [Novick et al. 2010], Ireland [Novick et al. 2010], the UK [Novick et al. 2010] and Austria [Rettenbacher et al. 2004]. Eleven studies [Aldebot and de Mamani 2009; Borras et al. 2007; Hudson et al. 2004; Janssen et al. 2006; Loffler et al. 2003; McCann et al. 2009; Novick et al. 2010; Olfson et al. 2006; Rettenbacher et al. 2004; Velligan et al. 2009; Weiden et al. 2004b] used subjective measures of adherence such as interviews and questionnaires completed by clinicians or patients, and four studies [Acosta et al. 2006; Ascher-Svanum, 2006; Linden et al. 2001; Valenstein et al. 2004] used objective measures of adherence such as the Medication Event Monitoring System (MEMS, AARDEX Group Ltd., Switzerland) and medication possession ratio (MPR), which was calculated based on the medical prescription information in the medical records or pharmacy data.
Table 1 presents factors that were found to either positively or negatively influence adherence rates in these studies.
Disease-related factors
Some symptoms of schizophrenia may inhibit the patient’s ability to cooperate during the treatment process. These disease-related factors, such as symptom severity and lack of illness insight, may influence adherence.
Symptom severity and adherence
Two prospective studies [Acosta et al. 2009; Hudson et al. 2004] supported a directional relation, in which symptom severity was associated with worse adherence. One cross-sectional study [Rettenbacher et al. 2004] reported that adherent patients showed significantly more negative symptoms than nonadherent patients (mean Positive and Negative Syndrome Scale negative score = 15.1 versus 9.8; p = 0.044) but found no statistical association between adherence and positive symptoms. A prospective study [Loffler et al. 2003] which studied subjective reasons for noncompliance among patients with schizophrenia reported that patients with more severe symptoms were less likely to consider relapse prevention as an important factor for their compliance [odds ratio (OR) 0.34; p = 0.009]. In contrast, another prospective study [Linden et al. 2001] reported no prognostic relation between symptom severity and adherence. The author states that this contrary finding may be due to the inclusion of more adherent patients in the latter study which may, in turn, influence the overall findings concerning patient adherence.
Lack of illness insight
Many individuals with schizophrenia have poor or no insight into their illness, meaning that they are not aware of the symptoms and consequences of their illness. Four studies (two prospective studies [Acosta et al. 2009; Loffler et al. 2003], one cross-sectional study [Olfson et al. 2006] and the survey of experts [Velligan et al. 2009]) found a directional relation in which lack of illness insight was associated with worse adherence. In fact, the survey involving clinical experts [Velligan et al. 2009] rated poor illness insight as the most important factor contributing to nonadherence. Another cross-sectional study [Aldebot and de Mamani, 2009] reported that individuals who dealt with the stress of their illness by ignoring their illness or the magnitude of their symptoms were less adherent to their medication. The author hypothesized that patients who refused to accept being ill may not believe that their symptoms are something that can be managed, and thus, may be less motivated to take steps to resolve their symptoms, such as taking medication. Only one prospective study [Linden et al. 2001] reported no relation between adherence and lack of insight. The author states that this contrary finding may be due to the inclusion of more adherent patients which may, in turn, influence the overall findings concerning patient adherence.
Patient-related factors
Six types of patient-related factors were reviewed: sociodemographic factors, substance abuse, beliefs about medication, prior adherence, obesity and religious factors.
Sociodemographic factors
Four studies (three prospective studies [Acosta et al. 2009; Linden et al. 2001; Loffler et al. 2003] and one cross-sectional study [Aldebot and de Mamani, 2009]) did not show a relation between adherence and sociodemographic variables such as gender [Acosta et al. 2009; Aldebot and de Mamani, 2009; Linden et al. 2001], age [Acosta et al. 2009], family/marital status [Acosta et al. 2009; Linden et al. 2001], ethnicity [Aldebot and de Mamani, 2009], occupational status/qualification [Linden et al. 2001] and level of education [Acosta et al. 2009; Aldebot and de Mamani, 2009; Linden et al. 2001; Loffler et al. 2003]. However, three prospective studies [Hudson et al. 2004; Janssen et al. 2006; Linden et al. 2001] and one retrospective database study [Valenstein et al. 2004] did report a positive relationship between sociodemographic factors and adherence. For example, a positive relationship with older age [Linden et al. 2001; Valenstein et al. 2004], and a negative relationship with low education level [Hudson et al. 2004; Janssen et al. 2006] were identified. In addition, one study found that African Americans were more likely to have poor adherence compared with white people [Valenstein et al. 2004].
Substance use
Five studies (four prospective studies [Ascher-Svanum, 2006; Hudson et al. 2004; Janssen et al. 2006; Novick et al. 2010] and the survey of experts [Velligan et al. 2009]) consistently found a significant negative relation between substance abuse and nonadherence. One of these studies [Ascher-Svanum, 2006] found that almost a third of nonadherent patients with schizophrenia were substance users compared with a fifth of adherent patients and that patients with prior or current abuse of alcohol or drugs were more likely to be nonadherent. Another prospective study [Acosta et al. 2009] found that patients in the nonadherent group had a higher percentage of present or past substance abuse compared with the adherent group, although the association was not significant.
Beliefs about medication
Patient perception of whether medication works appeared to contribute to adherence rates. A cross-sectional study [Rettenbacher et al. 2004] found that the variable which best predicted compliance was ‘positive effect on everyday life’ as a reason for taking the drug (p = 0.01). The survey of experts [Velligan et al. 2009] reported that one of the important predictors of adherence problems was “patient’s belief that medication does not work”. Another prospective study [Linden et al. 2001] found that adherent patients showed a tendency to feel less responsible for their illness and have more trust in the effectiveness of the medication. The evidence suggests that the patient’s belief and trust in the effectiveness of medication may positively influence adherence.
Prior adherence practice
Two prospective studies [Ascher-Svanum, 2006; Novick et al. 2010] found a relation between current adherence rates and the patient’s past adherence practice. In one of these studies, patients who reported being nonadherent in the 4 weeks prior to enrolment were 3.1 times more likely to be nonadherent in the first year following enrolment (p < 0.001) [Ascher-Svanum, 2006]. The second study [Novick et al. 2010] found that the significant predictor of future adherence was a good adherence in the month before baseline assessment (p < 0.001).
Obesity
One study was conducted in order to analyse the relation between the objective weight status, subjective distress from weight and recent compliance with antipsychotic medication. In this cross-sectional study which included 304 patients with schizophrenia, obese respondents were more than twice as likely as those with normal body mass index to be nonadherent [OR 2.5; 95% confidence interval (CI) 1.1–5.5]. The author states that this association between obesity and noncompliance was observed for both men and women and that it is likely to be caused by the distress over weight gain [Weiden et al. 2004b].
Religious/spiritual factors
A cross-sectional study [Borras et al. 2007] explored the effect of religious or spiritual practice on adherence in 103 stabilized patients with schizophrenia or other nonaffective disorders and found that 57% of patients had a representation of their illness directly influenced by their spiritual beliefs: positively in 31% (e.g. belief that illness is a test sent by God to put them on the right path), and negatively in 26% (e.g. belief that illness is a punishment from God or a demon). Adherent patients had higher levels of group religious practice (at least once a month) than nonadherent patients.
Treatment-related factors
Treatment-related factors such as adverse events and type of antipsychotic regimen were reviewed. Dosing regimen is another potentially important factor that may influence adherence; therefore, this topic was addressed in a separate publication focusing only on this link [Medic et al. 2013].
Adverse events
A prospective study [Hudson et al. 2004] found that approximately 35% of patients reported adverse drug reactions to be a barrier to medication adherence. Another prospective study [Loffler et al. 2003] assessed subjective reasons for noncompliance and found that 50% of patients reported distressed by side effects as a reason for noncompliance. The expert survey [Velligan et al. 2009] rated distress associated with persistent side effects (especially weight gain in women and excessive sedation) to be important contributors to adherence problems.
Two studies (one prospective study and one cross-sectional study) [Linden et al. 2001; Rettenbacher et al. 2004] found that adherent patients experienced more adverse events than nonadherent patients. These results could be explained by the higher risk of developing side effects in patients who take medications. These studies suggest that other factors made patients adherent despite experiencing the side effects of medication. However, a survey of patients did not find a correlation between experiencing side effects and omitting a dose [McCann et al. 2009]. The author mentions that this contrary finding may be explained by patients’ perceptions of the effectiveness of medications being more central than the deterrent influence of side effects.
Antipsychotic regimen
The effect of the antipsychotic regimen was assessed in some studies. A prospective study [Janssen et al. 2006] which included 500 patients with schizophrenia in Germany found that patients who switched from a typical to an atypical antipsychotic had a significantly higher rate of medication adherence at discharge than those who did not switch (p < 0.001). Other factors that may have influenced adherence in this group may be the fact that patients who switched had fewer previous psychiatric admissions, shorter illness duration, a higher probability of being admitted voluntarily, and fewer substance disorders than those maintained on typical drugs [Weinmann, 2004]. A retrospective database study which analysed data from 63,214 patients [Valenstein et al. 2004] did not find a significant improvement in adherence as a result of using atypical agents; except with clozapine, when patients were unlikely to have poor adherence (OR 0.08; 95% CI 0.06–0.11). The higher rates of adherence observed with clozapine could be explained by superior efficacy or the requirements for close monitoring when using clozapine.
Environment-related factors
External or environment-related factors included relationship with physician, stigma of disease, living situation and family support.
Relationship with physician
A prospective study [Linden et al. 2001] found that both nonadherent and adherent patients had a good relationship with their physicians. However, adherent patients trusted their physicians significantly more, and they expected that physicians would be helpful in treatment (p < 0.05). Another prospective study [Loffler et al. 2003] found that 41% of patients considered a positive relationship with physicians and therapists to be important for medication adherence. Furthermore, a review [Velligan et al. 2009] reported that the ‘positive relationship with clinical staff’ was a significant predictor of good adherence. However, ‘difficulties in building a therapeutic alliance’ and ‘poor clinician–patient relationship’ were among significant predictors of nonadherence. A cross-sectional study [Rettenbacher et al. 2004] assessed a link between the person who inquires (i.e. psychiatrist, relatives or others) about drug intake and adherence. Forty-one percent of adherent patients were asked about drug intake most frequently by their psychiatrist while none of the nonadherent patients reported this (p = 0.074). Among nonadherent patients, a higher proportion (60% versus 9% of adherent patients) stated that their relatives inquired most often about their drug intake.
Other environmental factors
A prospective study [Hudson et al. 2004] found that the most common barriers to patient adherence to medication were related to the stigma of taking medication and lack of support. Furthermore, a review [Velligan et al. 2009] reported that predictors of nonadherence included a disorganized or chaotic living situation, financial problems, housing problems and logistic problems, while predictors of good adherence included family and social support. Greater social activity was also found to be a predictor of good adherence (OR 1.26; p < 0.001) [Novick et al. 2010].
Physician perception on important factors of nonadherence
In the expert survey [Velligan et al. 2009] on potential contributors to adherence problems in schizophrenia, experts were asked to rate factors as very important, somewhat important and not important for medication adherence. The factors rated as very important included ‘poor insight into having an illness’ and ‘distress associated with persistent side effects or fear of potential side effects’. The key factors out of 12 factors rated as somewhat important related to efficacy, beliefs about medication, substance abuse and social support. The survey revealed a wide range of factors that clinicians found to be the potential factors of nonadherence.
Consequences of nonadherence
Three main types of consequences of nonadherence included consequences to patients, society and healthcare systems. Twenty-two papers were included on the consequences of nonadherence [Ahn et al. 2008; Ascher-Svanum et al. 2006; Byerly et al. 2007; Chen et al. 2005; Eaddy et al. 2005; Gilmer et al. 2004; Karve et al. 2009; Knapp et al. 2004; Kozma and Weiden, 2009; Laan et al. 2010; Law et al. 2008; Leucht and Heres, 2006; Llorca, 2008; Marcus and Olfson, 2008; Morken et al. 2008; Rittmannsberger et al. 2004; Rzewuska, 2002; Svarstad et al. 2001; Svestka and Bitter, 2007; Valenstein et al. 2002; Velligan et al. 2009; Weiden et al. 2004a]. Four of these were prospective longitudinal studies [Ascher-Svanum et al. 2006; Chen et al. 2005; Morken et al. 2008; Rzewuska, 2002], two were cross-sectional studies [Knapp et al. 2004; Rittmannsberger et al. 2004]. In addition, there were 11 retrospective database studies [Ahn et al. 2008; Eaddy et al. 2005; Gilmer et al. 2004; Karve et al. 2009; Kozma and Weiden, 2009; Laan et al. 2010; Law et al. 2008; Marcus and Olfson, 2008; Svarstad et al. 2001; Valenstein et al. 2002; Weiden et al. 2004a] and five reviews [Byerly et al. 2007; Leucht and Heres, 2006; Llorca, 2008; Svestka and Bitter, 2007; Velligan et al. 2009]. Fourteen studies [Ahn et al. 2008; Ascher-Svanum et al. 2006; Eaddy et al. 2005; Gilmer et al. 2004; Karve et al. 2009; Knapp et al. 2004; Kozma and Weiden, 2009; Laan et al. 2010; Law et al. 2008; Marcus and Olfson, 2008; Rzewuska, 2002; Svarstad et al. 2001; Valenstein et al. 2002; Weiden et al. 2004a] included more than 100 subjects, and 12 of these studies [Ahn et al. 2008; Ascher-Svanum et al. 2006; Eaddy et al. 2005; Gilmer et al. 2004; Karve et al. 2009; Knapp et al. 2004; Kozma and Weiden, 2009; Law et al. 2008; Marcus and Olfson, 2008; Svarstad et al. 2001; Valenstein et al. 2002; Weiden et al. 2004a] included more than 500 subjects. These studies were conducted in the USA [Ascher-Svanum et al. 2006; Eaddy et al. 2005; Marcus and Olfson, 2008; Valenstein et al. 2002], the Netherlands [Laan et al. 2010], Norway [Morken et al. 2008], Austria [Rittmannsberger et al. 2004], the UK [Knapp et al. 2004], Hong Kong [Chen et al. 2005] and Poland [Rzewuska, 2002]. Four studies [Ascher-Svanum et al. 2006; Chen et al. 2005; Knapp et al. 2004; Rittmannsberger et al. 2004] used subjective measures of adherence such as interview and questionnaires completed by clinician or patients, and 13 studies [Ahn et al. 2008; Eaddy et al. 2005; Gilmer et al. 2004; Karve et al. 2009; Kozma and Weiden, 2009; Laan et al. 2010; Law et al. 2008; Marcus and Olfson, 2008; Morken et al. 2008; Rzewuska, 2002; Svarstad et al. 2001; Valenstein et al. 2002; Weiden et al. 2004a] used objective measures of adherence such as MPR and medication gap which were calculated based on the claims data, prescription data or observational data. Table 2 presents the consequences of nonadherence and Table 3 presents the results of the 12 studies identified showing a link between nonadherence and hospitalization rates.
Consequences to patients
Many patients may initially feel well following their withdrawal from antipsychotics, potentially because undesirable side effects disappear. However, relapse is a risk for these patients. Three types of consequences to patients were reported: rehospitalization rates, suicide rates and impact on prognosis.
Hospitalization rates
Two retrospective database studies [Kozma and Weiden, 2009; Weiden et al. 2004a] which analysed data from 1499 and 4325 patients respectively, assessed adherence as measured by MPR. In both of these studies, patients who reported adherence of MPR greater than 70% were observed to have lower hospitalization rates compared with nonadherent patients (OR 0.831 and 0.87 respectively; p < 0.001 in both cases). Another retrospective database study [Valenstein et al. 2002] which analysed data from 67,079 patients and measured adherence by MPR found that patients with MPR less than 80% had a significantly higher hospitalization rate compared with adherent patients (OR 2.4; p < 0.0001). For patients with a MPR over 120%, hospitalization rates were significantly higher compared with adherent patients (i.e. MPR close to 100%; OR 3.0; p < 0.0001). In other words, patients who secured more medication than necessary to take their prescribed antipsychotic doses were also at increased risk for hospitalization. One prospective study [Morken et al. 2008] which included 50 patients and used patient interviews to assess adherence found that patients with good adherence had a lower hospitalization rate compared with nonadherent patients (32% versus 50%), although this finding was not significant (p = 0.201).
In all other studies, there was heterogeneity in definition of adherence and measures of adherence used, such as medication gap, consistency, persistency and other subjective measures such as surveys. Therefore, it was difficult to make comparisons, and it was not feasible to pool the quantitative results on the relationship between nonadherence and increased risk of hospitalization. However, regardless of the heterogeneity in adherence measures used, all studies consistently showed a link between lower adherence rates and higher hospitalization risk [Ahn et al. 2008; Eaddy et al. 2005; Gilmer et al. 2004; Karve et al. 2009; Knapp et al. 2004; Laan et al. 2010; Law et al. 2008; Morken et al. 2008; Svarstad et al. 2001].
Suicide rates
Suicide is one of the leading causes of premature death in patients with schizophrenia, but it is highly preventable. Nonadherence to antipsychotic medication is one of the risk factors for the development of suicidal behaviour in patients with schizophrenia. Four reviews [Leucht and Heres, 2006; Llorca, 2008; Svestka and Bitter, 2007; Velligan et al. 2009] looked into suicide rates as a result of nonadherence and reported a trend where nonadherence was related to a significant increase in the risk of suicide. A review [Leucht and Heres, 2006] reported that nonadherence to schizophrenia medication increases the risk of suicide fourfold (relative risk adjusted for age and gender 4.2, 95% CI 1.7–10.1) while another review [Llorca, 2008] reported that nonadherent patients (documented refusal of oral or depot injection) were at seven times greater risk of suicide.
Prognosis
Nonadherence may cause psychotic symptoms in patients, thus leading to serious consequences. One review [Byerly et al. 2007] reported that repeated psychotic relapses, particularly in the early stages of the illness, may worsen the course and prognosis of the patient, as it may result in resistance to antipsychotic medications and to the development of chronic psychotic symptoms.
Consequences to society
Two studies (one prospective study and one review) [Ascher-Svanum et al. 2006; Svestka and Bitter, 2007] investigated the impact of nonadherence on violence rates in patients with schizophrenia. Relapse after premature withdrawal from antipsychotic treatment was often associated with violence [Svestka and Bitter, 2007]. In a large prospective multisite study which included 1906 patients, nonadherent patients were more than twice as likely to be violent than adherent patients (10.8% versus 4.8%; p < 0.001). They were also more likely to be arrested than adherent patients (8.4% versus 3.5%; p < 0.001) [Ascher-Svanum et al. 2006].
Consequences to healthcare systems
Nonadherence to medication can lead to relapse, which can mean more visits to the emergency room, rehospitalizations and increased need for clinician intervention – all of which lead to increased costs to healthcare systems.
A large multisite prospective study [Ascher-Svanum et al. 2006] which included 1906 patients concluded that nonadherence was significantly associated with poorer outcomes, including a greater risk of psychiatric hospitalizations and use of emergency psychiatric services. Compared with adherent patients, those who were not adherent during the first year were more likely to be hospitalized in the following 2 years (OR 1.55; 95% CI 1.21–1.98) and more likely to use emergency psychiatric services in the following 2 years (OR 1.49; 95% CI 1.12–1.98). These were all drivers of direct medical cost. A survey study of 95 patients [Rittmannsberger et al. 2004] reported that nonadherent patients were hospitalized for significantly longer periods than adherent patients. In a large retrospective database study which analysed data from 67,709 patients [Valenstein et al. 2002], patients with poor adherence were 2.4 (95% CI 2.3–2.6) times more likely to be admitted to the hospital during the study year than patients with good adherence. Poor adherence during the outpatient periods in the study was also associated with psychiatric admissions in the following year. Patients reporting nonadherence were predicted to have excess inpatient costs of approximately £2500 (around €2000) per year in a survey study conducted in the UK [Knapp et al. 2004]. In this study, predicted excess total service costs for patients reporting nonadherence was over £5000 per year compared with total costs for adherent patients.
A retrospective database study which analysed data from 35,815 patients [Marcus and Olfson, 2008] reported that the fraction of acute care inpatient admissions attributable to not receiving antipsychotic medications was 12.3% (95% CI 11.7–12.6%) and the fraction of inpatient days attributable to not receiving antipsychotic medication was 13.1% (95% CI 9.8–16.5%) when a 15-day gap in the prescription record was used. Therefore, improving adherence by eliminating gaps in antipsychotic medication treatment could lower the number of acute care admissions and inpatient days.
Discussion
Antipsychotic medication is recognized as an essential component in the treatment of schizophrenia, and adherence to medication plays a critical role in preventing symptoms and costly relapses. This study therefore reviewed the main factors and consequences of nonadherence based on 37 full papers.
Several patient-related factors may contribute to increasing or decreasing medication adherence. The evidence suggests that sociodemographic factors such as gender [Acosta et al. 2009; Linden et al. 2001] and family/marital status [Acosta et al. 2009; Linden et al. 2001] do not influence adherence as the association between nonadherence and these variables were not significant in most studies. However, results were mixed concerning ethnicity [Aldebot and de Mamani, 2009; Valenstein et al. 2004], level of education [Acosta et al. 2009; Aldebot and de Mamani, 2009; Hudson et al. 2004; Janssen et al. 2006; Linden et al. 2001; Loffler et al. 2003] and age [Acosta et al. 2009; Linden et al. 2001; Valenstein et al. 2004]. Lack of insight was significantly associated with nonadherence in all studies [Acosta et al. 2009; Aldebot and de Mamani 2009; Loffler et al. 2003; Olfson et al. 2006] except one [Linden et al. 2001]. The author of this study mentions that the contrary finding may be due to the selection of patients with expected better adherence. Substance abuse [Ascher-Svanum, 2006; Hudson et al. 2004; Janssen et al. 2006; Novick et al. 2010], negative medication beliefs [Linden et al. 2001; Loffler et al. 2003], and a prior poor adherence practice [Ascher-Svanum, 2006; Novick et al. 2010] were found to be significantly associated with nonadherence.
Treatment-related factors were also reviewed. Patients and experts reported adverse events to be a barrier to adherence [Hudson et al. 2004; Loffler et al. 2003; Velligan et al. 2009]. However, in two studies [Linden et al. 2001; Rettenbacher et al. 2004] adherence was good despite the presence of adverse events. Due to the mixed results, it is difficult to make a conclusion on the causal relation between adverse events and nonadherence. Patients who were on atypical agents tended to have better adherence [Valenstein et al. 2004]. However, this may be related to other factors; different patient characteristics using atypical agents as opposed to typical agents or treatment monitoring that is required for the use of a specific drug. Given these confounding factors, conclusions about adherence and type of antipsychotic remain challenging.
External or environment-related factors included relationship with physician, stigma of disease, living situation and family support. The evidence suggests that a therapeutic relationship with monitoring and guidance in drug intake are important contributors to good adherence [Loffler et al. 2003; Rettenbacher et al. 2004; Velligan et al. 2009]. Other environmental factors that influence adherence positively include family or social support [Velligan et al. 2009] and greater social activities [Novick et al. 2010]. Stigma of taking medication [Hudson et al. 2004] and lack of social support [Hudson et al. 2004] were found to negatively influence adherence.
There are serious consequences, such as hospitalization and suicide, associated with nonadherence to treatment. Studies consistently showed that nonadherence was significantly associated with poorer outcomes, including greater risk of hospitalization [Ahn et al. 2008; Ascher-Svanum et al. 2006; Eaddy et al. 2005; Gilmer et al. 2004; Kozma and Weiden, 2009; Law et al. 2008; Morken et al. 2008; Svarstad et al. 2001; Valenstein et al. 2002; Weiden et al. 2004a], greater use of emergency services [Ascher-Svanum et al. 2006], longer length of hospital stay [Rittmannsberger et al. 2004; Valenstein et al. 2002] and greater risk of suicide [Leucht and Heres, 2006; Llorca, 2008]. The consequences to society included having to deal with the consequences of violence [Ascher-Svanum et al. 2006], substance abuse [Ascher-Svanum et al. 2006] and criminal behaviour [Ascher-Svanum et al. 2006]. Thus, improving adherence is likely to reduce medical costs as well as societal costs.
The most recent comprehensive review [Velligan et al. 2009] on nonadherence in schizophrenia, which involved both a literature review and experts’ ratings on the findings in the literature, found that poor insight and lack of illness awareness, a belief that medications are no longer needed, and lack of treatment efficacy were key factors that contributed to adherence problems. In that survey, experts gave more prominence to side effects as a contributor to adherence problems than has been reported in surveys of patients and other studies in the literature [Velligan et al. 2009]. Lack of disease insight is also found to be an important driver of poor adherence in our review. Yet for medication side effects, we found mixed results; in fact, two studies [Linden et al. 2001; Rettenbacher et al. 2004] found that adherent patients experienced more adverse events than nonadherent patients. Hence the literature does not seem to fully support the experts’ view that side effects are highly important for nonadherence.
For the consequences of nonadherence, another recent review [Llorca, 2008] reported that nonadherence and partial adherence can set in motion a ‘downward spiral’ of events resulting in inconsistent symptom control, relapse and rehospitalization, which in turn can lead to long-term functional disabilities, loss of autonomy, education or employment possibilities, homelessness, a likelihood of dropping out of care completely and even suicide. A clear link between nonadherence and an increased risk of hospitalization is found in our review; we also found support for the link between poor medication adherence and suicide risk.
This review is associated with at least three limitations. A first limitation of this review relates to the fact that there was heterogeneity in the definition of adherence and methods to measure medication adherence. Some studies used objective measures such as MEMS and medication gaps while others used subjective methods such as patient self-report questionnaires and patient interviews. Thus, it was difficult to compare results and make systematic conclusions. Second, study designs varied considerably, including prospective studies, retrospective data analyses and cross-sectional surveys. With different study designs, comparison of results becomes difficult. Third, due to the large amount of data identified, one criterion for inclusion in this review was study quality as measured by study size and design, which can be subjective, and recent publications were prioritized.
Despite these limitations, this is the first study, to our knowledge, to systematically and comprehensively explore both the factors and consequences of nonadherence in schizophrenia, with a particular focus on the link between nonadherence and hospitalization rates.
Our review found a large amount of heterogeneity in the definition and methods used to assess medication adherence. Thus, there is a great need for future research to use a consistent definition and measure of adherence in patients with schizophrenia in order to enable an unbiased and meaningful comparison of results. Moreover, additional large, prospective adherence studies would allow us to assess the causes of nonadherence with greater accuracy as the same patients are observed over time.
Our systematic review identified a wide range of factors and consequences of poor adherence in schizophrenia. Based on the evidence found, the most frequently reported driver and consequence of nonadherence appeared to be the lack of illness insight and greater risk of hospitalization, respectively. Factors positively related to adherence included a good therapeutic relationship with physician and perceiving the benefits of medication. Practicing physicians should be aware of the importance of building a therapeutic relationship with the patient based on trust as well as educating the patient on the medication’s impact on the symptoms and illness. Considering the substantial burden of nonadherence in schizophrenia on patients and society as a whole, improved adherence in schizophrenia is of great value to patients and society. As our review shows, nonadherence is a complex behavioural issue; therefore measures will need to address nonadherence from many angles and take a multifaceted approach with patients and healthcare providers.
Acknowledgments
We thank Kyoko Higashi of Mapi Consultancy, who provided medical writing support funded by AstraZeneca.
Footnotes
Funding: This systematic literature review was carried out by Mapi Consultancy, funded by AstraZeneca.
Conflict of interest statement: Dr De Hert has been a consultant for, received grant/research support and honoraria from, and been on the speakers/advisory boards of Astra Zeneca, Bristol-Myers Squibb, Eli Lilly, Janssen-Cilag, Lundbeck JA, Pfizer and Sanofi Aventis.
Contributor Information
Kyoko Higashi, Mapi Consultancy, De Molen 84, 3995 AX, Houten, The Netherlands.
Goran Medic, Mapi Consultancy, The Netherlands.
Kavi J. Littlewood, Mapi Consultancy, The Netherlands
Teresa Diez, AstraZeneca, Corporate Village, Belgium (former employee).
Ola Granström, AstraZeneca Nordic, Sweden (former employee).
Marc De Hert, Department of Neurosciences KU Leuven, University Psychiatric Centre Catholic University Leuven, Belgium.
References
- Acosta F., Bosch E., Sarmiento G., Juanes N., Caballero-Hidalgo A., Mayans T. (2009) Evaluation of noncompliance in schizophrenia patients using electronic monitoring (MEMS) and its relationship to sociodemographic, clinical and psychopathological variables. Schizophr Res 107: 213–217 [DOI] [PubMed] [Google Scholar]
- Ahn J., McCombs J., Jung C., Croudace T., McDonnell D., Ascher-Svanum H., et al. (2008) Classifying patients by antipsychotic adherence patterns using latent class analysis: characteristics of nonadherent groups in the California Medicaid (Medi-Cal) program. Value Health 11: 48–56 [DOI] [PubMed] [Google Scholar]
- Aldebot S., de Mamani A. (2009) Denial and acceptance coping styles and medication adherence in schizophrenia. J Nerv Men Dis 580–584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2006) Evidence-Based Treatments for Schizophrenia: Information for families and Other Supporters. Arlington, VA: American Psychiatric Association [Google Scholar]
- Ascher-Svanum H. (2006) A prospective study of risk factors for nonadherence with antipsychotic medication in the treatment of schizophrenia. J Clin Psychiatry 67: 1114–1123 [DOI] [PubMed] [Google Scholar]
- Ascher-Svanum H., Faries D., Zhu B., Ernst F., Swartz M., Swanson J. (2006) Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry 67: 453–460 [DOI] [PubMed] [Google Scholar]
- Boden R. (2011) Early non-adherence to medication and other risk factors for rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Res 133: 36–41 [DOI] [PubMed] [Google Scholar]
- Borras L., Mohr S., Brandt P., Gillieron C., Eytan A., Huguelet P. (2007) Religious beliefs in schizophrenia: their relevance for adherence to treatment. Schizophr Bull 33: 1238–1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byerly M., Nakonezny P., Lescouflair E. (2007) Antipsychotic medication adherence in schizophrenia. Psychiatr Clin North Am 30: 437–452 [DOI] [PubMed] [Google Scholar]
- Chen E., Hui C., Dunn E., Miao M., Yeung W., Wong C., et al. (2005) A prospective 3-year longitudinal study of cognitive predictors of relapse in first-episode schizophrenic patients. Schizophr Res 77: 99–104 [DOI] [PubMed] [Google Scholar]
- Eaddy M., Grogg A., Locklear J. (2005) Assessment of compliance with antipsychotic treatment and resource utilization in a Medicaid population. Clin Ther 27: 263–272 [DOI] [PubMed] [Google Scholar]
- Gilmer T., Dolder C., Lacro J., Folsom D., Lindamer L., Garcia P., et al. (2004) Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry 161: 692–699 [DOI] [PubMed] [Google Scholar]
- Hudson T., Owen R., Thrush C., Han X., Pyne J., Thapa P., Sullivan G. (2004) A pilot study of barriers to medication adherence in schizophrenia. J Clin Psychiatry 65: 211–216 [DOI] [PubMed] [Google Scholar]
- Janssen B., Gaebel W., Haerter M., Komaharadi F., Lindel B., Weinmann S. (2006) Evaluation of factors influencing medication compliance in inpatient treatment of psychotic disorders. Psychopharmacology 187: 229–236 [DOI] [PubMed] [Google Scholar]
- Karve S., Cleves M., Helm M., Hudson T., West D., Martin B. (2009) Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin 25: 2303–2310 [DOI] [PubMed] [Google Scholar]
- Knapp M., King D., Pugner K., Lapuerta P. (2004) Non-adherence to antipsychotic medication regimens: associations with resource use and costs. Br J Psychiatry 184: 509–516 [DOI] [PubMed] [Google Scholar]
- Kozma C., Weiden P. (2009) Partial compliance with antipsychotics increases mental health hospitalizations in schizophrenic patients: analysis of a national managed care database. Am Health Drug Benefits 2: 31–38 [PMC free article] [PubMed] [Google Scholar]
- Laan W., Does Y., Sezgi B., Smeets H., Stolker J., Wit N., et al. (2010) Low treatment adherence with antipsychotics is associated with relapse in psychotic disorders within six months after discharge. Pharmacopsychiatry 43: 221–224 [DOI] [PubMed] [Google Scholar]
- Law M., Soumerai S., Ross-Degnan D., Adams A. (2008) A longitudinal study of medication nonadherence and hospitalization risk in schizophrenia. J Clin Psychiatry 69: 47–53 [DOI] [PubMed] [Google Scholar]
- Leucht S., Heres S. (2006) Epidemiology, clinical consequences, and psychosocial treatment of nonadherence in schizophrenia. J Clin Psychiatry 67(Suppl. 5): 3–8 [PubMed] [Google Scholar]
- Liberati A., Altman D., Tetzlaff J., Mulrow C., Gøtzsche P., Ioannidis J., et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6: 1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman J. (2005) Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 353: 1209–1223 [DOI] [PubMed] [Google Scholar]
- Linden M., Godemann F., Gaebel W., Kopke W., Muller P., Muller-Spahn F., et al. (2001) A prospective study of factors influencing adherence to a continuous neuroleptic treatment program in schizophrenia patients during 2 years. Schizophr Bull 27: 585–596 [DOI] [PubMed] [Google Scholar]
- Liu-Seifert H. (2012) Factors associated with adherence to treatment with olanzapine and other atypical antipsychotic medications in patients with schizophrenia. Compr Psychiatry 53: 107–115 [DOI] [PubMed] [Google Scholar]
- Llorca P. (2008) Partial compliance in schizophrenia and the impact on patient outcomes. Psychiatry Res 161: 235–247 [DOI] [PubMed] [Google Scholar]
- Loffler W., Kilian R., Toumi M., Angermeyer M. (2003) Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry 36: 105–112 [DOI] [PubMed] [Google Scholar]
- Marcus S., Olfson M. (2008) Outpatient antipsychotic treatment and inpatient costs of schizophrenia. Schizophr Bull 34: 173–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCann T., Clark E., Lu S. (2009) Subjective side effects of antipsychotics and medication adherence in people with schizophrenia. J Adv Nurs 65: 534–543 [DOI] [PubMed] [Google Scholar]
- Medic G., Higashi K., Littlewood K., Diez T., Granström O., Kahn R. (2013) Dosing frequency and adherence in chronic psychiatric disease: systematic review and meta-analysis. Neuropsychiatric Disease and Treatment 9: 119–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morken G., Widen J., Grawe R. (2008) Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry 8: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novick D., Haro J., Suarez D., Perez V., Dittmann R., Haddad P. (2010) Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res 176: 109–113 [DOI] [PubMed] [Google Scholar]
- Olfson M., Marcus S., Wilk J., West J. (2006) Awareness of illness and nonadherence to antipsychotic medications among persons with schizophrenia. Psychiatr Serv 57: 205–211 [DOI] [PubMed] [Google Scholar]
- Rettenbacher M., Hofer A., Eder U., Hummer M., Kemmler G., Weiss E., et al. (2004) Compliance in schizophrenia: psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry 65: 1211–1218 [DOI] [PubMed] [Google Scholar]
- Rittmannsberger H., Pachinger T., Keppelmuller P., Wancata J. (2004) Medication adherence among psychotic patients before admission to inpatient treatment. Psychiatr Serv 55: 174–179 [DOI] [PubMed] [Google Scholar]
- Rzewuska M. (2002) Drug maintenance treatment compliance and its correlation with the clinical picture and course of schizophrenia. Progr Neuropsychopharmacol Biol Psychiatry 26: 811–814 [DOI] [PubMed] [Google Scholar]
- Svarstad B., Shireman T., Sweeney J. (2001) Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatr Serv 52: 805–811 [DOI] [PubMed] [Google Scholar]
- Svestka J., Bitter I. (2007) Nonadherence to antipsychotic treatment in patients with schizophrenic disorders. Neuroendocrinol Lett 28(Suppl. 1): 95–116 [PubMed] [Google Scholar]
- Valenstein M., Blow F., Copeland L., McCarthy J., Zeber J., Gillon L., et al. (2004) Poor antipsychotic adherence among patients with schizophrenia: medication and patient factors. Schizophr Bull 30: 255–264 [DOI] [PubMed] [Google Scholar]
- Valenstein M., Copeland L., Blow F., McCarthy J., Zeber J., Gillon L., et al. (2002) Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Med Care 40: 630–639 [DOI] [PubMed] [Google Scholar]
- Velligan D., Weiden P., Sajatovic M., Scott J., Carpenter D., Ross R., et al. ; Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness (2009) The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry 70(Suppl. 4): 1–46; quiz 47–48. [PubMed] [Google Scholar]
- Weiden P. (2007) Understanding and addressing adherence issues in schizophrenia: from theory to practice. J Clin Psychiatry 68(Suppl. 14): 14–19 [PubMed] [Google Scholar]
- Weiden P., Kozma C., Grogg A., Locklear J. (2004a) Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv 55: 886–891 [DOI] [PubMed] [Google Scholar]
- Weiden P., Mackell J., McDonnell D. (2004b) Obesity as a risk factor for antipsychotic noncompliance. Schizophr Res 66: 51–57 [DOI] [PubMed] [Google Scholar]
- Weinmann S. (2004) Switching antipsychotics in inpatient schizophrenia care – predictors and outcome. J Clin Psychiatry 65: 1099–1105 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2003) Adherence to Long-Term Therapies. Evidence for Action. Geneva: World Health Organization [Google Scholar]
- World Health Organization (2011) Schizophrenia. Geneva: World Health Organization [Google Scholar]