Abstract
In this 2 part series, analysis of the risk stratification tools that are available, definition for the scope of the problem, and potential solutions through a review of the literature are presented. A systematic review was used to identify articles for risk stratification and interventions. Three risk stratification systems are discussed, St Thomas’s Risk Assessment Tool in Falling Elderly Inpatients, Morse Fall Scale, and the Hendrich Fall Risk Model. Of these scoring systems, the Hendrich Fall Risk Model is the easiest to use and score. Predominantly, multifactorial interventions are used to prevent patient falls. Education and rehabilitation are common themes in studies with statistically significant results. The second article presents a guide to implementing a quality improvement project around hospital falls. A 10-step approach to Plan-Do-Study-Act (PDSA) cycles is described. Specific examples of problems and analysis are easily applicable to any institution. Furthermore, the sustainability of interventions and targeting new areas for improvement is discussed. Although specific to falls in the hospitalized patient, the goal is to present a stepwise approach which is broadly applicable to other areas requiring quality improvement.
Keywords: accidental falls, inpatients, review
Introduction
An increased focus is being placed on inpatient falls. The reasons for this are multiple including associated morbidity and mortality, increased cost of care, and lack of reimbursement from the payors. The World Health Organization defines a fall as “inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position.”1 Significantly, while having been reported in between 2% and 12% of admissions,2 these events are found to cause harm in up to 40% of the patients.3,4 In addition to the real personal cost, the financial impact associated with these falls are of consequence, associated with an increase in hospital charges and longer length of stay.5 Given the preventable nature of many of these events, scrutiny by payors has followed. The Centers for Medicare and Medicaid Services have listed falls as a “never” event and therefore do not reimburse hospitals for expenses associated with the care for an inpatient fall.6
The nature of falls and their prevalence in patients with neurologic admissions will inevitably affect the neurohospitalist, presenting an excellent opportunity for involvement in risk reduction. Patients with neurological weakness with or without a clouded sensorium are clearly at risk of falls. In addition, assessing patients with potentially significant head injuries after a fall may well involve the neurohospitalist by nature of their presence and specialty interest. Beyond the clinical care of the individual patient, however, falls may be addressed systematically. The result is the potential to improve the care of the entire hospital population and to develop or fortify the infrastructure necessary to do so for other clinical conditions or events.
In this 2-part series, we will first assess the risk stratification tools that are available, and then define the scope of the problem and potential solutions through a review of the literature. The second article will present a guide to implementing a quality improvement project around hospital falls. Although specific to falls in the hospitalized patient, the goal is to present a stepwise approach which is broadly applicable.
Methods
A literature search using PubMed database was performed for articles published prior to January 21, 2012 concerning inhospital fall prevention programs. No time limit was set. Combinations of the words accidental falls (MESH), patient falls, inhospital falls, hospitals, hospitalization (MESH), acute care, prevention, intervention, economics, risk management, and adult were used. The Cochrane library was searched using the phrase “hospital fall interventions.” References from included articles and reviews were used to complete the search. The search was used to identify articles about predicting falls and interventions to reduce falls. A review of all abstracts eliminated articles regarding falls in outpatient settings, children, and letters. For studies regarding interventions, studies that were not randomized were excluded.
Risk Stratification
Risk stratification of falling patients is difficult, as the etiology of inpatient falls is multifactorial. In the literature, there are over 35 common factors thought to be directly related to inpatient falls. Over 15 scales attempt to identify patients at risk of falling.7–21 The majority of these tools have not been validated, include only 1 population, or lack adequate sensitivity or specificity for clinical use. Three of these fall risk tools have been validated in multiple studies across the populations. These are the St Thomas’s Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY), the Morse Fall Scale (MFS), and the Hendrich Fall Risk Model (HFRM).
The original phases of STRATIFY were completed within various hospitals in London, England. The population (n = 548) was limited to inpatients ≥65 years of age. When predicting falls within a week of admission at a local hospital, a STRATIFY score of ≥2 points had a sensitivity of 93% and a specificity of 88%. A score of ≥3 points had a sensitivity of 69% and a specificity of 96%.20
Since the initial evaluation of the STRATIFY risk tool (Figure 1) in 1997, multiple studies have examined the validity of the tool.7,22–24 A meta-analysis of 12 articles on STRATIFY completed by Harrington et al revealed that STRATIFY may be clinically useful in the specific settings where studied, but may not have accurate clinical use outside these areas.22 When compared to other fall risk stratification tools, the STRATIFY had lower sensitivity and higher specificity.
Figure 1.
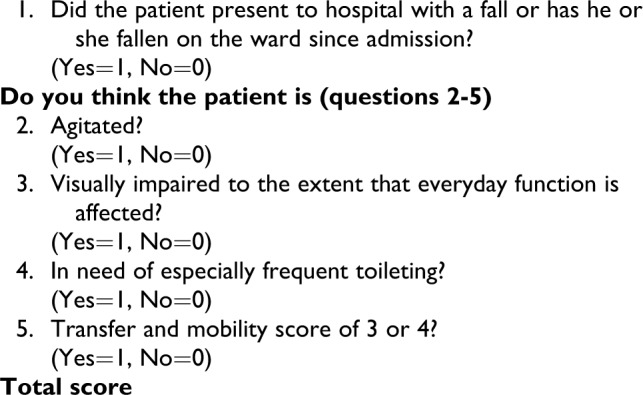
St Thomas’s Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) risk assessment tool.
The MFS (Figure 2) was prospectively trialed in 2 facilities and 3 types of clinical areas (n = 2689).18 Sensitivity of the original scale was 78% and specificity was 83%. This scale placed patients into categories of high risk (≥45), medium risk (25-44), and low risk (≤20). The meta-analysis by Harrington et al stated that the MFS had significantly higher sensitivity, but lower specificity than that of STRATIFY.22
Figure 2.
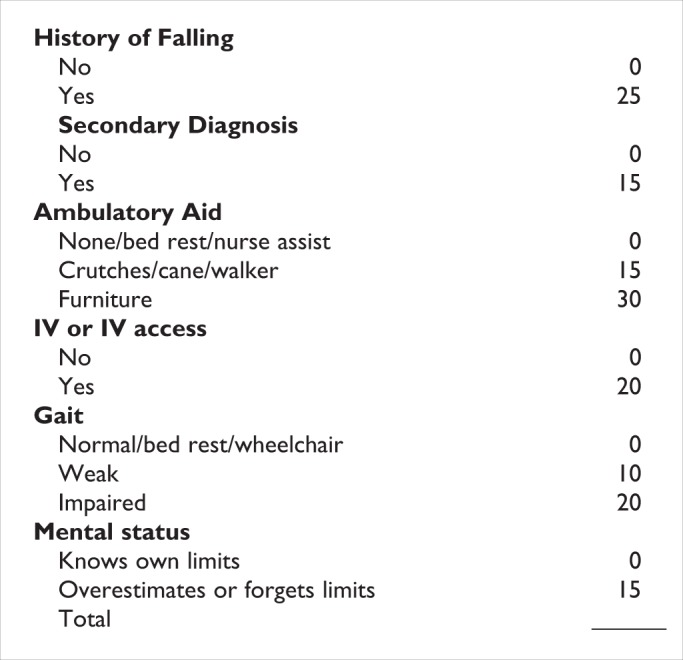
Morse Falls Scale.
The HFRM (Figure 3) divides patients into normal/low risk (0-2), high risk (3-6), and extremely high risk (>6) for inpatient falls.13 The original scale had a sensitivity of 77% and specificity of 72%. This study was a retrospective case–control chart review (n = 338) completed at a large Midwest teaching institution. Hendrich modified this scale into the Hendrich II Fall Risk Model (HFRM II) and validated the modified scale (Figure 4) with an additional case–control study (n = 338) in 2003 at a 750-bed acute care hospital. In this population, sensitivity and specificity of the HFRM II was similar to the HFRM in the first study (75% and 74%).14 The HFRM II has since been validated in an Italian acute geriatric unit (n = 179).25 The HFRM has been compared to the STRATIFY and the MFS. With a cutoff score of ≥5, the sensitivity of HFRM is 70% and specificity is 61%. Scoring ≥25 on the MFS has a higher specificity, 88%, but a lower specificity, 48.3%, makes the HFRM a more suitable tool. Of all the 3 tools, the HFRM was more user friendly and easier to score.23
Figure 3.
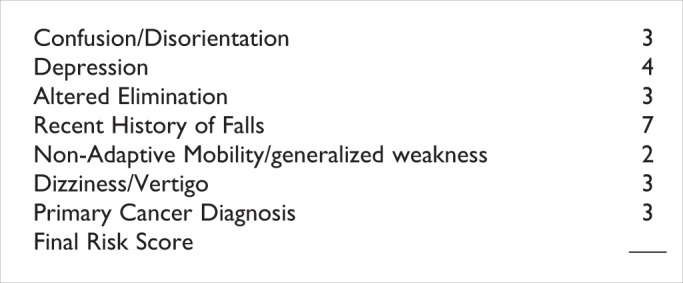
Hendrich High Risk Fall Model.
Figure 4.
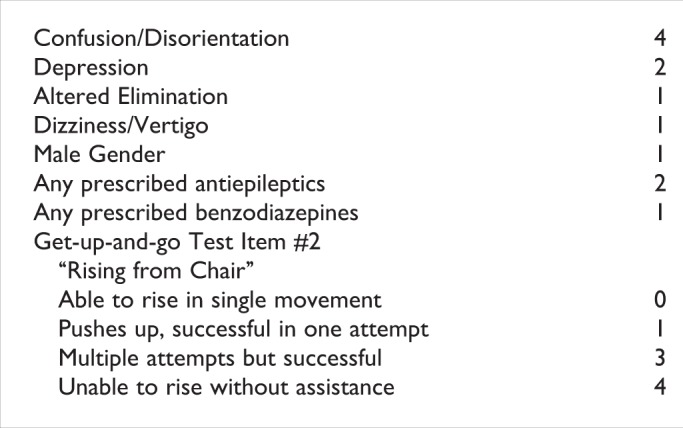
Hendrich II High Risk Fall Model.
Common themes that indicate increased risk of patient falls between these 3 tools, and others, include assessment for previous falls or admission secondary to falling, presence of mental confusion or agitation, necessity for frequent toileting, and altered gait or mobility.9,13,14,19,21,25–41 One of the most common populations studied and cited as high risk of falls is the older adult (≥65).8,16,17,27–30,42–48 Medications including benzodiazepines, anticonvulsants, antihypertensives, antidepressants, and sleep aids have also been targeted as high-risk medications.8,26–28,31–35,42,49–56 Two additional risk factors that are often mentioned are male sex and poor functioning or inability to independently perform activities of daily living.13,15,19,24,27,35,56,57
Although a multitude of studies have been performed on tools for fall risk stratification, the majority of these studies used tools specific to the institution or population of study, which makes it difficult, if not impossible, to generalize the use of these tools in practice. When selecting a tool, the operators must take into account the setting and the population of use. Many of these tools have been studied only in the older adult population. This is a glaring limitation when attempting to extrapolate their predictions to risk in patients younger than 65 years.
One must assess the performance of each tool in the context of tradeoff of sensitivity and specificity at the chosen risk cutoff score. The danger of decreasing sensitivity includes missed identification of patients at high risk of falling. Poor specificity can divert resources from the patients most at risk due to over targeting interventions toward patients at lower risk.
The most effective tools are those that are easy for the operator to use, allowing rescoring as patient status changes and providing adequate sensitivity and specificity for the specific population. The overall accuracy of each tool is greatly affected by setting and population. When looking for the highest sensitivity and specificity in general, the MFS has the highest sensitivity and STRATIFY tool has the highest specificity. If sheer ease of use is desired, the Hendrich Fall Model would be the tool of choice. It must be reiterated that if applying a new tool in a setting or population where previous study has not been completed, great caution and evaluation must be taken before permanent adoption of the new tool.
Interventions
Multiple interventions to prevent falls have been studied. Most studies are nonrandomized single-center reports with prospectively collected data. Our search criteria identified 15 randomized studies with a myriad of interventions. Table 1 briefly summarizes the studies, participants, interventions, and results. In the articles summarized in the table, there was no consensus regarding the method to screen patients. When screening tools were used, various screens were implemented, including the HFRM II, MFS, Downtown Fall Risk Score, and clinical judgment. Interventions were also variable including single interventions, multiple elements used on all patients, or elements targeted based on risk level or individual risk factors. Themes in the studies included staff and patient education, discreetly displaying high risk of falls, exercise, safety while ambulating (assistive devices, footwear, etc), medication use, and toileting.
Table 1.
Randomized Studies
| Study | Size | Participants | Intervention | Control | Outcome |
|---|---|---|---|---|---|
| Ang, 201158 | 1822. Intervention: 910. Control: 912. | Single center. Patients older than 21 years Score greater than 5 on the Hendrich II falls risk model. No in-hospital falls before risk assessment was performed. | Educational session (<30 minutes) to increase awareness of fall risk factors. Targeted interventions based upon risk factors. | Usual care, including a falls risk assessment, call button and bed locker placement, raised bed rails, and bed at the lowest position. | RR estimate of number of falls was 0.29 (95% CI 0.10-0.87 in favor of intervention group). HR 0.29% (95% CI 0.11-0.73, P = .019 log rank). Longer time to first fall (HR 0.29) |
| Barreca59 | 48. Intervention: 25. Control: 23. | Single center, rehabilitation unit. Block randomization. Stroke patients age 18 to 90 years, medically stable, postural control stage 3 or greater on Chedoke-McMaster Stroke Assessment (CMSA), and failed the third item of CMSA stage 4 postural control. | Staff education. Sit-to-stand exercise protocol for intervention group 3 times weekly for 45 minutes. Feedback between participants was encouraged. | Control group had 45 minutes of therapy 3 times weekly while seated in wheelchairs. Pet therapy, information sessions, word and picture games were included. | No difference in number of patients with falls (P = .70). Greater number of patients able to stand without using hands on 2 consecutive days (P = .02) |
| Burleigh60 | 205. Intervention: 101. Control: 104. Each group had 2 patients who stopped the drug and 1 with incomplete data. | Single center. General assessment and rehabilitation wards in an acute geriatric unit. Age older than 65. Exclusion: hypercalcemia, urolithiasis, dialysis, bed bound, previous calcium, and vitamin D supplementation. | Daily dose of 800 IU cholecalciferol plus 1200 mg calcium carbonate supplementation. | 1200 mg calcium carbonate supplementation daily. | No difference in falls (P = .263) or falls per person (P = .453). Trend toward fewer patients with falls, but not statistically significant (RR 0.82, 95% CI 0.59-1.16). |
| Cumming61 | 3999. Intervention: 2047, but only1907 received the intervention. Control: 1952. | Acute and rehabilitation elderly care wards in Sydney, Australia. 12 institutions with a total of 24 elderly care hospital wards. Cluster randomized trial, matched pairs of wards. | Risk assessment. Patient and family education. Walking aids, eyewear. Modifications to environment. Increased supervision. Discussion about medication, confusion, and foot issues with staff. Individual or group exercises. Sock alarm. | Usual care, which included fall prevention awareness. | No difference in falls between acute and rehabilitation wards per 1000 patient days. No difference in falls between intervention and control wards per 1000 patient days. |
| Donald62 | 54. Carpet: 28. Vinyl: 26. Additional physical therapy: 30. Routine therapy: 24. | Rehabilitation unit, elderly care patients. 2 × 2 controlled trial. | Risk assessment. Carpet flooring. Additional physical therapy. | Vinyl flooring. No additional therapy. | No significant difference in number of falls, but trend toward less falls on vinyl floor (P = .05, 95% CI 0.95-73). |
| Dykes63 | 10 264. Intervention: 5160. Control: 5104. | 4 hospitals. Cluster randomized design. Matched units randomized at each hospital, 8 total units. | Fall prevention tool kit in health information technology using Morse Falls Scale. Individualized poster placed above bed. Patient and family education individualized to patients needs. Fall plan automatically generated. | Usual care, which included Morse Falls scale, signs above beds for patients scoring >45 on scale, patient/family education, documentation in record. | Intervention group had fewer falls in per 1000 patient days (P = .04) and fewer patients with falls (P = .02). Not effective in the young, but lower fall rate per 1000 patient days (P = .004) in patients older than 65. |
| Haines64 | 1206. Complete program: 401. Materials only: 424. Control: 384 | 2 hospitals. Acute admission if >60 y old and expected to stay >3 days and all patients on subacute wards. More acute than subacute patients recruited. | 3-Group randomization, control, complete program, and materials only. Complete program: written and multimedia presentation (health-belief model) plus physiotherapist follow-up sessions over 1 week, and usual care. Materials only: written and video materials. | Usual care, which was variable between hospitals. Falls risk screening, arm bands, nursing checklist, and higher nurse to patient ratio for those who are agitated or confused. Physical and occupational therapy could be provided. | Fewer falls per 1000 patient days in cognitively intact patients’ intervention group when comparing the complete group vs materials only (aHR 0.51, 95% CI 0.28-0.93) and complete group vs control (aHR 0.43, 95% CI 0.24-0.78). No difference in fall rate per 1000 patient days in all the patients. |
| Haines65 | 626. Intervention: 310. Control: 316. | Single rehabilitation center. All patients accepted by geriatrician | Clinical judgment identified patients. Alert card with risk card with information brochure, exercise program, education program, and hip protectors. | Usual care, which included risk assessment tool and recommendations for interventions, but the interventions were not provided to the patients. | 30% fewer falls (P = .045) in intervention group. Trend toward reduction in number of fallers (RR 0.78, 95% CI 0.56-1.06, P = .02). |
| Healey66 | Intervention group before intervention implementation: 776. Intervention group after intervention implementation: 749. Control group before intervention implementation: 956. Control group after intervention implementation: 905. | 8 care of elderly wards or units of a hospital. 4 wards had acute patients or short-term rehabilitation. 2 wards had specialty wards (stroke and geriatric psychiatry) and 2 wards were long-term rehabilitation, respite, and terminal care. Intervention and control group participants were identified 6 months before and 6 months after intervention implementation. | Matched pairs of study wards. Risk factor screening. Care plans with targeted interventions including sensory aids, physiotherapy referrals, medication review, alterations to beds, evaluation for UTI, orthostasis, and footwear use. | Usual care, which included multidisciplinary interventions, such as physical therapy and mediation review. | Reduction of falls in intervention group, pre–post intervention (RR 0.79, CI 0.65-0.95), and intervention to control group (RR 0.71, 95% CI 0.55-0.90). |
| Kwok67 | 180. Intervention group with sensors used: 50. Intervention group with sensors not used: 40. Control: 90. | 2 geriatric wards specialized in stroke rehabilitation. | Bed-chair pressure sensors were encouraged. Education regarding use of sensors and improved outcomes when restraints not used. | Usual care, which included physical restraints and a fall prevention program. | No difference in use of physical restraints, improvement in mobility, or fall rate. |
| Mador68 | 71. Intervention: 36. Control: 35. | 2 hospitals. Patients with confusion and behavior disturbance, dementia, or delirium. >60 years old. Excluded if psychiatric illness as cause of behavior problems. | Assessment and advice from extended practice nurse on nonpharmacologic strategies for behavior. | Usual care, which included advice from a geriatrician regarding confusion and behavioral disturbance. | No significant change in number of patients who fell (P = .083). No difference in other outcome measures, such as agitation, medication use, length of stay, satisfaction, or discharge to nursing facility. |
| Mayo69 | 134 Intervention: 65. Control: 69. | Single rehabilitation facility. Patients with risk factors for falls or fractures only. | Bracelet identifying high-risk patients. | Usual care, which included a reminder to patients to be careful. | No difference in number of patients with falls (HR 1.3, 95% CI 0.8-2.4), injury from fall, or secondary end points. |
| Stenvall70 | 199. Intervention: 102. Control: 97. | Single center. Orthopedic and geriatric units. Femoral neck fracture. | 1 or 2 patients per room, 2 occupational therapists, dietician, staff education, care planning including plan to reduce recurrent falls and complications, nutritionist support, patient training in rehabilitation with emphasis on fall reduction. Home visits by PT/OT. | 1 to 4 patients per room, 0.5 occupational therapist, care planning was performed but not as frequently as intervention group, routine postoperative evaluation of complications. PT/OT provided, but no emphasis on fall risk factors. | Reduced rates of falls in intervention group (6.29 vs 16.28 per 1000 patient days). Fall incidence rate ratio 0.38 (P = .006, 95% CI 0.20-0.76) in favor of intervention units. |
| Tideiksaar71 | 70. Intervention: 35. Control: 35. | Single center, geriatric unit. | Performance-oriented environmental mobility screen. Bed alarm. | Usual care, which included nursing checks and physical restraints. | No statistical difference in falls (P = 1.00), but trend toward fewer falls in intervention group. |
| Vassallo72 | 825. Intervention: 275 (1 ward). Control group: 550 (2 wards). | Single center, rehabilitation unit. “Quasi-experimental.” thought to be quasi-randomization because study had no control over process and patients were randomly placed on 3 wards. | Downtown fall risk score. Multidisciplinary team including physician, nurse, occupational therapy, social work and physiotherapist. Weekly medical examination and fall risk assessment. Discussion and individualized interventions targeted at weekly meetings. | Usual care, which included discussion of falls at general meetings. Interventions could be implemented if recommended by a member of the care team. | Fewer fallers in intervention group (P = .033), fewer with injury (P = .025), and fewer falls (P = .045) during the study period. |
Abbreviations: aHR, adjusted hazard ratio; CI, confidence interval, HR, hazard ratio; IU, international unit; OT, occupation therapy; PT, physical therapy; RR, risk ratio; UTI, urinary tract infection.
Prior Systematic Reviews and Meta-Analyses
A Cochrane review analyzed 41 studies performed in the hospital setting. The rate of falls was reduced when multifactorial interventions were performed, as demonstrated in the 3 studies (risk ratio [RR] 0.73, 95% confidence interval [CI] 0.56-0.96). Three studies had exercise as the primary intervention, which reduced falls (RR 0.44, 95% CI 0.20-0.97).73 Other meta-analyses have variable results. One analysis suggested that fall prevention interventions did not reduce the number of falls, but was based on 8 studies of patients admitted to acute wards, rehabilitation, or extended care.2 A systematic review of 21 articles consisted of 2 randomized controlled trials, 1 prospective trial with parallel controls, and 18 articles that had historical controls. This review pooled the findings of the studies with historical controls and had a reduction in falls of 25%. The randomized and parallel control study interventions did not have a significant effect on the rate of falls.38 A subsequent review of 43 articles, 13 of which were related to inhospital falls, showed a rate ratio of 0.82 (95% CI 0.68-0.997) for falls and 0.59 (95% CI 0.22-1.58) for fractures, but the fracture rate reduction did not meet statistical significance.74 Limitations of prior systematic reviews include inclusion of studies which do not reflect the patient population seen in the typical acute care hospital.
Table 1 summarizes the studies of hospital fall reduction programs. Studies with variable sizes had a beneficial effect on fall rates, ranging from 19970 to 10 264 patients.63 The largest study that did not have a positive outcome had 3999 patients. It was not blinded, and the control group had fall reduction interventions instituted, as this was the hospital standard.61 The other negative studies were small, ranging from 5462 to 205 patients,60 and may have insufficient power to determine a clinical significance.
Of the 8 studies which showed interventions that had statistically significant results, the interventions were varied. Of the 8 studies, 7 had an impact on the number of fallers,58,63–66,70,72 while the remaining study had an effect on mobility.59 Themes across studies included patient education58,63–65,72 and rehabilitation modalities, such as exercise or physical therapy.59,64–66,70,72 Patient education tactics could be short, less than 30 minutes,58,65 and usually provided education that was specific to an individual patient.58,63,64 Only 1 study demonstrated a reduction in fall rates using a single intervention, education. Multimedia education proved to be superior to written education in patients with normal cognition.64
Rehabilitation experts, such as physical and occupational therapy, were frequent members of multidisciplinary teams, and provided a variety of interventions. Physical therapists provided education to patients in 1 instance,64 but provided exercise therapy in other studies.59,65,66,70,72 The intensity and specificity of the therapy was variable, ranging from a referral66 to 45-minute sessions targeted to a specific exercise program performed 3 times per week.59,65
The heterogenous nature of the positive studies makes identifying an effective single intervention or a combination of interventions difficult. Further investigation is needed to define interventions that will provide a significant reduction in falls or related harm in large populations in the acute care hospital.
Conclusion
In part 1, we defined the impact of falls on hospitalized patients as well as potentially effective interventions. One may be tempted to move directly to intervene once a problem is suspected. In order to effect real change, however, a true quality improvement initiative must be undertaken. This type of work is central to neurohospitalist practice, and part of what may distinguish a neurohospitalist from a neurologist who sees inpatients. Traditional neurology residency programs may touch on these processes, but quality improvement education more commonly occurs afterward, if at all.
Footnotes
Authors’ Note: All authors have contributed substantively to the conception design and analysis, the drafting of the manuscript or critical revision for important intellectual content, and final approval of the version to be published.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kalache A, Fu D, Yoshida S. WHO Global Report on Falls Prevention in Older Age. France: World Health Organization; 2007 [Google Scholar]
- 2. Coussement J, De Paepe L, Schwendimann R, Denhaerynck K, Dejaeger E, Milisen K. Interventions for preventing falls in acute- and chronic-care hospitals: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(1):29–36 [DOI] [PubMed] [Google Scholar]
- 3. Krauss MJ, Nguyen SL, Dunagan WC, et al. Circumstances of patient falls and injuries in 9 hospitals in a midwestern healthcare system. Infect Control Hosp Epidemiol. 2007;28(5):544–550 [DOI] [PubMed] [Google Scholar]
- 4. Fischer ID, Krauss MJ, Dunagan WC, et al. Patterns and predictors of inpatient falls and fall-related injuries in a large academic hospital. Infect Control Hosp Epidemiol. 2005;26(10):822–827 [DOI] [PubMed] [Google Scholar]
- 5. Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med. 1995;99(2):137–143 [DOI] [PubMed] [Google Scholar]
- 6.http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalAcqCond/Hospital-Acquired_Conditions.html Accessed May 21, 2012.
- 7. Barker A, Kamar J, Graco M, Lawlor V, Hill K. Adding value to the STRATIFY falls risk assessment in acute hospitals. J Adv Nurs. 2011;67(2):450–457 [DOI] [PubMed] [Google Scholar]
- 8. Browne JA, Covington BG, Davila Y. Using information technology to assist in redesign of a fall prevention program. J Nurs Care Qual. 2004;19(3):218–225 [DOI] [PubMed] [Google Scholar]
- 9. Byers V, Arrington ME, Finstuen K. Predictive risk factors associated with stroke patient falls in acute care settings. J Neurosci Nurs. 1990;22(3):147–154 [DOI] [PubMed] [Google Scholar]
- 10. Dempsey J. Risk assessment and fall prevention: practice development in action. Contemp Nurse. 2008;29(2):123–134 [DOI] [PubMed] [Google Scholar]
- 11. Forrester DA, McCabe-Bender J, Tiedeken K. Fall risk assessment of hospitalized adults and follow-up study. J Nurses Staff Dev. 1999;15(6):251–258 [DOI] [PubMed] [Google Scholar]
- 12. Haines TP, Hill K, Walsh W, Osborne R. Design-related bias in hospital fall risk screening tool predictive accuracy evaluations: systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci. 2007;62(6):664–672 [DOI] [PubMed] [Google Scholar]
- 13. Hendrich A, Nyhuis A, Kippenbrock T, Soja ME. Hospital falls: development of a predictive model for clinical practice. Appl Nurs Res. 1995;8(3):129–139 [DOI] [PubMed] [Google Scholar]
- 14. Hendrich AL, Bender PS, Nyhuis A. Validation of the hendrich ii fall risk model: a large concurrent case/control study of hospitalized patients. Appl Nurs Res. 2003;16(1):9–21 [DOI] [PubMed] [Google Scholar]
- 15. Large J, Gan N, Basic D, Jennings N. Using the timed up and go test to stratify elderly inpatients at risk of falls. Clin Rehabil. 2006;20(5):421–428 [DOI] [PubMed] [Google Scholar]
- 16. Lovallo C, Rolandi S, Rossetti AM, Lusignani M. Accidental falls in hospital inpatients: evaluation of sensitivity and specificity of two risk assessment tools. J Adv Nurs. 2010;66(3):690–696 [DOI] [PubMed] [Google Scholar]
- 17. Mertens EI, Halfens RJ, Dassen T. Using the care dependency scale for fall risk screening. J Adv Nurs. 2007;58(6):594–601 [DOI] [PubMed] [Google Scholar]
- 18. Morse JM, Black C, Oberle K, Donahue P. A prospective study to identify the fall-prone patient. Soc Sci Med. 1989;28(1):81–86 [DOI] [PubMed] [Google Scholar]
- 19. Myers H, Nikoletti S. Fall risk assessment: a prospective investigation of nurses' clinical judgement and risk assessment tools in predicting patient falls. Int J Nurs Pract. 2003;9(3):158–165 [DOI] [PubMed] [Google Scholar]
- 20. Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049–1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Salgado RI, Lord SR, Ehrlich F, Janji N, Rahman A. Predictors of falling in elderly hospital patients. Arch Gerontol Geriatr. 2004;38(3):213–219 [DOI] [PubMed] [Google Scholar]
- 22. Harrington L, Luquire R, Vish N, et al. Meta-analysis of fall-risk tools in hospitalized adults. J Nurs Adm. 2010;40(11):483–488 [DOI] [PubMed] [Google Scholar]
- 23. Kim EA, Mordiffi SZ, Bee WH, Devi K, Evans D. Evaluation of three fall-risk assessment tools in an acute care setting. J Adv Nurs. 2007;60(4):427–435 [DOI] [PubMed] [Google Scholar]
- 24. Milisen K, Staelens N, Schwendimann R, et al. Fall prediction in inpatients by bedside nurses using the St. Thomas's risk assessment tool in falling elderly inpatients (STRATIFY) instrument: a multicenter study. J Am Geriatr Soc. 2007;55(5):725–733 [DOI] [PubMed] [Google Scholar]
- 25. Ivziku D, Matarese M, Pedone C. Predictive validity of the Hendrich fall risk model II in an acute geriatric unit. Int J Nurs Stud. 2011;48(4):468–474 [DOI] [PubMed] [Google Scholar]
- 26. Ackerman DB, Trousdale RT, Bieber P, Henely J, Pagnano MW, Berry DJ. Postoperative patient falls on an orthopedic inpatient unit. J Arthroplasty. 2010;25(1):10–14 [DOI] [PubMed] [Google Scholar]
- 27. Cutillo-Schmitter TA, Rovner BW, Shmuely Y. Falls prevention study: a practical approach. J Healthc Risk Manag. 1996;16(4):56–68 [DOI] [PubMed] [Google Scholar]
- 28. Evans D, Hodgkinson B, Lambert L, Wood J. Falls risk factors in the hospital setting: a systematic review. Int J Nurs Pract. 2001;7(1):38–45 [DOI] [PubMed] [Google Scholar]
- 29. O'Hagan C, O'Connell B. The relationship between patient blood pathology values and patient falls in an acute-care setting: a retrospective analysis. Int J Nurs Pract. 2005;11(4):161–168 [DOI] [PubMed] [Google Scholar]
- 30. Salameh F, Cassuto N, Oliven A. A simplified fall-risk assessment tool for patients hospitalized in medical wards. Isr Med Assoc J. 2008;10(2):125–129 [PubMed] [Google Scholar]
- 31. Chen YC, Chien SF, Chen LK. Risk factors associated with falls among Chinese hospital inpatients in Taiwan. Arch Gerontol Geriatr. 2009;48(2):132–136 [DOI] [PubMed] [Google Scholar]
- 32. Chu LW, Pei CK, Chiu A, et al. Risk factors for falls in hospitalized older medical patients. J Gerontol A Biol Sci Med Sci. 1999;54(1):M38–M43 [DOI] [PubMed] [Google Scholar]
- 33. Frels C, Williams P, Narayanan S, Gariballa SE. Iatrogenic causes of falls in hospitalised elderly patients: a case-control study. Postgrad Med J. 2002;78(922):487–489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Giles LC, Whitehead CH, Jeffers L, McErlean B, Thompson D, Crotty M. Falls in hospitalized patients: can nursing information systems data predict falls? Comput Inform Nurs. 2006;24(3):167–172 [DOI] [PubMed] [Google Scholar]
- 35. Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732–739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Amador LF, Loera JA. Preventing postoperative falls in the older adult. J Am Coll Surg. 2007;204(3):447–453 [DOI] [PubMed] [Google Scholar]
- 37. Härlein J, Halfens RJ, Dassen T, Lahmann NA. Falls in older hospital inpatients and the effect of cognitive impairment: a secondary analysis of prevalence studies. J Clin Nurs. 2011;20(1-2):175–183 [DOI] [PubMed] [Google Scholar]
- 38. Oliver D, Hopper A, Seed P. Do hospital fall prevention programs work? A systematic review. J Am Geriatr Soc. 2000;48(12):1679–1689 [DOI] [PubMed] [Google Scholar]
- 39. Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122–130 [DOI] [PubMed] [Google Scholar]
- 40. Papaioannou A, Parkinson W, Cook R, Ferko N, Coker E, Adachi JD. Prediction of falls using a risk assessment tool in the acute care setting. BMC Med. Jan 2004;2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schmid AA, Wells CK, Concato J, et al. Prevalence, predictors, and outcomes of poststroke falls in acute hospital setting. J Rehabil Res Dev. 2010;47(6):553–562 [DOI] [PubMed] [Google Scholar]
- 42. Corsinovi L, Bo M, Ricauda Aimonino N, et al. Predictors of falls and hospitalization outcomes in elderly patients admitted to an acute geriatric unit. Arch Gerontol Geriatr. 2009 2009;49(1):142–145 [DOI] [PubMed] [Google Scholar]
- 43. Grue EV, Ranhoff AH, Noro A, et al. Vision and hearing impairments and their associations with falling and loss of instrumental activities in daily living in acute hospitalized older persons in five Nordic hospitals. Scand J Caring Sci. 2009;23(4):635–643 [DOI] [PubMed] [Google Scholar]
- 44. Halfon P, Eggli Y, Van Melle G, Vagnair A. Risk of falls for hospitalized patients: a predictive model based on routinely available data. J Clin Epidemiol. 2001;54(12):1258–1266 [DOI] [PubMed] [Google Scholar]
- 45. Heinze C, Halfens RJ, Dassen T. Falls in German in-patients and residents over 65 years of age. J Clin Nurs. 2007;16(3):495–501 [DOI] [PubMed] [Google Scholar]
- 46. Jones WJ, Simpson JA, Pieroni RE. Preventing falls in hospitals. The roles of patient age and diagnostic status in predicting falls. Hosp Top. 1991;69(3):30–33 [DOI] [PubMed] [Google Scholar]
- 47. Kerzman H, Chetrit A, Brin L, Toren O. Characteristics of falls in hospitalized patients. J Adv Nurs. 2004;47(2):223–229 [DOI] [PubMed] [Google Scholar]
- 48. Nakai A, Akeda M, Kawabata I. Incidence and risk factors for inpatient falls in an academic acute-care hospital. J Nihon Med Sch. 2006;73(5):265–270 [DOI] [PubMed] [Google Scholar]
- 49. Angalakuditi MV, Gomes J, Coley KC. Impact of drug use and comorbidities on in-hospital falls in patients with chronic kidney disease. Ann Pharmacother. 2007;41(10):1638–1643 [DOI] [PubMed] [Google Scholar]
- 50. Capone LJ, Albert NM, Bena JF, Morrison SM. Characteristics of hospitalized cancer patients who fall. J Nurs Care Qual. 2010;25(3):216–223 [DOI] [PubMed] [Google Scholar]
- 51. Chang CM, Chen MJ, Tsai CY, et al. Medical conditions and medications as risk factors of falls in the inpatient older people: a case-control study. Int J Geriatr Psychiatry. 2011;26(6):602–607 [DOI] [PubMed] [Google Scholar]
- 52. Patman SM, Dennis D, Hill K. The incidence of falls in intensive care survivors. Aust Crit Care. 2011;24(3):167–174 [DOI] [PubMed] [Google Scholar]
- 53. Rhalimi M, Helou R, Jaecker P. Medication use and increased risk of falls in hospitalized elderly patients: a retrospective, case-control study. Drugs Aging. 2009;26(10):847–852 [DOI] [PubMed] [Google Scholar]
- 54. Shorr RI, Guillen MK, Rosenblatt LC, Walker K, Caudle CE, Kritchevsky SB. Restraint use, restraint orders, and the risk of falls in hospitalized patients. J Am Geriatr Soc. 2002;50(3):526–529 [DOI] [PubMed] [Google Scholar]
- 55. Shuto H, Imakyure O, Matsumoto J, et al. Medication use as a risk factor for inpatient falls in an acute care hospital: a case-crossover study. Br J Clin Pharmacol. 2010;69(5):535–542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. McFarlane-Kolb H. Falls risk assessment, multitargeted interventions and the impact on hospital falls. Int J Nurs Pract. 2004;10(5):199–206 [DOI] [PubMed] [Google Scholar]
- 57. Czernuszenko A, Członkowska A. Risk factors for falls in stroke patients during inpatient rehabilitation. Clin Rehabil. 2009;23(2):176–188 [DOI] [PubMed] [Google Scholar]
- 58. Ang E, Mordiffi SZ, Wong HB. Evaluating the use of a targeted multiple intervention strategy in reducing patient falls in an acute care hospital: a randomized controlled trial. J Adv Nurs. 2011;67(9):1984–1992 [DOI] [PubMed] [Google Scholar]
- 59. Barreca S, Sigouin C, Lambert C, Ansley B. Effects of extra training on the ability of stroke survivors to perform an independent sit-to-stand: a randomized controlled trial. J Geriatr Phys Ther. 2004;27(4):59–68 [Google Scholar]
- 60. Burleigh E, McColl J, Potter J. Does vitamin D stop inpatients falling? A randomised controlled trial. Age Ageing. 2007;36(5):507–513 [DOI] [PubMed] [Google Scholar]
- 61. Cumming RG, Sherrington C, Lord SR, et al. Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital. BMJ. 2008;336(7647):758–760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Donald IP, Pitt K, Armstrong E, Shuttleworth H. Preventing falls on an elderly care rehabilitation ward. Clin Rehabil. 2000;14(2):178–185 [DOI] [PubMed] [Google Scholar]
- 63. Dykes PC, Carroll DL, Hurley A, et al. Fall prevention in acute care hospitals: a randomized trial. JAMA. 2010;304(17):1912–1918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Haines TP, Hill AM, Hill KD, et al. Patient education to prevent falls among older hospital inpatients: a randomized controlled trial. Arch Intern Med. 2011;171(6):516–524 [DOI] [PubMed] [Google Scholar]
- 65. Haines TP, Bennell KL, Osborne RH, Hill KD. Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial. BMJ. 2004;328(7441):676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age Ageing. 2004;33(4):390–395 [DOI] [PubMed] [Google Scholar]
- 67. Kwok T, Mok F, Chien WT, Tam E. Does access to bed-chair pressure sensors reduce physical restraint use in the rehabilitative care setting? J Clin Nurs. 2006;15(5):581–587 [DOI] [PubMed] [Google Scholar]
- 68. Mador JE, Giles L, Whitehead C, Crotty M. A randomized controlled trial of a behavior advisory service for hospitalized older patients with confusion. Int J Geriatr Psychiatry. 2004;19(9):858–863 [DOI] [PubMed] [Google Scholar]
- 69. Mayo NE, Gloutney L, Levy AR. A randomized trial of identification bracelets to prevent falls among patients in a rehabilitation hospital. Arch Phys Med Rehabil. 1994;75(12):1302–1308 [PubMed] [Google Scholar]
- 70. Stenvall M, Olofsson B, Lundström M, et al. A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporos Int. 2007;18(2):167–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Tideiksaar R, Feiner CF, Maby J. Falls prevention: the efficacy of a bed alarm system in an acute-care setting. Mt Sinai J Med. Nov 1993;60(6):522–527 [PubMed] [Google Scholar]
- 72. Vassallo M, Vignaraja R, Sharma JC, et al. The effect of changing practice on fall prevention in a rehabilitative hospital: the hospital injury prevention study. J Am Geriatr Soc. 2004;52(3):335–339 [DOI] [PubMed] [Google Scholar]
- 73. Cameron ID, Murray GR, Gillespie LD, et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Vol 1 The Cochrane Library2010: Art. No: DC005465 [DOI] [PubMed] [Google Scholar]
- 74. Oliver D, Connelly JB, Victor CR, et al. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2007;334(7584):82. [DOI] [PMC free article] [PubMed] [Google Scholar]


