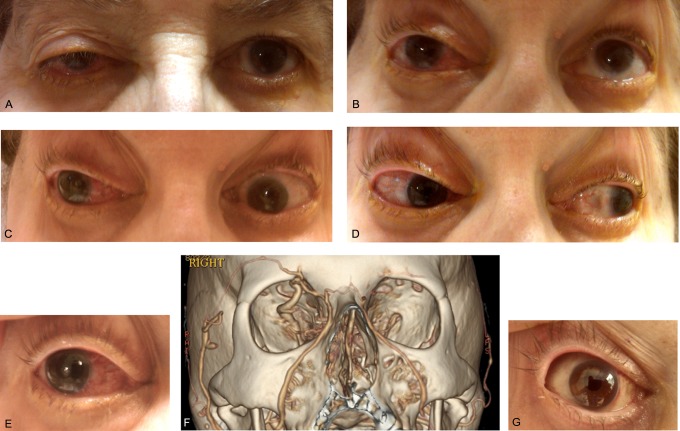
A 72-year-old woman awoke with double vision. Her physical examination revealed partial ptosis (Figure 1A); limitation of upgaze (Figure 1B), downgaze (Figure 1C), lateral gaze (Figure 1C), and medial gaze (Figure 1D); conjunctival injection (Figure 1E); and proptosis of the right eye. Computed tomography angiogram demonstrated an indirect carotid-cavernous fistula that was supplied by branches of the internal and external carotid arteries (Barrow D) and drained via superior ophthalmic, facial, and frontal cortical veins (Figure 1F). Given the risk of vision loss and intracerebral hemorrhage from retrograde cortical venous drainage,1 endovascular embolization was performed. One day following this, her conjunctival injection and double vision had improved (Figure 1G).
Figure 1.
Photographs of patient's extraocular examination prior to treatment demonstrating ptosis, gaze palsy, and conjunctival injection (A-E), computed tomography angiogram revealing dilated right superior ophthalmic and facial veins due to arteriovenous shunting from indirect carotid-cavernous fistula (F), and post-treatment photograph demonstrating resolution of conjunctival injection (G).
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Reference
- 1. van Dijk JM, terBrugge KG, Willinsky RA, Wallace MC. Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke. 2002;33(5):1233–1236 [DOI] [PubMed] [Google Scholar]