Abstract
The purine nucleoside adenosine is clinically employed in the treatment of supraventricular tachycardia. In addition, it has direct coronary vasodilatory effects, and may influence platelet aggregation. Experimental observations mechanistically link extracellular adenosine to cellular adaptation to hypoxia. Adenosine generation has been implicated in several pathophysiologic processes including angiogenesis, tumor defenses, and neurodegeneration. In solid organ transplantation, prolonged tissue ischemia and subsequent reperfusion injury may lead to profound graft dysfunction. Importantly, conditions of limited oxygen availability are associated with increased production of extracellular adenosine and subsequent tissue protection. Within the rapidly expanding field of adenosine biology, several enzymatic steps in adenosine production have been characterized and multiple receptor subtypes have been identified. In this review, we briefly examine the biologic steps involved in adenosine generation, and chronicle the current state of adenosine signaling in hepatic ischemia and reperfusion injury.
Keywords: Adenosine signaling, liver, ischemia, reperfusion
The first report describing adenosine signaling was published by Drury and Szent-Gyoergyi in 1929 (1). With the initial observation that intravenous adenosine causes rapid heart block, it is clinically employed in the treatment of supraventricular tachycardia (2). Biochemically, adenosine belongs to the molecular group of nucleosides composed of an adenine group attached to a ribose sugar. In addition to it's direct effects on heart conduction, there are clinical data to support a potent coronary vasodilatory effect (3) as well as inhibition of platelet aggregation (4).
As experimental experience is gained, numerous investigators suggest adenosine may possess multiple biologic functions in various tissues and cell types (5). Preclinical observations implicate adenosine as a key player in adaptation to hypoxia and leukocyte accumulation at the site of tissue injury. For example, signaling through various receptor subtypes may result in either enhanced or attenuated neutrophil adhesion to the vascular endothelium (6). In the setting of hypoxia, extracellular adenosine production attenuated neutrophil accumulation resulting in a potent anti-inflammatory signal. Conversely, selective adenosine receptor blockade enhanced pulmonary inflammation, edema, and attenuated gas exchange (7).
While several molecules involved in adenosine production have been recently characterized, and multiple receptor subtypes identified, the field of adenosine biology has rapidly expanded over the past decade. Herein, we briefly examine the basic biology of extracellular adenosine production, and chronicle the current role of adenosine signaling in hepatic ischemia and reperfusion injury.
Extracellular adenosine generation and signaling
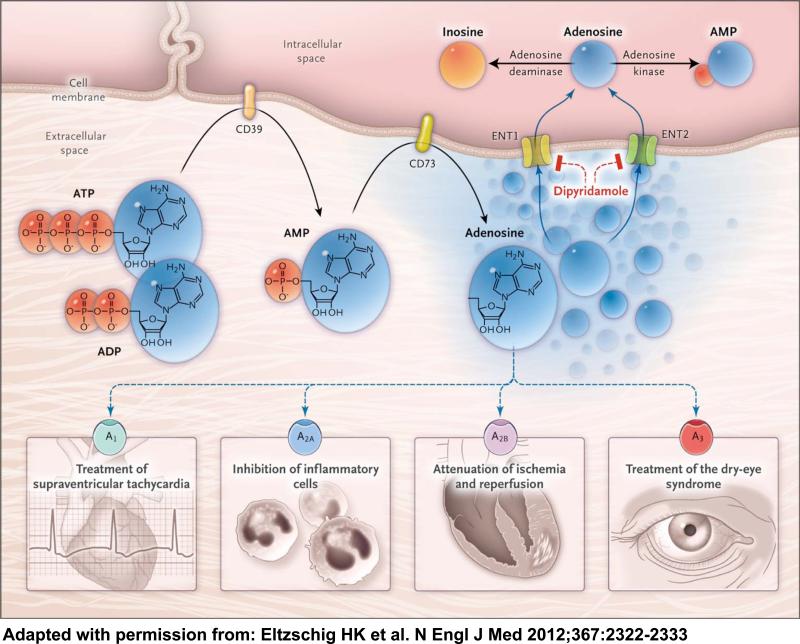
The enzymatic production of adenosine, from precursor molecules 5-adenosine triphosphate (ATP) and 5-adenosine di- and monophosphate (ADP, AMP), has recently been the focus of intense investigation. At baseline, intracellular concentrations of ATP are very high (5-8mM). Following cell death significant release into the pericellular space occurs. In addition, ATP and ADP are also delivered into the extracellular space from activated platelets by granular release or from inflammatory cells after activation (8). ATP and ADP are converted to AMP by ectoapyrase (CD39) expressed on the cell surface (Figure 1). This is a key step in the extracellular breakdown of ATP/ADP, both of which are central signaling molecules in thrombosis and inflammation (9). Consistent with this, gene-targeted mice for CD39 demonstrate increased susceptibility to ischemic injury in cardiac, renal, and hepatic ischemia (10-13), whereas overexpression confers protection observed in both warm and cold ischemic injury (14-16).
Figure 1. Extracellular adenosine signaling.
Extracellular adenosine is generated from enzymatic conversion of the precursor nucleotides ATP and ADP to AMP through the enzymatic activity of the ectonucleoside triphosphate diphosphohydrolase 1 (CD39) and the subsequent conversion of AMP to adenosine through ecto-5′-nucleotidase (CD73). Extracellular adenosine can signal through four distinct adenosine receptors: ADORA1 (A1), ADORA2A (A2A), ADORA2B (A2B), and ADORA3 (A3). Adapted from the New England Journal of Medicine with permission.
The final enzymatic step in adenosine production is catalyzed by 5-ecto-nucleotidase (CD73) which rapidly converts extracellular AMP to adenosine. This step is critical and appears to directly influence tissue injury. Reduced adenosine levels generally confer a proinflammatory state. Inhibition or genetic deletion of CD73 results in elevated AMP and reduced adenosine levels which may attenuate tissue injury (17, 18). For example, CD73 may have a critical role in intestinal barrier function during ambient hypoxia (19). In the setting of acute lung injury, both pharmacologic inhibition and targeted genetic deletion of cd73 resulted in worsening symptom severity (10). Reconstitution of either cd39 or cd73 null mice, with soluble apyrase or 5-nucleotidase, reversed the severity of ventilator-associated lung injury. Similar findings have been reported in cardiac and renal ischemia models (20, 21).
Adenosine can signal through four G-protein-coupled receptors, the ADORA1, ADORA2A, ADORA2B, and ADORA3. The ADORA1 and ADORA3 are coupled to the Gi subunit and thereby cause an inhibition of the cAMP pathway whereas the ADORA2A and ADORA2B are coupled to the Gs and Gq (22). Gs signaling activates protein kinase A, resulting in elevated cAMP. Gq activates protein kinase C, which also elevates cAMP. As these two pathways are often activated simultaneously, the end result is an elevation in intracellular calcium (23). The ADORA2B receptor has also been shown the activate mitogen activated protein kinase. However, the specific mechanisms are poorly understood. The ADORA1, ADORA2A, and ADORA3 are high-affinity receptors, and are activated by low concentrations (10nM - 1μM) of adenosine which are present under physiological conditions. In contrast, the ADORA2B is a low-affinity receptor, requiring higher concentrations of adenosine (10μM) for receptor activation (24). These levels of adenosine are typically seen in pathologic disturbances, such as during periods of hypoxia, ischemia, and other cellular distress (25). Extracellular adenosine has a very short half-life in the extracellular space mainly due to its rapid uptake into the intracellular space by nucleoside transporters (26, 27). Within the cell it is rapidly metabolized into inosine by adenosine deaminase or into AMP by adenosine kinase (28).
Of the four receptors identified, ADORA2B expression is induced during hypoxia. Over the past several years, studies using both pharmacologic (agonist/antagonist) approaches and/or genetic deletion, suggest a protective role of extracellular adenosine signaling via the ADORA2B receptor in several pathologic conditions. For example, in a murine model of experimental colitis the intestinal epithelia predominantly expressed the ADORA2B receptor (29). Furthermore, the severity of disease was increased in adora2b receptor deficient mice in the form of weight loss, colonic shortening, and disease activity indices. These findings may be linked to subsequent expression of anti-inflammatory markers including interleukin-10. Grenz and colleagues used gene-targeted mice to confirm a protective effect of ADORA2B signaling in renal ischemia. Following short intervals of ischemic preconditioning, 45 minutes of sustained arterial ischemia was performed. They documented a protective effect in mice deficient for each adenosine receptor subtype except the adora2b null mouse. Similarly, an ADORA2B antagonist blocked renal protection, while an agonist dramatically improved renal function and histologic injury (30). The authors’ suggest these observations have far reaching implications for renal preservation in the setting of solid organ transplantation.
Hypoxia and hepatic inflammation
With rare exception, hepatic inflammation following ischemia and reperfusion occurs in a sterile environment (31). This sterile response includes activation of both innate and adaptive responses. In 1997, Zwacka and colleagues made a simple but important observation demonstrating that T lymphocytes rapidly accumulated in the liver following ischemia and subsequent reperfusion which preceded the innate response (32). Confirmed by other investigators, these effects are likely induced by specific cytokine and chemokine expression (33). These early events lead to a disproportionate immune response that ultimately compromises organ function (34).
Depending on the relative expression pattern of adenosine receptors on different cell and tissue types, activation and signaling results in different biologic functions (35). Preclinical data suggest adenosine has a profound anti-inflammatory effect via ADORA2A signaling, mitigating T cell activation and proliferation (36). Furthermore, activation of macrophages, monocytes, platelets, and neutrophils is also attenuated by ADORA2A signaling (36, 37). In 2005, Day et. al. demonstrated that signaling via the ADORA2A receptor (i.e. – selective agonists, anatagonists, and gene deletion) dramatically reduced post-perfusion injury in the mouse liver. Subsequent work documents a definitive reduction in biochemical indices and histologic pathology using selective ADORA2A agonist (38).
Lappas and colleagues provided an alternate hypothesis to the rationale that hepatic ischemic injury is mediated by CD4+ T cells exclusively, yet found a similar link to ADORA2A activation (39). Interestingly, the rapidity of hepatic reperfusion injury was not consistent with the time frame required for activation of CD4+ T cell responses. In a very logical set of experiments they implicate a CD4+ T cell subset, the natural killer cell (NKT), in rapid parenchymal injury. Following exactly 72 minutes of total hepatic ischemia (via microclip portal occlusion) and 2 hours of reperfusion, they observed significant NKT expression of IFN-γ. Additionally, reduced reperfusion injury observed in RAG-1 knockout mice was restored to normal wild type levels following adoptive transfer of wild type NKT cells. The authors’ suggest that NKT activation is inhibited by ADORA2A receptor activation and conclude that reperfusion injury occurs as result of NKT-dependent IFN-γ expression resulting in cytokine expression from other cells in the liver.
NKT cells make up as much as 30% of total lymphocyte population in the mouse liver and are considered a central component of the innate immune response (40). This immune compartment can be rapidly activated with a marked upregulation of numerous proinflammatory cytokines and chemokines. Coa and colleagues at the University of Pittsburgh selectively activated NKT cells prior to hepatic ischemia as a cell-based form of preconditioning (41). Activation one hour prior to the ischemic insult significantly reduced subsequent neutrophil accumulation and tissue injury. The authors’ suggest these observations may be linked to both interleukin-13 and ADORA2A receptor-dependent mechanisms. NKT-induced protection was reversed by administration of an IL-13 neutralizing antibody as well as specific blockade of ADORA2A receptor. While other investigators implicate the NKT cell as a predominant mediator in post-perfusion liver injury, Coa suggests that early NKT activation may actually contribute to tissue protection via an ADORA2A-dependent pathway.
Until recently, the role of NKT cells following cold ischemia was not clear. A recent study by Pommey and colleagues provides a counter argument to the role of NKT cells in post-ischemic hepatic injury (42). Murine liver transplants were performed between donor mice overexpressing CD39 and wild type recipients. Following 18 hours of cold preservation, serum levels of alanine aminotransferase and interleukin-6 were lower at 6 hours post-transplant in the recipients transplanted with livers overexpressing CD39. Furthermore, pre-transplant depletion of CD4+ T cells in the donor, not deficiency of NKT cells, protected liver grafts from early reperfusion injury. The authors’ concluded that reduction in the number of resident CD4+ T cells in the donor, secondary to CD39 overexpression or pharmacologic depletion, resulted in significant protection associated with prolonged cold storage. This study suggests that the immune response may differ in the setting of prolonged cold ischemia and subsequent organ transplant versus warm local ischemia. In this model, conventional CD4+ T cell may be the “prime orchestrators” of early hepatic injury (39).
Hepatic conversion of adenosine and ADORA2B signaling
The principle cause of initial allograft dysfunction in solid organ transplantation is due to prolonged ischemia and subsequent reperfusion Unfortunately, restriction of blood flow, followed by restoration of perfusion results in tissue damage with extensive alteration in cellular function. The specific pathological processes involved include endothelial cell dysfunction (43), activation of cell-death programs (i.e. – apoptosis, autophagy, and necrosis), and alterations in transcriptional control of gene expression (31). These cellular changes result in a delay in graft function and may predispose liver recipients to both early and late graft loss. While long-term outcomes in liver transplant have dramatically improved over the last four decades, there is an intense scientific effort underway to enhance early graft dysfunction (44). As the donor pool is expanded in the form of extended criteria organs and living donation, therapeutic approaches targeting ischemia/reperfusion injury become increasingly more important.
Conditions of limited oxygen availability – such as hepatic ischemia – are associated with increased production of adenosine from precursor nucleotides (45). Hepatic ischemia is associated with the transcriptional induction of the ecto-apyrase (CD39) (19). Cd39−/− mice are more prone to hepatic ischemia and reperfusion, while CD39 is also critical for liver regeneration (46). Additional observations suggest that ischemic preconditioning of the mouse liver resulted in a significant increase in CD39 expression and improved outcomes following ischemia and reperfusion (13). Interestingly, targeted therapy with small interfering RNA for the transcription factor Sp1 attenuated CD39 expression and increased post-ischemic liver injury. CD39 disruption also resulted in impaired liver regeneration, increased vascular injury, and decreased survival (46). Following partial hepatectomy, mice chimeric with cd39 null bone marrow demonstrated impaired hematopoietic stem cell mobilization (47). Stem cell mobilization directly correlated with restoration of liver volume and function. Importantly, hematopoietic stem cells expressing CD39 were also mobilized in humans following major liver resection, and may be linked to regeneration. Overall, CD39 may instrumental in post-ischemic liver protection, and promoting regeneration, via local and systemic anti-inflammatory effects.
As CD39 continues to emerge as a potential therapeutic target in liver injury, less is known about the specific role of CD73 in protection from hepatocellular injury. Previous studies have shown adenosine production to have a protective role in liver ischemia. Following intervals of ischemic preconditioning, tissue levels of adenosine significantly increase and may directly influence to hepatocelluar function (48). Furthermore, preconditioning prior to a prolonged ischemic insult leads to several important changes in signaling. While preconditioning is associated with induction of CD73 expression, gene deletion or pharmacologic inhibition of CD73 worsened hepatic injury (18). Secondly, ischemic preconditioning resulted in increases in extracellular adenosine which was abolished in cd73 null mice. Finally, administration of soluble 5’-nucleotidase completely restored ischemic preconditioning-driven hepatic protection. Therefore, targeting CD73 activity, via 5”-nucleotidase-mediated increases in adenosine, may be a viable
At present, there are emerging data to suggest that the ADORA2B receptor plays a significant role in tissue protection during hypoxia and inflammation in several animal models (30, 49). However, characterization of adenosine signaling specifically in the setting of hepatic ischemia and reperfusion injury is in the early phases. Chouker and colleagues recently observed that the protective effects achieved by hypoxic preconditioning in the murine liver were negated when the ADORA2B is nonfunctional. Following brief exposure to hypoxia, mice underwent 45 minutes of left lobe liver ischemia followed by 4 hours of reperfusion. Biochemical indices, inflammatory markers, and histologic injury were used as quantitative endpoints. While hypoxic-preconditioning was protective in general, this effect was blunted in mice with adora2b gene deletions as well as those pre-treated with an ADORA2B antagonist. The authors’ suggest that the ADORA2B signaling pathway may be critical in the prevention of warm local ischemia and reperfusion injury (50). Currently, the role of the adenosine-ADORA2B signaling pathway following cold ischemic injury is unknown.
Implications and future directions
Cumulatively, extracellular adenosine production appears to have a global anti-inflammatory influence in the setting of hypoxia and inflammation. However, adenosine-mediated effects in the post-ischemic liver are not well characterized. While the ADORA2A receptor may be an important signaling mediator directing post-perfusion immune responses, the role of the ADORA2B receptor in the liver continues to be defined. Promising observations by several investigators suggest that signaling via the ADORA2B receptor is protective during limited oxygen availability. The ADORA2B receptor may represent a potential therapeutic target in hypoxia as baseline expression is generally low with significant elevation in the setting of inflammation (23). However, the transition from mice to human patients will require defining clinically significant side effects of pharmacologic agents that take advantage of adenosine signaling. In solid organ transplantation, the potential advantage of manipulating the adenosine-ADORA signaling pathways may provide a viable therapeutic strategy to reduce immune-mediated reperfusion injury and possibly influence hepatocellular function directly. Finally, the biology of adenosine generation, transport, and signaling in warm and cold ischemia require further study.
Acknowledgments
The present research work was supported by 1 KO8HL103900-02 to MAZ, an American Heart Association Grant to AG and National Health Institute Grants R01-HL0921, R01-DK083385, R01-HL098294 and a grant by the Crohn's and Colitis Foundation of America (CCFA) to HKE
Abbreviations
- ATP
adenosine triphosphate
- ADP
adenine diphosphate
- AMP
adenine monophosphate
- ADORA2B receptor
adenosine 2B receptor
- NKT
natural killer T-cell
Footnotes
Disclosure
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Reference
- 1.Drury AN, Szent-Gyorgyi A. The physiological activity of adenine compounds with especial reference to action upon the mammalian heart. J Physiol. 1929;68:213–237. doi: 10.1113/jphysiol.1929.sp002608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Belhassen B, Pelleg A. Electrophysiologic effects of adenosine triphosphate and adenosine on the mammalian heart: clinical and experimental aspects. Journal of the American College of Cardiology. 1984;4(2):414–24. doi: 10.1016/s0735-1097(84)80233-8. Epub 1984/08/01. [DOI] [PubMed] [Google Scholar]
- 3.Picano E, Trivieri MG. Pharmacologic stress echocardiography in the assessment of coronary artery disease. Curr Opin Cardiol. 1999;14(6):464–70. doi: 10.1097/00001573-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Hart ML, Kohler D, Eckle T, Kloor D, Stahl GL, Eltzschig HK. Direct treatment of mouse or human blood with soluble 5'-nucleotidase inhibits platelet aggregation. Arterioscler Thromb Vasc Biol. 2008;28(8):1477–83. doi: 10.1161/ATVBAHA.108.169219. [DOI] [PubMed] [Google Scholar]
- 5.Eltzschig HK, Carmeliet P. Hypoxia and inflammation. N Engl J Med. 2011;364(7):656–65. doi: 10.1056/NEJMra0910283. Epub 2011/02/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang D, Zhang Y, Nguyen HG, Koupenova M, Chauhan AK, Makitalo M, et al. The A2B adenosine receptor protects against inflammation and excessive vascular adhesion. The Journal of clinical investigation. 2006;116(7):1913–23. doi: 10.1172/JCI27933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eckle T, Faigle M, Grenz A, Laucher S, Thompson LF, Eltzschig HK. A2B adenosine receptor dampens hypoxia-induced vascular leak. Blood. 2008;111(4):2024–35. doi: 10.1182/blood-2007-10-117044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eltzschig HK, Eckle T, Mager A, Kuper N, Karcher C, Weissmuller T, et al. ATP release from activated neutrophils occurs via connexin 43 and modulates adenosine-dependent endothelial cell function. Circ Res. 2006;99(10):1100–8. doi: 10.1161/01.RES.0000250174.31269.70. [DOI] [PubMed] [Google Scholar]
- 9.Enjyoji K, Sevigny J, Lin Y, Frenette PS, Christie PD, Esch JS, 2nd, et al. Targeted disruption of cd39/ATP diphosphohydrolase results in disordered hemostasis and thromboregulation. Nature medicine. 1999;5(9):1010–7. doi: 10.1038/12447. [DOI] [PubMed] [Google Scholar]
- 10.Eckle T, Fullbier L, Wehrmann M, Khoury J, Mittelbronn M, Ibla J, et al. Identification of ectonucleotidases CD39 and CD73 in innate protection during acute lung injury. J Immunol. 2007;178(12):8127–37. doi: 10.4049/jimmunol.178.12.8127. [DOI] [PubMed] [Google Scholar]
- 11.Grenz A, Zhang H, Hermes M, Eckle T, Klingel K, Huang DY, et al. Contribution of E-NTPDase1 (CD39) to renal protection from ischemia-reperfusion injury. Faseb J. 2007;21(11):2863–73. doi: 10.1096/fj.06-7947com. [DOI] [PubMed] [Google Scholar]
- 12.Guckelberger O, Sun XF, Sevigny J, Imai M, Kaczmarek E, Enjyoji K, et al. Beneficial effects of CD39/ecto-nucleoside triphosphate diphosphohydrolase-1 in murine intestinal ischemia-reperfusion injury. Thrombosis and haemostasis. 2004;91(3):576–86. doi: 10.1160/TH03-06-0373. Epub 2004/02/26. [DOI] [PubMed] [Google Scholar]
- 13.Hart ML, Gorzolla IC, Schittenhelm J, Robson SC, Eltzschig HK. SP1-dependent induction of CD39 facilitates hepatic ischemic preconditioning. J Immunol. 2010;184(7):4017–24. doi: 10.4049/jimmunol.0901851. Epub 2010/03/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu B, Rajakumar SV, Robson SC, Lee EK, Crikis S, d'Apice AJ, et al. The impact of purinergic signaling on renal ischemia-reperfusion injury. Transplantation. 2008;86(12):1707–12. doi: 10.1097/TP.0b013e31819022bc. Epub 2008/12/24. [DOI] [PubMed] [Google Scholar]
- 15.Crikis S, Lu B, Murray-Segal LM, Selan C, Robson SC, D'Apice AJ, et al. Transgenic overexpression of CD39 protects against renal ischemia-reperfusion and transplant vascular injury. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2010;10(12):2586–95. doi: 10.1111/j.1600-6143.2010.03257.x. Epub 2010/09/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dwyer KM, Robson SC, Nandurkar HH, Campbell DJ, Gock H, Murray-Segal LJ, et al. Thromboregulatory manifestations in human CD39 transgenic mice and the implications for thrombotic disease and transplantation. The Journal of clinical investigation. 2004;113(10):1440–6. doi: 10.1172/JCI19560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hart ML, Henn M, Kohler D, Kloor D, Mittelbronn M, Gorzolla IC, et al. Role of extracellular nucleotide phosphohydrolysis in intestinal ischemia-reperfusion injury. Faseb J. 2008;22(8):2784–97. doi: 10.1096/fj.07-103911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hart ML, Much C, Gorzolla IC, Schittenhelm J, Kloor D, Stahl GL, et al. Extracellular adenosine production by ecto-5'-nucleotidase protects during murine hepatic ischemic preconditioning. Gastroenterology. 2008;135(5):1739–50. e3. doi: 10.1053/j.gastro.2008.07.064. [DOI] [PubMed] [Google Scholar]
- 19.Synnestvedt K, Furuta GT, Comerford KM, Louis N, Karhausen J, Eltzschig HK, et al. Ecto-5'-nucleotidase (CD73) regulation by hypoxia-inducible factor-1 mediates permeability changes in intestinal epithelia. The Journal of clinical investigation. 2002;110(7):993–1002. doi: 10.1172/JCI15337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eckle T, Krahn T, Grenz A, Kohler D, Mittelbronn M, Ledent C, et al. Cardioprotection by ecto-5'-nucleotidase (CD73) and A2B adenosine receptors. Circulation. 2007;115(12):1581–90. doi: 10.1161/CIRCULATIONAHA.106.669697. [DOI] [PubMed] [Google Scholar]
- 21.Grenz A, Zhang H, Eckle T, Mittelbronn M, Wehrmann M, Kohle C, et al. Protective role of ecto-5'-nucleotidase (CD73) in renal ischemia. J Am Soc Nephrol. 2007;18(3):833–45. doi: 10.1681/ASN.2006101141. [DOI] [PubMed] [Google Scholar]
- 22.Hasko G, Linden J, Cronstein B, Pacher P. Adenosine receptors: therapeutic aspects for inflammatory and immune diseases. Nature reviews Drug discovery. 2008;7(9):759–70. doi: 10.1038/nrd2638. Epub 2008/09/02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hasko G, Csoka B, Nemeth ZH, Vizi ES, Pacher P. A(2B) adenosine receptors in immunity and inflammation. Trends in immunology. 2009;30(6):263–70. doi: 10.1016/j.it.2009.04.001. Epub 2009/05/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fredholm BB, Irenius E, Kull B, Schulte G. Comparison of the potency of adenosine as an agonist at human adenosine receptors expressed in Chinese hamster ovary cells. Biochemical pharmacology. 2001;61(4):443–8. doi: 10.1016/s0006-2952(00)00570-0. Epub 2001/02/28. [DOI] [PubMed] [Google Scholar]
- 25.Fredholm BB. Adenosine, an endogenous distress signal, modulates tissue damage and repair. Cell Death Differ. 2007;14(7):1315–23. doi: 10.1038/sj.cdd.4402132. [DOI] [PubMed] [Google Scholar]
- 26.Eltzschig HK, Abdulla P, Hoffman E, Hamilton KE, Daniels D, Schonfeld C, et al. HIF-1-dependent repression of equilibrative nucleoside transporter (ENT) in hypoxia. The Journal of experimental medicine. 2005;202(11):1493–505. doi: 10.1084/jem.20050177. Epub 2005/12/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morote-Garcia JC, Rosenberger P, Nivillac NM, Coe IR, Eltzschig HK. Hypoxiainducible factor-dependent repression of equilibrative nucleoside transporter 2 attenuates mucosal inflammation during intestinal hypoxia. Gastroenterology. 2009;136(2):607–18. doi: 10.1053/j.gastro.2008.10.037. [DOI] [PubMed] [Google Scholar]
- 28.Morote-Garcia JC, Rosenberger P, Kuhlicke J, Eltzschig HK. HIF-1-dependent repression of adenosine kinase attenuates hypoxia-induced vascular leak. Blood. 2008;111(12):5571–80. doi: 10.1182/blood-2007-11-126763. [DOI] [PubMed] [Google Scholar]
- 29.Frick JS, MacManus CF, Scully M, Glover LE, Eltzschig HK, Colgan SP. Contribution of adenosine A2B receptors to inflammatory parameters of experimental colitis. J Immunol. 2009;182(8):4957–64. doi: 10.4049/jimmunol.0801324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grenz A, Osswald H, Eckle T, Yang D, Zhang H, Tran ZV, et al. The reno-vascular A2B adenosine receptor protects the kidney from ischemia. PLoS Med. 2008;5(6):e137. doi: 10.1371/journal.pmed.0050137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eltzschig HK, Eckle T. Ischemia and reperfusion--from mechanism to translation. Nature medicine. 2011;17(11):1391–401. doi: 10.1038/nm.2507. Epub 2011/11/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zwacka RM, Zhang Y, Halldorson J, Schlossberg H, Dudus L, Engelhardt JF. CD4(+) T-lymphocytes mediate ischemia/reperfusion-induced inflammatory responses in mouse liver. The Journal of clinical investigation. 1997;100(2):279–89. doi: 10.1172/JCI119533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Caldwell CC, Okaya T, Martignoni A, Husted T, Schuster R, Lentsch AB. Divergent functions of CD4+ T lymphocytes in acute liver inflammation and injury after ischemia-reperfusion. Am J Physiol Gastrointest Liver Physiol. 2005;289(5):G969–76. doi: 10.1152/ajpgi.00223.2005. [DOI] [PubMed] [Google Scholar]
- 34.van Golen RF, van Gulik TM, Heger M. The sterile immune response during hepatic ischemia/reperfusion. Cytokine & growth factor reviews. 2012;23(3):69–84. doi: 10.1016/j.cytogfr.2012.04.006. Epub 2012/05/23. [DOI] [PubMed] [Google Scholar]
- 35.Eltzschig HK, Thompson LF, Karhausen J, Cotta RJ, Ibla JC, Robson SC, et al. Endogenous adenosine produced during hypoxia attenuates neutrophil accumulation: coordination by extracellular nucleotide metabolism. Blood. 2004;104(13):3986–92. doi: 10.1182/blood-2004-06-2066. [DOI] [PubMed] [Google Scholar]
- 36.Lappas CM, Rieger JM, Linden J. A2A adenosine receptor induction inhibits IFN-gamma production in murine CD4+ T cells. J Immunol. 2005;174(2):1073–80. doi: 10.4049/jimmunol.174.2.1073. [DOI] [PubMed] [Google Scholar]
- 37.Ohta A, Gorelik E, Prasad SJ, Ronchese F, Lukashev D, Wong MK, et al. A2A adenosine receptor protects tumors from antitumor T cells. Proc Natl Acad Sci U S A. 2006;103(35):13132–7. doi: 10.1073/pnas.0605251103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Day YJ, Li Y, Rieger JM, Ramos SI, Okusa MD, Linden J. A2A adenosine receptors on bone marrow-derived cells protect liver from ischemia-reperfusion injury. J Immunol. 2005;174(8):5040–6. doi: 10.4049/jimmunol.174.8.5040. [DOI] [PubMed] [Google Scholar]
- 39.Lappas CM, Day YJ, Marshall MA, Engelhard VH, Linden J. Adenosine A2A receptor activation reduces hepatic ischemia reperfusion injury by inhibiting CD1d-dependent NKT cell activation. J Exp Med. 2006;203(12):2639–48. doi: 10.1084/jem.20061097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hammond KJ, Pellicci DG, Poulton LD, Naidenko OV, Scalzo AA, Baxter AG, et al. CD1d-restricted NKT cells: an interstrain comparison. J Immunol. 2001;167(3):1164–73. doi: 10.4049/jimmunol.167.3.1164. [DOI] [PubMed] [Google Scholar]
- 41.Cao Z, Yuan Y, Jeyabalan G, Du Q, Tsung A, Geller DA, et al. Preactivation of NKT cells with alpha-GalCer protects against hepatic ischemia-reperfusion injury in mouse by a mechanism involving IL-13 and adenosine A2A receptor. Am J Physiol Gastrointest Liver Physiol. 2009;297(2):G249–58. doi: 10.1152/ajpgi.00041.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pommey S, Lu B, McRae J, Stagg J, Hill P, Salvaris E, et al. Liver grafts from CD39-overexpressing rodents are protected from ischemia reperfusion injury due to reduced numbers of resident CD4(+) T cells. Hepatology. 2013;57(4):1597–606. doi: 10.1002/hep.25985. Epub 2012/07/26. [DOI] [PubMed] [Google Scholar]
- 43.Ogawa S, Gerlach H, Esposito C, Pasagian-Macaulay A, Brett J, Stern D. Hypoxia modulates the barrier and coagulant function of cultured bovine endothelium. Increased monolayer permeability and induction of procoagulant properties. The Journal of clinical investigation. 1990;85(4):1090–8. doi: 10.1172/JCI114540. Epub 1990/04/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tullius SG, Garcia-Cardena G. Organ procurement and perfusion before transplantation. N Engl J Med. 2009;360(1):78–80. doi: 10.1056/NEJMe0809215. [DOI] [PubMed] [Google Scholar]
- 45.Zeiser R, Penack O, Holler E, Idzko M. Danger signals activating innate immunity in graft-versus-host disease. J Mol Med (Berl) 2011;89(9):833–45. doi: 10.1007/s00109-011-0767-x. Epub 2011/05/17. [DOI] [PubMed] [Google Scholar]
- 46.Beldi G, Wu Y, Sun X, Imai M, Enjyoji K, Csizmadia E, et al. Regulated catalysis of extracellular nucleotides by vascular CD39/ENTPD1 is required for liver regeneration. Gastroenterology. 2008;135(5):1751–60. doi: 10.1053/j.gastro.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schmelzle M, Duhme C, Junger W, Salhanick SD, Chen Y, Wu Y, et al. CD39 modulates hematopoietic stem cell recruitment and promotes liver regeneration in mice and humans after partial hepatectomy. Annals of surgery. 2013;257(4):693–701. doi: 10.1097/SLA.0b013e31826c3ec2. Epub 2013/03/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yoshizumi T, Yanaga K, Soejima Y, Maeda T, Uchiyama H, Sugimachi K. Amelioration of liver injury by ischaemic preconditioning. Br J Surg. 1998;85(12):1636–40. doi: 10.1046/j.1365-2168.1998.00917.x. [DOI] [PubMed] [Google Scholar]
- 49.Hart ML, Jacobi B, Schittenhelm J, Henn M, Eltzschig HK. Cutting Edge: A2B Adenosine receptor signaling provides potent protection during intestinal ischemia/reperfusion injury. J Immunol. 2009;182(7):3965–8. doi: 10.4049/jimmunol.0802193. Epub 2009/03/21. [DOI] [PubMed] [Google Scholar]
- 50.Chouker A, Ohta A, Martignoni A, Lukashev D, Zacharia LC, Jackson EK, et al. In Vivo Hypoxic Preconditioning Protects From Warm Liver Ischemia-Reperfusion Injury Through the Adenosine A2B Receptor. Transplantation. 2012 doi: 10.1097/TP.0b013e31826a9a46. Epub 2012/10/18. [DOI] [PMC free article] [PubMed] [Google Scholar]