Abstract
Study Objectives:
Given the high prevalence of sleep problems in early childhood and the significant impact of parenting on children's sleep, the current study aimed to determine the factor structure and psychometric properties of a new measure for assessing sleep-related parenting behaviors and interactions among preschool-aged children—The Parent-Child Sleep Interactions Scale (PSIS).
Methods:
Data was collected among parents of 209 preschool-aged children in two diverse metropolitan areas. All parents completed demographic questionnaires, the Parent-Child Sleep Interaction Scale (PSIS), and the Child Behavior Checklist (CBCL). A subset of parents completed structured interviews using the Preschool Age Psychiatric Assessment (PAPA). Following data reduction procedures, exploratory factor analysis (EFA) using principal axis extraction and oblique rotation was conducted, and internal consistency was assessed. Associations between PSIS scores and sleep problems based on the CBCL and PAPA as well as child sleep problems during infancy were examined. Differences based on demographic variables including race/ethnicity were also investigated.
Results:
EFA revealed a three-factor solution explaining 60% of the variance in total PSIS scores. Individual factors based on 12 items were labeled Sleep Reinforcement, Sleep Conflict, and Sleep Dependence. Internal consistency for all subscales and total PSIS scores was acceptable. PSIS subscales were positively correlated with both CBCL and PAPA Sleep Problems. Sleep problems during the first year of life were associated with Sleep Conflict and total PSIS scores. Significant differences in PSIS scores based on race/ ethnicity were found.
Conclusions:
The PSIS shows promise as a valid measure of sleep-related parent/child behaviors and interactions among preschoolers.
Citation:
Alfano CA; Smith VC; Reynolds KC; Reddy R; Dougherty LR. The Parent-Child Sleep Interactions Scale (PSIS) for preschoolers: factor structure and initial psychometric properties. J Clin Sleep Med 2013;9(11):1153-1160.
Keywords: Parent-Child Sleep Interactions Scale (PSIS), sleep problems, bedtime, preschoolers, children, parenting behaviors, race, ethnicity
Adequate sleep is an important aspect of healthy development. Evidence for this conclusion comes from a large body of research documenting associations between inadequate or disrupted sleep and decrements in cognitive functioning, school adjustment, emotional regulation, and behaviors during the preschool and school-age years.1–6 Persistent early sleep disturbances also forecast the later development of psychopathology and substance use.7–9 Understanding of factors that promote and/or contribute to inadequate or disrupted sleep patterns early in life therefore has implications for both research and clinical practice.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Parenting behaviors are theorized to influence child sleep patterns, but validated instruments are lacking. The current study aimed to develop and test a brief measure for assessing sleep-related parenting behaviors and interactions among preschool-aged children, The Parent-Child Sleep Interactions Scale (PSIS).
Study Impact: The PSIS demonstrated good internal consistency and showed strong associations with independent measures of child sleep and behavior problems. The PSIS shows promise as a brief and valid measure of sleep-related parenting practices and interactions among preschool-aged children.
Bedtime resistance, nighttime fears, and middle of the night awakenings are common in preschoolers, affecting up to 35% of typically developing children.10–12 Although a range of child-level variables including neurodevelopmental and temperamental factors contribute to sleep-based individual differences, research has similarly established the influence of parenting behaviors as significant determinants of children's sleep patterns and behaviors.13–15 For example, one particularly important aspect of parenting is the establishment of and adherence to a consistent and appropriate bedtime. A regular bedtime, which helps facilitate transition from wakefulness to sleep, is independently associated with better sleep and adjustment in children.2,16–17 In preschool-aged children, later and irregular bedtimes are associated with longer periods required to initiate sleep, less overall sleep, and poorer sleep quality.18 Conversely, consistent bedtime routines have been linked with better sleep and daytime behaviors including fewer tantrums.19
Along with regular bedtimes and presleep routines, a range of other parenting practices and parent-child interactions likely serve to encourage or interfere with a child's capacity for sleep regulation. Surprisingly little research has focused on these relationships during the preschool years (i.e., 3-5 years). This empirical gap is particularly remarkable in light of normative developmental changes that occur during this period. As children transition from a crib to a bed, give up daytime naps, and learn to dress and care for themselves, parental involvement in sleep routines declines. Consistent with these changes, negative relationships between certain nighttime parenting behaviors and the quality and duration of child sleep have been reported. For instance, parental presence at sleep onset or after a nighttime awakening is associated with greater sleep-related problems in young children.10,14 The preschool years may therefore be a critical period for understanding the influence of specific parenting behaviors on children's sleep.
Importantly, the decisions that parents make with regard to their children's sleep reflect not only individual differences but also ethnically/culturally based beliefs and traditions. For example, whereas White preschool-aged children in the U.S. most commonly sleep in their own beds, a majority of Black and Hispanic children sleep with their parents.15 Black children also give up daytime naps at later ages than do White children.20 Such differences are similarly evident with regard to sleep schedules and routines. Among a large U.S. sample, Hale and colleagues13 found that Black and Hispanic families were significantly less likely to provide young children with regular bedtimes and bedtime routines even after accounting for a range of other relevant factors. Milan and colleagues15 also found significant racial/ethnic differences in specific presleep activities (e.g., White parents commonly read to their children at bedtime, while Black parents more often include bathing in bedtime routines). Although the precise nature of these differences is not well understood, there is a clear need to consider the role of culture as part of scale development related to children's sleep.
Several brief validated questionnaires for assessing children's sleep-wake patterns have emerged in recent years.21 Most measures screen for a range of potential sleep problems and disorders (e.g., insomnia, sleep disordered breathing, parasomnias) by assessing the occurrence/frequency of these problems. Measures for evaluating parenting behaviors and interactions surrounding sleep are comparatively lacking. Such assessment differs from sleep-wake assessment but is no less important to the construct of sleep since it provides necessary understanding of factors that may give rise to and/or exacerbate sleep problems.21 Indeed, the effectiveness of behavioral interventions may hinge upon such information. At least one validated questionnaire designed to assess parenting behaviors in relation to infants' sleep is available (e.g., the Parental Interactive Bedtime Behavior Scale),22 but no such measure exists for use in preschool-aged children.
The primary goals of the present study were to determine the factor structure of a new instrument for assessing sleep-related parent behaviors and interactions among preschool-aged children—the Parent-Child Sleep Interactions Scale (PSIS)— and to determine the instrument's psychometric properties. Thus, using exploratory factor analysis, we examined relationships between PSIS scores and child sleep problems based on a parent-report measure and a structured clinical interview. Associations between PSIS scores and parent-reported sleep problems during the first year of life also were explored. In addition, based on established relationships between nighttime sleep and daytime behavior problems,1–4 associations with internalizing and externalizing behaviors were investigated. Finally, we examined differences in PSIS scores based on race/ethnicity.
METHODS
Participants
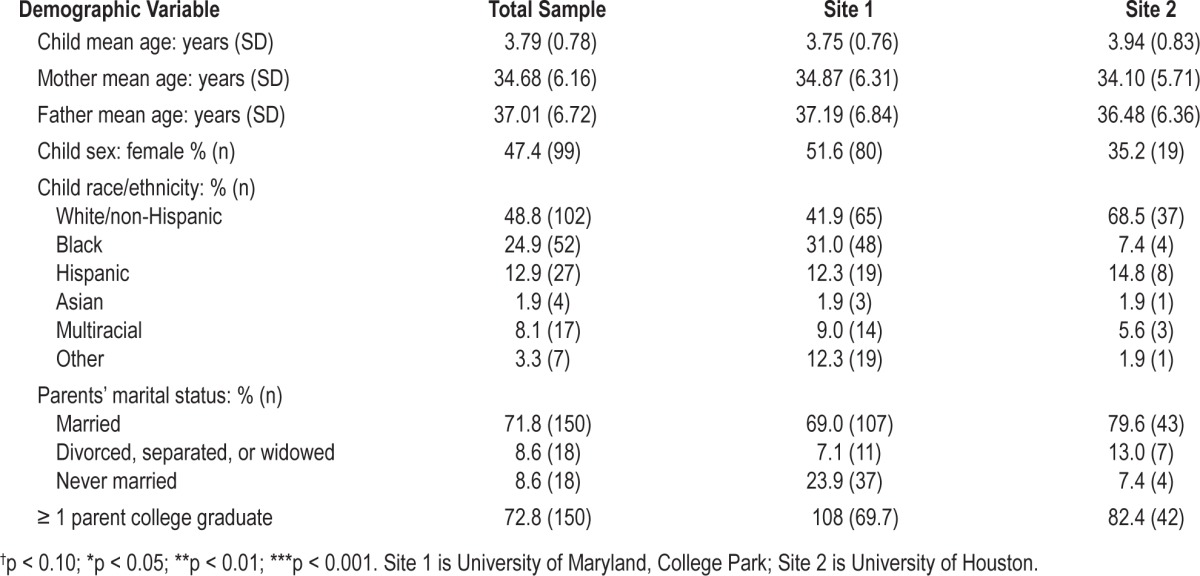
The parents of 209 preschool-aged children (ages 3 to 5 years; M = 3.79 years, SD = 0.78; 47.4% female) comprised the current sample. Families were recruited from the local community in 2 diverse metropolitan areas: Washington, DC, and Houston, TX. Families from the Washington, DC, area (n = 155; M = 3.75 years, SD = 0.76; 51.6% female) were recruited for a study on neuroendocrine function and risk for depression. Potential families were identified using advertisements/flyers sent to local schools, daycares, and health care providers. A proportion of flyers specifically targeted parents with a history of depression. Families with a child between 3 and 5 years of age who lived with an English-speaking biological parent, and who did not have significant medical conditions or developmental disabilities were eligible for the study. Participation included 2 laboratory visits that included observational assessments of child emotionality and behavior and parent-child interactions, and child and parent clinical assessments. The mean ages of mothers and fathers were 34.87 years (SD = 6.31) and 37.19 years (SD = 6.84), respectively. Participating families were White (41.9%), Black (31.0%), Hispanic (12.3%), Asian (1.9%), multiracial (9.0%), or other race/ethnicity (12.3%). Most children lived with 2 parents (72.9%) and had at least one parent with a 4-year college degree (69.7%).
Families in the Houston, TX, area (n = 54; M = 3.94 years, SD = 0.83; 35.2% female) were recruited for a study examining daytime and nighttime behavior in preschool-aged children using community flyers and advertisements. Families with a child between 3 and 5 years of age were invited to complete an online anonymous survey. None of the children had significant medical conditions or developmental disabilities. The mean ages of mothers and fathers were 34.10 years (SD = 5.71) and 36.48 years (SD = 6.36), respectively. Participating families were White (68.5%), Black (7.4%), Hispanic (14.8%), Asian (1.9%), multiracial (5.6%), or other race/ethnicity (1.9%). Like the Washington, DC, sample, most children lived with both biological parents (74.1%) and had at least one parent with a 4-year college degree (82.4%). Comparisons between the 2 subsamples did not reveal any significant site differences in child age, child gender, maternal age, paternal age, race/ ethnicity, parental marital status, and parental education (all p > 0.07). Similarly, the samples did not significantly differ in terms of any sleep or behavior measure. Therefore, data from both sites were combined in subsequent analyses. Demographic characteristics of the study sample are presented in Table 1. Both studies were approved by the institutional review boards at the University of Maryland and University of Houston.
Table 1.
Demographic characteristics of the study sample by site (N = 209)
Measures
Demographics/Child Development Questionnaire
All parents completed a questionnaire pertaining to the demographic characteristics of the family (race/ethnicity, marital status, and parental education, etc.) as well as the child's medical and developmental history. The questionnaire included a dichotomously scored item assessing whether the child had problems sleeping during the first year of life.
Parent-Child Sleep Interaction Scale
Parents completed the Parent-Child Sleep Interaction Scale (PSIS), a parent report measure developed to measure a wide range of bedtime behaviors and interactions among parents and their preschool-aged child. Thus, rather than specific bedtimes or other quantitative sleep indices, the PSIS was developed to assess sleep-related behaviors and parent-child interactions related to sleep that may give rise to and/or maintain problematic sleep patterns/disorders in young children, such as parental involvement in sleep routines, non-independent sleep patterns, and reinforcement of good sleep behaviors.
The PSIS was constructed based upon recommended procedures outlined by Spruyt and Gozal,23 including: (1) initial generation of items based on clinical and empirical evidence; (2) solicitation of input from experts; (3) administration of the questionnaire to a community sample; (4) item reduction procedures; (5) exploratory factor analysis (EFA); and (6) examination of internal consistency and convergent validity. Specifically, an initial list of items was generated by the first author and sent to 3 pediatric sleep experts (including a psychologist, a psychiatrist, and a developmental pediatrician) for review based on the items' relevance in assessing child sleep/bedtime routines. Expert feedback and recommendation resulted in an initial 35-item version of the measure. A Likert-type response format was created requiring parents to indicate how frequently each behavior/interaction occurred during the past month: 0 = never; 1 = rarely; 2 = sometimes; 3 = frequently; 4 = always/almost always.
Child Behavior Checklist for Ages 1½-5 (CBCL24)
All parents completed the CBCL, a 113-item parent-report scale assessing a broad range of behavioral problems, and social and academic functioning. The CBCL is one of the most extensively tested rating scales available and possesses excellent psychometrics.24 The measure yields a Total Problem Behavior score, 2 broad-band Internalizing and Externalizing scores, and 8 subscale scores. For the purpose of this study, the Internalizing, Externalizing and Sleep Problems Subscales were examined. The Sleep Problems Scale is composed of 7 items including: doesn't want to sleep alone, has trouble getting to sleep, nightmares, resists going to bed at night, sleeps less than most kids during day and/or night, talks or cries out in sleep, and wakes up often at night. As with other items on the CBCL, parents were asked to describe their child now or within the past 6 months (0 = not true, 1 = somewhat or sometimes true, and 2 = very true or often true). Internal consistency (Cronbach's α) for the Sleep Problems scale in the current study was 0.77.
Preschool Age Psychiatric Assessment (PAPA25)
Parents of preschoolers from the Washington, DC, sample (n = 155) were interviewed in person using the Preschool Age Psychiatric Assessment (PAPA), which uses a structured-format and interviewer-based approach to assess psychopathology in preschool-aged children, 2 to 6 years.25 Interviews were conducted by advanced graduate students in clinical psychology supervised by a Ph.D. level, licensed psychologist with extensive experience and training in the PAPA.
Fourteen dichotomously scored items from the PAPA assessing sleep problems were examined. Given the range of item content, an EFA was conducted using principle axis extraction and oblique rotation to identify an underlying factor structure. Items were removed if they failed to load onto any primary factor (i.e., loading < 0.40). Based on the eigenvalue > 1.0 rule and inspection of the scree plot, 3 factors were extracted consisting of a total of 9 items. Items from each factor were summed to yield 3 sleep scales: Inadequate Sleep (restless sleep, inadequately rested by sleep, morning irritability), Sleep Assistance (sleeps with family members, reluctance to sleep alone, night waking, rises to check on family members), and Daytime Sleepiness (seems sleepy during day, easily tired). In addition, all 9 items were summed to create a Total PAPA Sleep Problems scale. Interrater ICCs were acceptable for all scales: Inadequate Sleep (1.00); Sleep Assistance (0.98); Daytime Sleepiness (1.00), and PAPA Total Sleep Problems (0.99).
Data Analysis
Initial item reduction procedures were based on examination of item endorsement, content, and item-total correlations. An EFA using principal axis extraction and oblique rotation (oblimin) was used, as associations between sleep behaviors and interactions tend to be interrelated. Since little work has been conducted on presleep behaviors and parent-child interaction among preschoolers, we did not attempt to group the initial list of items within conceptually based factors. The critical eigenvalue was set at 1.0. Items were removed if they failed to load on any factor (loading < 0.50) or had high secondary loadings (> 0.30), and the analysis was re-run with the remaining items. The EFA continued in this manner until all remaining items had a primary factor loading > 0.50 and secondary loadings < 0.30. The psychometric properties of the fully scale and subscales were then assessed. Internal consistency was assessed by calculating Cronbach's α for PSIS total and all subscale scores.
Differences in PSIS scores based on demographic characteristics (e.g., child sex, parental education, and household income) were examined using t-tests, univariate analyses of variance (ANOVAs), and Pearson correlation coefficients. In order to assess convergent validity, correlations were calculated to determine associations between PSIS total and subscale scores, CBCL Sleep Problems Scores, and Sleep Problems reported during the PAPA. Correlations between PSIS scores, CBCL Internalizing and Externalizing subscales, and parent-endorsed sleep problems during the first year of life were also examined.
To increase statistical power for analyses, racial/ethnic groups were collapsed into 4 categories: White, Black, Hispanic, and Other. The “Other” group (n = 28) included children identified as multiracial, Asian, or other. Analyses using these 4 categories as compared to 6 racial/ethnic groups (i.e., White, Black, Hispanic, Asian, multiracial, and other) revealed similar results. All subsequent analyses therefore used the more parsimonious solution of 4 groups. To examine differences in PSIS scores across racial/ethnic groups, a series of univariate ANOVAs were conducted with race/ethnicity as the between-subject factor. Significant main effects were followed with post-hoc comparisons using Tukey's honestly significant difference (HSD) tests.
RESULTS
PSIS Item Reduction
We first examined response distributions for the 35 PSIS items to identify items with low variability (i.e., low sensitivity to individual differences). Six of the 35 items evidenced significantly unbalanced distributions (all skew and kurtosis p's < 0.01) and were therefore removed from the item pool. Next, using the criterion of 0.30 as an acceptable item-total correlation value,29 we examined item–total correlations among the remaining PSIS items. Eleven of the remaining 29 items failed to meet this criterion and were removed. One additional item was removed based on redundancy with another item (i.e., “My child sleeps in my bed all night” versus “My child sleeps in my room all night”). This resulted in a final list of 17 items used for factor analysis. The Kaiser-Meyer Olkin (KMO) statistic (0.784) and Bartlett's test of sphericity (χ2 = 1151.65) were both significant (p < 0.001) indicating suitability of these items for factor analysis.
Factor Structure of the PSIS
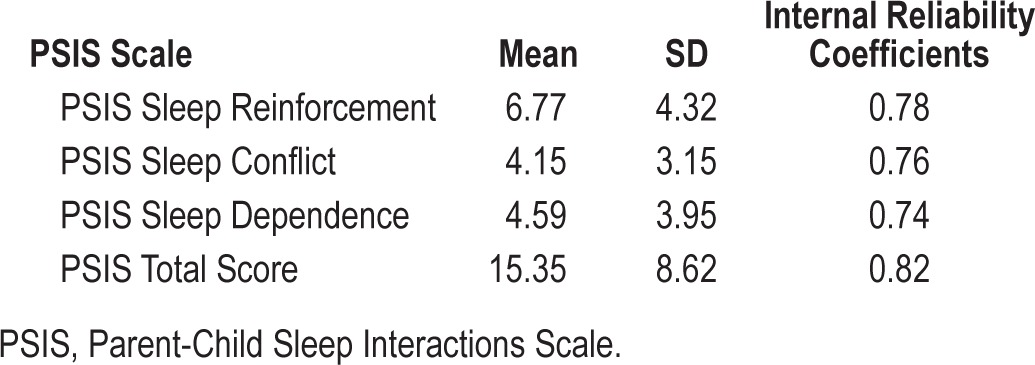
An EFA using principal axis extraction and oblimin rotation was conducted to identify the structure of the PSIS. Two of the 17 items did not load onto any individual factor and were removed from the dataset. The scree plot of eigenvalues for the remaining 15 items indicated that a 4-factor solution could be interpreted. The fourth factor (eigenvalue = 1.10) accounted for 7.3% of the variance in PSIS scores. However, the three items comprising this factor showed limited content/conceptual overlap and similarly low internal consistency (Cronbach's α = 0.53). These items were therefore removed and the EFA was re-run revealing a 3-factor solution (Table 2). Items loading on the first factor indicated this to be a measure of parental reassurance/reinforcement of child sleep behaviors. This factor was named Sleep Reinforcement and accounted for 33.1% of the variance in PSIS scores. The second factor, which accounted for 14.5% of the total variance, was named Sleep Conflict based on item loadings related to conflict and child noncompliance surrounding sleep. Item loadings on the third factor were indicative of problems with independent sleep. The third factor was named Sleep Dependence and accounted for 12.6% of the variance in PSIS scores. The 12-item PSIS scale showed good internal consistency (Cronbach's α = 0.82). Means, standard deviations, and internal consistency for the PSIS subscales also were acceptable and are presented in Table 3.
Table 2.
Rotated factor loadings from an exploratory factor analysis of items from the Parent-Child Sleep Interactions Scale
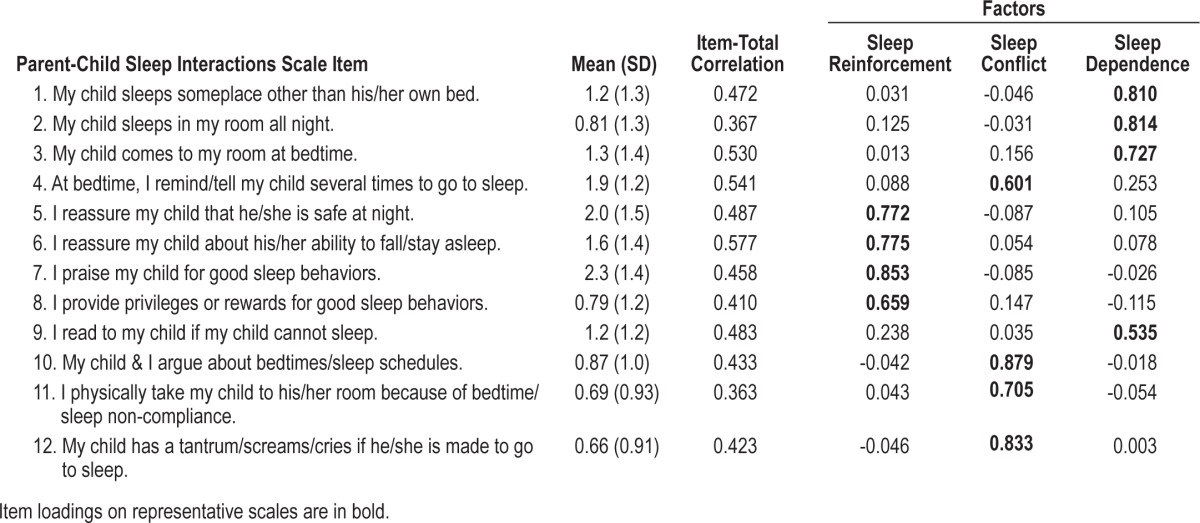
Table 3.
Means, standard deviations, and internal reliability coefficients for the PSIS scales
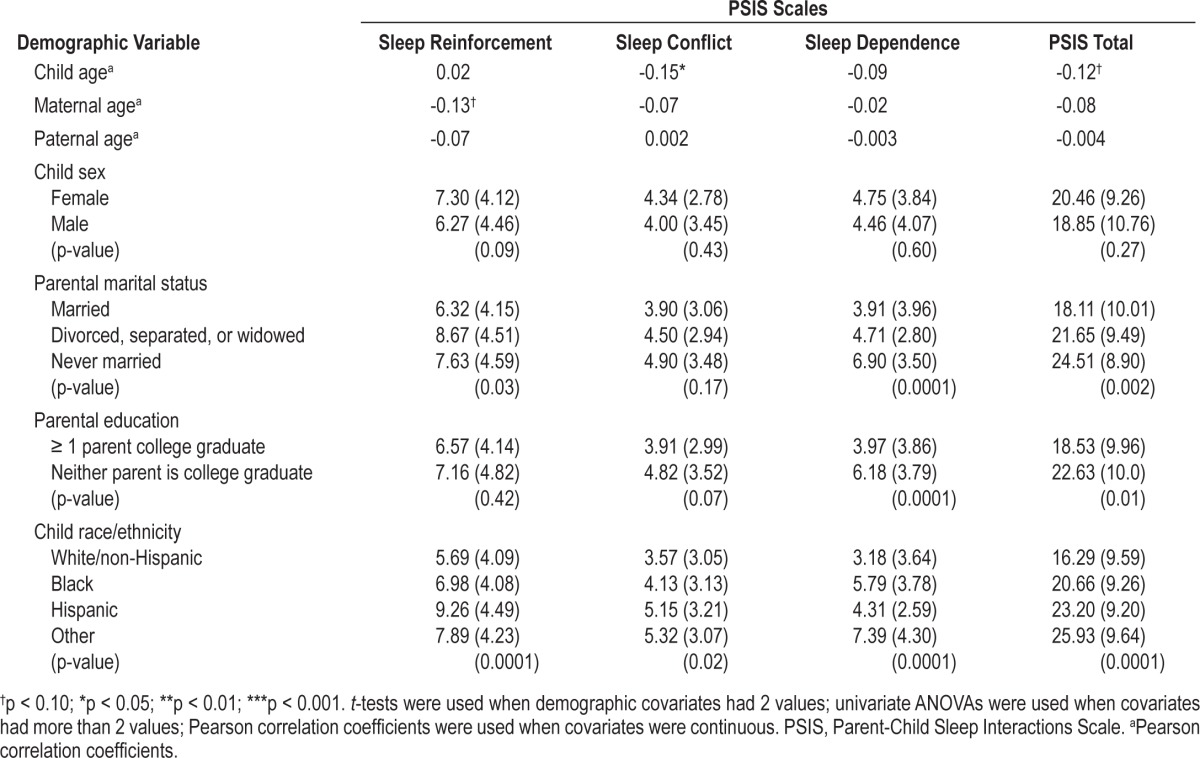
Associations between PSIS Scores and Demographic Variables
Table 4 summarizes the extent to which the PSIS scales were significantly associated with demographic variables. Child age was significantly negatively associated with Sleep Conflict scores; marital status was significantly associated with PSIS Total, Sleep Reinforcement, and Sleep Dependence scores, whereby married parents reported lower scores than children of parents who were divorced, separated, widowed, and/or never married; and parental education was significantly negatively associated with PSIS Total and Sleep Dependence scores. No significant associations were observed for maternal age or child gender.
Table 4.
Means and standard deviations by demographic variables on PSIS Scales
Associations between PSIS Scales and CBCL Sleep Problems
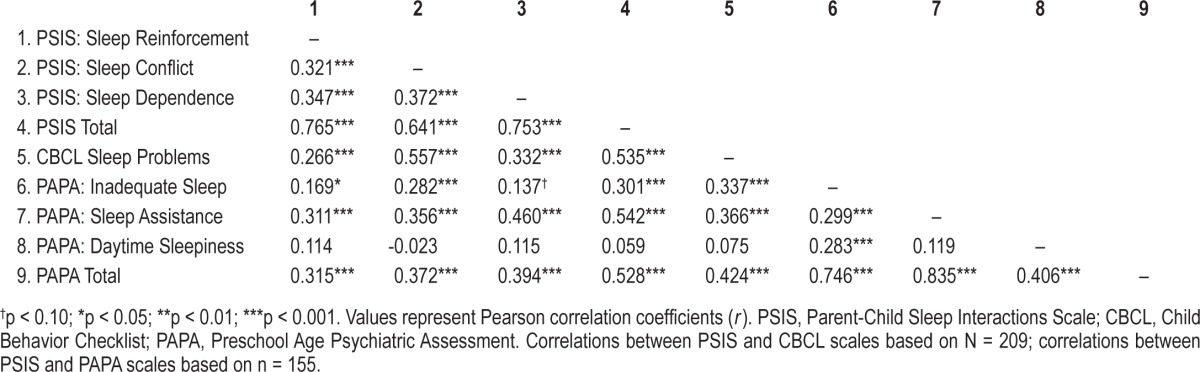
As shown in Table 5, PSIS Total scores as well as all 3 subscale scores were significantly positively correlated with CBCL Sleep Problems.
Table 5.
Convergent validity of the Parent-Child Sleep Interactions Scale with Child Behavior Checklist Sleep Problems, and Preschool Age Psychiatric Assessment Sleep Problems
Associations between PSIS Scales and CBCL Behavior Problems
CBCL Externalizing scores correlated significantly with PSIS Total scores (r = 0.30, p < 0.01), Sleep Conflict (r = 0.37, p < 0.01), and Sleep Dependence (r = 0.25, p < 0.01) scores. CBCL Internalizing scores were significantly correlated with PSIS Total (r = 0.24, p < 0.01) and Sleep Conflict (r = 0.31, p < 0.01) scores.
Associations between PSIS Scales and PAPA Sleep Problems
Correlation coefficients for the PSIS scales and PAPA Sleep scales are presented in Table 5.
Inadequate Sleep
PSIS Total scores, Sleep Reinforcement, and Sleep Conflict scores were significantly positively associated with PAPA Inadequate Sleep scores. Sleep Dependence was positively associated with PAPA Inadequate Sleep at a trend-level of significance.
Sleep Assistance
PSIS Total scores, Sleep Reinforcement, Sleep Conflict and Sleep Dependence scores were significantly positively associated with PAPA Sleep Assistance.
Daytime Sleepiness
No significant associations were observed between any of the PSIS scales and the PAPA Daytime Sleepiness scale.
PAPA Total Sleep Problems
PSIS Total scores, Sleep Reinforcement, Sleep Conflict, and Sleep Dependence scales were significantly positively associated with PAPA Total Sleep Problems.
Associations between PSIS Scores and Sleep Problems During Infancy
Child sleep problems during the first year of life were modestly but significantly associated with PSIS Sleep Conflict scores (r = 0.15, p < 0.05) as well as PSIS Total scores (r = 0.19, p < 0.01).
Racial/Ethnic Differences in PSIS Total and Subscale Scores
Univariate analysis of PSIS Total scores revealed a signifi-cant main effect for race/ethnicity, F3, 191 = 9.23, p < 0.001. Post hoc tests revealed that Black (M = 20.66, SD = 9.26), Hispanic (M = 23.20, SD = 9.20), and children of other race/ethnicities (M = 25.93, SD = 9.20) had significantly higher PSIS Total scores than White children (M = 16.29, SD = 9.59), p < 0.05, p = 0.01, and p < 0.001, respectively.
PSIS Sleep Reinforcement
A significant main effect of race/ethnicity was found for Sleep Reinforcement scores, F3, 203 = 6.20, p < 0.001. Post hoc tests indicated that Hispanic participants had significantly higher scores (M = 9.26, SD = 4.49) than White children (M = 5.69, SD = 4.09), p = 0.001.
PSIS Sleep Conflict
Analysis of Sleep Conflict scores revealed a significant main effect for race/ethnicity, F3, 205 = 3.48, p = 0.02. Tukey HSD post hoc tests revealed children in the Other race/ethnicity group to have significantly higher Sleep Conflict scores (M = 5.32, SD = 3.07) than White children (M = 3.57, SD = 3.05), p = 0.04.
PSIS Sleep Dependence
A significant main effect for race/ethnicity also emerged based on Sleep Dependence scores, F3, 197 = 12.09, p < 0.001. Post hoc tests revealed Black children to have significantly higher scores (M = 5.79, SD = 3.78) compared to White children (M = 3.18, SD = 3.64), p < 0.001. Children in the Other race/ethnicity group demonstrated significantly higher Sleep Dependence scores (M = 7.39, SD = 4.30) than White children (M = 3.18, SD = 3.64) and Hispanic children (M = 4.31, SD = 2.59), p < 0.001, and p < 0.01, respectively.
Results based on racial/ethnic group differences were similar when other demographic variables significantly associated with PSIS scores (i.e., child age, paternal age, parental marital status, parental education) were included in analyses.
DISCUSSION
Parent-child interactions are theorized to serve a regulating function on child sleep patterns since they act as external regulators of biological rhythms and capacity for self-regulation.26,27 As compared to measures that screen for specific sleep problems and disorders,28 validated instruments for assessing parent behaviors and parent-child interactions related to sleep are lacking. The factor structure and initial psychometric properties of the Parent-Child Sleep Interactions Scale (PSIS) were therefore evaluated in a large sample of preschool-aged children. Three discrete factors with substantial face validity emerged including Sleep Reinforcement, Sleep Conflict, and Sleep Dependence. These subscales explained 60% of the variance in Total PSIS scores. Internal consistency (i.e., reliability) for all subscales in addition to the total scale was good.
Associations between PSIS total and subscale scores and independent measures of child sleep problems (CBCL and PAPA sleep scales) provide evidence of satisfactory convergent validity. As would be expected, associations between the PSIS and sleep problems scales were positive and in the moderate range, with the exception of the PAPA Daytime Sleepiness scale for which nonsignificant associations were found. The latter result is somewhat surprising in light of significant relationships between PSIS scores and inadequate sleep scores on the PAPA but may relate to how sleepiness is exhibited during this developmental period (i.e., young children who are overly tired often become hyperactive). Significant associations also were identified between PSIS scores and CBCL Internalizing and Externalizing scores, corroborating findings from a wealth of research documenting associations between children's sleep at night and their emotional/behavioral functioning during the day.1–4
PSIS total and subscale scores also demonstrated expected associations with demographic variables. Consistent with normative declines in parental involvement related to sleep, we found a negative relationship between Sleep Conflict and child age. Children of married parents had lower Sleep Reinforcement and Sleep Dependence scores than children of parents who were divorced, separated, widowed, and/or never married. Also, lower levels of parental education were associated with higher PSIS total and Sleep Dependence scores. Overall, these findings are consistent with previous research demonstrating lower SES to be associated with more problematic sleep in children.30–32
Findings with regard to racial/ethnic differences are somewhat consistent with results from previous research13,15,20 and underscore the role of cultural differences in understanding child sleep habits and parent-child sleep interactions. White children in our sample had significantly lower PSIS total scores than all other racial/ethnic groups. Based on examinations of specific subscales, Black children had higher Sleep Dependence scores than White children, a finding consistent with those reported by Milan and colleagues.15 Children in the “Other” race/ethnicity category also scored higher on Sleep Dependence than both White and Hispanic children and had higher Sleep Conflict scores than White children. Finally, Hispanic children scored higher on Sleep Reinforcement than Caucasian children. To some extent, these results corroborate findings from previous studies13,15 indicating Black and Hispanic children are less likely to have consistent bedtimes and bedtime routines than White children.
Although we were able to examine potential differences among Black, Hispanic, and White children, the diverse composition of the “Other” racial/ethnic group renders these findings difficult to interpret. Indeed, this catch-all category necessarily included children of Asian, mixed, and other races/ ethnicities due to the overall small number of children falling into these groups. Larger multiracial samples are therefore an important direction for future research.33,34 It is similarly necessary to emphasize the importance of not assuming that ethnoracial differences in child sleep behaviors/patterns translate to child sleep problems or impairment. As an example, Milan and colleagues15 found that despite differences in bedtime routines and sleeping arrangements, no differences in sleep onset or daytime tiredness were found among Black, Hispanic, and White children. Overall, the growing diversity of families in the U.S. creates need for research focused on understanding relationships between culturally based sleep practices and children's sleep.
A number of other limitations are noteworthy. Due to the cross-sectional design of our study it is not possible to determine the directionality of identified relationships. For example, although some research suggests that greater parental involvement in bedtime and sleep routines interferes with a child's ability to regulate their sleep independently, it is equally possible that young children who experience problems sleeping require greater parental attention/interaction at night to help them settle to sleep. Follow-up studies based on prospective rather than retrospective reports are needed to clarify these relationships. Our study did not include an independent, validated measure of sleep problems in this age group but instead relied on two other validated but broad instruments for assessing behavior problems in young children. In conjunction with validated sleep instruments, future research including clinical populations (e.g., children with behavioral or sleep disorders) is needed to determine whether the PSIS can discriminate among subgroups of preschoolers. Finally, the fact that parents completed measures concerning sleep interactions/behaviors as well as child sleep problems creates the possibility of shared reporter variance. Convergent validity of the PSIS based on other types of sleep assessments (e.g., actigraphy, video of bedtime routines) remains to be established.
In summary, the PSIS is a brief, easy to administer measure of parent-child interactions and behaviors related to sleep in preschool-aged children. We envision the PSIS to have both clinical and empirical utility in identifying behaviors/interactions that may lead to and/or maintain sleep-related problems in young children. The PSIS may also have utility as a measure of effectiveness of behavioral sleep interventions. For example, an elevated Sleep Dependence score might signal a need for graduated extinction procedures in helping children to learn to sleep independently, whereas an elevated Sleep Conflict score might inform a focus on positive bedtime routines as part of treatment. In research settings, the PSIS may assist in delineating specific environmental mechanisms of early childhood insomnia. The PSIS items and scoring are included in Table 2 and we invite further use of this measure among clinicians and researchers.
DISCLOSURE STATEMENT
This was not an industry supported study. This research was supported in part by the University of Maryland (UMD) College of Behavioral and Social Sciences Dean's Research Initiative Award (LRD) and the UMD Research and Scholars Award (LRD) awarded to the last author. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the families who participated in this study.
REFERENCES
- 1.Anders T, Iosif A, Schwichtenberg AJ, Tang K, Goodlin-Jones B. Sleep and daytime functioning: a short-term longitudinal study of three preschool-age comparison groups. Am J Intellect Dev Disabil. 2012;117:275–90. doi: 10.1352/1944-7558-117.4.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bates JE, Viken RJ, Alexander DB, Beyers J, Stockton L. Sleep and adjustment in preschool children: sleep diary reports by mothers relate to behavior reports by teachers. Child Dev. 2002;73:62–75. doi: 10.1111/1467-8624.00392. [DOI] [PubMed] [Google Scholar]
- 3.DeVincent C, Gadow K, Delosh D, Geller L. Sleep disturbance and its relation to DSM-IV psychiatric symptoms in preschool-age children with pervasive developmental disorder and community controls. J Child Neurol. 2007;22:161–9. doi: 10.1177/0883073807300310. [DOI] [PubMed] [Google Scholar]
- 4.Lavigne J, Arend R, Rosenbaum D, et al. Sleep and behavior problems among preschoolers. J Dev Behav Pediatr. 1999;20:164–9. doi: 10.1097/00004703-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Dev. 2002;73:405–417. doi: 10.1111/1467-8624.00414. [DOI] [PubMed] [Google Scholar]
- 6.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 2003;74:444–55. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 7.Gregory A, Caspi A, Eley T, Moffitt T, O'Connor T, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J Abnorm Child Psychol. 2005;33:157–63. doi: 10.1007/s10802-005-1824-0. [DOI] [PubMed] [Google Scholar]
- 8.Roberts R, Roberts C, Chen I. Impact of insomnia on future functioning of adolescents. J Psychosom Res. 2002;53:561–9. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- 9.Wong M, Brower K, Zucker R. Childhood sleep problems, early onset of substance use and behavioral problems in adolescence. Sleep Med. 2009;10:787–96. doi: 10.1016/j.sleep.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson N, McMahon C. Preschoolers' sleep behaviour: Associations with parental hardiness, sleep-related cognitions and bedtime interactions. J. Child Psychol Psychiatry. 2008;49:765–73. doi: 10.1111/j.1469-7610.2007.01871.x. [DOI] [PubMed] [Google Scholar]
- 11.McGreavey J, Donnan P, Pagliari H, Sullivan F. The Tayside children's sleep questionnaire: a simple tool to evaluate sleep problems in young children. Child Care Health Dev. 2005;31:539–44. doi: 10.1111/j.1365-2214.2005.00548.x. [DOI] [PubMed] [Google Scholar]
- 12.Tikotzky L, Sadeh A. Sleep patterns and sleep disruptions in kindergarten children. J Clin Child Psychol. 2001;30:581–91. doi: 10.1207/S15374424JCCP3004_13. [DOI] [PubMed] [Google Scholar]
- 13.Hale L, Berger L, LeBourgeois M, Brooks-Gunn J. Social and demographic predictors of preschoolers' bedtime routines. J Dev Behav Pediatr. 2009;30:394–402. doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hayes M, Parker K, Sallinen B, Davare A. Bedsharing, temperament, and sleep disturbance in early childhood. Sleep. 2001;24:657–62. doi: 10.1093/sleep/24.6.657. [DOI] [PubMed] [Google Scholar]
- 15.Milan S, Snow S, Belay S. The context of preschool children's sleep: racial/ ethnic differences in sleep locations, routines, and concerns. J Fam Psychol. 2007;21:20–8. doi: 10.1037/0893-3200.21.1.20. [DOI] [PubMed] [Google Scholar]
- 16.Mindell JA, Telofski LS, Wiegand B, Kurtz ES. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep. 2009;32:599–606. doi: 10.1093/sleep/32.5.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Short M, Gradisar M, Wright H, Lack LC, Dohnt H, Carskadon MA. Time for bed: parent-set bedtimes associated with improved sleep and daytime functioning in adolescents. Sleep. 2011;34:797–800. doi: 10.5665/SLEEP.1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iwata S, Iwata O, Iemura A, Iwasaki M, Matsuishi T. Sleep architecture in healthy 5-year-old preschool children: associations between sleep schedule and quality variables. Acta Paediatr. 2012;101:e110–4. doi: 10.1111/j.1651-2227.2011.02515.x. [DOI] [PubMed] [Google Scholar]
- 19.Adams LA, Rickert VI. Reducing bedtime tantrums: comparison between positive routines and Graduated Extinction. Pediatrics. 1989;84:756–61. [PubMed] [Google Scholar]
- 20.Crosby B, LeBourgeois MK, Harsh JR. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics. 2005;115:225–32. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spruyt K, Gozal D. Pediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instruments. Sleep Med Rev. 2011;15:19–32. doi: 10.1016/j.smrv.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morrell J, Cortina-Borja M. The developmental change in strategies parents employ to settle young children to sleep, and their relationship to infant sleeping problems, as assessed by a new questionnaire: the Parental Interactive Bedtime Behavior Scale. Infant Child Dev. 2002;11:17–41. [Google Scholar]
- 23.Spruyt K, Gozal D. Development of pediatric sleep questionnaires as diagnostic or epidemiological tools: a brief review of dos and don'ts. Sleep Med Rev. 2011;15:7–17. doi: 10.1016/j.smrv.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Achenbach TM. Burlington, Vermont: Department of Psychiatry, University of Vermont; 1991. Manual for the child behavior checklist/4-18 and profile. [Google Scholar]
- 25.Egger HL, Ascher BH, Angold A. The Preschool Age Psychiatric Assessment: Version 1.1. Durham, North Carolina: Duke University Medical Center, Department of Psychiatry and Behavioral Sciences, Center for Developmental Epidemiology; 1999. [Google Scholar]
- 26.Anders TF. Infant sleep, nighttime relationships, and attachment. Psychiatry. 1994;57:11–21. doi: 10.1080/00332747.1994.11024664. [DOI] [PubMed] [Google Scholar]
- 27.Erath SA, Tu KM. The parenting context of children's sleep. In: El-Sheikh M, editor. Sleep and development: Familial and socio-cultural considerations. New York: Oxford University Press; 2011. pp. 29–49. [Google Scholar]
- 28.Gregory AM, O'Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41:964–71. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Nunnally JC, Bernstein IH. Psychometric theory. New York: McGraw-Hill; 1994. [Google Scholar]
- 30.Kelly RJ, El-Sheikh M. Marital conflict and children's sleep: reciprocal relations and socioeconomic effects. J Fam Psychol. 2011;25:412–22. doi: 10.1037/a0023789. [DOI] [PubMed] [Google Scholar]
- 31.Acebo C, Sadeh A, Seifer R, Tzischinsky O, Hafer A, Carskadon MA. Sleep/ wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children. Sleep. 2005;28:1568–77. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
- 32.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:e60. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 33.Iwata S, Iwata O, Matsuishi T. Sleep patterns of Japanese preschool children and their parents: implications for co-sleeping. Acta Paediatr. 2013;102:e257–62. doi: 10.1111/apa.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jenni OG, O'Connor BB. Children's sleep: an interplay between culture and biology. Pediatrics. 2005;115:204–16. doi: 10.1542/peds.2004-0815B. [DOI] [PubMed] [Google Scholar]


