Abstract
Kleine-Levin syndrome (KLS) is a rare sleep disorder characterized by periodic hypersomnia and various degrees of cognitive and behavioral disturbance, hyperphagia, and hypersexuality. Effective treatment is challenging. Stimulants marginally address sleepiness, but may increase irritability and do not improve cognitive and behavioral disturbances. Modafinil may shorten the symptomatic period but not the recurrence rate. Lithium and carbamazepine are beneficial in some cases, possibly related to similarities between KLS and affective disorders. Currently, no single medication is consistently successful in treating the syndrome. Here we report the short-term effect of clarithromycin in a patient with KLS.
Citation:
Rezvanian E; Watson NF. Kleine-Levin syndrome treated with clarithromycin. J Clin Sleep Med 2013;9(11):1211-1212.
Keywords: Kleine-Levin, hypersomnia, clarithromycin
Kleine-Levin Syndrome (KLS) is a rare sleep disorder of unknown cause characterized by repetitive, intermittent cycles of extreme sleepiness, and cognitive/behavioral disturbances including confusion, feelings of unreality, aggressiveness, and hypersexuality. Gamma-aminobutyric acid (GABA) is the predominant inhibitory neurotransmitter in the brain with well-known effects on sleep/wake cycle regulation. The GABAA receptor is the site where sleep-inducing drugs such as diazepam have their effects, and recent research suggests GABAA receptor antagonists may be useful in the treatment of hypersomnia.1 We sought to learn if clarithromycin, an antibiotic with GABAA receptor antagonistic properties, would be beneficial in the treatment of KLS.
REPORT OF CASE
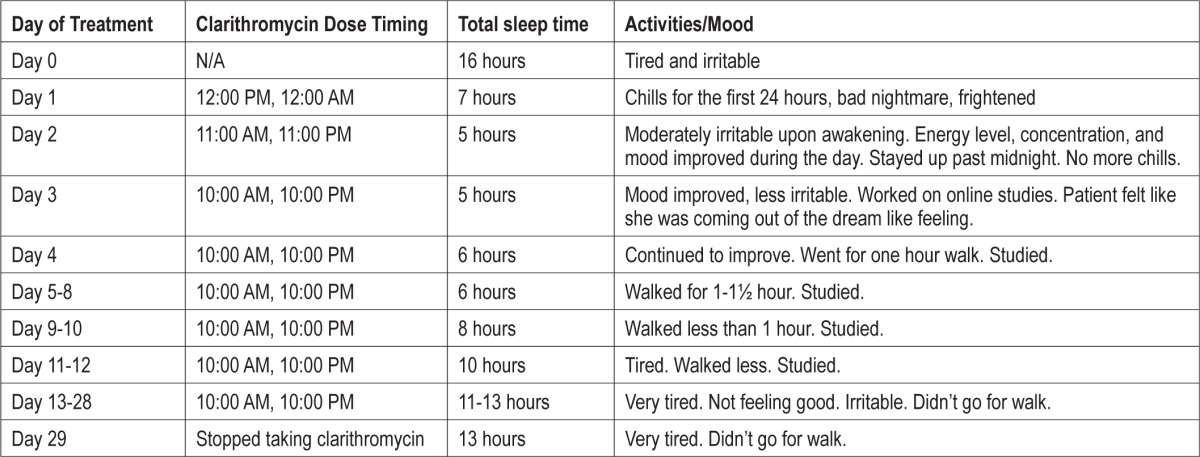
We report a 23-year-old female with KLS beginning at 10 years of age. Her diagnosis was consistent with ICSD-2 criteria and based on recurrent symptoms of hypersomnia, hypersexuality, irritability, and child-like behavior with a dreamlike state.2 KLS episode triggers included alcohol, upper respiratory infections, and general anesthesia. She slept 14 to 18 h/night during hyper-somnia episodes, which could last from weeks to months. She typically had headache, nausea, and vomiting at episode onset. MRI perfusion showed episode related reductions in thalamic perfusion.3 Episode length and duration were variable, but over time they had decreased in severity allowing performance of some of her daily life functions. Between episodes her sleep duration was approximately 9 h/night with normal mood and activity levels. She had no comorbid illness and took no regular medications. She had tried a number of medications for KLS, including prazosin, acetazolamide, methylphenidate, and liothyronine, all of which were discontinued due to either side effects or ineffectiveness. In the midst of a recent episode she had been started on clarithromycin 500 mg every 12 hours. She was on no other medications at that time. Within 24 h, her sleepiness had improved and sleep duration had decreased from 14-18 h to 5-8 h per night. She was able to complete her school work and resume her pre-KLS episode exercise regimen. Episode-related behavioral changes also improved, but mild cognitive issues persisted. Table 1 provides sleep diary information with subjective sleep hours and activities while being treated with clarithromycin. She experienced no side effects on the medication. Over ensuing weeks her sleep duration, daytime sleepiness, and ability to perform academically and physically slowly deteriorated back to pre-treatment levels. She ultimately discontinued clarithromycin after 29 days of use due to ineffectiveness.
Table 1.
Subjective sleep hours and activities while treated with clarithromycin
DISCUSSION
We report a case of KLS with an initial clinical response to clarithromycin, a macrolide antibiotic best known for inhibiting bacterial protein synthesis, but also functioning as a GABAA receptor antagonist. This latter functionality led us to use this treatment in our KLS patient.
Excitatory monoamines are either increased4 or within normal limits in the CSF of KLS patients,5 explaining the limited effectiveness of stimulants, which increase CSF monoamines, in treating this syndrome. This lack of monoaminergic involvement suggests a pathogenesis rooted in naturally occurring excess GABAergic signaling. Recent work suggests the presence of as yet undefined positive allosteric modulators of the GABAA receptor in hypersomnia patients, potentiating the effect of GABA on the receptor and enhancing GABAergic signaling.1
We observed a short-term beneficial effect of clarithromycin that dissipated over time. The time-limited effect of this medication has a number of potential explanations. Clarithromycin penetrates extra-cerebral tissue well, but reaches sufficient CSF concentration only in the presence of meningeal inflammation due to high molecular mass and affinity for P-glycoprotein.6 Viral and autoimmune causative factors have been suggested in KLS, based on the frequent report of flu-like meningeal symptoms such as headache, photophobia, confusion, altered consciousness, irritability, and drowsiness during episodes, and a significant association with DQB1*02.7,8 Meningeal inflammation that fades over time could influence CSF penetration of clarithromycin and dissipate its effectiveness. This notion supports the hypothesis of viral or post-infectious autoimmune meningoencephalitis as a cause of KLS.7 This dissipation effect may also explain why CSF is typically non-inflammatory in KLS,8 as this would be dependent on CSF sampling in relation to disease course. Another potential explanation is that undefined KLS-related CSF somnogens may act at sites in addition to the GABAA receptor.
In conclusion, this report shows a short-term beneficial effect of clarithromycin in KLS. The time-limited nature of the effect limits the practical usefulness of this medication, but it implies a role of the GABAA receptor in KLS pathophysiology. This finding suggests other medications that readily cross the blood brain barrier and act at this receptor, such as flumazenil,1 may have utility in KLS. This case also suggests the possible presence of meningeal inflammation during syndromic episodes. Further research demonstrating meningeal inflammation or disease-related CSF somnogens is needed.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Rye DB, Bliwise DL, Parker K, et al. Modulation of vigilance in the primary hypersomnias by endogenous enhancement of GABAA receptors. Sci Transl Med. 2012;4:161ra151. doi: 10.1126/scitranslmed.3004685. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Sleep Medicine. International classification of sleep disorders, 2nd edition: Diagnostic and coding manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 3.Billings ME, Watson NF, Keogh B. Dynamic fMRI Changes in Kleine-Levin Syndrome. Sleep Med. 2011;5:532. doi: 10.1016/j.sleep.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 4.Koerber RK, Torkelson R, Haven G, Donaldson J, Cohen SM, Case M. Increased cerebrospinal fluid 5-hydroxytryptamine and 5-hydroxyindoleacetic acid in Kleine-Levin syndrome. Neurology. 1984;34:1597–600. doi: 10.1212/wnl.34.12.1597. [DOI] [PubMed] [Google Scholar]
- 5.Landtblom AM, Dige N, Schwerdt K, Safstrom P, Granerus G. A Case of Kleine-Levin syndrome examined with SPECT and neuropsychological testing. Acta Neurol Scand. 2002;105:318–21. doi: 10.1034/j.1600-0404.2002.1c162.x. [DOI] [PubMed] [Google Scholar]
- 6.Periti P, Mazzei T, Mini E, et al. Clinical pharmacokinetic properties of the macrolide antibiotics. Effects of age and various pathophysiological states(part II) Clin Pharmacokinet. 1989;16:261–82. doi: 10.2165/00003088-198916050-00001. [DOI] [PubMed] [Google Scholar]
- 7.Dauvilliers Y, Mayer G, Lecendreux M, et al. Kleine-Levin syndrome: an autoimmune hypothesis based on clinical and genetic analyses. Neurology. 2002;59:1739–45. doi: 10.1212/01.wnl.0000036605.89977.d0. [DOI] [PubMed] [Google Scholar]
- 8.Arnulf I, Lin L, Gadoth N, et al. Kleine-Levin syndrome: a systematic study of 108 patients. Ann Neurol. 2008;63:482–93. doi: 10.1002/ana.21333. [DOI] [PubMed] [Google Scholar]


