Abstract
Background and aims: The current investigation was aimed at the development of a novel non-invasive treatment system, “pinpoint plantar long-wavelength infrared light irradiation (PP-LILI)”, which may be able to relieve mental stress and reduce stress-related hormones.
Materials (Subjects) and methods: We compared the subcutaneous temperature, blood pressure, the degree of secretion of stress hormones before and after pinpoint irradiations (wavelength: 8–11 μm; output: 30mW). The study enrolled 15 subjects (Japanese healthy adults; 8 males, 7 females; average age 47.8 ± 14.6 years). Two parts of the planter region were irradiated for 15 min respectively. The stress markers such as ACTH, salivary amylase and cortisol were measured. As well, core body temperature and blood pressure were analyzed before and after the irradiation.
Results: A series of experiments revealed increased body temperature, decreased levels of blood pressure and stress markers described above after the irradiation.
Conclusions: These results clearly suggest that the PP-LILI system will be quite useful for relieving stress and improvement of homeostatic functions in the body.
Keywords: Pinpoint plantar long-wavelength light irradiation (PP-LILI), relieving stress, stress hormones, body temperature, blood pressure
Introduction
In recent years, there has been a rapid increase in diseases caused by the stress of daily living, but specific treatment methods have yet to be developed to treat these conditions. According to the 2010 Comprehensive Survey of the Living Conditions of the People performed by the Ministry of Health, Labour and Welfare of Japan, 46.5% of individuals aged 14 years and above undergo stress. Stress stimulates the sympathetic nerves and is known to reduce peripheral blood circulation and homeostatic functions. 1–4)
Stress-related diseases are increasing in incidence and have long been a social problem. Excessive stress is detected by the cerebral neocortex and its signaling pathways are communicated to the hypothalamus, which then secretes corticotropin-releasing hormone (CRH). CRH communicates stress through two pathways: (1) via the endocrine system by promoting the secretion of cortisol from the adrenal cortex and adrenocorticotropic hormone (ACTH) from the anterior pituitary gland and (2) via the autonomic nervous system by promoting the secretion of adrenaline/noradrenaline from the adrenal medulla resulting in the stimulation of the sympathetic nervous system to promote the secretion of noradrenaline.
This response leads to vasoconstriction, reducing peripheral blood circulation, and causes harmful biological responses including hypothermia and sensitivity to the cold. Although warm foot baths and other methods have been suggested to cope with stress, there is no clear scientific proof to support their use in evidence-based medicine (EBM). This study employed non-invasive pinpoint irradiation in the plantar region and the measurement and statistical analysis on changes in peripheral subcutaneous temperature, blood pressure, and stress hormones (amylase, cortisol, ACTH) after the treatment to assess whether this method may reduce stress-related adverse responses and improve homeostatic functions (Figure 1).
Figure 1:
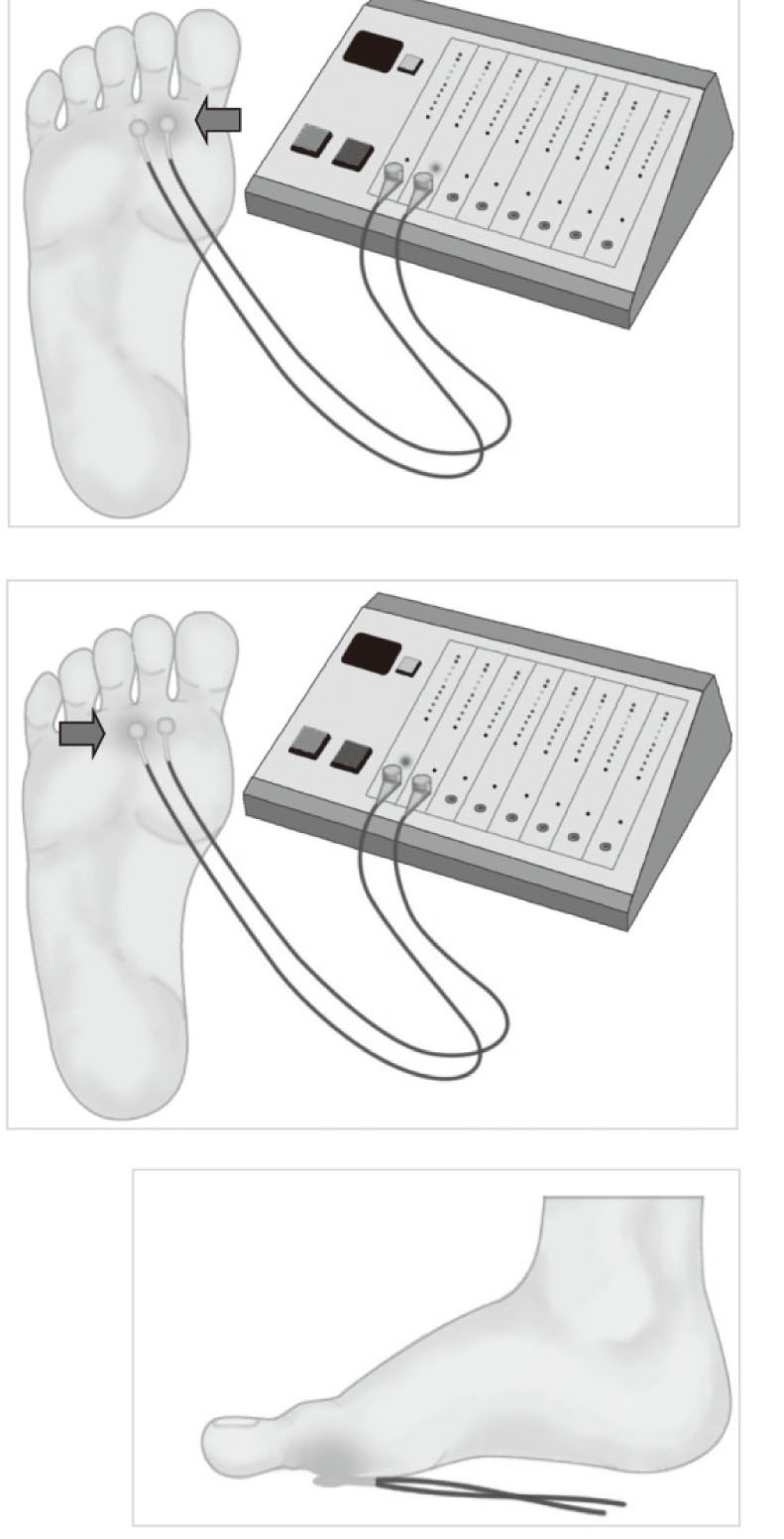
Pinpoint planter long-wavelength infrared light irradiation
Point A: Halfway between the heads of the 1st and 2nd metatarsals (also used as a placibo in a double-blind method).
Point B: Halfway between the lower part of the 2nd and 3rd metatarsals.
Materials and methods
This study enrolled 15 subjects (8 males, 7 females; average age 47.8 ± 14.6 years). After a 15-min period of rest in a supine position, parts of the plantar region were irradiated for 15 min (wavelength: 8–11 μm; output: 30 mW using irradiation probe (size: 5mm diameter; material: fused quartz). Two parts of the plantar region were irradiated: point A was located halfway between the heads of the 1st and 2nd metatarsals, while point B was located halfway between the lower part of the 2nd and 3rd metatarsals (Figure 1). In the preliminary study, maximal stress-relief effects were observed when laser was irradiated at the point A. Therefore, we have investigated more detail of such effects in this study. Point B was used as the negative control of point A (point B separates a metatarsal and is located next to point A). To eliminate both experimenter bias and placebo (belief) effect, a double blind procedure was used.
To analyze the stress markers, 3 cm3 of blood was collected from the antecubital vein and centrifuged for 5 min at 1200G. From the plasma obtained, amylase was quantified using α-glucosidase and 4, 6-ethylidine α-D-maltoheptaside-ρ-nitrophenyl (Et-G7-PNP), cortisol using a chemiluminescence immunoassay (CLIA), and ACTH using an electrochemiluminescence immunoassay (ECLIA). Salivary amylase was similarly measured using α-glucosidase and Et-G7-PNP an enzyme analysis device to assess optical density (AMY manufactured by Nipro). In order to take into account the impact of circadian rhythms and other factors, all conditions were made uniform, including the time of day when measurements were made and blood samples were collected.
Measurement of subcutaneous temperature (core body temperature)
Core body temperature is usually measured orally or rectally, but Fox et al. developed a deep body thermometer that allows the simple and accurate measurement of body temperature without any effect from the ambient temperature through the attachment of a temperature sensor to the body surface. 5–7) The theory behind this deep body thermometer involves what is known as heat-flux compensation. The method involves electrical detection of heat dissipation from a part of the body surface and the continuous recording of heat dissipation. In this research, a deep body thermometer (Coretemp CM-210, Terumo, Tokyo, Japan) was used to measure and analyze the palmar subcutaneous temperature at 3 mm and 5 mm.
Allocation and statistical processing
Allocation was performed by an operator not acquainted with the study subjects and a third-party coordinator who was not involved in the measurements. After stratifying the subjects according to gender, the subjects were divided into the point A irradiation group (n=10) and the point B irradiation group (n=10), as well as a non-irradiated placebo group (n=5). Same patients were treated with both of point A and B irradiation. ANOVA was performed and a multiple comparison made using Student's t-test and Tukey-Scheffé tests, with a significance level of P<0.05. This study was approved by Ryotokuji University's Institutional Review Board (approval no. 2304). All subjects provided a written informed consent to their participation in the research.
Results
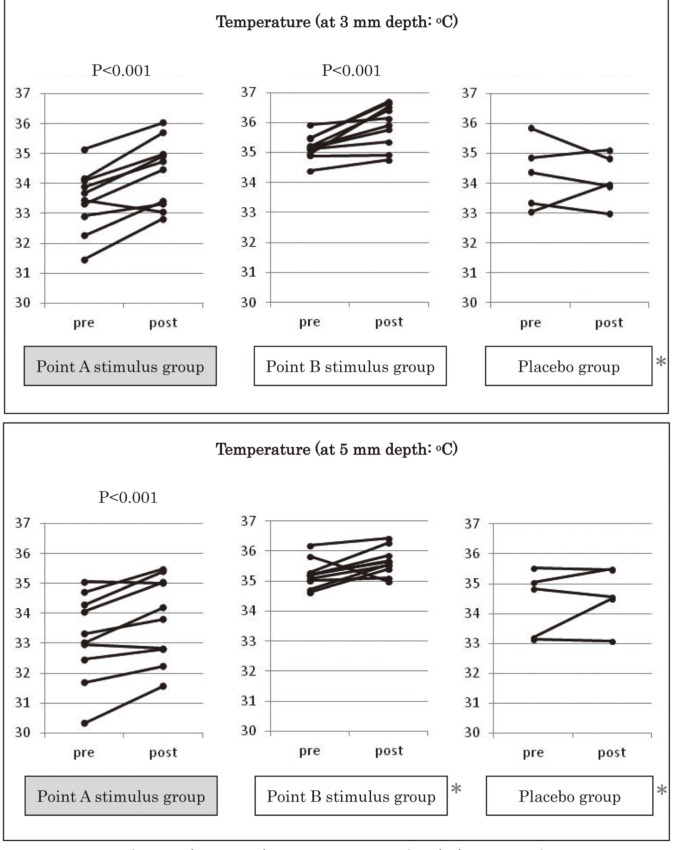
Changes in subcutaneous temperature (core body temperature) and blood pressure
After PP-LILI, in the point A stimulus group (n=10) the palmar subcutaneous temperature at 3 mm was significantly higher (P<0.001) after irradiation (34.3±1.1°C) than before irradiation (33.4±1.0°C). The palmar subcutaneous temperature at 5 mm was also significantly higher (P<0.001) after irradiation (33.8±1.4°C) than before irradiation (33.1±1.5°C) (Figure 2). The results showed a marked increase in the core body temperature at both 3 mm and 5 mm in the point A stimulus group at a significance level of ≥0.001%. In the point B stimulus group (n=10), the palmar subcutaneous temperature at 3 mm was significantly higher (P<0.001) after irradiation (35.9±0.7°C) than before irradiation (35.1±0.4°C), and the palmar subcutaneous temperature at 5 mm was also higher after irradiation (35.6±0.5°C) than before irradiation (35.2±0.5°C) although no statistically significant difference was observed (Figure 2). In the point A placebo group (n=5), the palmar subcutaneous temperature at 3 mm was slightly higher after treatment (34.1±0.8°C) than before treatment (34.2±1.1°C), and the palmar subcutaneous temperature at 5 mm was higher after irradiation (34.6±1.0°C) than before irradiation (34.3±1.1°C). But in either case, no statistically significant differences were observed (Figure 2). An intergroup comparison between the three groups confirmed a statistically significant increase (P<0.05) in core body temperature in the point A stimulus group (Figure 2).
Figure 2:
Changes in subcutaneous temperature (core body temperature) *P< 0.005 is intergroup comparison with the point A stimulus group.
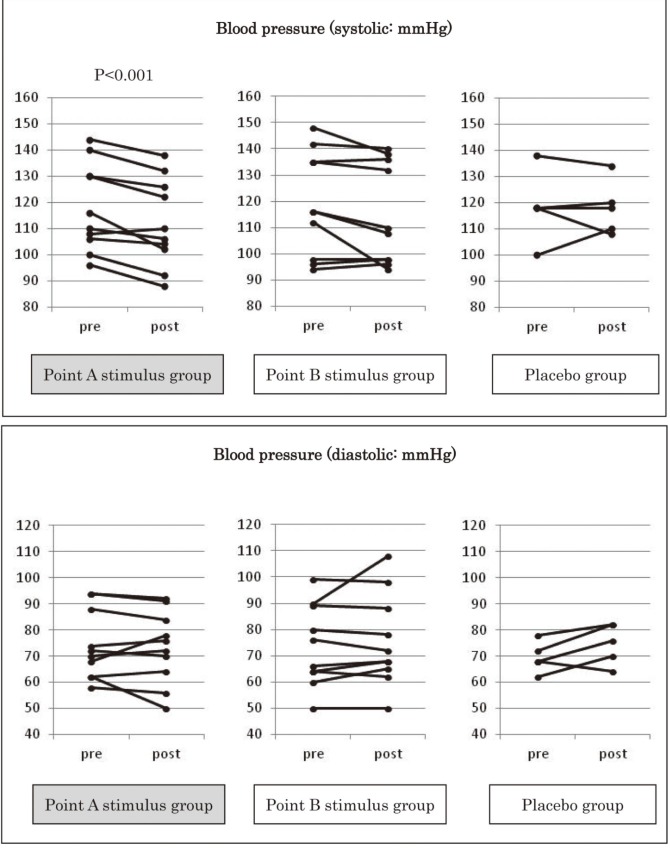
Measurement of the comparative change in blood pressure (systolic, diastolic) before and after PP-LILI (Figure 3) showed that in the point A stimulus group, systolic blood pressure fell significantly (P<0.001) after irradiation (112.0±16.8 mmHg) compared to before irradiation (118.0±16.9 mmHg), and diastolic blood pressure fell non-significantly after irradiation (73.3±13.9 mmHg) compared to before irradiation (74.2±13.3 mmHg). In the point B stimulus group, systolic blood pressure non-significantly fell after irradiation (115.0±19.3mmHg) compared to before irradiation (119.2±19.8 mmHg), and diastolic blood pressure nonsignificantly rose after irradiation (75.7±17.6 mmHg) compared to before irradiation (73.8±15.6 mmHg). In the point A placebo group, systolic blood pressure was unchanged after irradiation (118.0±10.3 mmHg) compared to before irradiation (118.4±13.4 mmHg), and diastolic blood pressure rose non-significantly after irradiation (74.8±7.8 mmHg) compared to before irradiation (69.6±5.9 mmHg). A comparison between the groups showed no statistically significant difference.
Figure 3:
Changes in blood pressure
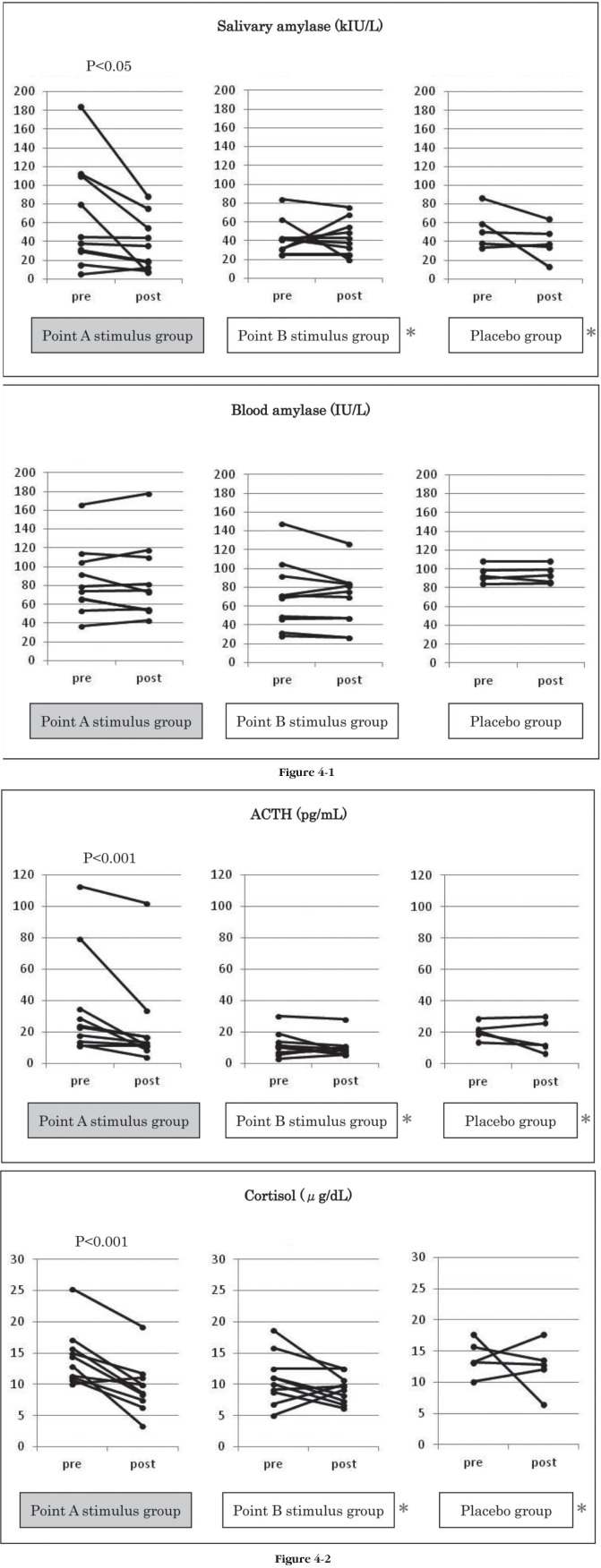
Changes in stress hormones
Irradiation at point A produced a marked reduction in the secretion amounts of the stress indicators salivary amylase and blood amylase, cortisol, and ACTH (Figure 4). Salivary amylase fell from 64.8±56.0 kIU/L before irradiation to 36.0±28.7 kIU/L after irradiation in the point A stimulus group (P<0.05), increased slightly from 42.7±18.2 kIU/L before irradiation to 43.3±18.7 kIU/L after irradiation in the point B stimulus group, and fell from 53.2±21.0 kIU/L before irradiation to 39.2±18.8 kIU/L after irradiation in the point A placebo group. Intergroup comparison confirmed a significant reduction in the point A stimulus group (P<0.05).
Figure 4:
Changes in stress hormones
*P< 0.005 is intergroup comparison with the point A stimulus group.
Blood amylase fell from 85.1±36.7 IU/L before irradiation to 84.1±41.2 IU/L after irradiation in the point A stimulus group, fell from 71.1±36.5 IU/L before irradiation to 66.9±30.4 IU/L after irradiation in the point B stimulus group, and was unchanged at 94.4±9.1 IU/L before irradiation and 94.2±9.6 IU/L after irradiation in the point A placebo group. Intergroup comparison confirmed no significant differences.
Blood ACTH fell significantly (P<0.001) from 35.7±33.7 pg/mL before irradiation to 23.0±28.9 pg/mL after irradiation in the point A stimulus group, fell nonsignificantly from 12.3±7.6 pg/mL before irradiation to 9.69±6.8 pg/mL after irradiation in the point B stimulus group, and fell non-significantly from 21.0±5.5 pg/mL before irradiation to 14.8±10.0 pg/mL after irradiation in the point A placebo group. Intergroup comparison confirmed a significant reduction in ACTH in the point A stimulus group (P<0.05). Blood cortisol fell significantly (P<0.001) from 14.3±4.5 μg/dL before treatment to 9.6±4.2 μg/dL after irradiation in the point A stimulus group. There was a slight fall from 10.9±4.1 μg/dL before irradiation to 9.3±2.2 μg/dL after irradiation in the B group, but the difference was not significant. There was also a slight fall from 13.9±2.9 μg/dL before irradiation to 12.5±4.6 μg/dL after irradiation in the point A placebo group but the difference was not significant. Intergroup comparison confirmed a significant reduction in cortisol in the point A stimulus group (P<0.05).
Discussion
Changes in subcutaneous temperature (core body temperature) and blood pressure
Under normal conditions, body temperature does not differ much between individuals and is maintained at a uniform level. However, with many diseases, including autonomic symptoms caused by stress, body temperature is low due to a reduction in peripheral blood circulation.
Body temperature measurements can be easily affected by the ambient temperature, so the measurement of core body temperature—that is not influenced by the ambient temperature—is the recommended method for temperature monitoring (for example, axillary, oral, or rectal temperature). 8–10) In this research, we used a deep body thermometer (Coretemp CM-210, manufactured by Terumo). The results showed a significant increase in core body temperature as indicated by the palmar subcutaneous temperature at 3 mm and 5 mm. We speculate that this indicates a similar underlying action to that reported in previous studies on moxibustion on the toes of mice: i.e. a promotion of blood vessel permeability, an increased peripheral blood flow, and a reduced sympathetic nerve activity. 11–13)
For the blood pressure, a systematic review of LASER and moxibustion treatment for hypertension has not confirmed its efficacy 14), but the combustion temperature of moxa is over 50°C; therefore it could stimulate the sympathetic nerves. However, we suggest that PP-LILI used in this research does not stimulate the sympathetic nerves and may improve peripheral circulation to normalize blood pressure.
The part of the plantar region selected for irradiation does not include the organ system reflex points or the acupuncture points used in oriental medicine. Anatomically, the point A, which produced a superior therapeutic effect, has a connective tissue containing fat at the depression between the medial plantar protuberance protuberance (ball of the big toe) and the more lateral plantar protuberance (ball of the smaller toes). During a normal movement such as walking, the direct force is not easily transmitted to this region and the applied force tends to be dispersed easily, so that irradiation targeted at this site could produce a positive effect on peripheral circulation. There is no clear evidence supporting the use of foot reflexology in EBM—the only results 15) confirm improved systemic blood flow and promoted lymph duct flow—and there have been few reports 16) to date on the effects of applying a LASER irradiation to one point in the plantar region.
Changes in stress hormones
Psychological stress stimulates sympathetic nerves via the limbic system and causes vasoconstriction and reduced microcirculation in the body. At the same time, the hypothalamus (paraventricular nucleus) is stimulated to secrete CRH, which results in the secretion of ACTH by the anterior pituitary gland and the glucocorticoid cortisol by the adrenal cortex. 17) These hormones have therefore been used as important indicators for stressful experience. 1,4,18) Irradiation at point A increased the peripheral subcutaneous temperature at 3 mm and 5 mm and suppressed the secretion of stress hormones (amylase, cortisol, ACTH). These results may be due to the suppressing effect of the irradiation of plantar point A on excessive response of hypothalamic-pituitary-stimulating hormones and the stimulation of the sympathetic nerves caused by stress on the body.
Asking & Gjörstrup showed that the activity of the stress marker salivary amylase is controlled by noradrenaline from the adrenal system mediated by the sympathetic nerves. 19) Research by van Stegeren et al. showed a significant decrease in amylase secretion in the saliva when a β-adrenergic receptor blocker (propranolol) was administered under stressful conditions. 20) Takai et al. reported that salivary amylase secretion increased significantly when the subjects were presented with the images of corneal transplant surgery but fell with the images of beautiful scenery. 21) Yamaguchi et al. demonstrated that salivary amylase secretion increased when the subjects walked in an urban environment, but fell when they walked in a forest environment. 22)
To summarize, we suggest the “PP-LILI” used in this research increased peripheral blood flow by suppressing stress hormones including salivary amylase and by curbing the sympathetic nervous tension caused by stress.
Other reports have shown that full-body heating in a sauna can be helpful in improving the symptoms of chronic fatigue, severe heart failure, or arteriosclerosis obliterans through the activation of bioprotective mechanisms such as the autonomic nervous system and immunostimulation. 23–26) However, PP-LILI that we devised did not involve the full-body heating via the pinpoint irradiation, where there are no side effects such as dehydration, hot flashes, or dizziness, but nevertheless this procedure gradually improved blood flow dynamics across the entire body. Our study suggests this treatment may gradually increase subcutaneous temperature as a result of a moderate reduction in peripheral vascular resistance through the suppression of both sympathetic nerve activity and adrenocortical hormone secretion.
We expect this treatment method to play a significant role in the prevention of myocardial infarction or arteriosclerosis caused by temporary ischemia and reperfusion because of sympathetic nerve stimuli. 17, 18) Furthermore, our preliminary observation suggests that irradiation at point A in the individuals with hypertension and diabetes reduced their blood pressure and resulted in a marked reduction in HbA1c, blood sugar levels, and the total cholesterol. At the gene level, we also observed that the activity of the JAK-STAT pathway that responds to the stimuli from interferon and other cytokines was increased. We now plan to confirm the effectiveness of this treatment through largerscale clinical studies.
Conclusions
This study showed that PP-LILI resulted in elevated subcutaneous temperature, reduced blood pressure and suppressed secretion of stress hormones such as amylase, cortisol and ACTH.
These differences between pre- and post-irradiation were statistically significant.
The results therefore suggest that PP-LILI is a potential approach to counteract the reduction in peripheral circulation and to suppress the overreaction of hypothalamic-pituitary-stimulating hormones that are involved with excessive sympathetic nerve stimulation under stress.
[Acknowledgements]
This research was conducted jointly by the medical education Ryotokuji College, Faculty of Health Sciences Ryotokuji University, and Medical Corporation Ryotokuji Group. We thank all the individuals involved in this study. Stress hormone quantification was performed in collaboration with Showa Medical Science.
References
- 1: Jacobsen TN. (1996). Sympathetic reflex regulation of the peripheral circulation in humans, Dan Med Bull 43:126-140 [PubMed] [Google Scholar]
- 2: Bonyhay I, Freeman R. (2004). Sympathetic nerve activity in response to hypotensive stress in the postural tachycardia syndrome. Circulation 110:3193-3198 [DOI] [PubMed] [Google Scholar]
- 3: Mori T, Ogawa S, Cowely AW, Jr, Ito S. (2011). Role of Renal Medullary Oxidative/ Carbonyl stress in Salt-Sensitive Hypertension and Diabetes. Clin Exp Pharmacol Physiol 39:125-131 [DOI] [PubMed] [Google Scholar]
- 4: Ebstrup JF, Jørgensen T. (2012). Stress and cardiovascular disease. Ugeskr Laeger 174:204-207 [PubMed] [Google Scholar]
- 5: Fox RH, Solman AJ. (1971). A new technique for monitoring the deep body temperature in man from the intact skin surface. J Physiol 212:8-10 [PubMed] [Google Scholar]
- 6: Fox RH, Solman AJ, Isaacs R, Fry AJ, MacDonald LC. (1973). A new method for monitoring deep body temperature from the skin surface. Clin Sci 44:81-86 [DOI] [PubMed] [Google Scholar]
- 7: Kitamura K, Zhu X, Chen W, Nemoto T. (2010). Development of a new method for the noninvasive measurement of deep body temperature without a heater. Med Eng Phys 32:1-6 [DOI] [PubMed] [Google Scholar]
- 8: Cooper KE, Kenyon JR. (1957). A comparison of temperatures measured in the rectum, oesophagus, and on the surface of the aorta during hypothermia in man. Br J Surg 44:616-619 [DOI] [PubMed] [Google Scholar]
- 9: Smitz S, Giagoultsis T, Dewé W, Albert A. (2000). Comparison of rectal and infrared ear temperatures in older hospital inpatient. J Am Geriatr Soc 48:63-66 [DOI] [PubMed] [Google Scholar]
- 10: Huang M, Chen W. (2010). Theoretical simulation of the dual-heat-flux method in deep body temperature measurements. Conf Proc IEEE Eng Med Biol Soc: 561-564 [DOI] [PubMed]
- 11: Okazaki M, Aizawa S, Yamauchi M, Oguchi K. (1990). Effects of single moxibustion on cutaneous blood vessel and microvascular permeability in mice. Am J Chin Med 18:121-130 [DOI] [PubMed] [Google Scholar]
- 12: Okazaki M, Sakamoto H, Suzuki M, Oguchi K. (1990). Effects of single and multiple moxibustions on activity of platelet function, blood coagulation and fibrinolysis in mice. Am J Chin Med 18:77-85 [DOI] [PubMed] [Google Scholar]
- 13: Shen X, Ding G, Wei J, Zhao L, Zhou Y, Deng H, Lao L. (2006). An infrared radiation study of the biophysical characteristics of traditional moxibustion. Complement Ther Med 14:213-219 [DOI] [PubMed] [Google Scholar]
- 14: Kim JI, Choi JY, Lee H, Lee MS, Ernst E. (2010). Moxibustion for hypertension: a systematic review. BMC Cardiovasc Disord 10:33-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15: Lu WA, Chen GY, Kuo CD. (2011). Foot reflexology can increase vagal modulation, decrease sympathetic modulation, and lower blood pressure in healthy subjects and patients with coronary artery disease. Altern Ther Health Med 17:8-14 [PubMed] [Google Scholar]
- 16: Schaffer M, Bonel H, Sroka R, Schaffer PM, Busch M, Reiser M, Duhmeke E. (2000). Effect of 780 nm diode laser irradiation on blood microcirculation: preliminary finding on time-dependent T1-weighted contrast-enhanced magnetic resonance imaging (MRI). J Photochem Photobiol B 54:55-60 [DOI] [PubMed] [Google Scholar]
- 17: Wiersma A, Konsman JP, Knollema S, Bohus B, Koolhaas JM. (1998). Differential effects of CRH infusion into the central nucleus of the amygdala in the Roman high-avoidance and low-avoidance rats. Psychoneuroendocrinology 23:261-274 [DOI] [PubMed] [Google Scholar]
- 18: Wiersma A, Bohus B, Koolhaas JM. (1993). Corticotropin-releasing hormone microinfusion in the central amygdala diminishes a cardiac parasympathetic outflow under stress-free conditions. Brain Res 625:219-227 [DOI] [PubMed] [Google Scholar]
- 19: Asking B, Gjörstrup P. (1987). Synthesis and secretion of amylase in the rat parotid gland following autonomic nerve stimulation in vivo. Acta Physiol Scand 130:439-445 [DOI] [PubMed] [Google Scholar]
- 20: van Stegeren A, Rohleder N, Everaerd W, Wolf OT. (2006). Salivary alpha amylase as marker for adrenergic activity during stress: effect of betablockade. Psychoneuroendo- crinology 31:137-141 [DOI] [PubMed] [Google Scholar]
- 21: Takai N, Yamaguchi M, Aragaki T, Eto K, Uchihashi K, Nishikawa Y. (2004). Effect of psychological stress on the salivary cortisol and amylase levels in healthy young adults. Arch Oral Biol 49:963-968 [DOI] [PubMed] [Google Scholar]
- 22: Yamaguchi M, Deguchi M, Miyazaki Y. (2006). The effects of exercise in forest and urban environments on sympathetic nervous activity of normal young adults. J Int Med Res 34:152-159 [DOI] [PubMed] [Google Scholar]
- 23: Tei C, Horikiri Y, Park JC, Jeong JW, Chang KS, Toyama Y, Tanaka N. (1995). Acute hemodynamic improvement by thermal vasodilation in congestive heart failure. Circulation 91:2582-2590 [DOI] [PubMed] [Google Scholar]
- 24: Kihara T, Biro S, Imamura M, Yoshifuku S, Takasaki K, Ikeda Y, Otuji Y, Minagoe S, Toyama Y, Tei C. (2002). Repeated sauna treatment improves vascular endothelial and cardiac function in patients with chronic heart failure. J Am Coll Cardiol 39:754-759 [DOI] [PubMed] [Google Scholar]
- 25: Masuda A, Kihara T, Fukudome T, Shinsato T, Minagoe S, Tei C. (2005). Repeated thermal therapy for two patients with chronic fatigue syndrome. J Psychosom Res 58:383-387 [DOI] [PubMed] [Google Scholar]
- 26: Masuda A, Nakazato M, Kihara T, Minagoe S, Tei C. (2005). Repeated thermal therapy diminishes appetite loss and subjective complaints in mildly depressed patients. Psychosom Med 67,643-647 [DOI] [PubMed] [Google Scholar]