Abstract
Objective
To describe the management and impact of pancreatic fistulas in a high-volume center.
Design
Retrospective case series.
Setting
Tertiary academic center.
Patients
Five hundred eighty-one consecutive patients who underwent pancreaticoduodenectomy from January 2001 through June 2006.
Main Outcome Measures
Development of a pancreatic fistula (defined as > 30 mL of amylase-rich fluid from drains on or after postoperative day 7, or discharge with surgical drains in place, regardless of amount); the need for additional interventions or total parenteral nutrition; other morbidity; and mortality.
Results
Seventy-five patients (12.9%) developed a pancreatic fistula. Fistulas were managed with gradual withdrawal of surgical drains. This allowed for patient discharge and eventual closure at a mean of 18 days in 38.7% of cases; these were classified as low-impact fistulas. The remaining 46 patients (61.3%) had an associated abscess, required percutaneous drainage or total parenteral nutrition, or developed bleeding; these were classified as high-impact fistulas and closed a mean of 35 days after surgery. Standard 30-day in-hospital mortality was 1.9% for all pancreaticoduodenectomies and 6.7% for those who developed a pancreatic fistula. The overall fistula- related mortality was 9.3% (7 patients), all but 1 of which was related to major hemorrhage.
Conclusions
More than one-third of pancreatic fistulas are clinically insignificant (low impact). The remaining 60% of fistulas have a high clinical impact and nearly an 8-fold increase in overall mortality.
Pancreatic fistulas are the hallmark of complications following pancreaticoduodenectomy, and numerous articles have addressed this problem, particularly their prevention. Because there was no attempt until recently to reach a consensus regarding what constitutes a pancreatic fistula,1 multiple definitions abound, and thus it has been difficult to analyze accurately the true clinical impact of this problem. To compound the lack of a consistent definition, there is a paucity of information regarding the best management strategies for this complication. 1–3 While it is clear that a proportion of pancreatic fistulas have no, or very little, clinical impact, many still cause major morbidity and mortality.3–6 These clinically significant fistulas span a wide spectrum of severity, from a delay in hospital discharge and implementation of parenteral nutrition to an abscess or bleeding pseudoaneurysm. Included in this group are those patients who had an occult fistula. These are patients who initially appear to have no fistula based on drain output or amylase level but who present within weeks to months after surgery with intraabdominal collections, sepsis, and/or life-threatening hemorrhages. Some of these patients do not survive and, given the delay in presentation of their fistula, are sometimes not reported as having a pancreatic fistula and are not included in reported operative mortality statements. The objective of this study was to review our contemporary experience with pancreatic fistulas following pancreaticoduodenectomy, outline their management, and analyze their clinical impact.
METHODS
A retrospective review of all patients undergoing pancreaticoduodenectomy at the Massachusetts General Hospital between January 2001 and June 2006 was performed. During this interval, all pancreaticoduodenectomies were prospectively entered into a database. Patients who developed a pancreatic fistula were identified and their characteristics were compared with those who did not develop a fistula. Hospital and office records of patients with a pancreatic fistula were reviewed in detail to analyze their clinical course and management.
A patient was considered to have a pancreatic fistula if she or he had 30 mL or more of amylase-rich fluid (3 × greater than a normal serum value) from surgically placed drains on or after postoperative day 7 or if she or he was sent home with a surgical drain in place with amylase-rich fluid regardless of the amount. In addition, patients who underwent interventional radiology–guided or surgical drainage of fluid collections that were amylase rich or located in the vicinity of the pancreatic anastomosis were also considered to have a pancreatic fistula.
From the medical record review of those patients who developed a pancreatic fistula, we obtained the following information: demographics, preoperative diagnosis, final pathology, type of anastomosis, length of operation, length of hospital stay, need for readmission, need for interventional radiology, need for antibiotics, use of total parenteral nutrition, use of somatostatin, daily drain outputs, drain amylase levels, duration of fistula, bleeding, need for reoperation, other major complications, and mortality. The duration of the fistula was defined as the time between the day of surgery and the day the last drain was removed (either the surgically placed Jackson-Pratt drain or the interventional radiology–guided catheter). Operative mortality was defined as any death within 30 days of surgery or during the same hospitalization as the pancreaticoduodenectomy. Overall fistula-related mortality was defined as any death directly resulting as a consequence of the fistula, regardless of postoperative day.
Pancreatic fistulas were categorized based on their clinical course as either low or high impact. Low-impact fistulas were those with no additional morbidity or need for further intervention. Most of these fistulas were treated in the outpatient setting and did not require further hospitalization. Highimpact fistulas were those that required interventional radiology– guided drainage, total parenteral nutrition, reoperation, prolonged hospitalization, or readmission. Also, any fistula that resulted in an abscess, delayed gastric emptying, bleeding, or death was considered high impact. Statistical analysis was performed using a 2-sided Wilcoxon rank sum test for nonparametric variables and a Fisher exact test for categorical data.
RESULTS
Five-hundred eighty-one patients underwent pancreaticoduodenectomy during the course of the study. Most of these patients had a 2-layer, end-to-side pancreaticojejunostomy with stenting of the anastomosis using a pediatric feeding tube (82%) or without stenting (16%). In cases in which the pancreatic duct could not be visualized or was not considered suitable to hold sutures (2%), an invaginating or telescoped end-to-end anastomosis was performed.
A total of 75 patients developed a pancreatic fistula (12.9%). The fistula rate was higher in the 14 patients with the end-to-end invaginating anastomosis (50%) compared with the 567 patients who had an end-to-side pancreaticojejunostomy (11.9%) (P <.001).
MANAGEMENT OF PANCREATIC FISTULAS
Postoperatively, nasogastric tubes were removed within 24 to 48 hours and patients were advanced to a clear-liquid diet in the following 2 days and then to 6 small low-fat meals per day as tolerated. Changes in the amount and character of the drain fluid were noted as diets advanced. Fluid amylase levels were measured on postoperative day 4 or 5 once the patient was eating. Drains were discontinued if the fluid amylase was low or the output was minimal (usually < 10 mL/d). Pancreatic fistulas were managed with gradual withdrawal (2 cm every several days) of surgically placed drains in any patient who was clinically stable and tolerating a diet. In general, drain withdrawal (advancement) was initiated after postoperative days 5 to 7 and continued at outpatient visits until output was less than 10 mL per day. For high-output fistulas (> 150–200 mL of amylase-rich fluid per day), patients were made nil per os, placed on total parenteral nutrition, and treated with octreotide. If fistula output decreased substantially with these measures and the patient remained clinically well, drain withdrawal was initiated and oral intake was slowly restarted. If fistula output did not decrease with these measures, drains were initially left in place to control the fistula. If the patient remained well despite high output, drains were slowly advanced in an attempt to decrease the output and close the fistula. Any patient who developed fever, abdominal pain, or an inability to tolerate oral intake did not have the drains withdrawn and underwent an abdominal computed tomographic scan. If any drainable collections were identified, the patient underwent interventional radiology– guided drainage and was started on broad-spectrum antibiotics. Interventional radiology drains were kept in place and flushed daily. Once the output declined to less than 10 mL per day, the drains were sequentially withdrawn and discontinued.
Gastrointestinal bleedingwasmanagedinitially with upper endoscopy and/or angiography. If a bleeding pseudoaneurysm was identified on angiography, attempts at coil embolization were made. Patients with persistent or life-threatening hemorrhages underwent surgical exploration.
COMPARISON OF PATIENTS WITH AND WITHOUT A PANCREATIC FISTULA
The characteristics of the 75 patients who developed a pancreatic fistula and the 506 who did not are presented in Table 1. Male patients and those with ampullary adenocarcinoma were significantly more likely to develop a pancreatic fistula than those with pancreatic adenocarcinoma (27.3% and 4.9%, respectively, P < .001). Not unexpectedly, patients who developed a pancreatic fistula had a significantly greater length of hospital stay, need for stay in an intensive care unit, use of parenteral nutrition, need for readmission, and delayed gastric emptying. The mortality was 7.7 times greater in patients with a pancreatic fistula (9.3% vs 1.2%, P=.001).
Table 1.
Comparison of Patients Who Developed a Pancreatic Fistula With Those Who Did Not
| No. (%) | |||||
|---|---|---|---|---|---|
| Characteristic | Patient With Fistula (n = 75) |
Patient Without Fistula (n = 506) |
All Patients (N = 581) |
Odds Ratio |
P Value |
| Age, mean (SD), y | 63 (13.8) | 63 (13.2) | 63 (13.3) | .92 | |
| Male sex | 48 (64.0) | 245 (48.4) | 293 (50.4) | 1.9 | .01 |
| Pathologic diagnosis | |||||
| Cystic lesion | 19 (15.6) | 103 (84.4) | 122 (21.0) | 1.3 | .36 |
| Ampullary adenocarcinoma | 18 (27.3) | 48 (72.7) | 66 (11.4) | 3.0 | < .001 |
| Pancreatic adenocarcinoma | 9 (4.9) | 174 (95.1) | 183 (31.5) | 0.26 | < .001 |
| Chronic pancreatitis | 6 (12.2) | 43 (87.8) | 49 (8.4) | 0.94 | > .99 |
| Neuroendocrine tumor | 4 (12.1) | 29 (87.9) | 33 (5.7) | 0.93 | > .99 |
| Other | 19 (14.8) | 109 (85.2) | 128 (22.0) | 1.2 | .46 |
| Preoperative albumin level, mean (SD), g/dL | 3.7 (0.64) | 3.7 (0.57) | 3.7 (0.58) | .83 | |
| Length of operation, mean (SD), min | 377.1 (119.1) | 342.1 (96.1) | 346.6 (99.9) | .02 | |
| Length of hospital stay, mean (SD), d | 23.6 (20.1) | 8.7 (5.9) | 10.6 (10.3) | < .001 | |
| Need for stay in intensive care unit | 20 (26.7) | 17 (3.4) | 37 (6.4) | < .001 | |
| Need for TPN | 31 (41.3) | 14 (2.8) | 45 (7.8) | < .001 | |
| Need for readmission | 20 (26.7) | 56 (11.1) | 76 (13.1) | < .001 | |
| Delayed gastric emptying | 7 (9.3) | 16 (3.2) | 23 (4.0) | .02 | |
| Need for IR drainage | 28 (37.3) | 24 (4.7) | 52 (9.0) | < .001 | |
| Reoperation | 5 (6.7) | 11 (2.2) | 16 (2.8) | .04 | |
| Mortality | |||||
| 30-Day or in-hospital | 5 (6.7) | 6 (1.2) | 11 (1.9) | .008 | |
| Fistula-related | 7 (9.3) | 6 (1.2) | 13 (2.2) | < .001 | |
Abbreviations: IR, interventional radiology; TPN, total parenteral nutrition.
SI conversion factor: To convert albumin to grams per liter, multiply by 10.
PATIENTS WITH LOW-AND HIGH-IMPACT FISTULAS
Pancreatic fistulas were classified according to their clinical impact as described, and their characteristics are listed in Table 2. More than one-third (38.7%) were low-impact fistulas that required no additional intervention and were mostly treated in the outpatient setting (nearly 80% of patients were sent home with drains). Four of these patients received octreotide early in their postoperative course because of high output. Three of them had a substantial decrease in output within 3 days of initiation, while the fourth had a less pronounced response and received outpatient octreotide therapy. These fistulas had a mean output of 114 mL (median, 75 [interquartile range, 30–159] mL) on postoperative day 7 or just before the patient’s discharge from the hospital, and they closed a mean of 18 days after surgery.
Table 2.
Low- vs High-Impact Fistulas in Patients Who Underwent Pancreaticoduodenectomy
| No. (%) | |||
|---|---|---|---|
| Characteristic | Low-Impact Fistula (n = 29) |
High-Impact Fistula (n = 46) |
P Value |
| Age, mean (SD), y | 62 (11.1) | 63 (15.4) | .47 |
| Length of stay, mean (SD), d | 10.3 (5.5) | 32 (21.4) | <.001 |
| Length of operation, mean (SD), min | 353.0 (92.0) | 392.3 (132.1) | .21 |
| Discharged with drain | 23 (79.3) | 23 (50.0) | .02 |
| JP drain output on postoperative day 7, mean (SD), mL | 114.1 (116.0) | 229.4 (223.2) | .01 |
| Use of antibiotics | 8 (27.6) | 39 (84.8) | <.001 |
| Use of octreotide | 4 (13.8) | 32 (69.6) | <.001 |
| Use of TPN | 1 (3.5) | 30 (65.2) | <.001 |
| Duration of fistula, mean (SD), d | 17.8 (6.3) | 35.4 (17.5) | <.001 |
| Associated abscess or collection | NA | 36 (78.3) | <.001 |
| Need for IR drainage | NA | 28 (60.9) | <.001 |
| Delayed gastric emptying | NA | 7 (15.2) | .04 |
| Need for reoperation | NA | 5 (10.9) | .15 |
| Bleeding | NA | 9 (19.6) | .01 |
| Mortality | |||
| 30-Day or in-hospital | NA | 5 (10.9) | .15 |
| Fistula-related | NA | 7 (15.2) | .04 |
Abbreviations: IR, interventional radiology; JP, Jackson-Pratt; NA, not applicable (by definition, low-impact fistulas do not result in these complications); TPN, total parenteral nutrition.
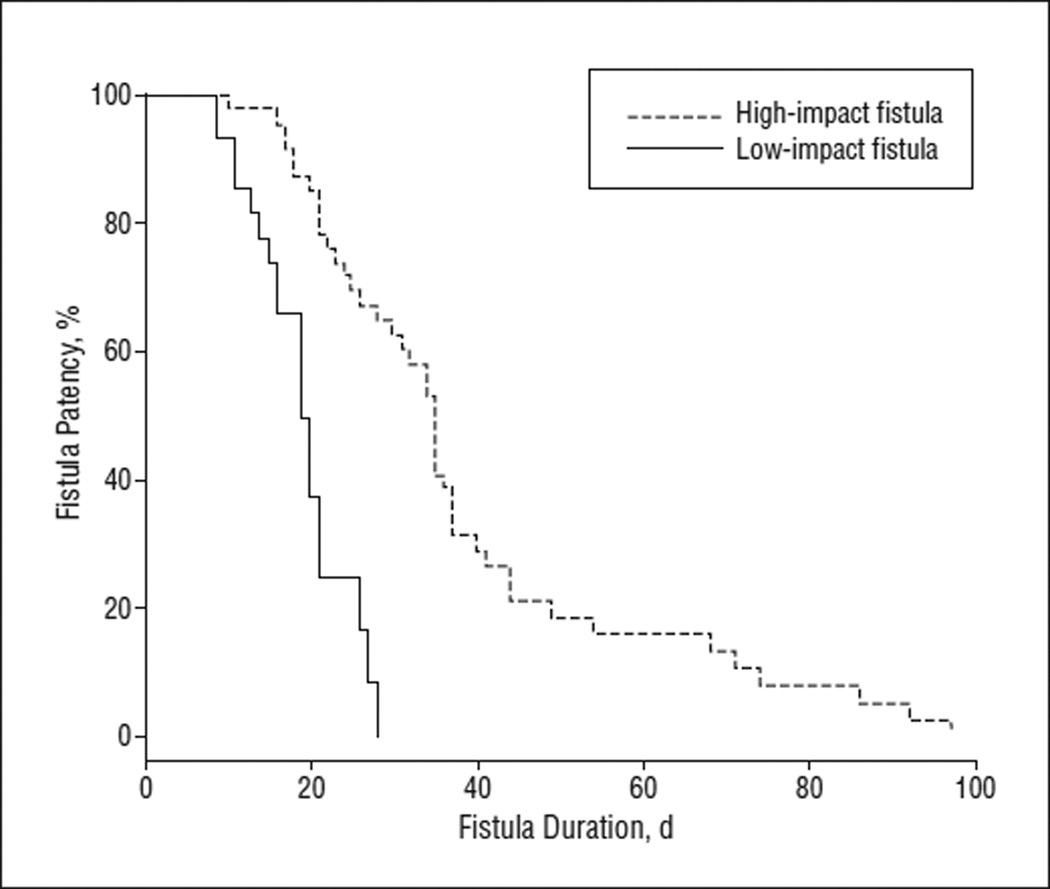
The remaining 46 patients (61.3%) had a high-impact fistula. These patients had longer hospital stays and frequently were treated with antibiotics, octreotide, and total parenteral nutrition. These fistulas had a mean output of 229 mL on postoperative day 7 (median, 165 [interquartile range, 60–320] mL), and they closed a mean of 35 days after surgery (P < .001) (Figure). More than three-fourths of patients with high-impact fistulas developed an associated abscess or collection, and more than half required interventional radiology–guided drainage (61%). There were 9 patients (12% of all fistulas and 20% of the high-impact fistulas) who had major hemorrhages.
Figure.
Duration of low-impact vs high-impact fistulas in patients who underwent pancreaticoduodenectomy (P < .001).
OCCULT PANCREATIC FISTULAS
High-impact fistulas were further divided into overt and occult. Overt high-impact fistulas were those that were evident within the first postoperative week and resulted in major morbidity and/or mortality. Occult fistulas were those that initially were not manifest (ie, drain outputs did not meet the criteria to qualify as a pancreatic fistula and were therefore removed) but subsequently resulted in an associated abscess, collection, major hemorrhage, or death that was felt to be related to a pancreatic leak that had not been identified. There were 33 overt high-impact fistulas and 13 occult fistulas in our series. Comparison of these 2 groups showed significantly more readmissions in those with an occult fistula, but there were no differences in the need for intervention, associated abscess, reoperation, bleeding, or mortality (Table 3).
Table 3.
Overt vs Occult High-Impact Fistulas in Patients Who Underwent Pancreaticoduodenectomy
| No. (%) | |||
|---|---|---|---|
| Characteristic | Overt Fistula (n = 33) |
Occult Fistula (n = 13) |
P Value |
| Length of stay, mean (SD) d | 32.2 (19.0) | 31.7 (27.4) | .37 |
| Length of operation, mean (SD), min | 413.5 (135.1) | 338.5 (111.4) | .11 |
| Discharged with drain | 18 (54.5) | 5 (38.5) | .51 |
| JP drain output on postoperative day 7, mean (SD), mL | 229.4 (223.2) | NA | |
| Use of antibiotics | 27 (81.8) | 12 (92.3) | .65 |
| Use of octreotide | 27 (81.8) | 5 (38.5) | .01 |
| Use of TPN | 23 (69.7) | 7 (53.9) | .33 |
| Duration of fistula, mean (SD), d | 37.3 (19.9) | 30.5 (7.6) | .23 |
| Associated abscess or collection | 24 (72.7) | 12 (92.3) | .24 |
| Need for IR drainage | 17 (51.5) | 11 (84.6) | .05 |
| Need for readmission | 10 (30.3) | 10 (76.9) | .007 |
| Need for reoperation | 4 (12.1) | 1 (7.7) | >.99 |
| Need for stay in intensive care unit | 13 (39.4) | 6 (46.2) | .75 |
| Bleeding | 7 (21.2) | 2 (15.4) | >.99 |
| Mortality | |||
| 30-Day or in-hospital | 4 (12.1) | 1 (7.7) | >.99 |
| Fistula-related | 5 (15.2) | 2 (15.4) | >.99 |
Abbreviations: IR, interventional radiology; JP, Jackson-Pratt; NA, not applicable (by definition); TPN, total parenteral nutrition.
MORTALITY RELATED TO FISTULAS
There were 7 deaths in patients who developed a pancreatic fistula (overall fistula-related mortality of 9.3%). Only 2 deaths occurred within 30 days of surgery, and 4 occurred during the initial hospitalization (30-day, in-hospital mortality of 6.7%). The other 2 patients died at later times or hospital admissions, but their deaths were related to their fistula. Bleeding was associated with all but 1 death, and the 3 reoperations performed were all related to bleeding (Table 4).
Table 4.
Fistula-Related Mortality in Patients Who Underwent Pancreaticoduodenectomy
| Postoperative Day of Death |
Cause of Death |
Death During Initial Admission |
Reoperation | Reason for Reoperation |
|---|---|---|---|---|
| 10 | Bleeding | Yes | Yes | Bleeding GDA pseudoaneurysm |
| 86 | Bleeding and sepsis | Yes | No | NA |
| 37 | Aspiration pneumonia | Yes | No | NA |
| 35 | Bleeding | Yes | Yes | Infected hematoma after hemorrhage |
| 36 | Bleeding | No | No | NA |
| 17 | Bleeding and sepsis | No | No | NA |
| 92 | Bleeding and sepsis | No | Yes | Bleeding GDA pseudoaneurysm |
Abbreviations: GDA, gastroduodenal artery; NA, not applicable.
COMMENT
Analysis of this contemporary cohort of pancreaticoduodenectomies shows that pancreatic fistulas continue to be a problem in the 21st century. Using a definition that has been in place at our institution since 1990,7,8 which is similar to one used by others,2,9 we found a pancreatic fistula rate of 12.9%. This rate is comparable with those from other large pancreatic centers.2,3,9–11 Our original intent was to apply the definition and classification recently proposed by the International Study Group on Pancreatic Fistula (ISGPF) to our cohort1 but found this was not feasible in a retrospective fashion. On the one hand, the ISGPF defines a pancreatic fistula as the presence of any measurable, amylase-rich (3 × the normal serum value) fluid output on or after postoperative day 3. Applying this definition mandates that drain amylase levels be checked on postoperative day 3 and on a daily basis thereafter until the drain is removed. Since this has never been our routine, we lack these measurements; therefore, by this criterion, we would be underestimating the fistula rate, though the added fistulas would all probably be benign. One potential pitfall of applying a very sensitive definition (such as that proposed by the ISGPF) is the overdiagnosis of pancreatic fistulas, which leads to an underestimation of the true clinical impact.
Despite the relatively low pancreatic fistula rate of 12.9%, we found that morbidity associated with this event is substantially high (and higher than we anticipated). Overall, patients with a pancreatic fistula had 3 times as many reoperations, an 8-fold increase in the need for stay in an intensive care unit and interventional radiology procedures, a marked increase in the length of stay (23.6 vs 8.7 days), and nearly a 27% readmission rate. These consequences of pancreatic fistulas following pancreaticoduodenectomy have been well described in other studies. 3,5,6,12,13 In addition, we found increased mortality, which has not been uniformly found to be affected by pancreatic fistulas. Some studies have shown no difference whatsoever,2,12,13 while others have described substantial increases.3–5,14 In the present study, 9.3% of patients with a pancreatic fistula died, nearly an 8-fold increase relative to the patients without a fistula (1.2%). This very significant and marked difference is in part related to inclusion of patients who died beyond the traditional 30-day or same-hospitalization mark (the mortality in the fistula group would have only been 2.7% if we had used the 30-day definition, or 6.7% if we had used the 30-day or same-hospitalization definition). It is noteworthy that the studies that have found no difference in the mortality of patients with and without a pancreatic fistula have all used 30-day mortality for their comparisons. 2,12,13 Based on this critical review of pancreatic fistulas, we feel the mortality rate of 9.3% is very accurate and highlights the clinical importance of this complication following pancreaticoduodenectomy.
Mortality from a pancreatic fistula is frequently the result of a major hemorrhage. Death in patients with a pancreatic fistula occurred at a median of 36 days (range, 10–92 days). There were 9 patients (12%) who had major hemorrhages from their fistula, with a mortality of 66.7%. The median postoperative day of bleeding was 22 (range, day 9–41), and there were 2 patients in whom the source of bleeding was not definitively identified (both died). The remaining 7 patients all had bleeding pseudoaneurysms (4 from the gastroduodenal artery and 3 from the hepatic artery). Five of these patients underwent angiographic embolization and 2 required emergent laparotomy. In those patientswhounderwent angiographic intervention, 2 (40%) survived and 3 (60%) ultimately died after an initially successful coil embolization.
We have recently performed a detailed analysis of the clinical and economic impact of pancreatic leaks after distal pancreatectomy.15 In a cohort of 259 patients, we found that the risk of pancreatic fistulas or fistula-related complications (such as an abscess in the vicinity of the pancreatic stump) is almost 3 times higher after a distal pancreatectomy than after pancreaticoduodenectomy. However, despite the marked increase in readmissions, hospital stay, and need for interventional radiology procedures in patients with pancreatic leaks after distal pancreatectomy, there were no added mortality in these patients or bleeding events related to the fistula.16 It is unclear if this difference is due to the absence of an enteric component in the leak or to other factors.
Our study also shows that not all pancreatic fistulas have the same clinical impact. This difference was also recognized in the ISGPF schema, which proposed classifying fistulas in 3 grades of severity (A, B, and C).1 We attempted to apply this grading system and found it relatively simple to identify the patients with grade A pancreatic fistulas (those without clinical impact) but very difficult to separate the rest of the patients into groups B and C (both of which have a high impact). Part of the difficulty lies in the subjectivity of some of the terms within the ISGPF proposal and part lies in the apparent lack of inclusion of what we term occult fistulas (those in which surgical drains were removed because there were no apparent fistulas but manifested weeks later as an abscess or collection in the vicinity of the pancreatic anastomosis, in some cases with potentially lethal hemorrhage). Given the clear differences, we emphasize the importance of the distinction between low- and high-impact fistulas (grade A vs grades B and C, respectively) when reporting or analyzing outcomes after pancreaticoduodenectomy as opposed to simply listing a pancreatic fistula rate. This distinction should correct for the variation in the reports of the frequency of fistulas (which differ depending on how inclusive or restrictive the used definition may have been), since the total number of clinically significant fistulas should be identified similarly.
Our study did not focus on the risk factors for development of pancreatic fistulas or their prevention. Several studies have addressed this issue.9,17–22 However, we did find a marked difference in the fistula rate in relation to diagnosis and a higher incidence in men and in patients undergoing end-to-end anastomosis compared with our preferred technique of stented end-to-side, mucosa- to-mucosa pancreaticojejunostomy. Other studies have identified these risk factors as well.13,23,24 Other authors have described the consistency of the pancreas and the duct diameter as equally significant; but we were not able to confirm this because we did not invariably detail this information in the operative reports.
Our general management strategy is as follows: Once a patient meets the defined criteria for a pancreatic fistula, the clinical status is assessed. If the patient has abdominal pain, fever, leukocytosis, an inability to tolerate an oral diet, nausea, or vomiting after postoperative day 5, a computed tomographic scan is obtained. If there are any drainable collections, these are managed with interventional radiology–guided drainage. If the patient is clinically well, the fistula output is low (< 100–150 mL/ d), and the patient is tolerating at least a liquid diet, the surgical drains are advanced (withdrawn) 2 cm. If the drain output falls to less than 10 mL/d and the patient remains well, drains are removed regardless of the amylase level in the fluid. If the drain output is between 20 and 150 mL/d after the first advancement, the patient is discharged with the drain in place. A follow-up appointment is made within 5 to 7 days and the drain is advanced again or removed if the daily output is less than 10 mL. If the output is high (> 150 mL/d), the patient is made nil per os, given parenteral nutrition, and treated with octreotide. As the fistula output decreases, the drain is withdrawn sequentially and an oral diet is restarted slowly. Once the drain output falls to less than 10 mL/d, the drain is removed. If the patient’s condition deteriorates, a computed tomographic scan is obtained and drains are not advanced. If the fistula output does not slow with bowel rest and octreotide, the drains are left in place; however, if the clinical condition does not deteriorate, the drain is advanced slowly after 5 to 7 days. In general, most patients can be discharged with drains if they are eating and otherwise clinically well. Clearly, close follow-up is required and daily outputs need to be monitored by a visiting nurse. Occasionally drain output will increase significantly with the initial drain advancement. In this situation, the drain should remain in position to control the output and be managed as described.
Our management strategy of slow drain withdrawal was successful in 95% of overt fistulas (3 failures in 62 fistulas). In those with failed management, drain advancement was initiated when daily outputs were greater than 100 mL, and all subsequently required interventional radiology–guided drainage of an abscess or collection. Among these 3 failures, there were no deaths or need for reoperation. In the 18 patients who had a recognized fistula (ie, not occult) that needed interventional radiology drainage, embolization, or reoperation, the additional intervention was done while the drain was still in place, suggesting that the surgical drain was poorly located or otherwise inadequate to control the fistula.
In summary, this large contemporary series of pancreaticoduodenectomy shows that postoperative pancreatic fistulas occur in 12.9% of patients. About one-third of these patients experience no, or very little, impact from the fistula, which closes at a mean of 18 days with gradual drain advancement. The remaining 60% have complications from pancreatic fistulas with a high clinical impact. These patients have twice as much drain output on postoperative day 7 and require significantly more interventional radiology procedures, total parenteral nutrition, and stays in an intensive care unit and consequently have an increased length of hospital stay and more secondary readmissions. More importantly, this study shows that the mortality associated with pancreatic fistulas is 9.3% and that most of these deaths are related to bleeding and occur beyond the traditional 30-day mark. This observation highlights the need for more accurate reporting of postoperative pancreatic fistulas and their stratification by severity. Until we can diminish or prevent pancreatic anastomotic leaks, heightened attention to high-impact fistulas and perhaps earlier intervention, such as immediate angiographic evaluation of any bleeding from the surgical site, is warranted.
Footnotes
Author Contributions: Study concept and design: Veillette and Fernández-del Castillo. Acquisition of data: Veillette, Dominguez, McGrath, and Fernández-del Castillo. Analysis and interpretation of data: Veillette, Ferrone, Thayer, Warshaw, and Fernández-del Castillo. Drafting of the manuscript: Veillette, Dominguez, McGrath, and Fernández-del Castillo. Critical revision of the manuscript for important intellectual content: Ferrone, Thayer, Warshaw, and Fernández-del Castillo. Administrative, technical, and material support: Veillette, Dominguez, Ferrone, Thayer, Warshaw, and Fernández-del Castillo. Study supervision: Warshaw and Fernández-del Castillo.
Financial Disclosure: None reported.
Previous Presentation: This paper was presented at the 88th Annual Meeting of the New England Surgical Society; September 30, 2007; Burlington, Vermont; and is published after peer review and revision.
REFERENCES
- 1.Bassi C, Dervenis C, Butturini G, et al. Post-operative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138(1):8–13. doi: 10.1016/j.surg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Kazanjian KK, Hines OJ, Eibl G, Reber HA. Management of pancreatic fistulas after pancreaticoduodenectomy: results in 437 consecutive patients. Arch Surg. 2005;140(9):849–855. doi: 10.1001/archsurg.140.9.849. [DOI] [PubMed] [Google Scholar]
- 3.Aranha GV, Aaron JM, Shoup M, Pickleman J. Current management of pancreatic fistula after pancreaticoduodenectomy. Surgery. 2006;140(4):561–569. doi: 10.1016/j.surg.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 4.Choi SH, Moon HJ, Heo JS, Joh JW, Kim YI. Delayed hemorrhage after pancreaticoduodenectomy. J Am Coll Surg. 2004;199(2):186–191. doi: 10.1016/j.jamcollsurg.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Muscari F, Suc B, Kirzin S, et al. French Associations for Surgical Research. Risk factors for mortality and intra-abdominal complications after pancreaticoduodenectomy: multivariate analysis in 300 patients. Surgery. 2006;139(5):591–598. doi: 10.1016/j.surg.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 6.Munoz-Bongrand N, Sauvanet A, Denys A, Sibert A, Vilgrain V, Belghiti J. Conservative management of pancreatic fistula after pancreaticoduodenectomy with pancreaticogastrostomy. J Am Coll Surg. 2004;199(2):198–203. doi: 10.1016/j.jamcollsurg.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Fernández-del Castillo C, Rattner DW, Warshaw L. Standards for pancreatic resection in the 1990s. Arch Surg. 1995;130(3):295–300. doi: 10.1001/archsurg.1995.01430030065013. [DOI] [PubMed] [Google Scholar]
- 8.Balcom JH, Rattner DW, Warshaw AL, Chang Y, Fernández-del Castillo C. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001;136(4):391–398. doi: 10.1001/archsurg.136.4.391. [DOI] [PubMed] [Google Scholar]
- 9.Yeo CJ, Cameron JL, Maher MM, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995;222(4):580–588. doi: 10.1097/00000658-199510000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yeo CJ, Cameron JL, Sohn TA, et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg. 1997;226(3):248–257. doi: 10.1097/00000658-199709000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aranha GV, Aaron JM, Shoup M. Critical analysis of pancreaticogastrostomy after pancreaticoduodenectomy. Arch Surg. 2006;141(6):574–580. doi: 10.1001/archsurg.141.6.574. [DOI] [PubMed] [Google Scholar]
- 12.Pratt WB, Maithel SK, Vanounou T, Huang ZS, Callery MP, Vollmer CM. Clinical and economic validation of the International Study Group of Pancreatic Fistula (ISGPF) classification scheme. Ann Surg. 2007;245(3):443–451. doi: 10.1097/01.sla.0000251708.70219.d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin JW, Cameron JL, Yeo CJ, Riall TS, Lillemoe KD. Risk factors and outcomes in postpancreaticoduodenectomy pancreaticocutaneous fistula. J Gastrointest Surg. 2004;8(8):951–959. doi: 10.1016/j.gassur.2004.09.044. [DOI] [PubMed] [Google Scholar]
- 14.Winter JM, Cameron JL, Campbell KA, et al. Does pancreatic duct stenting decrease the rate of pancreatic fistula following pancreaticoduodenectomy? results of a prospective randomized trial. J Gastrointest Surg. 2006;10(9):1280–1290. doi: 10.1016/j.gassur.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 15.Rodrĺguez JR, Germes SS, Pandharipande PV, et al. Implications and cost of pancreatic leak following distal pancreatic resection. Arch Surg. 2006;141(4):361–366. doi: 10.1001/archsurg.141.4.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodrĺguez JR, Madanat MG, Healy BC, et al. Distal pancreatectomy with splenic preservation revisited. Surgery. 2007;141(5):619–625. doi: 10.1016/j.surg.2006.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarr MG Pancreatic Surgery Group. The potent somatostatin analogue vapreotide does not decrease pancreas-specific complications after elective pancreatectomy: a prospective, multicenter, double-blinded, randomized, placebo-controlled trial. J Am Coll Surg. 2003;196(4):556–565. doi: 10.1016/S1072-7515(03)00104-2. [DOI] [PubMed] [Google Scholar]
- 18.Ramos-De la Medina A, Sarr MG. Somatostatin analogues in the prevention of pancreas-related complications after pancreatic resection. J Hepatobiliary Pancreat Surg. 2006;13(3):190–193. doi: 10.1007/s00534-005-1033-9. [DOI] [PubMed] [Google Scholar]
- 19.Yeo CJ, Cameron JL, Lillemoe KD, et al. Does prophylactic octreotide decrease the rates of pancreatic fistula and other complications after pancreaticoduodenectomy? results of a prospective randomized placebo-controlled trial. Ann Surg. 2000;232(3):419–429. doi: 10.1097/00000658-200009000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lowy AM, Lee JE, Pisters PW, et al. Prospective, randomized trial of octreotide to prevent pancreatic fistula after pancreaticoduodenectomy for malignant disease. Ann Surg. 1997;226(5):632–641. doi: 10.1097/00000658-199711000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barnett SP, Hodul PJ, Creech S, Pickleman J, Aranha GV. Octreotide does not prevent postoperative pancreatic fistula or mortality following pancreaticoduodenectomy. Am Surg. 2004;70(3):222–227. [PubMed] [Google Scholar]
- 22.Lillemoe KD, Cameron JL, Kim MP, et al. Does fibrin glue sealant decrease the rate of pancreatic fistula after pancreaticoduodenectomy? a prospective trial. J Gastrointest Surg. 2004;8(7):766–774. doi: 10.1016/j.gassur.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 23.Shrikhande SV, Qureshi SS, Rajneesh N, Shukla PJ. Pancreatic anastomoses after pancreaticoduodenectomy: do we need further studies? World J Surg. 2005;29(12):1642–1649. doi: 10.1007/s00268-005-0137-3. [DOI] [PubMed] [Google Scholar]
- 24.Bartoli FG, Arnone GB, Ravera G, et al. Pancreatic fistula and relative mortality in malignant disease after pancreaticoduodenectomy: review and statistical meta-analysis regarding 15 years of literature. Anticancer Res. 1991;11(5):1831–1848. [PubMed] [Google Scholar]