Abstract
Background
This evidence-based analysis reviews relational and management continuity of care. Relational continuity refers to the duration and quality of the relationship between the care provider and the patient. Management continuity ensures that patients receive coherent, complementary, and timely care. There are 4 components of continuity of care: duration, density, dispersion, and sequence.
Objective
The objective of this evidence-based analysis was to determine if continuity of care is associated with decreased health resource utilization, improved patient outcomes, and patient satisfaction.
Data Sources
MEDLINE, EMBASE, CINAHL, the Cochrane Library, and the Centre for Reviews and Dissemination database were searched for studies on continuity of care and chronic disease published from January 2002 until December 2011.
Review Methods
Systematic reviews, randomized controlled trials, and observational studies were eligible if they assessed continuity of care in adults and reported health resource utilization, patient outcomes, or patient satisfaction.
Results
Eight systematic reviews and 13 observational studies were identified. The reviews concluded that there is an association between continuity of care and outcomes; however, the literature base is weak. The observational studies found that higher continuity of care was frequently associated with fewer hospitalizations and emergency department visits. Three systematic reviews reported that higher continuity of care is associated with improved patient satisfaction, especially among patients with chronic conditions.
Limitations
Most of the studies were retrospective cross-sectional studies of large administrative databases. The databases do not capture information on trust and confidence in the provider, which is a critical component of relational continuity of care. The definitions for the selection of patients from the databases varied across studies.
Conclusions
There is low quality evidence that:
Higher continuity of care is associated with decreased health service utilization.
There is insufficient evidence on the relationship of continuity of care with disease-specific outcomes.
There is an association between high continuity of care and patient satisfaction, particularly among patients with chronic diseases.
Plain Language Summary
There are 3 broad categories of continuity of care: informational, management and relational. Relational continuity is the main focus of this review. Relational continuity refers to the ongoing relationship between the care provider and the patient. This review identified several observational studies that assessed continuity of care through the use of validated indices. All of the studies identified demonstrated that higher continuity was associated with either reduced hospitalization rates or reduced emergency department visits. The limitations of this review are that the primary data source was from retrospective studies of administrative data and that all of the studies were focused on physician continuity with a patient—no studies were identified which assessed continuity with other providers such as nurses, social workers or other allied health professionals.
Background
In July 2011, the Evidence Development and Standards (EDS) branch of Health Quality Ontario (HQO) began developing an evidentiary framework for avoidable hospitalizations. The focus was on adults with at least 1 of the following high-burden chronic conditions: chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), atrial fibrillation, heart failure, stroke, diabetes, and chronic wounds. This project emerged from a request by the Ministry of Health and Long-Term Care for an evidentiary platform on strategies to reduce avoidable hospitalizations.
After an initial review of research on chronic disease management and hospitalization rates, consultation with experts, and presentation to the Ontario Health Technology Advisory Committee (OHTAC), the review was refocused on optimizing chronic disease management in the outpatient (community) setting to reflect the reality that much of chronic disease management occurs in the community. Inadequate or ineffective care in the outpatient setting is an important factor in adverse outcomes (including hospitalizations) for these populations. While this did not substantially alter the scope or topics for the review, it did focus the reviews on outpatient care. HQO identified the following topics for analysis: discharge planning, in-home care, continuity of care, advanced access scheduling, screening for depression/anxiety, self-management support interventions, specialized nursing practice, and electronic tools for health information exchange. Evidence-based analyses were prepared for each of these topics. In addition, this synthesis incorporates previous EDS work, including Aging in the Community (2008) and a review of recent (within the previous 5 years) EDS health technology assessments, to identify technologies that can improve chronic disease management.
HQO partnered with the Programs for Assessment of Technology in Health (PATH) Research Institute and the Toronto Health Economics and Technology Assessment (THETA) Collaborative to evaluate the cost-effectiveness of the selected interventions in Ontario populations with at least 1 of the identified chronic conditions. The economic models used administrative data to identify disease cohorts, incorporate the effect of each intervention, and estimate costs and savings where costing data were available and estimates of effect were significant. For more information on the economic analysis, please contact either Murray Krahn at murray.krahn@theta.utoronto.ca or Ron Goeree at goereer@mcmaster.ca.
HQO also partnered with the Centre for Health Economics and Policy Analysis (CHEPA) to conduct a series of reviews of the qualitative literature on “patient centredness” and “vulnerability” as these concepts relate to the included chronic conditions and interventions under review. For more information on the qualitative reviews, please contact Mita Giacomini at giacomin@mcmaster.ca.
The Optimizing Chronic Disease Management in the Outpatient (Community) Setting mega-analysis series is made up of the following reports, which can be publicly accessed at http://www.hqontario.ca/evidence/publications-and-ohtac-recommendations/ohtas-reports-and-ohtac-recommendations.
Optimizing Chronic Disease Management in the Outpatient (Community) Setting: An Evidentiary Framework
Discharge Planning in Chronic Conditions: An Evidence-Based Analysis
In-Home Care for Optimizing Chronic Disease Management in the Community: An Evidence-Based Analysis
Continuity of Care: An Evidence-Based Analysis
Advanced (Open) Access Scheduling for Patients With Chronic Diseases: An Evidence-Based Analysis
Screening and Management of Depression for Adults With Chronic Diseases: An Evidence-Based Analysis
Self-Management Support Interventions for Persons With Chronic Diseases: An Evidence-Based Analysis
Specialized Nursing Practice for Chronic Disease Management in the Primary Care Setting: An Evidence-Based Analysis
Electronic Tools for Health Information Exchange: An Evidence-Based Analysis
Health Technologies for the Improvement of Chronic Disease Management: A Review of the Medical Advisory Secretariat Evidence-Based Analyses Between 2006 and 2011
Optimizing Chronic Disease Management Mega-Analysis: Economic Evaluation
How Diet Modification Challenges Are Magnified in Vulnerable or Marginalized People With Diabetes and Heart Disease: A Systematic Review and Qualitative Meta-Synthesis
Chronic Disease Patients’ Experiences With Accessing Health Care in Rural and Remote Areas: A Systematic Review and Qualitative Meta-Synthesis
Patient Experiences of Depression and Anxiety With Chronic Disease: A Systematic Review and Qualitative Meta-Synthesis
Experiences of Patient-Centredness With Specialized Community-Based Care: A Systematic Review and Qualitative Meta-Synthesis
Objective of Analysis
The objective of this analysis was to determine if continuity of care is associated with health resource utilization and patient outcomes. This evidence-based analysis on continuity of care is a part of the larger mega-analysis on Optimizing Chronic Disease Management.
Technology/Technique
There are 3 defined areas of continuity of care: informational, management, and relational or interpersonal. (1) This evidence-based analysis will address management1 and relational continuity, but not informational continuity:
Informational continuity is continuity where previous patient information is available (usually through a patient chart or an electronic medical record) and used to provide patient-appropriate care. Ideally the patient information is available to multiple health care professionals in different settings.
Management continuity involves the use of standards and protocols to ensure that care is provided in an orderly, coherent, complementary, and timely fashion. Often this applies to when care is being provided my multiple providers. This also includes accessibility (availability of appointments, medical tests), flexibility to adapt to care needs, and consistency of care and transitions of care (e.g., the coordination of home care by a family physician).
Relational continuity (interpersonal) refers to the ongoing relationship between the care provider and the patient. It refers to the duration of the relationship as well as the quality of the relationship, which is affected by the attentiveness, inspiration of confidence, and the medical knowledge of the health professional.
Several indices have been developed to assess the 4 primary components of relational continuity of care: (2)
duration—length of time with a particular provider
density—number of visits with the same provider over a defined time period
dispersion—number of visits with distinct providers
sequence—order in which different providers are seen
Commonly used indices are listed in Table 1.
Table 1: Measures of Continuity of Care.
| Name of Index | Description | Score Range | Index Measures | Strengths | Weaknesses | |||
| Durationa | Densityb | Dispersionc | Sequenced | |||||
| Usual Provider of Continuity (UPC) index | The number of visits to a usual provider in a given period over the total number of visits to similar providers | 0 to 1 | Yes | Yes | No | No | Since a ‘usual provider’ is defined, it may be useful in analyzing the role of other health providers in addition to physicians | Only assesses visits with usual provider, other providers not included in the index Not independent of utilization levels Measure decreases as number of visits increases |
| Continuity of Care (COC) index | Measures both the dispersion and concentration of care among all providers seen | 0 to 1 | Yes | Yes | Yes | No | Sensitive to shifts in the distribution of visits among providers Good mathematical performance; tends to have a mean of 0.5 and a large coefficient of variation |
May mask important differences in sequencing of care Mot independent of utilization levels Measure decreases as number of visits increases Measure falls rapidly with increasing number of providers seen |
| Modified Continuity Index (MCI) | Measure of concentration of care in population of patients calculated by dividing the average number of visits by a group by the average number of providers in the a population | 0 to 1 | Yes | Yes | Yes | No | Requires summary utilization measures only (compared with COC which requires more utilization data) | Extremes of continuity not reflected in measure (i.e., 2 visits to same provider yields an intermediate result rather than perfect continuity) |
| Modified Modified Continuity Index (MMCI) | Measure of concentration of care with providers at the individual patient level Developed to account for problems of COC and MCI indices |
0 to 1 | Yes | Yes | Yes | No | Requires summary utilization measures only (compared with COC which requires more utilization data) Not overly sensitive to large number of providers |
No sequential data captured |
| Sequential Continuity (SECON) index | Fraction of sequential visit pairs where the same provider is seen | 0 to 1 | Yes | Yes | No | Yes | Sensitive to shifts in sequence of visits Potentially useful as measure of amount of inter-provider communication necessary because of transfers of care |
Insensitive to the distribution of visits among providers if sequencing remains constant |
Duration refers to the length of time with a particular provider.
Density refers to the number of visits with the same provider over a defined time period.
Dispersion refers to the number of visits with distinct providers.
Sequence refers to the order in which different providers are seen.
Source: Reid et al, 2002. (3)
The Usual Provider of Care (UPC) index is primarily aimed at addressing the density of care, while the Continuity of Care Index (COC) addresses density, but really focuses on the dispersion of care. In other words, the COC index measures the number of different providers seen; the more providers that are seen, the lower the continuity index. The Modified COC and Modified Modified COC indices were designed to improve the COC index; however, these indices are not reported as widely in the literature as the original COC index. The Sequential Continuity (SECON) Index is designed to assess the sequence of visits. In an ideal continuity of care scenario, a patient would be seen consecutively by one provider (provider A) for one episode of care, and then seen by another provider (provider B) consecutively for another episode of care. Thus, the sequence would be AAABBB, rather than ABABAB, which would result in a low SECON index.
Evidence-Based Analysis
Research Question
Is higher continuity of care effective at reducing health resource utilization and improving patient outcomes?
Research Methods
Literature Search
Search Strategy
A literature search was performed on December 8, 2011 (then updated January 27, 2012) using OVID MEDLINE, OVID MEDLINE In-Process and Other Non-Indexed Citations, OVID EMBASE, EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL), the Wiley Cochrane Library, and the Centre for Reviews and Dissemination database, for studies published from January 1, 2002, until December 8, 2011 (updated January 27, 2012). A 10-year timeframe was chosen because there was a comprehensive systematic review by Cabana and Jee published in 2004 that included studies up until 2002. (4) Abstracts were reviewed by a single reviewer and, for those studies meeting the eligibility criteria, full-text articles were obtained. Reference lists were also examined for any additional relevant studies not identified through the search. The full search strategy is listed in Appendix 1.
Inclusion Criteria
English language full-reports
published between January 1, 2002, and January 27, 2012
randomized controlled trials, systematic reviews, meta-analyses, prospective observational, and retrospective studies
studies with adult patients
studies investigating provider level or clinic level continuity
studies investigating interpersonal (relational) continuity or management continuity2
studies with patients with diabetes, heart failure, chronic obstructive pulmonary disease (COPD), atrial fibrillation, stroke, coronary artery disease, chronic wounds or studies with patients with multiple chronic conditions
studies reporting at least 1 outcome of interest
Exclusion Criteria
studies of informational continuity
studies with physicians in training, residents, fellows
studies of patients in hospital, mental health facilities, or long-term care facilities
studies of transitions of patients to or from inpatient setting
studies including only a pediatric population
studies focusing on prevention or screening for disease
case series, case reports, editorials
non-English studies
Outcomes of Interest
health resource utilization (hospitalizations, emergency department visits [ED])3
mortality
disease-specific outcomes
quality of life
patient satisfaction
Quality of Evidence
The quality of the body of evidence for each outcome is examined according to the GRADE Working Group criteria. (5) The overall quality is determined to be very low, low, moderate, or high using a step-wise, structural methodology.
Study design is the first consideration; the starting assumption is that randomized controlled trials are high quality, whereas, observational studies are low quality. Five additional factors—risk of bias, inconsistency, indirectness, imprecision, and publication bias—are then taken into account. Limitations or serious limitations in these areas result in downgrading the quality of evidence. Finally, 3 main factors are considered which may raise the quality of evidence: large magnitude of effect, dose response gradient, and accounting for all residual confounding. (5) For more detailed information, please refer to the latest series of GRADE articles. (5)
As stated by the GRADE Working Group, the final quality score can be interpreted using the following definitions:
| High | Very confident that the true effect lies close to the estimate of the effect |
| Moderate | Moderately confident in the effect estimate—the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different |
| Low | Confidence in the effect estimate is limited—the true effect may be substantially different from the estimate of the effect |
| Very Low | Very little confidence in the effect estimate—the true effect is likely to be substantially different from the estimate of effect |
Results of Evidence-Based Analysis
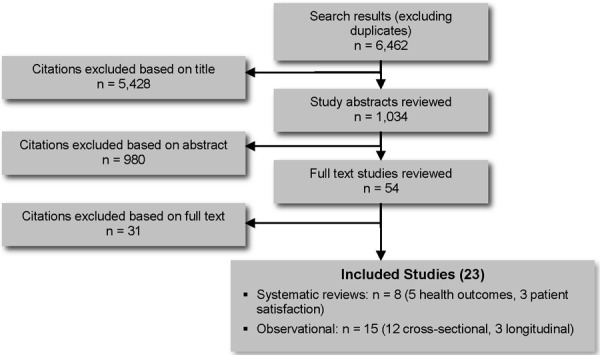
The database search yielded 6,462 citations published between January 1, 2002, and December 8, 2011 (with duplicates removed). Articles were excluded based on information in the title and abstract. The full texts of potentially relevant articles were obtained for further assessment. Figure 1 shows the breakdown of when and for what reason citations were excluded in the analysis. Twenty-three studies (8 systematic reviews and 15 observational studies) met the inclusion criteria.
Figure 1: Citation Flow Chart.
The results of the evidence-based analysis were stratified under the following subheadings:
systematic reviews assessing the effectiveness of continuity of care (5 studies)
studies of continuity of care in patients with any condition (5 studies)
studies of continuity of care in patients with diabetes (10 studies [3 studies of the same trial])
studies of continuity of care in patients with COPD (1 study)
studies of continuity of care in patients with coronary artery disease (1 study)
systematic reviews assessing patient satisfaction associated with continuity of care (3 studies)
For each included study, the study design was identified and is summarized below in Table 2, which is a modified version of a hierarchy of study design by Goodman. (6)
Table 2: Body of Evidence Examined According to Study Design.
| Study Design | Number of Eligible Studies |
| RCT Studies | |
| Systematic review of RCTs | |
| Large RCT | |
| Small RCT | |
| Observational Studies | |
| Systematic review of non-RCTs with contemporaneous controls | |
| Non-RCT with non-contemporaneous controls | |
| Systematic review of non-RCTs with historical controls | 8 |
| Non-RCT with historical controls | |
| Database, registry, or cross-sectional study | 15 |
| Case series | |
| Retrospective review, modelling | |
| Studies presented at an international conference | |
| Expert opinion | |
| Total | 23 |
Abbreviation: RCT, randomized controlled trial.
Systematic Reviews Assessing the Effectiveness of Continuity of Care
Five systematic reviews were identified that assessed the effectiveness of continuity of care on health system utilization and patient outcomes (Table 3). None of the reviews specifically focused on patients with chronic conditions. With the exception of the review by Worrall and Knight, (7) the reviews included studies with any patient population. The Worrall and Knight systematic review included studies of adults 50 years or older. (7)
Table 3: Summary of Systematic Reviews on Continuity of Care.
| Study | Research Question | Sources & Years Searched | Inclusion Criteria | Number of Studies Included | Conclusion |
| van Walraven et al, 2010 (8) | Is there an association between continuity of care and outcomes? | MEDLINE (1950–2008) | Studies measuring continuity and outcomes Accounted for relative timing of continuity and outcomes |
18 | “Increased provider continuity is associated with improved patient outcomes and satisfaction” |
| Jee & Cabana, 2006 (2) | What are the indices of continuity of care? | MEDLINE, PSYCH INFO (1966–2002) | Studies with a defined measure of continuity | 44 | There is variability in the continuity indices |
| van Servellen et al, 2006 (9) | To what extent are informational, management, and relational continuity associated with quality of care indicators? | MEDLINE (1996–2005) | Studies measuring continuity and outcomes Any patient population |
32 | No summary statement on literature |
| Worrall & Knight, 2006 (7) | How important is continuity of care for older patients in family practice? | MEDLINE, EMBASE, CINAHL (1970–2005) | Interpersonal continuity and outcomes Adults > 50 years |
5 | Evidence that continuity in the elderly is ‘scanty’ |
| Cabana & Jee, 2004 (4) | Does continuity of care improve patient outcomes? | MEDLINE, PSYCHINFO (1966–2002) | Primary care setting Continuity and outcomes |
18 | Continuity improves quality of care consistently in patients with chronic diseases |
Unlike the other systematic reviews identified, the systematic review by Jee and Cabana (2) did not assess the effectiveness of continuity of care, but rather the intent of this review was to identify the indices to assess continuity of care. The authors only included studies with a clearly defined measure of continuity and they found that there was considerable heterogeneity across indices for measuring continuity.
The systematic review by van Walraven et al (8) assessed quality of continuity of care using 4 criteria: the representativeness of the cohort; how the continuity measure was collected; how the outcome measure was collected and; and the adequacy of follow-up. Of the 18 studies included, 16 studies met 3 or 4 of the criteria. Only 1 study met only 1 criterion, and the other met 2 criteria.
Overall, the systematic reviews found that there appears to be an association between continuity of care and improved patient outcomes; however, the literature base is weak.
Studies of Continuity of Care in Patients With Any Condition
Five studies were identified that assessed continuity of care in patients with any condition (Tables 4, 5). There was 1 longitudinal study that tracked patient data for 7 year; (10) the others were cross-sectional studies. (11-14) Four of the studies analyzed data from administrative databases, and the other used survey data to generate results on continuity of care. (13) The studies using the larger administrative databases included from 30,000 to more than 500,000 patients. The selection of patients analysed from the databases differed across the studies. Selection criteria varied in terms of age cut-off, minimum number of visits, and the duration that data were gathered for. In each of the studies continuity with the patients’ primary physicians was assessed. The literature search did not identify continuity of care assessments with other health care providers. Three of the studies are Canadian (1 from Newfoundland & Labrador, and 2 from Manitoba) and the other 2 are from Taiwan. In Taiwan, national health insurance is relatively new (mid 1990s). The system has been arranged so that patients choose their primary care physician and their specialists. They do not require a referral to see a specialist and they can choose to see any primary care physician and go back and forth to different primary care providers as they choose. Thus, the issue of continuity of care is of interest to Taiwan to see if inconsistent contact with physicians is impacting health outcomes.
Table 4: Characteristics of Studies Assessing Continuity of Care in Patients With Any Condition.
| Study | Type of Study | Research Question | Population | N | Continuity With Whom/What | Primary Outcomes |
| Cheng et al, 2011 (11) (Taiwan) | Cross-sectional database study | Does continuity of care matter in a health care system that lacks referral arrangements? | Patients with more than 4 physician visits within 1 year | 134,422 | Measurement of continuity with the same physician provider | Hospitalization and ED visits |
| Cheng et al, 2010 (10) (Taiwan) | Longitudinal database study | What is the effect of continuity of care on avoidable hospitalization and hospital admission for any condition in a health care system with a high level of access to care? | 3 or more physician visits per year | 30,830 | Measurement of continuity with the same physician provider | Avoidable hospitalization and hospitalization for any condition |
| Ionescu-Ittuet al, 2007(12) (Canada) | Cross-sectional database study | Is continuity of primary care associated with ED visits in elderly people in both urban and rural areas? | Adults ≥ 65 years with 3 or more physician visits over 2 year period | 95,173 | Measurement of continuity with the same physician provider | ED visits |
| Menec et al, 2006 (13) (Canada) | Retrospective analysis of survey data | Does continuity of care with a family physician reduce hospitalizations among older adults? | Adults ≥ 67 years with 4 or more physician visits in 2 year period | 1,863 | Measurement of continuity with the same physician provider | Hospitalization |
| Menec et al, 2005 (14) (Canada) | Cross-sectional database study | Does continuity of care matter in a universally insured population? | All individuals who had at least 1 physician contact in 2 year period | 536,893 | Measurement of continuity with the same physician provider | ED visits and preventive care (pap smears, mammograms, flu shots) |
Abbreviations: ED, emergency department; N, number of patients.
Table 5: Results of Studies Assessing Continuity of Care in Patients With Any Condition.
| Study | N | Indices Used (How Was Continuity Measured?) | Continuity Cut-Off | Proportion of Patients in Each Continuity Category | Hospitalization | ED Visits |
| Cheng et al, 2011 (11) (Taiwan) | 134,422 | UPC, COC, SECON | 3 equal tertiles for each index—UPC, COC, SECON | UPC Low: 31.9% Medium: 34.7% High: 33.4% |
Odds ratio (No CI reported): UPC Low: 1.00 Medium: 0.92a High: 0.79a |
Odds ratio (No CI reported): UPC Low: 1.00 Medium: 0.88a High: 0.70a |
| COC Low: 30.6% Medium: 32.7% High: 28.4% |
COC Low: 1.00 Medium: 0.77a High: 0.90a |
COC Low: 1.00 Medium: 0.85a High: 0.68a |
||||
| SECON Low: 30.2% Medium: 28.9% High: 32.5% |
SECON Low: 1.00 Medium: 0.88a High: 0.87a |
SECON Low: 1.00 Medium: 0.82a High: 0.71a |
||||
| Cheng et al, 2010 (10) (Taiwan) | 30,830 | COC | 0–16% low continuity 17–33% medium continuity 34–100% high continuity (equal tertiles based on study population) |
NR | ≥ 65 years (any hospitalization) Odds ratio (95% CI) Low: 1.00 Medium: 0.62 (0.56–0.67)a High: 0.32 (0.29–0.36)a |
NR |
| Ionescu-Ittu et al, 2007(12) (Canada) | 95,173 | UPC | ≤ 50% low continuity 50–80% med continuity > 80% high continuity |
Low: 21% Medium: 32% High: 30% |
NR | Rate ratio (95% CI): Low: 1.00 Medium: 0.79 (0.77–0.80)a High: 0.68 (0.66–0.69)a |
| Menec et al, 2006 (13) (Canada) | 1,863 | “majority of care definition”—patients who made 75% of all visits to their family physician—high continuity | ≤ 75% low continuity > 75% high continuity |
Low: 35.5% High: 64.5% |
Odds ratio (95% CI): All Conditions Low: 1.00 High: 0.83 (0.67–1.01) ACSC Low: 1.00 High: 0.67 (0.51–0.90)a |
NR |
| Menec et al, 2005 (14) (Canada) | 536,893 | “majority of care definition”—patients who made 75% of all visits to their family physician—high continuity | ≤ 75% low continuity > 75% high continuity And < 50% low continuity > 50% high continuity |
NR | NR | Odds ratio (99% CI): COC 75% (Adults ≥15 yrs): Low: 1.00 High: 0.85 (0.80–0.90)a COC 50% (Adults ≥15 yrs): Low: 1.00 High: 0.78 (0.73–0.83)a |
Abbreviations: ACSC, ambulatory care sensitive conditions; CI, confidence interval; COC, Continuity of Care index; ED, emergency department; MMCI, Modified Modified Continuity Index; N, number of patients; NR, not reported; SECON, Sequence of Continuity index; UPC, Usual Provider of Care index.
P < 0.05
The study by Cheng et al from 2011 (11) reported that across 3 indices of continuity, higher continuity was associated with lower rates of hospital admissions and ED visits. This study used data from 2005 to assess continuity using the indices, and they applied this data to 2005 and 2006 outcomes for hospitalization and ED visits. The authors noted that although still significant, the effect of high continuity in 2005 was diminished in 2006. The results were consistent across all 3 indices of continuity used.
The prospective Ontario-based study by van Walraven et al (15) from 2010 assessed the continuity of care of patients discharged to the community after a hospitalization (either elective or emergency). The authors were specifically looking at physician continuity before, during, and after hospitalization. The study reported that continuity with the preadmission physician (either family physician or specialist) was associated with a decrease in subsequent hospitalizations (adjusted hazard ratio 0.94; 95% confidence interval, 0.91–0.98). In other words, if the patient saw the preadmission physician after discharge they were less likely to be readmitted to hospital than if they had been seen by another physician post discharge. Visits with the hospital physician post discharge did not have a significant impact on readmissions or mortality.
Three of 5 studies reported hospitalization rates in relation to continuity of care. Higher continuity was associated with a statistically significant reduced hospitalization rate in 2 of the 3 studies. (10;11) The study by Menec et al (13) reported a statistically significant reduction in the rate of hospitalizations in patients being admitted for ambulatory care–sensitive conditions, but not for all admissions.
Three of 5 studies reported ED visits in relation to continuity of care. All 3 studies reported a statistically significant reduction in ED visits in patients with higher continuity, regardless of how continuity was assessed. (11;12;14)
Studies of Continuity of Care in Patients With Diabetes
Eight studies were identified that assessed continuity of care in patients with diabetes (Tables 6, 7). More studies were identified for assessing continuity with diabetes care than any other chronic disease.
Table 6: Continuity of Care Index Results From Chen and Cheng’s Sensitivity Analysis by Visit Tertiles.
| Variable | Hospitalization | ED Visits | |
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | ||
| Low visit group (4–19 visits/year) | |||
| Low continuity | 1.00 | 1.00 | |
| Medium continuity | 0.59 (0.56–0.62) | 0.66 (0.62–0.70) | |
| High continuity | 0.24 (0.23–0.26) | 0.33 (0.31–0.36) | |
| Medium visit group (20–32 visits/year) | |||
| Low continuity | 1.00 | 1.00 | |
| Medium continuity | 0.57 (0.55–0.60) | 0.66 (0.63–0.70) | |
| High continuity | 0.26 (0.24–0.27) | 0.34 (0.32–0.36) | |
| High visit group (≥ 33 visits/year) | |||
| Low continuity | 1.00 | 1.00 | |
| Medium continuity | 0.57 (0.55–0.59) | 0.62 (0.59–0.65) | |
| High continuity | 0.28 (0.27–0.30) | 0.36 (0.33–0.38) | |
Abbreviation: CI, confidence interval.
Source: Chen and Cheng, 2011. (17)
Table 7: Characteristics of Studies Assessing Continuity of Care in Patients With Diabetes.
| Study | Type of Study | Research Question | Population | N | Continuity With Whom/What | Primary Outcomes |
| Chen & Cheng, 2011(17) (Taiwan) | Longitudinal database study | What is the effect of continuity of care on health care utilization and expenses for patients with diabetes? | Adult patients with diabetes (type 1 or 2) with 3 or more physician visits per year for 7 years | 48,107 | Measurement of continuity with the same physician provider | Healthcare utilization and healthcare expenses |
| Worrall &Knight, 2011 (21) (Canada) | Cross-sectional database study | What is the relationship between continuity of family physician care and all-cause mortality and hospitalizations in older people with diabetes? | Patients with diabetes over 65 years with 2 or more fee for service claims within 2 year period | 305 | Measurement of continuity with the same physician provider | Mortality Hospitalization |
| Hong et al, 2010 (22) (Korea) | Cross-sectional database study | Is there an association between continuity of care and health outcomes? | Patients with diabetes aged 65 to 84 years with 4 or more physician visits within previous 3 years | 268,220 | Measurement of continuity with the same physician provider | Hospitalizations, ED visits |
| Lin et al, 2010 (18) (Taiwan) | Cross-sectional database study | Is the discontinuity of care associated with hospitalization? | Patients with diabetes with 4 visits over 5 years | 6,476 | Measurement of continuity with the same physician provider | Diabetes-related admissions |
| Liu et al, 2010 (23) (USA) | Cross-sectional database study | What is the association between patterns of fragmented care and ED use among people with diabetes? | Patients with diabetes with 2 or more visits to a primary care practice within the previous year | 3,873 | Measurement of continuity by clinic site not individual providers | ED visits |
| Atlas et al, 2009 (19) (USA) | Cross-sectional database study | Does patient-physician connectedness affect measures of clinical performance? | Adults with 1 or more visits to primary care physician in a 3 year period | 155,590 | Measurement of continuity by clinic site and physician providers | HbA1c |
| Knight et al, 2009 (16) (Canada) | Longitudinal database study | Does higher continuity of family physician care reduce hospitalizations in elderly people with diabetes? | Elderly (> 65 years) with newly diagnosed diabetes; 6 physician visits over 3 years | 1,143 | Measurement of continuity with the same physician provider | Hospitalizations |
| Mainous et al, 2004 (20) & Koopman et al, 2003 (24) &Harvey et al, 2004 (25) (USA) | Cross-sectional database study | What is the relationship between continuity of care and diabetes control? | Patients with diabetes who participated in the 3rd NHANES | 1,400 | Measurement of continuity with the same physician provider | HbA1c, blood pressure, lipid control |
Abbreviations: ED, emergency department; HbA1c, glycosylated hemoglobin; N, number of patients; NHANES, National Health and Nutrition Examination Survey.
Knight et al (16) hypothesized that patients with more chronic conditions had lower continuity of care because they were more likely to be seen more urgently and thus not always able to visit their usual care provider on short notice compared to those patients with fewer chronic conditions who may have not needed to see their provider as urgently.
In 2011, Chen and Cheng (17) assessed continuity of care using 3 indices: UPC, COC, and SECON. They reported consistently that higher continuity of care was associated with fewer hospitalizations and ED visits. They also conducted a sensitivity analysis of the effect of the COC index on health care utilization by tertile of physician visits. Patients were stratified into low number of visits per year (4–19 visits), medium number of visits per year (20–32 visits), or high number of visits per year (≥ 33 visits). Again, the authors reported the same results, where patients with high continuity of care were associated with fewer hospitalizations and ED visits, regardless of which tertile of number of visits the patients were assigned (Table 6). The analysis was adjusted for age, sex, low-income status, hospitalizations in previous year, and diabetes complication severity index score.
The study by Liu et al (18) used the Fragmentation of Care Index (FCI) to assess continuity with clinic site; it did not assess individual care provider continuity. The study reported, not surprisingly, that patients with more chronic diseases had higher fragmentation scores (i.e., lower continuity) because they had more specialist appointments at different clinic sites. The study found that there was a significant association between the number of ED visits and the FCI. They calculated that for each 0.1 increase in FCI, there was an 18% increase in ED visits over the 2-year study period.
The study by Atlas et al (19) did not use a previously published index of continuity to measure continuity; instead, they assessed patients’ ‘connectedness’ with a physician or practice using a validated algorithm developed by the study authors. The study found that being connected to a physician versus being connected to a practice significantly improved glycosylated hemogolbin (HbA1c) levels in patients with diabetes (P = 0.004).
The study by Mainous et al (20) used data from the National Health and Nutrition Examination Survey (NHANES) to examine if there was an association between continuity of care and diabetes control. The study assessed continuity of care using the following questions from the survey: “Is there a particular clinic, health centre, doctor’s office, or other place that you usually go if you are sick, need advice about your health, or for routine care?” If they responded yes to the preceding question then they were asked “Is there one particular doctor or health professional you usually see?” Based on the responses to these questions, a continuity variable was created based on 3 categories: 1) no usual source of care; 2) usual site but no usual provider; or 3) usual site and provider. The study found that 85% of the respondents reported that they had both a usual site and a usual provider of care. Five percent reported having no usual source of care and 9% reported a usual site, but no usual provider of care. They reported a significant improvement in HbA1c levels in patients with high continuity of care (usual provider) versus low continuity (no provider), but they did not report a significant difference associated with continuity for systolic blood pressure or lipid levels.
Five studies reported hospitalization rates associated with continuity. Four studies reported that there were statistically significantly fewer hospitalizations associated with higher continuity compared to low or medium continuity. (16;17;21;22) These studies each used different indices to measure continuity. The study by Lin et al (18) reported a significant reduction in long-term complications leading to hospitalization (as defined by the International Classification of Diseases codes) in patients with high continuity of care compared to low continuity, but not compared to medium continuity. They did not report a significant difference in the relationship between continuity and short-term complications leading to hospitalization (defined by International Classification of Diseases codes). The authors attributed the nonsignificance to a low rate of events (n = 50).
Three studies reported the number of ED visits associated with continuity. All 3 studies reported a significantly reduced number of ED visits in patients with higher continuity of care. (17;22;23) Two of the studies used the COC index and the other used the FCI.
Two studies reported HbA1c levels in relation to continuity of care. Both reported that optimal glycemic control was more likely in patients with higher continuity compared to lower continuity. (19;20) The study by Mainous et al (20) also reported systolic blood pressure and lipid levels, but the study did not identify any significant differences in these outcomes in relation to continuity of care.
Studies of Continuity of Care in Patients With COPD
One cross-sectional study was identified that assessed continuity of care in patients with COPD (Tables 8, 9). This study by Hong et al (22) also included elderly patients (aged 65–84 years) with diabetes, hypertension, and asthma, in addition to COPD. The authors stratified the results by chronic disease. They used a Korean health administrative database to gather information of continuity on 131,512 patients with COPD. They reported a statistically significant increase in hospitalizations and ED visits in patients with low or medium continuity compared to patients with high continuity of care (P < 0.001).
Table 8: Results of Studies Assessing Continuity of Care in Patients With Diabetes.
| Study | N | Indices Used | Continuity Cut-Off | Proportion of Patients in Each Continuity Category | Hospitalization | ED Visits | Diabetes-Specific Outcomes |
| Chen &Cheng, 2011 (17) (Taiwan) | 48,107 | UPC, COC, SECON | < 0.47 low continuity 0.47–0.86 medium continuity ≥ 0.87 high continuity |
NR | Odds ratio (95% CI) UPC Low: 1.00 Medium: 0.61 (0.59–0.62) High: 0.26 (0.25–0.27) COC Low: 1.00 Medium: 0.58 (0.56–0.59) High: 0.26 (0.25–0.27) SECON Low: 1.00 Medium: 0.67 (0.66–0.69) High: 0.30 (0.29–0.31) |
Odds ratio (95% CI) UPC Low: 1.00 Medium: 0.68 (0.66–0.70) High: 0.35 (0.0.34–0.36) COC Low: 1.00 Medium: 0.64 (0.62–0.66) High: 0.34 (0.33–0.36) SECON Low: 1.00 Medium: 0.69 (0.67–0.72) High: 0.36 (0.35–0.37) |
NR |
| Worrall & Knight, 2011 (21) (Canada) | 305 | UPC | ≥ 0.75 high continuity < 0.75 low continuity |
Low: 27.2% High: 72.8% |
Percentage over 3 years: Low: 67.5% High: 54.5%b |
NR |
Mortality (percentage over 3 years): Low: 18.1% High: 9.0%b |
| Hong et al, 2010 (22) (Korea) | 268,220 | COC | Equal tertiles based on study population | NR | Odds ratio (95% CI) Low: 1.00 Medium: 0.75 (0.72–0.78)a High: 0.68 (0.66–0.71)a |
Odds ratio (95% CI) Low: 1.00 Medium: 0.77 (0.69–0.85)a High: 0.71 (0.64–0.79)a |
NR |
| Lin et al, 2010 (18) (Taiwan) | 6,476 | UPC | < 0.47 low continuity 0.47–0.75 medium continuity ≥ 0.75 high continuity |
NR | Odds ratio (95% CI) Long-term complications leading to admissions: Low: 1.00 Medium: 0.76 (0.58–1.00) High: 0.75 (0.58–0.98) a Short-term complications leading to admissions: Low: 1.12 (0.55–2.31) Medium: 0.78 (0.38–1.59) High: 0.89 (0.43–1.82) |
NR | NR |
| Liu et al, 2010 (23) (USA) | 3,873 | FCI (0–1) (low score, higher continuity) | Divided into quintiles | NR | NR | IRR: 0.87 (95% CI, 0.83–0.92; P < 0.01) | NR |
| Atlas et al, 2009 (19) (USA) | 155,590 (~10,000 with diabetes) | Created algorithm to define connectedness to physician, practice, or neither. | Equal tertiles based on study population | NR | NR | NR | HbA1c < 8% Physician connectedness: 74.7% (95% CI, 73.4–76.0) Practice connectedness: 70.5% (95% CI, 67.8–73.0) P = 0.004 |
| Knight et al, 2009 (16) (Canada) | 1,143 | UPC, COC, SECON | ≥ 0.75 high continuity < 0.75 low continuity |
COC Low: 36.6% High: 63.4% UPC Low: 23.7% High: 76.3% SECON Low: 18.5% High: 81.4% |
Odds Ratio (95% CI) High COC 0.82 (0.69–0.97) High UPC 0.82 (0.68–0.98) High SECON 0.75 (0.61–0.91) |
NR | NR |
| Mainous et al, 2004 (20) & Koopman et al, 2003(24) & Harvey et al, 2004(25) (USA) | 1400 | Based on responses to questions on NHANESa | 3 categories: no usual source of careusual site, but no usual providerusual site and provider | NR | NR | NR |
c Odds ratio, 95% CI HbA1c ≤ 7% No usual source: 1.00 Usual site: 11.81 (4.02–34.71) Usual provider: 6.69 (2.61–17.18) HbA1c ≤ 8% No usual source: 1.00 Usual site: 6.13 (2.08–18.04) Usual provider: 4.62 (2.02–10.60) SBP ≤ 130mmHg No usual source: 1.00 Usual site: 2.76 (0.70–10.93) Usual provider: 1.78 (0.55–5.72) SBP ≤ 140mmHg No usual source: 1.00 Usual site: 1.02 (0.28–3.78) Usual provider: 0.87 (0.36–2.13) Lipids ≤ 100mg/dL No usual source: 1.00 Usual site: 1.93 (0.71–5.24) Usual provider 1.10 (0.44–2.73) Lipids ≤ 130mg/dL No usual source: 1.00 Usual site: 2.37 (0.82–6.79) Usual provider: 1.59 (0.55–4.57) |
Abbreviations: CI, confidence interval; HbA1c, glycosylated haemoglobin; IRR, incidence rate ratio; N, number of patients; NHANES, National Health and Nutrition Examination Survey; NR, not reported.
Based on responses to the following questions on the NHANES:
• Is there a particular clinic, health center, doctor’s office, or other place that you usually go if you are sick, need advice about your health, or for routine care?
• If yes, is there one particular doctor or health professional you usually see?
P < 0.05
Results for all outcomes adjusted for age, gender, education, insurance coverage, health status, income, length of time with diabetes
Table 9: Characteristics of Studies Assessing Continuity of Care in Patients With COPD.
| Study | Type of Study | Research Question | Population | N | Continuity With Whom/What | Primary Outcomes |
| Hong et al, 2010 (22) (Korea) | Cross-sectional database study | Is there an association between continuity of care and health outcomes? | Patients with COPD aged 65 to 84 years with 4 or more physician visits within previous 3 years | 131,512 | Measurement of continuity with the same clinic site | Hospitalizations, ED visits |
Abbreviations: COPD, chronic obstructive pulmonary disease; ED, emergency department; N, number of patients.
Studies of Continuity of Care in Patients With Coronary Artery Disease
One cross-sectional study was identified that reported continuity of care in patients with coronary artery disease (CAD) (Tables 10, 11). This study also reported outcomes for patients with diabetes. They did not use a previously published index of continuity to measure continuity. Instead, Atlas et al (19) assessed patients’ ‘connectedness’ with a physician or practice using a validated algorithm developed by the study authors. They found that being connected to a physician versus being connected to a practice did not significantly influence cholesterol levels in patients with CAD.
Table 10: Results of Studies Assessing Continuity of Care in Patients With COPD.
| Study | Indices Used | Continuity Cut-Off | Proportion of Patients in Each Continuity Category | Hospitalization | ED visits |
| Hong et al, 2010 (22) (Korea) | COC | Equal tertiles based on study population | NR | Odds ratio (95% CI) Low 1.00 Medium 0.67 (0.62–0.71)a High 0.50 (0.47–0.69)a |
Odds ratio (95% CI) Low 1.00 Medium 0.77 (0.63–0.94)a High 0.56 0.46–0.69)a |
Abbreviations: CI, confidence interval; COC, continuity of care; COPD, chronic obstructive pulmonary disease; ED, emergency department; NR, not reported.
P < 0.05
Table 11: Characteristics of Studies Assessing Continuity of Care in Patients With CAD.
| Study | Type of Study | Research Question | Population | N | Continuity With Whom/What | Primary Outcome |
| Atlas et al, 2009(19) (USA) | Cross-sectional database study | Does patient-physician connectedness affect measures of clinical performance? | Adults with 1 or more visits to primary care physician in a 3 year period. | 155,590 (~7,000 with CAD) | Measurement of continuity by clinic site and physician providers | LDL cholesterol |
Abbreviations: CAD, coronary artery disease; LDL, low density lipoprotein; N, number of patients.
Limitations
The studies identified for this review were designed to assess the continuity of care, and not the most appropriate care. The continuity indices have been designed to measure continuity by implying that dispersion (i.e., seeing many different providers) is not optimal. However, there are situations in which this reasoning does not apply, especially for patients with chronic diseases that require some dispersion and need to see various specialists to optimally manage their care. Therefore, there are circumstances where dispersion is good and important for quality care. The continuity indices are not able to distinguish the ‘good’ dispersion from the ‘inappropriate’ dispersion.
Another limitation of this body of literature is that all of the studies were assessing physician continuity. There were no studies identified which assessed continuity of care among other health care providers (nurses, social workers, diabetes educators, etc.).
The majority of studies assessing continuity of care were large cross-sectional studies based on data from health administrative databases. There are some limitations associated with using large administrative datasets, including the accuracy of diagnosis. Often the databases are not used for research purposes; rather, the data is used for insurance claims which question the validity of the diagnosis. Many studies required that patients had multiple visits in order to be included in the study sample, thus trying to minimize the risk of error. Another limitation is the heterogeneity in the methods for choosing patients for the sample. For instance, some studies required 4 visits over a defined time period, while others required only 2 visits to be eligible for the study. Also, using large datasets allows for a large sample size, but the amount of data that can be gathered is limited. These large datasets do not capture information on trust and confidence in a patient’s provider or measures of patient and provider satisfaction.
Also, results from studies from countries where there is not a formal referral system, such as Taiwan, may not be generalizable to Ontario where most patients seek care first through primary care physicians.
Systematic Reviews Assessing Patient Satisfaction Associated With Continuity of Care
Three systematic reviews were identified that examined the relationship between continuity of care and patient satisfaction (Table 12). (1;26;27)
Table 12: Results of Studies Assessing Continuity of Care in Patients With CAD.
| Study | Indices Used | Continuity Cut-Off | Proportion of Patients in Each Continuity Category | Hospitalization | ED Visits | CAD-Specific Outcomes |
| Atlas et al, 2009 (19) (USA) | Created algorithm to define connectedness to physician, practice, or neither | Equal tertiles based on study population | NR | NR | NR | LDL level < 2.59 mmol/L Physician connectedness: 77.0% (95% CI, 75.7–78.4) Practice connectedness: 77.6% (95% CI, 74.4–80.5) P = 0.74 |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; ED, emergency department; LDL, low density lipoprotein; NR, not reported.
In 2012, Waibel et al (1) published a synthesis of qualitative studies assessing patients’ perspectives on continuity of care. This meta-synthesis was thorough in describing the methods of identifying studies, selecting studies for inclusion, extracting data, and in defining themes. As is common with many search strategies for qualitative studies, their literature search may have missed some studies due to the inconsistency of terminology used in studies and the terms indexed in the literature search databases. To mitigate some of this bias, they hand-searched references of selected studies for any studies missed in the original literature search. Waibel et al (1) identified 25 studies to include in their analysis and stratified the studies into 3 groups: relational continuity, management continuity, and informational continuity. The majority of the studies were focused on relational continuity. In other words, they were interested in the patient-provider interaction and relationship. Based on the meta-synthesis of the qualitative studies, Waibel et al (1) concluded that chronically ill patients valued continuity with one provider over time, compared to younger patients who valued both continuity with the provider and convenient access.
In 2010, Adler et al (26) published a systematic review on continuity of care focused specifically on relational continuity. The authors reported that patient satisfaction was described in several different ways in the 12 studies included in their review. This heterogeneity did not permit them to make strong conclusions as to whether there was an association between continuity and patient satisfaction.
Saultz and Albedaiwi (27) also reviewed the association between relational continuity of care and patient satisfaction. Like Adler et al, (26) Saultz and Albedaiwi (27) also identified a lot of heterogeneity in the literature on continuity of care and patient satisfaction. Nonetheless, they concluded that patient satisfaction was improved with higher continuity of care because of the consistency of results in the studies they identified.
Overall, there does appear to be a positive relationship between high continuity of care and patient satisfaction.
Table 13: Summary of Systematic Reviews of Patient Satisfaction.
| Study | Research Question | Sources & Years Searched | Inclusion Criteria | Number of Studies Included | Conclusions |
| Waibel et al, 2012 (1) | What do we know about patients’ perceptions of continuity of care? | MEDLINE, Social Sciences Citation Index (up to 2009) | Explicit or implicit analysis of continuity Qualitative study design patient’s perspective |
25 | Continuity is valued more in patients with chronic illnesses compared with younger, healthier patients |
| Adler et al, 2010 (26) | What is the evidence on the relationship between continuity and patient satisfaction? | MEDLINE, CINAHL (1984–2007) | Reported measures of relational continuity and patient satisfaction | 12 | Inconsistent results across studies |
| Saultz & Albedaiwi, 2004 (27) | What is the association between interpersonal continuity and the level of patient satisfaction? | MEDLINE (1996–2002) | Reported measures of relational continuity and patient satisfaction | 22 | “A consistent and significant positive relationship exists between interpersonal continuity and patient satisfaction” |
Conclusions
There is low quality evidence that:
Despite heterogeneity in how continuity is measured, higher continuity of care appears to decrease health service utilization (hospitalizations and ED visits).
There is insufficient evidence to comment on the relationship of continuity of care with disease-specific outcomes.
There appears to be a positive association between high continuity and patient satisfaction, particularly among patients with chronic disease.
Table 14: Summary of Findings.
| Outcome | Number of Studies (N) | Results | GRADE |
| Hospitalizations | 9 (622,573) | 9/9 studies reported fewer hospitalizations with higher continuity | LOW |
| ED visits | 7 (1,218,200) | 7/7 studies reported fewer ED visits with higher continuity | LOW |
| HbA1c (Diabetes) | 2 (11,400) | 2/2 studies reported greater HbA1c control with higher continuity | LOW |
| LDL cholesterol (CAD) | 1 (7,000) | No difference | VERY LOW |
| Patient satisfaction | 3 systematic reviews | Positive association between high continuity and patient satisfaction | LOWa |
Abbreviations: CAD, coronary artery disease; ED, emergency department; HbA1c, glycosylated hemoglobin; LDL, low density lipoprotein; n, number of patients.
Grading is based on the most recent systematic review by Waibel et al. (1)
Acknowledgements
Editorial Staff
Irina Alecu
Medical Information Services
Kaitryn Campbell, BA(H), BEd, MLIS
Kellee Kaulback, BA(H), MISt
Expert Panel for Health Quality Ontario: Optimizing Chronic Disease Management in the Community (Outpatient) Setting
| Name | Title | Organization |
|---|---|---|
| Shirlee Sharkey (chair) | President & CEO | Saint Elizabeth Health Care |
| Theresa Agnew | Executive Director | Nurse Practitioners’ Association of Ontario |
| Onil Bhattacharrya | Clinician Scientist | Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto |
| Arlene Bierman | Ontario Women’s Health Council Chair in Women’s Health | Department of Medicine, Keenan Research Centre in the Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto |
| Susan Bronskill | Scientist | Institute for Clinical Evaluative Sciences |
| Catherine Demers | Associate Professor | Division of Cardiology, Department of Medicine, McMaster University |
| Alba Dicenso | Professor | School of Nursing, McMaster University |
| Mita Giacomini | Professor | Centre of Health Economics & Policy Analysis, Department of Clinical Epidemiology & Biostatistics |
| Ron Goeree | Director | Programs for Assessment of Technology in Health (PATH) Research Institute, St. Joseph’s Healthcare Hamilton |
| Nick Kates | Senior Medical Advisor | Health Quality Ontario – QI McMaster University Hamilton Family Health Team |
| Murray Krahn | Director | Toronto Health Economics and Technology Assessment (THETA) Collaborative, University of Toronto |
| Wendy Levinson | Sir John and Lady Eaton Professor and Chair | Department of Medicine, University of Toronto |
| Raymond Pong | Senior Research Fellow and Professor | Centre for Rural and Northern Health Research and Northern Ontario School of Medicine, Laurentian University |
| Michael Schull | Deputy CEO & Senior Scientist | Institute for Clinical Evaluative Sciences |
| Moira Stewart | Director | Centre for Studies in Family Medicine, University of Western Ontario |
| Walter Wodchis | Associate Professor | Institute of Health Management Policy and Evaluation, University of Toronto |
Appendices
Appendix 1: Literature Search Strategies
Search date: December 8-9th, 2011
Databases searched: OVID MEDLINE, OVID MEDLINE In-Process and Other Non-Indexed Citations, OVID EMBASE, Wiley Cochrane, EBSCO CINAHL, Centre for Reviews and Dissemination.
Limits: 2002-present; English; NOT comments, editorials, letters (conference abstracts in Embase)
Database: Ovid MEDLINE(R) <1948 to November Week 3 2011>, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations <December 8, 2011>, Embase <1980 to 2011 Week 48>
Search Strategy:
| # | Searches | Results |
| 1 | Continuity of Patient Care/use mesz | 12501 |
| 2 | “Referral and Consultation”/use mesz | 46299 |
| 3 | (((continuity or continuum) adj 5 (care or health care or healthcare or in-patient? or inpatient? or patient? or physician? or provider? or out-patient? or outpatient? or visit?)) or continuity-of-care or continuous care or continuous health care or continuous healthcare).ti,ab. | 16244 |
| 4 | ((patient-physician relation* or physician-patient relation* or patient relation?) and (continuous* or length or time)).mp. | 15553 |
| 5 | *Patient Care/use emez | 35993 |
| 6 | *Patient Referral/use emez | 11041 |
| 7 | or/1-6 | 130862 |
| 8 | exp Coronary Artery Disease/ | 210163 |
| 9 | exp Myocardial Infarction/use mesz | 136258 |
| 10 | exp heart infarction/use emez | 213996 |
| 11 | (coronary artery disease or cad or heart attack).ti. | 44510 |
| 12 | ((myocardi* or heart or cardiac or coronary) adj2 (atheroscleros* or arterioscleros* or infarct*)).ti. | 150312 |
| 13 | or/8-12 | 538832 |
| 14 | exp Atrial Fibrillation/use mesz | 28533 |
| 15 | exp heart atrium fibrillation/use emez | 53857 |
| 16 | ((atrial or atrium or auricular) adj1 fibrillation*).ti,ab. | 72761 |
| 17 | or/14-16 | 98450 |
| 18 | exp heart failure/ | 299162 |
| 19 | ((myocardi* or heart or cardiac) adj2 (failure or decompensation or insufficiency)).ti,ab. | 236085 |
| 20 | 18 or 19 | 381647 |
| 21 | exp Stroke/ | 177440 |
| 22 | exp Ischemic Attack, Transient/use mesz | 16615 |
| 23 | exp transient ischemic attack/use emez | 19389 |
| 24 | exp stroke patient/use emez | 5349 |
| 25 | exp brain infarction/or exp cerebrovascular accident/use emez | 101283 |
| 26 | (stroke or tia or transient ischemic attack or cerebrovascular apoplexy or cerebrovascular accident or cerebrovascular infarct* or brain infarct* or CVA).ti,ab. | 280877 |
| 27 | or/21-26 | 391325 |
| 28 | exp Diabetes Mellitus, Type 2/use mesz | 70333 |
| 29 | exp non insulin dependent diabetes mellitus/use emez | 100079 |
| 30 | exp diabetic patient/use emez | 11998 |
| 31 | (diabetes or diabetic* or niddm or t2dm).ti,ab. | 767609 |
| 32 | or/28-31 | 792582 |
| 33 | exp Skin Ulcer/ | 72332 |
| 34 | ((pressure or bed or skin) adj2 (ulcer* or sore* or wound*)).ti,ab. | 29008 |
| 35 | (decubitus or bedsore*).ti,ab. | 8583 |
| 36 | or/33-35 | 91251 |
| 37 | exp Pulmonary Disease, Chronic Obstructive/use mesz | 17237 |
| 38 | exp chronic obstructive lung disease/use emez | 53936 |
| 39 | (chronic obstructive adj2 (lung* or pulmonary or airway* or airflow or respiratory) adj (disease* or disorder*)).ti,ab. | 54470 |
| 40 | (copd or coad).ti,ab. | 45341 |
| 41 | chronic airflow obstruction.ti,ab. | 1067 |
| 42 | exp Emphysema/ | 37319 |
| 43 | exp chronic bronchitis/use emez | 6930 |
| 44 | ((chronic adj2 bronchitis) or emphysema).ti,ab. | 51113 |
| 45 | or/37-44 | 159066 |
| 46 | exp Chronic Disease/ | 344492 |
| 47 | (chronic*adj2 disease* or (chronic* adj2 ill*)).ti,ab. | 32477 |
| 48 | 46 or 47 | 363168 |
| 49 | Comorbidity/ | 143490 |
| 50 | (comorbid* or co-morbid* or multimorbid* or multi-morbid* or (complex* adj patient*) or (multiple adj2 (condition* or disease* or patient*))).ti,ab. | 228158 |
| 51 | 49 or 50 | 309127 |
| 52 | 13 or 17 or 20 or 27 or 32 or 36 or 45 or 48 or 51 | 2739149 |
| 53 | 7 and 52 | 13143 |
| 54 | limit 53 to yr="2002 - 2012" | 8443 |
| 55 | limit 54 to english language | 7414 |
| 56 | Case Reports/or Comment.pt. or Editorial.pt. or Letter.pt. use mesz | 2943299 |
| 57 | Case Report/or Editorial/or Letter/or Conference Abstract.pt. use emez | 5773844 |
| 58 | 55 not (56 or 57) | 6462 |
| 59 | remove duplicates from 58 [Sets larger than 6000 cannot be de-duped] | 6462 |
Appendix 2: GRADE Tables
Table A1: GRADE Evidence Profile for Continuity of Care.
| Number of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
| Hospitalization | |||||||
| 8 (observational) | No serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| ED Visits | |||||||
| 6 (observational) | No serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
| Patient Satisfaction | |||||||
| 25 (observational) from Waibel et al (1) systematic review | No serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | None | ⊕⊕ Low |
Abbreviation: ED, emergency department.
Table A2: Risk of Bias Among Observational Trials on the Effectiveness of Continuity of Care on Health Resource Utilization.
| Author, Year | Appropriate Eligibility Criteria | Appropriate Measurement of Exposure | Appropriate Measurement of Outcome | Adequate Control for Confounding | Complete Follow-Up |
| Chen & Cheng, 2011 (17) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Cheng et al, 2011 (11) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Worrall & Knight, 2011 (21) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Cheng et al, 2010 (10) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Hong et al, 2010 (22) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Lin et al, 2010 (18) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Liu et al, 2010 (23) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Atlas et al, 2009 (19) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Knight et al, 2009 (16) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Ionescu-Ittu et al, 2007 (12) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Menec et al, 2006 (13) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Menec et al, 2005 (14) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Mainous et al, 2004 (20) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Harvey et al, 2004 (25) | No limitations | No limitations | No limitations | No limitations | No limitations |
| Koopman et al, 2003 (24) | No limitations | No limitations | No limitations | No limitations | No limitations |
Suggested Citation
This report should be cited as follows: Health Quality Ontario. Continuity of care to optimize chronic disease management in the community setting: an evidence-based analysis. Ont Health Technol Assess Ser [Internet]. 2013 September;13(6):1–41. Available from: http://www.hqontario.ca/en/documents/eds/2013/full-report-OCDM-continuity-of-care.pdf
Indexing
The Ontario Health Technology Assessment Series is currently indexed in MEDLINE/PubMed, Excerpta Medica/EMBASE, and the Centre for Reviews and Dissemination database.
Permission Requests
All inquiries regarding permission to reproduce any content in the Ontario Health Technology Assessment Series should be directed to: EvidenceInfo@hqontario.ca.
How to Obtain Issues in the Ontario Health Technology Assessment Series
All reports in the Ontario Health Technology Assessment Series are freely available in PDF format at the following URL: http://www.hqontario.ca/en/mas/mas_ohtas_mn.html.
Conflict of Interest Statement
All reports in the Ontario Health Technology Assessment Series are impartial. There are no competing interests or conflicts of interest to declare.
Peer Review
All reports in the Ontario Health Technology Assessment Series are subject to external expert peer review. Additionally, Health Quality Ontario posts draft reports and recommendations on its website for public comment prior to publication. For more information, please visit: http://www.hqontario.ca/en/mas/ohtac_public_engage_overview.html.
About Health Quality Ontario
Health Quality Ontario (HQO) is an arms-length agency of the Ontario government. It is a partner and leader in transforming Ontario’s health care system so that it can deliver a better experience of care, better outcomes for Ontarians and better value for money.
Health Quality Ontario strives to promote health care that is supported by the best available scientific evidence. HQO works with clinical experts, scientific collaborators and field evaluation partners to develop and publish research that evaluates the effectiveness and cost-effectiveness of health technologies and services in Ontario.
Based on the research conducted by HQO and its partners, the Ontario Health Technology Advisory Committee (OHTAC) — a standing advisory sub-committee of the HQO Board — makes recommendations about the uptake, diffusion, distribution or removal of health interventions to Ontario’s Ministry of Health and Long-Term Care, clinicians, health system leaders and policy-makers.
This research is published as part of Ontario Health Technology Assessment Series, which is indexed in CINAHL, EMBASE, MEDLINE, and the Centre for Reviews and Dissemination. Corresponding OHTAC recommendations and other associated reports are also published on the HQO website. Visit http://www.hqontario.ca for more information.
About the Ontario Health Technology Assessment Series
To conduct its comprehensive analyses, HQO and/or its research partners reviews the available scientific literature, making every effort to consider all relevant national and international research; collaborates with partners across relevant government branches; consults with clinical and other external experts and developers of new health technologies; and solicits any necessary supplemental information.
In addition, HQO collects and analyzes information about how a health intervention fits within current practice and existing treatment alternatives. Details about the diffusion of the intervention into current health care practices in Ontario add an important dimension to the review. Information concerning the health benefits; economic and human resources; and ethical, regulatory, social, and legal issues relating to the intervention assist in making timely and relevant decisions to optimize patient outcomes.
The public consultation process is available to individuals and organizations wishing to comment on reports and recommendations prior to publication. For more information, please visit: http://www.hqontario.ca/en/mas/ohtac_public_engage_overview.html.
Disclaimer
This report was prepared by HQO or one of its research partners for the Ontario Health Technology Advisory Committee and developed from analysis, interpretation, and comparison of scientific research. It also incorporates, when available, Ontario data and information provided by experts and applicants to HQO. It is possible that relevant scientific findings may have been reported since completion of the review. This report is current to the date of the literature review specified in the methods section, if available. This analysis may be superseded by an updated publication on the same topic. Please check the HQO website for a list of all publications: http://www.hqontario.ca/en/mas/mas_ohtas_mn.html.
Health Quality Ontario
130 Bloor Street West, 10th Floor
Toronto, Ontario
M5S 1N5
Tel: 416-323-6868
Toll Free: 1-866-623-6868
Fax: 416-323-9261
Email: EvidenceInfo@hqontario.ca
ISSN 1915-7398 (online)
ISBN 978-1-4606-1239-2 (PDF)
© Queen’s Printer for Ontario, 2013
List of Tables
| Table 1: Measures of Continuity of Care |
| Table 2: Body of Evidence Examined According to Study Design |
| Table 3: Summary of Systematic Reviews on Continuity of Care |
| Table 4: Characteristics of Studies Assessing Continuity of Care in Patients With Any Condition |
| Table 5: Results of Studies Assessing Continuity of Care in Patients With Any Condition |
| Table 6: Continuity of Care Index Results From Chen and Cheng’s Sensitivity Analysis by Visit Tertiles |
| Table 7: Characteristics of Studies Assessing Continuity of Care in Patients With Diabetes |
| Table 8: Results of Studies Assessing Continuity of Care in Patients With Diabetes |
| Table 9: Characteristics of Studies Assessing Continuity of Care in Patients With COPD |
| Table 10: Results of Studies Assessing Continuity of Care in Patients With COPD |
| Table 11: Characteristics of Studies Assessing Continuity of Care in Patients With CAD |
| Table 12: Results of Studies Assessing Continuity of Care in Patients With CAD |
| Table 13: Summary of Systematic Reviews of Patient Satisfaction |
| Table 14: Summary of Findings |
| Table A1: GRADE Evidence Profile for Continuity of Care |
| Table A2: Risk of Bias Among Observational Trials on the Effectiveness of Continuity of Care on Health Resource Utilization |
List of Abbreviations
- CAD
Coronary artery disease
- COC
Continuity of Care Index
- COPD
Chronic obstructive pulmonary disease
- ED
Emergency department
- FCI
Fragmentation of Care Index
- HbA1c
Hemoglobin A1c
- NHANES
National Health and Nutrition Examination Survey
- SECON
Sequential Continuity Index
- UPC
Usual Provider of Care Index
Footnotes
No studies specifically focused on management continuity were identified from the literature search.
No studies specifically focused on management continuity were identified from the literature search.
Please note: All hospitalization and ED visit data represent all-cause hospitalizations, and do not distinguish between initial hospitalization or ED visit and rehospitalization or repeat ED visits.
References
- 1.Waibel S, Henao D, Aller MB, Vargas I, Vazquez ML, et al. What do we know about patients’ perceptions of continuity of care? A meta-analysis of qualitative studies. Int J Qual Health Care. 2012;24:39–48. doi: 10.1093/intqhc/mzr068. [DOI] [PubMed] [Google Scholar]
- 2.Jee SH, Cabana MD, et al. Indices for continuity of care: A systematic review of the literature. Med Care Res Rev. 2006;63(2):158–88. doi: 10.1177/1077558705285294. [DOI] [PubMed] [Google Scholar]
- 3.Reid R, Haggerty J, McKendry R, Defusing the confusion: concepts and measures of continuity of healthcare [internet]. Canadian Health Services Research Foundation. [2002 [cited: 2012 Mar 4].]. Available from: http://www.chsrf.ca/publicationsandresources/researchreports/commissionedresearch/02-03-01/58a53ce8-39f2-466a-8e98-8ffc36cf456c.aspx .
- 4.Cabana MD, Jee SH, et al. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):974–80. [PubMed] [Google Scholar]
- 5.Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A, et al. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380–2. doi: 10.1016/j.jclinepi.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 6.Goodman C, et al. Literature searching evidence interpretation for assessing health care practices. Stockholm, Sweden: Swedish Council on Technology Assessment in Health Care. 1996;119E doi: 10.1017/s0266462300008321. [DOI] [PubMed] [Google Scholar]
- 7.Worrall G, Knight J, et al. Continuity of care for older patients in family practice. Can Fam Physician. 2006;52:755–9. [PMC free article] [PubMed] [Google Scholar]
- 8.van Walraven C, Oake N, Jennings A, Forster AJ, et al. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010;16:947–56. doi: 10.1111/j.1365-2753.2009.01235.x. [DOI] [PubMed] [Google Scholar]
- 9.van Servellen G, Fongwa M, Mockus DE, et al. Continuity of care and quality care outcomes for people experiencing chronic conditions: A literature review. Nurs Health Sci. 2006;8(3):185–95. doi: 10.1111/j.1442-2018.2006.00278.x. [DOI] [PubMed] [Google Scholar]
- 10.Cheng S-H, Chen C-C, Hou YF, et al. A longitudinal examination of continuity of care and avoildable hospitalization. Arch Intern Med. 2010;170:1671–7. doi: 10.1001/archinternmed.2010.340. [DOI] [PubMed] [Google Scholar]
- 11.Cheng S-H, Hou YF, Chen C-C, et al. Does continuity of care matter in a health care system that lacks referral arrangements? Health Policy Plan. 2011;26:157–62. doi: 10.1093/heapol/czq035. [DOI] [PubMed] [Google Scholar]
- 12.Ionescu-Ittu R, McCusker J, Ciampi A, Vadeboncoeur AM, Roberge D, Larouche D, et al. Continuity of primary care and emergency department utilization among elderly people. Can Med Assoc J. 2007;177(11):1362–8. doi: 10.1503/cmaj.061615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menec VH, Sirski M, Attawar D, Katz A, et al. Does continuity of care with a family physician reduce hospitalizations among older adults? J Health Serv Res Policy. 2006;11:196–201. doi: 10.1258/135581906778476562. [DOI] [PubMed] [Google Scholar]
- 14.Menec VH, Sirski M, Attawar D, et al. Does continuity of care matter in a universally insured population? Health Serv Res. 2005;40:389–400. doi: 10.1111/j.1475-6773.2005.00363.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Walraven C, Taljaard M, Etchells E, Bell CM, Stiell IG, Zarnke K, et al. The independent association of provider and information continuity on outcomes after hospital discharge: implications for hospitalists. J Hosp Med. 2010;5(7):398–405. doi: 10.1002/jhm.716. [DOI] [PubMed] [Google Scholar]
- 16.Knight JC, Dowden JJ, Worrall GJ, Gadag VG, Murphy MM, et al. Does higher continuity of family physician care reduce hospitalizations in elderly people with diabetes? Popul Health Manag. 2009;12(2):81–6. doi: 10.1089/pop.2008.0020. [DOI] [PubMed] [Google Scholar]
- 17.Chen C-C, Cheng S-H, et al. Better continuity of care reduces costs for diabetic patients. Am J Manag Care. 2011;17(6):420–7. [PubMed] [Google Scholar]
- 18.Lin W, Huang IC, Wang SL, Yang MC, Yaung CL, et al. Continuity of diabetes care is associated with avoidable hospitalizations: Evidence from Taiwan’s National Health Insurance scheme. Int J Qual Health Care. 2010;22(1):3–8. doi: 10.1093/intqhc/mzp059. [DOI] [PubMed] [Google Scholar]
- 19.Atlas SJ, Grant RW, Ferris TG, Chang Y, Barry MJ, et al. Patient-physician connectedness and quality of primary care. Ann Intern Med. 2009;150(5):325–35. doi: 10.7326/0003-4819-150-5-200903030-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mainous III AG, Koopman RJ, Gill JM, Baker R, Pearson WS, et al. Relationship between continuity of care and diabetes control: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2004;94(1):66–70. doi: 10.2105/ajph.94.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Worrall G, Knight J, et al. Continuity of care is good for elderly people with diabetes. Can Fam Physician. 2011;57:16–20. [PMC free article] [PubMed] [Google Scholar]
- 22.Hong JS, Kang HC, Kim J, et al. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea. J Korean Med Sci. 2010;25(9):1259–71. doi: 10.3346/jkms.2010.25.9.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu CW, Einstadter D, Cebul RD, et al. Care fragmentation and emergency department use among complex patients with diabetes. Am J Manag Care. 2010;16(6):413–20. [PubMed] [Google Scholar]
- 24.Koopman RJ, Mainous III AG, Baker R, Gill JM, Gilbert GE, et al. Continuity of care and recognition of diabetes, hypertension, and hypercholesterolemia. Arch Intern Med. 2003;163(11):1357–61. doi: 10.1001/archinte.163.11.1357. [DOI] [PubMed] [Google Scholar]
- 25.Harvey P, et al. Attending a single care site associated with improved glycaemic control in people with diabetes. Evid Based Healthcare. 2004;8(4):192–4. [Google Scholar]
- 26.Adler R, Vasiliadis A, Bickell N, et al. The relationship between continuity and patient satisfaction: a systematic review. Fam Pract. 2010;27:171–8. doi: 10.1093/fampra/cmp099. [DOI] [PubMed] [Google Scholar]
- 27.Saultz JW, Albedaiwi W, et al. Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004;2:445–51. doi: 10.1370/afm.91. [DOI] [PMC free article] [PubMed] [Google Scholar]


