Abstract
Background:
Sudden cardiac death (SCD) events are tragic. Secondary prevention of SCD depends on availability of automated external defibrillators (AEDs). High school athletes represent a high-risk group for SCD, and current efforts aim to place AEDs in all high schools.
Hypothesis:
The prevalence of AEDs and emergency planning for sudden cardiac arrest (SCA) in Vermont high schools is similar to other states. Understanding specific needs and limitations in rural states may prevent SCD in rural high schools.
Study Design:
Cross-sectional survey.
Methods:
A survey was distributed to all 74 Vermont high school athletic directors. Outcome measures included AED prevalence, AED location, individuals trained in cardiopulmonary resuscitation (CPR) and AED utilization, funding methods for AED attainment, and the establishment of an emergency action plan (EAP) for response to SCA.
Results:
All schools (100%, 74 of 74) completed the survey. Of those, 60 (81%) schools have at least 1 AED on school premises, with the most common location for AED placement being the main office or lobby (50%). Larger sized schools were more likely to have an AED on the premises than smaller sized schools (P = 0.00). School nurses (77%) were the most likely individuals to receive formal AED training. Forty-one schools (55%) had an EAP in place for response to SCA, and 71% of schools coordinated AED placement with local emergency medical services (EMS) responders.
Conclusion:
In Vermont, more than two-thirds of high schools have at least 1 AED on school premises. However, significant improvement in the establishment of EAPs for SCA and training in CPR and AED utilization is essential given the rural demography of the state of Vermont.
Clinical Relevance:
Rural high schools inherently have longer EMS response times. In addition to obtaining AEDs, high schools must develop a public access to defibrillation program to maximize the chance of survival following cardiac arrest, especially in rural settings.
Keywords: automated external defibrillators, sudden cardiac arrest, emergency action plan
Sudden cardiac arrests (SCAs) in young, healthy-appearing individuals are tragic and unexpected. When these events occur, they are often the topic of extensive media coverage and focus our attention on the prevention of sudden cardiac death. To date, research on the utilization of automated external defibrillators (AEDs) to treat high school students with SCA has been limited. SCA in the young population is often a result of underlying structural heart disease, which may be more resistant to delays in defibrillation and account for poor survival outcomes when defibrillation is employed.8 Nevertheless, the placement of AEDs in locations for public access and use by trained or untrained personnel has shown a survival benefit following out-of-hospital cardiac arrest.5,14,17 Early defibrillation is the strongest determinant of survival following out-of-hospital cardiac arrest, with survival rates declining from 7% to 10% with every minute that defibrillation is delayed.1 Given the favorable outcomes with employment of public access defibrillation and the desire to prevent sudden cardiac death in the school-aged population, there has recently been a widespread movement toward the implementation of AEDs in many high schools across the country. The purpose of this investigation was to investigate the prevalence of AEDs and emergency planning for SCA in high schools throughout the state of Vermont.
Methods
A 22-question Web-based survey (see online appendix available at http://sph.sagepub.com/content/suppl) was developed, and invitations to participate were distributed via electronic mail to all high school athletic directors in the state of Vermont (n = 74). The survey was adapted from the Web-based National Registry for AED Use in Sports (http://www.AEDSPORTS.com). Subsequent follow-up with redistribution of the survey took place at 4-, 8-, and 12-week intervals after the initial distribution. After 12 weeks, all remaining nonresponders were contacted by telephone in attempts to complete the survey. The survey was first distributed in May 2011, and all surveys were completed by December 2011. All identifying information was kept confidential, and only the authors conducting the study knew the individual results of each responder.
The survey consisted of questions pertaining to the population of each high school, the number of students participating in athletics, the existence of an emergency action plan (EAP) in response to SCA, the prevalence of AEDs in each high school, those formally trained in cardiopulmonary resuscitation (CPR) and AED utilization, the coordination of AED location in each school with local emergency medical services (EMS), as well as the location, cost, and funding for the AEDs. Categorical data were analyzed utilizing the Cochran-Armitage test for trend (SAS v.9.3 SAS Institute, Cary, North Carolina), and 2-sided P values were reported.
An online survey tool (SurveyMonkey.com, LLC, Palo Alto, California) was used to help implement the questionnaire. Using the site, we were able to track responses as well as collect and analyze our results. This study was exempted from institutional review as this was public information, placed no patient population at risk, did not apply any form of intervention toward patients, and was designed to gather only descriptive information about high schools in the state of Vermont.
Results
All high schools in Vermont (100%, 74 of 74) responded to our survey. In all but 1 instance, the survey was completed by the high school athletic director. In the 1 exception, the athletic director forwarded the survey on to the school nurse, as it was felt that the nurse was more capable of providing the information needed to complete the survey. Although all 74 schools responded, 4 schools did not fill out the survey to completion. However, the categorical data that those 4 schools did provide were included within our statistical analysis. Of the 74 schools that responded, 60 (81%) reported having at least 1 AED on site. When comparing size of school to AED prevalence, larger schools (>800 students) were more likely to have an AED on school grounds than smaller schools (<400 students) (Z score = −3.13, P = 0.00) (Table 1). Of the 60 schools with an AED, 56 completed the survey in its entirety, providing information on the total number of AEDs in place. Of the 56 schools, 23 (41%) had 2 AEDs, 7 (13%) had 3 AEDs, and 4 (7%) had 4 or more devices. The remaining schools (39%) had a single device on site (Figure 1).
Table 1.
AED prevalence in Vermont high schools
| School Size (students) | Number of Schools | No AED | AED | Percentage With AED |
|---|---|---|---|---|
| <200 | 25 | 9 | 16 | 36 |
| 201-400 | 20 | 5 | 15 | 75 |
| 401-600 | 10 | 0 | 10 | 100 |
| 601-800 | 7 | 0 | 7 | 100 |
| 801-1000 | 8 | 0 | 8 | 100 |
| >1000 | 4 | 0 | 4 | 100 |
AED, automated external defibrillator.
Figure 1.
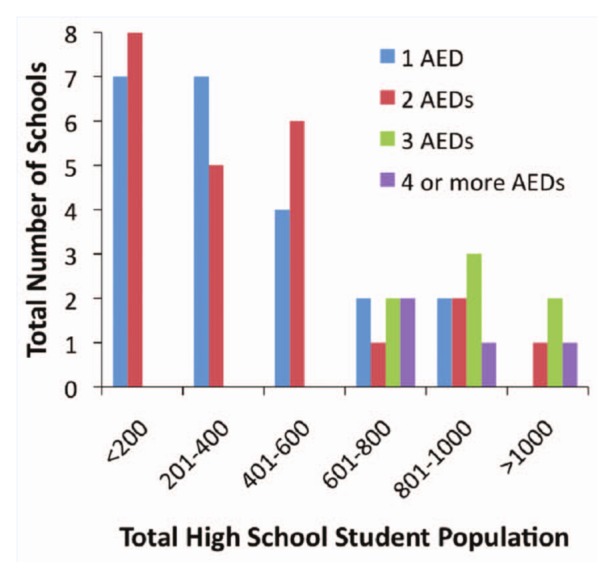
Overall automated external defibrillator (AED) distribution among 56 Vermont high schools.
The most common sites in which AEDs could be found within the high schools were the main office or lobby (50%) and the nurse’s office (45%). Only 30% of schools kept an AED within the gymnasium, 29% kept an AED within the training room, and 16% kept an AED at athletic fields or arenas (eg, hockey rinks). Of schools with AED(s), 71% reported that they had coordinated the location of their AED(s) with local EMS responders and that those responders were able to access the AED(s) upon arrival.
In schools with AEDs, the school nurse (77%) was most likely to receive formal AED training. Other school personnel trained in the utilization of an AED included teachers (57%), administrators (54%), and athletic trainers (48%). Coaches (45%) were one of the least likely to have training in AED use. CPR training among school personnel followed a similar trend, with 74% of nurses being CPR certified. After school nurses, 47% of coaches, 45% of athletic trainers, and 43% of administrators were trained in CPR.
When asked about the cost for each high school to acquire a single AED, 48% of schools reported that it would cost them between $1001 and $2000 per AED. Of the various means available to finance the purchase of an AED, survey participants reported that 46% of schools purchased their AED(s) with funding from the school budget, while 39% were funded through grants and 27% were given as donations.
Of the 74 high schools in Vermont, 41 (55%) have an EAP in place to respond to SCA. However, of those 41 schools, only 15 (37%) practice and review their EAP at least once annually. There were no reported incidents of AED utilization or sudden cardiac arrest within the past year prior to survey completion.
Discussion
Despite the overall success in cardiac arrest survival rates with the placement of AEDs in public locations, their acquisition by high schools across the country has been slow to materialize. In 2001, only 25% of high schools in the states of Iowa and California had at least 1 AED on school grounds.11 Perhaps one reason that schools may be hesitant to purchase AEDs is because the incidence of SCA in children and adolescents initially was felt to be much lower.12 Previous studies on the prevalence of sudden cardiac death (SCD) in high school athletes in Minnesota estimated the incidence of SCD to be in the range of 1:200,000 per year.12 Newer studies suggest that the annual incidence of SCA in high school student athletes may be even higher, approximately 4.4 in 100,000.7 In the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest for population-based data on pediatric cardiac arrest, research suggests that in the pediatric population (age <20 years), the overall incidence of out-of-hospital cardiac arrest was 8.04 per 100,000 pediatric person-years.2 Comparatively, the frequency in which SCA occurs in adults (age >35 years) appears to be much higher, occurring in roughly 1:1000.1
Over the past decade, the number of high schools across the country implementing AEDs appears to be on the rise. In 2004, 143 of the 400 public high schools in Wisconsin (35%) volunteered to take part in Project ADAM,4 a program designed to educate adults as well as students about SCA in children and adolescents. As part of the program, emphasis on CPR training for graduating seniors was encouraged, and participating schools agreed to place AED(s) on school grounds.3,4 More recently, high schools in Washington and North Carolina have also shown a growing prevalence of AED placement within their schools (54% and 72%, respectively).13,15 In Vermont, 60 of the 74 high schools (81%) reported having at least 1 AED. In addition to the low rates of SCA in the adolescent population, there is also the concern that AEDs are expensive to purchase and place additional stress on already reduced school budgets. In the AEDs in the Schools program, which sought to donate AEDs to high schools in Greater Boston, 27 of 29 schools that received a device as a donation reported a lack of funding as the major deterrent to the purchase of additional devices.9 Yet, after the initial donation, 25 high schools decided to purchase additional AEDs, with most reporting that the only impetus for purchasing them was information they learned regarding the effectiveness of AEDs.9 In this investigation, the majority of AEDs were funded through the school budget (46%), while only 27% were funded through donation. Further studies are needed to determine whether financial resources are an obstacle for those schools in Vermont currently lacking sufficient AEDs.
The 2010 US Census Bureau reported the population in the state of Vermont was 625,741, making it the second least populous state in the United States.16 Of those living in Vermont, 414,480 live in rural Vermont. Fifteen hospitals and 6 long-term care facilities provide health services to residents who are dispersed over an area of 9,250 square miles. Of these institutions, 8 are identified as critical access hospitals, ensuring health care services to those living in rural areas.10,18 Given the rural nature of Vermont and that many high schools remain isolated from health care professionals, it is crucial that school personnel who serve as first responders be prepared to act in the event that an SCA occurs. An integral part of preparation as a first responder means receiving proper training in both CPR as well as formal AED training.7 Given their close proximity to high school athletes at the time of collapse, coaches are often first responders at the time of SCA.
While being trained in CPR and AED utilization is important for those responding to SCA events, that alone is not adequate emergency preparedness. To ensure that precious time is not wasted, schools should have in place an EAP for response to SCA, which should include any potential first responder (teachers, coaches, athletic trainers, students, etc) trained in CPR and AED utilization. In 2007, an interassociation task force released a consensus statement regarding recommendations for emergency preparedness and management of SCA in high school and collegiate athletic programs. In that statement, the essential elements of an EAP should include: formulation of an effective communication system, training responders in CPR and AED use, access to an AED for prompt defibrillation, coordination and integration of on-site responder and AED programs with local EMS responders, and practice of the response plan.6 As our study showed, slightly more than half of the schools in Vermont (55%, 41 of 74) already have established an EAP for SCA. However, of the 41 high schools with EAPs, annual practice and review of these plans was limited to only 15 (37%). This highlights a significant deficiency in the ability of Vermont high schools to plan accordingly for emergency situations and must be a point of emphasis for the future.
In its scientific statement on response to cardiac arrest, selected life-threatening emergencies, and the medical emergency response plan,1 the American Heart Association recommended the implementation of an AED program in schools with at least 1 of the following:
A reasonable probability of the AED use within 5 years of rescuer training and AED placement or an episode of SCA has occurred within the previous 5 years.
There are children or adults at the school who are believed to be at high risk for SCA.
An EMS call-to-shock interval of less than 5 minutes cannot be achieved reliably with conventional EMS services and a collapse-to-shock interval of less than 5 minutes can be achieved reliably (>90% of cases) by training and equipping lay persons to function as first responders.1
Given the rural nature of Vermont, it is likely the call-to-shock interval of less than 5 minutes cannot be achieved reliably. Many schools in Vermont are situated a long distance from the nearest hospital and/or emergency response services, making the implementation of AEDs in schools that much more important. EMS involvement is critical given that they can alert the caller or bystander to the location of the AED as well as offer recommendations on optimal locations for AED placement.
The unique rural demographics of the state of Vermont and the high schools within the state create specific challenges if an SCA were to occur. Long distances to health care facilities and potentially longer EMS response times mean that AED implementation programs within high schools may serve as the only way of achieving life-saving, early defibrillation in rural areas. Proper steps toward emergency preparedness must be taken. While there have been other studies looking at the prevalence and utilization of AEDs in high schools,13,15 response rates have been low and they have been conducted in larger, more urban areas of the country where immediate access to advanced medical care may be more readily available. To our knowledge, this represents the first study looking at the prevalence of AEDs in high schools within a predominantly rural setting and the first that was able to achieve a 100% response rate. This study establishes deficiencies in emergency preparedness for SCA that may be similar in other rural states. Follow-up work is needed to target the 14 schools without AEDs in an effort to achieve AED implementation for all Vermont high schools. The Vermont Principals’ Association Sports Medicine Advisory Committee is aware of our findings, and outreach efforts are underway.
The primary limitation of this study is the inherent limitations of a retrospective survey. Although the study achieved a 100% response rate, recall bias or incomplete information may have been provided. The study was also not designed to investigate the incidence or outcomes of SCA in Vermont high schools. Because of the relatively small number of total high schools, a longer study period would be needed to examine the frequency and outcomes of SCA in this rural state.
Conclusion
In Vermont, the majority of high schools have at least 1 AED on school grounds and approximately half have an EAP in place for SCA. However, only one third of schools practice and review their EAPs on an annual basis, and significant improvement in the establishment of EAPs for sudden cardiac arrest is needed. High schools in Vermont must work to train more individuals in CPR and AED and improve coordination of AED placement with local EMS responders. Further investigation into the barriers that exist for AED acquisition for the remaining Vermont high schools is warranted.
Acknowledgments
The authors thank Bob Johnson of the Vermont Principals’ Association for his help with the distribution of our survey to all Vermont high school athletic directors. We would also like to thank Bruce Beynnon, PhD, and Jon Drezner, MD, for their assistance with the statistical analysis and manuscript, respectively. Funding for this project was provided by the University of Vermont Department of Orthopaedics and Rehabilitation, Burlington, Vermont, USA
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. The American Heart Association in Collaboration with the International Liaison Committee on Resuscitation Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care, part 4: the automated external defibrillator: key link in the chain of survival. Circulation. 2000;102(suppl 8):160-176 [PubMed] [Google Scholar]
- 2. Atkins DL, Everson-Stewart S, Sears GK, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484-1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berger S, Utech L, Hazinski MF. Lay rescuer automated external defibrillator programs for children and adolescents. Pediatr Clin North Am. 2004;51:1463-1478 [DOI] [PubMed] [Google Scholar]
- 4. Berger S, Whitstone BN, Frisbee SJ, et al. Cost-effectiveness of Project ADAM: a project to prevent sudden cardiac death in high school students. Pediatr Cardiol. 2004;25:660-667 [DOI] [PubMed] [Google Scholar]
- 5. Caffrey SL, Willoughby PJ, Pepe PE, et al. Public use of automated external defibrillators. N Engl J Med. 2002;347:1242-1247 [DOI] [PubMed] [Google Scholar]
- 6. Drezner JA, Courson RW, Roberts WO, et al. Inter-association task force recommendations on emergency preparedness and management of sudden cardiac arrest in high school and college athletic programs: a consensus statement. J Athl Train. 2007;42:143-158 [PMC free article] [PubMed] [Google Scholar]
- 7. Drezner JA, Rao AL, Heistand J, et al. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009;120:518-525 [DOI] [PubMed] [Google Scholar]
- 8. Drezner JA, Rogers KJ. Sudden cardiac arrest in intercollegiate athletes: detailed analysis and outcomes of resuscitation in nine cases. Heart Rhythm. 2006;3:755-759 [DOI] [PubMed] [Google Scholar]
- 9. England H, Hoffman C, Hodgman T, et al. Effectiveness of automated external defibrillators in high schools in greater Boston. Am J Cardiol. 2005;95:1484-1486 [DOI] [PubMed] [Google Scholar]
- 10.Flex Monitoring Team: A Performance Monitoring Resource for Critical Access Hospitals, States, and Communities. Available at: http://www.flexmonitoring.org/cahlistRA.cgi?state=Vermont Accessed January 28, 2012
- 11. Jones E, Vijan S, Fendrick AM, et al. Automated external defibrillator deployment in high schools and senior centers. Prehosp Emerg Care. 2005;9:382-385 [DOI] [PubMed] [Google Scholar]
- 12. Maron BJ, Gohman TE, Aeppli D. Prevalence of sudden cardiac death during competitive sports activities in Minnesota high school athletes. J Am Coll Cardiol. 1998;32:1881-1884 [DOI] [PubMed] [Google Scholar]
- 13. Monroe A, Rosenbaum DA, Davis S. Emergency planning for sudden cardiac events in North Carolina high schools. NC Med J. 2009;70:198-204 [PubMed] [Google Scholar]
- 14. Page RL, Joglar JA, Kowal RC, et al. Use of automated external defibrillators by a US airline. N Engl J Med. 2000;343:1210-1216 [DOI] [PubMed] [Google Scholar]
- 15. Rothmier JD, Drezner JA, Harmon KG. Automated external defibrillators in Washington State high schools. Br J Sports Med. 2007;41:301-305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Census Bureau: State and county quick facts Available at: http://quickfacts.census.gov/qfd/states/50000.html Accessed January 28, 2012
- 17. Valenzuela TD, Roe DJ, Nichol G, et al. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206-1209 [DOI] [PubMed] [Google Scholar]
- 18. Vermont Association of Hospitals and Health Systems Available at: http://www.vahhs.org/index.php?option=com_content&view=article&id=53&Itemid=157 Accessed January 28, 2012


