Abstract
Background:
Anterior cruciate ligament (ACL) rupture is a significant injury in National Basketball Association (NBA) players.
Hypotheses:
NBA players undergoing ACL reconstruction (ACLR) have high rates of return to sport (RTS), with RTS the season following surgery, no difference in performance between pre- and postsurgery, and no difference in RTS rate or performance between cases (ACLR) and controls (no ACL tear).
Study Design:
Case-control.
Methods:
NBA players undergoing ACLR were evaluated. Matched controls for age, body mass index (BMI), position, and NBA experience were selected during the same years as those undergoing ACLR. RTS and performance were compared between cases and controls. Paired-sample Student t tests, chi-square, and linear regression analyses were performed for comparison of within- and between-group variables.
Results:
Fifty-eight NBA players underwent ACLR while in the NBA. Mean player age was 25.7 ± 3.5 years. Forty percent of ACL tears occurred in the fourth quarter. Fifty players (86%) RTS in the NBA, and 7 players (12%) RTS in the International Basketball Federation (FIBA) or D-league. Ninety-eight percent of players RTS in the NBA the season following ACLR (11.6 ± 4.1 months from injury). Two players (3.1%) required revision ACLR. Career length following ACLR was 4.3 ± 3.4 years. Performance upon RTS following surgery declined significantly (P < 0.05) regarding games per season; minutes, points, and rebounds per game; and field goal percentage. However, following the index year, controls’ performances declined significantly in games per season; points, rebounds, assists, blocks, and steals per game; and field goal and free throw percentage. Other than games per season, there was no significant difference between cases and controls.
Conclusion:
There is a high RTS rate in the NBA following ACLR. Nearly all players RTS the season following surgery. Performance significantly declined from preinjury level; however, this was not significantly different from controls. ACL re-tear rate was low.
Clinical Relevance:
There is a high RTS rate in the NBA after ACLR, with no difference in performance upon RTS compared with controls.
Keywords: anterior cruciate ligament, ACL, National Basketball Association, NBA, knee injury
Anterior cruciate ligament (ACL) tears are one of the most common knee injuries in both contact and noncontact sports.6 It is estimated that there are 250,000 ACL tears annually,2 over half of which will be reconstructed.7 ACL reconstruction in the general population is regarded as having a high success rate.8 However, there are little data concerning National Basketball Association (NBA) athletes and their rate of return to sports (RTS) and performance upon RTS after an ACL tear. Starkey13 found that the knee is the most prevalent site of orthopaedic trauma in NBA players (13.8%) and accounts for the greatest percentage (26.6%) of time lost each year. Busfield et al3 reported a 2.7% frequency of ACL tears in NBA players between 1994 and 2005. Lost playing time in the NBA due to ACL injury has substantial financial repercussions for both players and the NBA, since the average NBA annual salary is US$6,000,000 and the income of the NBA was $3.817 billion for the 2010-2011 season.1
The primary purposes of this article are to determine: (1) rate of RTS in the NBA following ACL reconstruction, (2) timing of RTS following ACL reconstruction, (3) performance upon RTS following ACL reconstruction, and (4) the difference in RTS and performance between players who sustained an ACL tear and age-, body mass index (BMI)–, sex-, and NBA experience–matched control players. The authors hypothesize that NBA players who sustain an ACL tear and undergo reconstruction will have high rates of RTS, with RTS the season following surgery. They also hypothesize that there will be no difference in performance upon RTS between presurgery and postsurgery; however, performance declines with time. In addition, it is assumed that there will be no difference in rate of RTS or performance between cases (ACL reconstruction) and controls (no ACL tear).
Materials and Methods
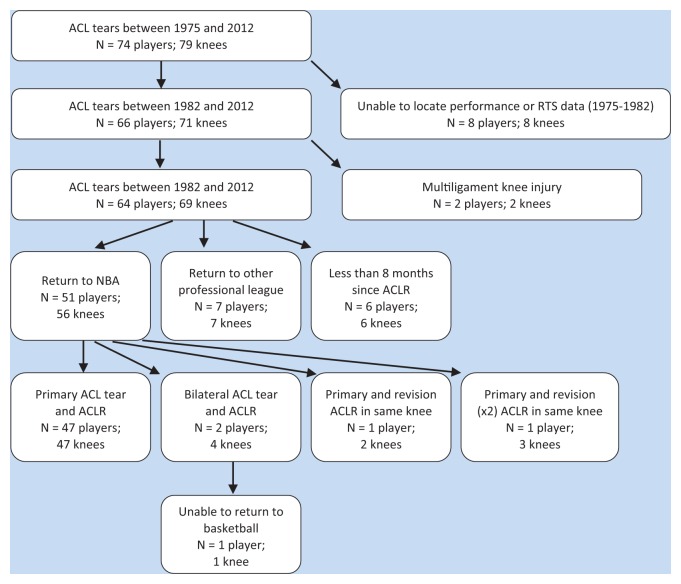
Players in the NBA who sustained an ACL tear and underwent reconstruction between 1975 and 2012 were evaluated. These players were identified through NBA team websites, publically available Internet-based injury reports, player profiles and biographies, and press releases, thus precluding formal institutional review board approval. The search was manually conducted by an orthopaedic surgery resident and a sports medicine fellow, with validation of the findings by the senior author. Searches were performed for all NBA teams and players. Players who sustained ACL tear and underwent ACL reconstruction in the 2011-2012 season were excluded from analysis because they had less than a 1-year opportunity to RTS. All players identified were included in this study as it related to RTS rate. A player was deemed to have RTS in the NBA if he played in any NBA game after surgery. Secondarily, RTS in other leagues were also analyzed: RTS in any game in either the NBA D-league or International Basketball Federation (FIBA) after surgery. A player did not RTS if he failed to meet any of the aforementioned criteria. The subject inclusion criterion consisted of any male NBA player (at least 1 game played in NBA prior to acute ACL tear). Players with concomitant knee injuries, when known, were included (articular cartilage injury, meniscal tear, and medial or lateral collateral ligament tear [but not both at the same time]). Subject exclusion criteria were female players (Women’s NBA [WNBA]), collegiate players (National Collegiate Athletic Association [NCAA]), and bicruciate (ACL and complete posterior cruciate ligament [PCL]) or combined ACL and bicollateral ligament injury. Players in which no RTS or performance data could be found were also excluded (8 players from 1975-1982) (Figure 1).
Figure 1.
Flow chart of selection process for inclusive NBA players within a priori selected years of subjects. The 1 player unable to return to sports (RTS) sustained 2 ACL tears (bilateral) over his NBA career. He was able to RTS in the NBA after the first ACL tear but unable to RTS in the NBA or any professional league after the second ACL tear.
Between 1975 and 2012, there were 79 ACL tears in the NBA (74 players) (Figure 1). Demographic data (age at time of injury, BMI [kg/m2], position [guard, forward, center], months from injury to RTS, side of injury [right vs left], half [first vs second] and quarter [first, second, third, fourth] of play in which the injury occurred, “All-Star” status before and after injury, games played per season, and if the player returned to the NBA the season following the injury) as well as average in-game performance data (minutes per game [MPG], field goal [FG] percentage, free throw [FT] percentage, points per game [PPG], rebounds per game [RPG], steals per game [SPG], blocks per game [BPG], and assists per game [APG]) were collected and analyzed. In-game performance variables were analyzed as an average over the pre- and postinjury course of the players’ careers. In addition, in-game performance variables were analyzed separately in each of the first 5 subsequent seasons the player returned to the NBA following injury.
A control group was selected to compare the data from the study group to that of the rest of the NBA. Controls were matched to cases based on sex, age, BMI, position, and years of experience in the NBA. ACL reconstruction occurred at a mean of 4.1 ± 3.0 years into a player’s career. Thus, player experience in the control group was matched at 4 years into their career. The fifth year allowed for assignment of the “index year” used in other studies of NBA players.4,11 Demographic and in-game performance data were collected and analyzed over the course of their careers before and after the index year (each season analyzed individually and collectively).
Single-variable analyses for all continuous variables (performance measures) within groups were performed using paired-samples Student t tests. One-sample Kolmogorov-Smirnov goodness-of-fit tests for Gaussian data distribution were performed and confirmed normality of all data. Comparisons between case and control groups were made using paired-samples Student t tests. Comparisons were made between cases and controls for survival in the NBA and each individual parameter’s overall mean (all years before and after ACL reconstruction [or index year]) and each individual year (up to 5 years) following ACL reconstruction (or index year in controls). Chi-square analysis was performed for analysis of incidence of ACL tear dependent on in-game timing (quarter, half) with a null hypothesis of no difference between quarters or halves. Linear regression analysis was performed for analysis of the relationship between position and in-game timing of injury (overall quarter injured, time left in quarter). Linear regression was also used for analysis of the relationship between quarter injured and time left in quarter when injury occurred. All statistical analyses were performed using PASW Statistics Student Version 18.0.0 (IBM, Armonk, New York).
Results
Sixty-four NBA players (69 ACL tears) were identified with RTS and performance data (Figure 1). Demographic data of all players undergoing ACL reconstruction are reported in Table 1. With the numbers available, there were no statistically significant differences observed between injury timing based on the quarter in which the injury occurred (P = 0.08). ACL tears occurred at 16.5 ± 11.8 minutes into the players’ game time (based on this information being available from 91% of subjects). Sixty-five percent of tears occurred in the final 6 minutes of the quarter (29% in the final 3 minutes, 21% in the final 2 minutes, 15% in the final minute). No player returned to game play after they sustained injury. No significant relationship (P > 0.05) was demonstrated for position and injury quarter or position and time left in the quarter when the injury occurred. No significant relationship (P > 0.05) was demonstrated between the quarter of the injury and the time left in the quarter when the injury occurred. No significant relationship (P > 0.05) was demonstrated between player position and the quarter in which the injury occurred. Since 1992, there has been at least 1 ACL tear in each regular season (2.5 ± 1.7 per season since 1985) (Figure 2). Graft type for surgical reconstruction was identified only in 5 subjects (2 bone-patellar tendon-bone, 3 hamstring; 4 autograft, 1 allograft). Concurrent knee injuries were identified in only 18 subjects (8 meniscus, 10 medial collateral ligament).
Table 1.
Demographic data of NBA players
| n | |
|---|---|
| Number of players Number of ACL tearsa |
64 69 |
| Mean age, y | 25.7 ± 3.5 |
| Mean body mass index, kg/m2 | 25.0 ± 2.1 |
| Right knee | 35 |
| Left knee | 34 |
| Mean years of experience in NBA prior to ACL tear | 4.1 ± 3.0 |
| Position Guard Forward Center |
29 23 12 |
| Number of All-Stars | 13 (20%) |
| Mean salary prior to ACL tear, US$ millions | 1.73 |
| ACL tear timing In-season game First quarter Second quarter Third quarter Fourth quarter In-season practice Preseason basketball Off-season basketball Non–basketball related |
45 11 (24%) 6 (13%) 10 (22%) 18 (40%) 4 10 8 2 |
Sixty players had a primary ACL tear; 2 players had bilateral nonsimultaneous ACL tears; 1 player had a primary and retear in the same knee; 1 player had a primary and 2 retears in the same knee.
Figure 2.
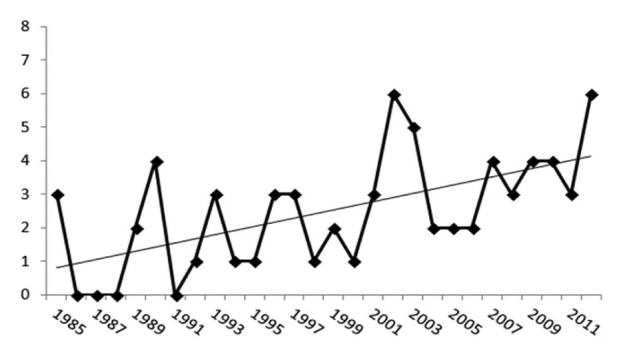
Number of ACL tears per year in the NBA.
Fifty players (55 knees) returned to the NBA after ACL reconstruction (86% rate of return to NBA). Forty-nine players (98%) were able to return the season following injury and reconstruction (mean, 11.6 ± 4.1 months). Length of career following ACL reconstruction was 4.3 ± 3.4 years (range, 0-14 years). However, 13 players (25%) who were able to return to play in the NBA are still currently playing. Seven players (7 knees; 12%) were unable to return to play in the NBA but were able to return to professional basketball in either the FIBA or NBA D-league. Thus, the rate of return to professional basketball overall was 98%. The sole player who did not return to playing professional basketball anywhere tore his contralateral ACL 3 years prior and successfully returned to the NBA after that injury but did not return after his most recent tear. Interestingly, he did return to professional baseball as a pitcher in the minor leagues.
All centers (12/12; 100%) returned to the NBA after ACL reconstruction versus 95% (21/22) of forwards and 71% (17/24) of guards. Those unable to RTS in the NBA played in either the FIBA or NBA D-league. Survival (participation in at least 1 NBA game in the regular season) within the NBA following ACL reconstruction is illustrated in Figure 3. The rate of revision ACL reconstruction was 3.1% (2 players required revision ACL reconstruction for ACL retear [3 knees; 1 player required 2 revisions]). Performance upon RTS following ACL reconstruction (Table 2) was significantly declined in the following parameters (vs presurgery): mean games per season; minutes, points, and rebounds per game; and field goal percentage. In addition, there were significantly fewer players selected for the All-Star team following ACL reconstruction (vs preinjury). Nevertheless, annual salary was significantly increased after ACL reconstruction.
Figure 3.
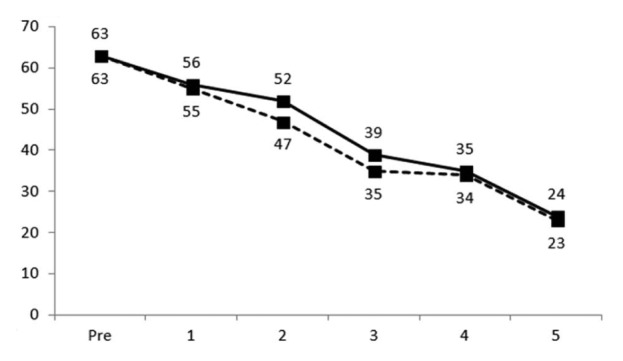
Number of players in the NBA before and after ACL reconstruction (solid line) or post–index year for controls (dashed line) (years 1-5).
Table 2.
Performance comparison before and after ACL reconstructiona
| Before ACL Tear | After ACL Reconstruction | P Value (paired samples Student t test) | |
|---|---|---|---|
| Mean seasons NBA experience | 4.1 ± 3.0 | 5.1 ± 3.1 | NA |
| Mean games played per season | 52.1 ± 22.8 | 44.0 ± 18.7 | 0.04 |
| Mean minutes per game | 22.7 ± 8.6 | 19.1 ± 7.5 | 0.00 |
| Mean points per game | 10.3 ± 5.7 | 7.9 ± 4.3 | 0.00 |
| Mean rebounds per game | 4.1 ± 2.2 | 3.4 ± 2.0 | 0.00 |
| Mean assists per game | 2.0 ± 1.9 | 1.9 ± 2.0 | 0.47 |
| Mean steals per game | 0.8 ± 0.5 | 0.9 ± 1.2 | 0.56 |
| Mean blocks per game | 0.5 ± 0.4 | 0.5 ± 0.7 | 0.27 |
| Mean annual salary, US$ millions | 1.7 ± 1.6 | 3.6 ± 3.0 | < 0.00 |
| Mean field goal percentage | 46.8 ± 6.2 | 44.0 ± 5.1 | 0.01 |
| Mean free throw percentage | 73.4 ± 8.8 | 73.1 ± 9.9 | 0.71 |
| Number of All-Stars | 12 | 4 | 0.02 |
NA, not applicable.
Fifty patients were able to return to the NBA.
The control population (Table 3) was not significantly different from the case population (in comparison of year of ACL reconstruction [cases] and index year [controls]) (P = 0.63 [age], P = 0.24 [BMI], P = 0.72 [seasons NBA experience], P = 0.15 [salary], P = 0.00 [position]). Mean control player age was 25.5 ± 3.4 years. Mean BMI was 24.8 ± 2.2 kg/m2. Mean total number of years played in the NBA was 9.7 ± 3.4 years. Seven control players are still in the NBA. There were 23 forwards, 29 guards, and 12 centers. There were 15 All-Stars in the control group. Performance in the season following the index year in controls (Table 3) was significantly declined for the following parameters: mean games per season; points, rebounds, assists, blocks, and steals per game; and field goal and free throw percentage. In addition, there were significantly fewer All-Star selections following the index year in controls. Nevertheless, annual salary was significantly increased after the index year in controls.
Table 3.
Control population performance before and after index year
| Before Index Season | After Index Season | P Value (paired samples Student t test) | |
|---|---|---|---|
| Mean seasons NBA experience | 4.0 ± 0.0 | 5.1 ± 3.4 | NA |
| Mean games played per season | 62.6 ± 17.1 | 54.7 ± 22.9 | 0.02 |
| Mean minutes per game | 23.8 ± 8.5 | 19.9 ± 7.8 | <0.00 |
| Mean points per game | 10.3 ± 6.0 | 7.5 ± 4.5 | <0.00 |
| Mean rebounds/game | 4.3 ± 2.7 | 3.3 ± 2.0 | <0.00 |
| Mean assists/game | 2.4 ± 2.0 | 2.0 ± 1.9 | <0.00 |
| Mean steals/game | 1.0 ± 1.0 | 0.7 ± 0.5 | 0.01 |
| Mean blocks per game | 0.6 ± 0.7 | 0.4 ± 0.4 | <0.00 |
| Mean annual salary, US$ millions | 1.3 ± 0.9 | 3.2 ± 3.5 | <0.00 |
| Mean field goal percentage | 44.8 ± 9.1 | 42.2 ± 6.3 | 0.03 |
| Mean free throw percentage | 74.5 ± 8.3 | 70.3 ± 12.1 | <0.00 |
| Number of All-Stars | 15 | 5 | 0.02 |
NA, not applicable.
There was no significant difference in survival in the NBA (playing at least 1 game per season) between preoperative (or pre–index year in controls) and postoperative years 1 through 5 (Figure 3). Following ACL reconstruction (or index year [controls]), there were several statistically significant differences identified between cases and controls (Tables 2, 3 and Appendices 1 to 5, available at http://sph.sagepub.com/content/suppl).
Discussion
This case-control study of 64 NBA players who underwent 69 ACL reconstructions has demonstrated a high rate of return to play in professional basketball (98%) and the NBA (86%), with nearly all players returning the season following surgery. Although performance declined following surgery, the same performance parameters also significantly declined in controls. Survival in the NBA and performance upon RTS in the NBA was not significantly different between cases and controls. The rate of revision ACL reconstruction for ACL retear was low (3.1%). All but 1 study hypothesis was confirmed (the authors hypothesized no significant difference between pre- and post-ACL reconstruction, although 1 was observed).
ACL tears are serious injuries that, if not reconstructed and rehabilitated properly, can jeopardize an NBA player’s career.5 Prior studies have shown both favorable9,10 and unfavorable outcomes3 after ACL reconstruction with regard to patient satisfaction, specifically in athletes. Although the current study observed that ACL tears have an approximate incidence of 2.54 per year in NBA players, there have been little published data on the RTS and overall performance of NBA players after an ACL reconstruction. Namdari et al12 evaluated performance in WNBA athletes who tore their ACL and found 78% returned to play in the WNBA, with only slight decreases in field goal percentage and steals per game compared with their preinjury levels. Namdari et al11 and Cerynik et al4 evaluated the outcomes of NBA players after microfracture and found a 67% and 79% return to the NBA, respectively. Both studies showed a decrease in minutes per game postinjury. Busfield et al3 examined 27 NBA players who tore their ACLs and found a 78% return to the NBA, similar to the findings of the current study (80%). The current study further identified an additional 7 players who RTS in other professional leagues, increasing the overall RTS rate. Busfield et al3 also found statistically significant decreases in field goal percentage after the players returned from their ACL injury, concurrent with the findings of the present investigation.
This study demonstrated that 40% of ACL tears occurred in the fourth quarter and nearly two-thirds (62%) in the second half. Although the difference between quarters and halves was not statistically significant (P > 0.05), this potentially implicates the role of fatigue in timing of ACL tears in the NBA. This fact may affect how coaches decide when to take their starting players out toward the end of games when their team is far ahead. In addition, the player’s position may have a role in injury incidence. Further, 65% (45/69) of ACL tears occurred during an in-season game.
Although this study is a comprehensive analysis of RTS in the NBA and performance upon RTS, there are limitations. First, there may have been NBA players whose ACL tears were not discovered because of the search methodology. Although both an orthopaedic surgery resident and a fellow in a sports medicine orthopaedic program conducted separate searches to identify all possible NBA players for inclusion, some may have been omitted due to electronic news reporting at the time of the injury. However, Busfield et al3 utilized the National Basketball Athletic Trainers Association database of injuries in NBA athletes. In comparison with the current study (see Figure 2) and the enrollment period utilized by Busfield et al, the number of ACL tears was exactly the same, thus assuring the same level of accuracy of the current investigation’s search methodology. Further, the authors are unable to comment on player satisfaction or personal perception of knee pain, function, and stability in comparison with preinjury. Nearly all surgical technique demographics (single- vs double-bundle, 1-incision vs 2-incision, bone-patellar tendon-bone vs hamstring, autograft vs allograft, transtibial vs accessory anteromedial femoral tunnel drilling, meniscal and articular cartilage concomitant injury) were unavailable in publicly accessible sources. In addition, postoperative physical examination (eg, Lachman, pivot-shift), instrumented laxity (KT-1000 arthrometer), and imaging (radiographic assessment of degenerative changes, MRI assessment of meniscal and/or chondral damage) outcomes were unavailable. The date of injury was easily identified in the search methodology. However, the date of surgery was seldom identified, thus potentially limiting the applicability of the timing of RTS. Additionally, the nature of progression of rehabilitation postoperatively was unavailable. Even though some players were unable to return to play in the NBA following ACL reconstruction, the inability to return cannot solely be attributed to the ACL injury and surgery, as other confounders inevitably coexist. The inability to reliably obtain these confounders demonstrates the need for a comprehensive NBA electronic medical record that tracks variables that might help predict timing, risk of reinjury, and performance following ACL reconstruction. Further, although all performance-based measures were used to compare pre- and postoperative outcomes and between cases and controls, other immeasurable intangibles (team leadership, teammate motivation, etc) cannot be assessed for relationships. Manual selection of the control group was matched by sex, age, BMI, position, and experience in the NBA. Despite this, other parameters (eg, performance, points, rebounds, assists per game) could have been utilized for control group matching (not just physical parameters, but also skill-based parameters). Although one may claim that experience in the NBA may underscore a player’s skill, performance-based matching may provide a more apt control group. Further, a strong confounder is the financial motivation that incentivizes these highly talented and gifted athletes to return to professional basketball.
Conclusion
There is a high rate of RTS in the NBA following ACL reconstruction. Nearly all players RTS the season following surgery. Guards have the most difficult time with RTS, and centers have the most predictable outcomes. In-game performance significantly declined from preinjury levels; however, this was not significantly different from a control population. The rate of ACL retear is low.
Footnotes
The following authors declared potential conflicts of interest: Bernard R. Bach, Jr, MD, received royalties from SLACK Inc. and payment for work from Arthrex, Smith and Nephew, Ossur, and Linvatec; Brian Forsythe, MD, has received payment for work from Arthrex, Smith and Nephew, Ossur, and Linvatec; and Brian J. Cole, MD, MBA, is a board member for AAOS Board, American Journal of Orthopedics, American Journal of Sports Medicine, Cartilage, Educational Committee AANA, Elsevier, International Committee AANA, Journal of Bone and Joint Surgery - American, and Journal of Shoulder and Elbow Surgery; a consultant for Allosource, Arthrex, Inc, Biomimetic, Carticept, DePuy, A Johnson & Johnson Company, and Zimmer; received payment for lectures from Genzyme; received royalties from Arthrex, Inc, DJ Orthopaedics and Elsevier; and received payment for work from Arthrex, Ossur, Smith and Nephew, and Linvatec.
References
- 1. Aschburner S. NBA’s “average” salary—$5.15M—a trendy, touchy subject NBA Media Ventures, LLC. http://www.nba.com/2011/news/features/steve_aschburner/08/19/average-salary/index.html Published August 19, 2011. Accessed December 15, 2012
- 2. Barrera Oro F, Sikka RS, Wolters B, et al. Autograft versus allograft: an economic cost comparison of anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1219-1225 [DOI] [PubMed] [Google Scholar]
- 3. Busfield BT, Kharrazi FD, Starkey C, Lombardo SJ, Seegmiller J. Performance outcomes of anterior cruciate ligament reconstruction in the National Basketball Association. Arthroscopy. 2009;25:825-830 [DOI] [PubMed] [Google Scholar]
- 4. Cerynik D, Lewullis G, Joves B, Palmer M, Tom J. Outcomes of microfracture in professional basketball players. Knee Surg Sports Traumatol Arthrosc. 2009;17:1135-1139 [DOI] [PubMed] [Google Scholar]
- 5. Cheatham SA, Johnson DL. Anatomic revision ACL reconstruction. Sports Med Arthrosc. 2010;18:33-39 [DOI] [PubMed] [Google Scholar]
- 6. DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14:218-224 [DOI] [PubMed] [Google Scholar]
- 7. Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1997;79:1556-1576 [DOI] [PubMed] [Google Scholar]
- 8. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756-1769 [DOI] [PubMed] [Google Scholar]
- 9. McAllister DR, Tsai AM, Dragoo JL, et al. Knee function after anterior cruciate ligament injury in elite collegiate athletes. Am J Sports Med. 2003;31:560-563 [DOI] [PubMed] [Google Scholar]
- 10. Mitsou A, Vallianatos P. Reconstruction of the anterior cruciate ligament using a patellar tendon autograft. A long term follow up. Int Orthop. 1996;20:285-289 [DOI] [PubMed] [Google Scholar]
- 11. Namdari S, Baldwin K, Anakwenze O, Park M, Huffman G, Sennett B. Results and performance after microfracture in National Basketball Association Athletes. Am J Sports Med. 2009;37:943-948 [DOI] [PubMed] [Google Scholar]
- 12. Namdari S, Scott KB, Milby A, Baldwin K, Lee GC. Athletic performance after ACL reconstruction in the Women’s National Basketball Association. Phys Sportsmed. 2011;39:36-41 [DOI] [PubMed] [Google Scholar]
- 13. Starkey C. Injuries and illnesses in the national basketball association: a 10-year perspective. J Athl Train. 2000;35:161-167 [PMC free article] [PubMed] [Google Scholar]