Abstract
Background
Tailored, web-assisted interventions can reach many smokers. Content from other smokers (peers) through crowdsourcing could enhance relevance.
Purpose
To evaluate whether peers can generate tailored messages encouraging other smokers to use a web-assisted tobacco intervention (Decide2Quit.org).
Methods
Phase 1: In 2009, smokers wrote messages in response to scenarios for peer advice. These smoker-to-smoker (S2S) messages were coded to identify themes. Phase 2: resulting S2S messages, and comparison expert messages, were then emailed to newly registered smokers. In 2012, subsequent Decide2Quit.org visits following S2S or expert-written e-mails were compared.
Results
Phase 1: a total of 39 smokers produced 2886 messages (message themes: attitudes and expectations, improvements in quality of life, seeking help, and behavioral strategies). For not-ready-to-quit scenarios, S2S messages focused more on expectations around a quit attempt and how quitting would change an individual’s quality of life. In contrast, for ready-to-quit scenarios, S2S messages focused on behavioral strategies for quitting. Phase 2: In multivariable analysis, S2S messages were more likely to generate a return visit (OR=2.03, 95% CI=1.74, 2.35), compared to expert messages. A significant effect modification of this association was found, by time-from-registration and message codes (both interaction terms p<0.01). In stratified analyses, S2S codes that were related more to “social” and “real-life” aspects of smoking were driving the main association of S2S and increased return visits.
Conclusions
S2S peer messages that increased longitudinal engagement in a web-assisted tobacco intervention were successfully collected and delivered. S2S messages expanded beyond the biomedical model to enhance relevance of messages.
Introduction
Widely accessible public health resources such as computer-tailored web-assisted tobacco interventions have the potential to improve smoking-cessation rates.1–6 Computer-tailored communication systems assess an individual’s unique background, needs, interests, and concerns in order to relay a personalized message to motivate behavior change.3,7,8 By directly addressing the specific needs of an individual, the tailored message can be more personally informative and motivating.7,9 Tailored messages show promise in helping participants reach behavior change goals,9–15 and use of online, tailored, quit-smoking tools is associated with 6-month smoking-cessation abstinence.16 Tailored e-mails can encourage website use,17 are economical, and can cover a broad geographic area.18
Although theoretically sound,19–21 these expert-written tailoring systems may not account for sociocultural concepts that have intrinsic importance to the targeted population, limiting their relevance to the audience.22–26 Expert-written messages may also omit some topics relevant to smokers and may be written in a form or use wording that poorly reflects the real-world experiences of the smokers engaged in the intervention. Messages “in a smoker’s own words” may be more persuasive to other smokers because they reflect shared experiences, allowing smokers to more easily identify with message content.
Peer-to-peer communication is increasingly recognized as an important form of persuasive communication. Recent interventions have used patient storytelling or narrative communication effectively to motivate behavior change.27–30 Peer-to-peer communication does map to important constructs within Social Cognitive Theory (SCT) (i.e., role modeling).31 SCT argues that an individual’s social and physical environments; observational learning (i.e., role modeling); and behavioral capabilities (i.e., skills) can influence behavioral change.31 Peer-to-peer communication can exemplify all of these factors by illustrating the difficulties, skills, and strategies needed for smoking cessation. Peer-to-peer communication also enhances homophily, a feeling of similarity between the message writer and the message reader.
Crowdsourcing, a new web-based business model emerging in 200632 has been described as a way to “…harness the creative solutions of a distributed network of individuals through what amounts to an open call for proposals.”33 By drawing on the collective wisdom of a group of people, more varied and applicable information can be collected as compared to the output of a small group of experts. To date, this method has predominately been used in the business sector in producing products (e.g., commercials, T-shirt designs, solutions to research and development problems) that vastly outperform those developed by industry professionals.33 Health-related uses of crowdsourcing have been used on websites such as “PatientsLikeMe,” which allows registered users to link to other patients with similar medical profiles.34
This article evaluates the feasibility of crowdsourcing message-writing, and describes the success of peer-written communication solicitation. Short smoker-to-smoker (S2S) messages were solicited directly from those who, in the preceding 6 months, had successfully quit smoking (former smoker) or had at least one quit attempt (current smoker with a recent quit attempt). It was anticipated that peer message writers would change the messages they wrote (tailor their advice) based on the framing of various situations presented about attempts to quit smoking (scenarios). These peer-written messages were incorporated into a tailored, automated e-mail messaging system used in a web-assisted tobacco intervention. The influence that S2S messages had on intervention participation was evaluated.
Methods
Study Design
The S2S study had two phases: (1) S2S message solicitation, wherein peer message writers were recruited (former smokers and smokers with a recent quit attempt) to write messages by responding to various scenarios; and (2) message evaluation—a within-subject comparison was conducted of subsequent use of the web-assisted tobacco intervention Decide2Quit.org35,36 when receiving a S2S peer-written message compared to when receiving an expert-written message (Figure 1). The protocol was approved by the IRB at the University of Massachusetts Medical School and the University of Alabama at Birmingham.
Figure 1.
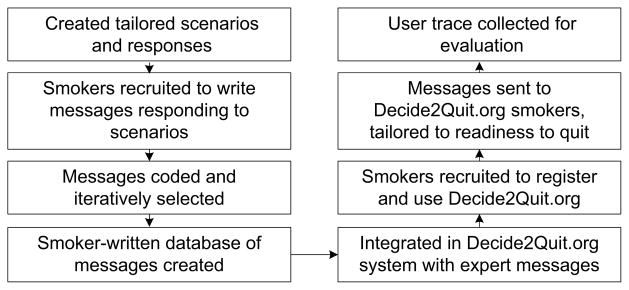
Flowchart of message development and evaluation process
Decide2Quit.org: A Web-Assisted Tobacco Intervention
Decide2Quit.org includes information about quitting smoking, secure asynchronous messaging with a Certified Tobacco Treatment Specialist, an online support group, and automated motivational e-mails tailored to each smoker.35,36 Decide2Quit.org is currently being evaluated within two large RCTs. QUIT-PRIMO (Quality Improvement in Tobacco Provider Referrals & Internet-delivered Microsystem Optimization) is a study of Decide2Quit.org in primary care medical practices; the HI-QUIT (Hygienists to Internet Quality Improvement in Tobacco) study is a similar study in dental practices. The protocol for these studies has been previously published.36 The S2S motivational e-mail messages and the expert-written control messages were deployed within the context of these interventions.
Smoker-to-Smoker Message Solicitation (Phase 1)
For S2S Phase 1 (message solicitation), smokers were recruited through advertisements on Google AdWords.37 After clicking on the advertisement, eligible smokers (those aged >19 years) were directed to an online informed consent before agreeing to participate. Participation included a short survey collecting demographics and smoking behavior. Successful quitters (former smokers) were defined as anyone who has smoked cigarettes or cigars in their lifetime but has not had at least one puff in the past 7 days. Current smokers with a recent quit attempt were defined as smoking at least one puff of a cigarette or cigar in the past 7 days but reporting having at least one serious quit attempt lasting 24 hours in the past 6 months. Current smokers were included because even though the participant had not successfully quit smoking long term, the experiences gained from any quit attempt can still be valuable to other smokers. Message writers’ e-mail and telephone numbers were collected for follow-up contact to confirm an address for reimbursement.
The scenarios varied on readiness to quit smoking (ready to quit or not ready to quit); age; and gender (Appendix A, available online at www.ajpmonline.org). Each individual responded to four scenarios: two matched to the peer message writer’s age and gender and two randomly generated. The ready-to-quit scenarios addressed advice and experiences that might be useful to other smokers before, on, and after the quit date. The not-ready-to-quit scenarios addressed reasons, rewards, risks, roadblocks to quitting,38 and commitment to change. Participants received a $50 gift card for their time.
Smoker -to-Smoker Message Coding of Peer Messages (Phase 1)
Two certified tobacco treatment specialists reviewed the messages. Example messages included: “It helped a lot to set up milestones like I won’t smoke while I do this one thing” or “Keep in mind that cravings are temporary and will pass.” To develop a coding schema, a subset of messages was reviewed by both coders together. Additional messages were reviewed until the coders began to experience theme saturation. All messages were then reviewed once independently by both coders, and they then met to resolve any discrepancies. Multiple codes could be used for each message.
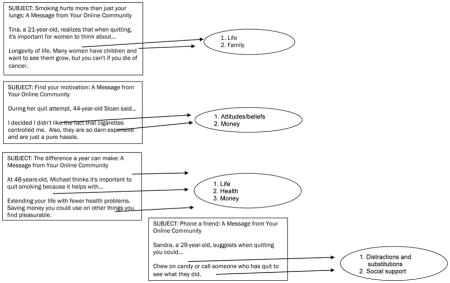
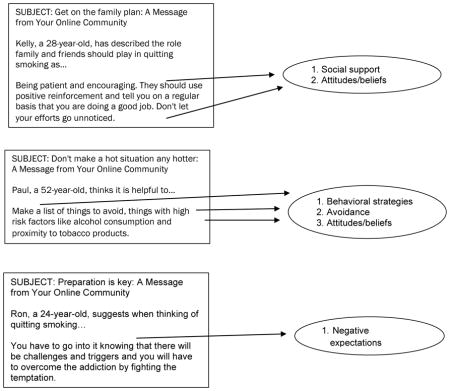
Smoker-to-smoker messages were selected for Phase 2 using specific criteria: whether the message could be directly quoted, the behavioral content of the message, and whether the message followed the key concepts in SCT (Appendix B, available online at www.ajpmonline.org). Directly quotable means the message was written in sentence form and contained a clear, detailed message targeted to the scenario. For example, “Focus on how great it is that you can do the same things without smoking [and] that you don’t need to smoke to enjoy your friends” meets all three inclusion criteria. However, “think about why you want to quit” is quotable but does not contain strong behavioral content, or personal experiences on how to overcome this challenge. A final iterative group review with behaviorists, physicians, and nurses ensured that the messages were appropriate and relevant to the intervention goals.
Expert-Written Messages: The Comparison Control
For Decide2Quit.org, 194 brief, expert-written (behaviorists, physicians, nurses), tailored e-mail messages encouraging cessation were developed through an iterative expert group review process. Expert message e-mail content was guided by current guidelines38 and SCT.31 The current guideline provided evidence-based content on successful cessation strategies. SCT, which incorporates vicarious learning and verbal persuasion, guided the expert messages. Messages reflected theoretic determinants of quitting, such as positive outcome expectations and small goals to enhance self-efficacy.31
Expert and Smoker-to-Smoker Message Evaluation (Phase 2)
When registering at Decide2Quit.org, smokers consented and completed an assessment of smoking behaviors and readiness to quit. Smokers then received a series of automated e-mail messages—both the S2S messages and the expert-written ones—that were tailored to the readiness-to -quit data that the smoker entered when registering. The study was conducted between June 2010 and June 2011. Each message was sent only one time per smoker.
Readiness to quit was assessed.39 The readiness question consisted of five options: I am not thinking of quitting (precontemplation); I am thinking of quitting (contemplation); I have set a quit date (preparation); I quit today (action); and I have already quit (maintenance). In the first week of registration, four messages were sent to the user (two of each). Every week thereafter, one expert and one smoker-to-smoker message was sent. Messages were sent alternately. In this design, each smoker serves as their own control, as on some days they received S2S messages, and some days they received the comparison control expert-written messages. The e-mail message subject indicated whether the message was expert-written or smoker-written. The subject line of the expert-written messages was “A message from Decide2Quit online smoking cessation system,” whereas the smoker-written message subject line was “A Message from Your Online Community.”
Data Analysis
For Phase 1, to verify that peer message writers would change (tailor) their advice based on the scenarios, the range and frequency of the S2S message codes were assessed and compared across scenario type (ready-to-quit versus not-ready-to-quit scenarios). For Phase 2, to evaluate whether S2S-written tailored messages resulted in greater subsequent website participation, number of visits occurring after S2S message e-mails was compared to visits following expert-written e-mails. Visits that did not occur in relation to a message were excluded. Each smoker received expert messages and peer messages. Thus, each participant serves as their own control.
The analysis was conducted at the message level (within-in participant). As messages were clustered within patients and the unit of observation was at the patient level, a modeling approach appropriate to hierarchic data was used. The primary dependent variable was visiting the website on the day a message was sent. The independent variable was type of message sent (S2S message or expert-written); adjusting for the smoker’s demographic variables (age, gender); baseline readiness to quit (not thinking of quitting, thinking of quitting, have set a quit date, and quit); routine use of the Internet (e.g., e-mail, gaming); and the difference between the message date and the patient’s registration date (time to message).
Common approaches to clustered data include generalized estimating equations and generalized linear mixed models.40,41 As the number of messages (observations) per patient varied, a generalized linear mixed model approach with adaptive quadrature and robust variance estimates with a logit link for binary outcomes was used, as this approach is more robust to variations in intraclass correlation coefficient and cluster size.40,41 Analyses were implemented using the Generalized Linear Latent and Mixed Models (GLLAMM) procedure in STATA.
In addition to modeling the overall effect of the S2S messages, several hypothesis-generating sensitivity analyses were conducted. First, an interaction of the effect of S2S messages and time-from-registration by adding an interaction term to the main model was assessed. Models stratified by specific time periods (days: 0–14, 15–30, 30–90, 90–120, and >120) were then created. Similarly, to see if the S2S varied by content, an interaction between S2S message effect and individual content codes was investigated.
Results
Results of Google Advertising and Participants
The Google advertisements were available from March 10–June 4, 2009. During this time, 411 Google users clicked through to the survey. From the 411 users who viewed the study consent, 39 participants who, in the past 6 months, had successfully quit smoking or were current smokers with a recent quit attempt, completed the message-solicitation scenarios (Table 1).
Table 1.
Demographic characteristics of Google Ad message writers
| N = 39 | % | |
|---|---|---|
| Gender | ||
| Male | 13 | 33.3 |
| Female | 26 | 66.7 |
| Age, years | ||
| 19–35 | 16 | 41.0 |
| 36–50 | 15 | 38.5 |
| 51–64 | 7 | 18.0 |
| 65+ | 1 | 2.6 |
| Race | ||
| White | 32 | 82.1 |
| African-American | 4 | 10.3 |
| Native Hawaiian or Other | 1 | 2.6 |
| Italian/White | 1 | 2.6 |
| Refused | 1 | 2.6 |
| Smoker | 32 | 82.1 |
| Former smoker | 7 | 18 |
Peer-to-Peer Messages Solicited
A total of 2886 messages (1404 messages in response to a not-ready-to-quit scenario, and 1482 messages in response to a ready to quit scenario) were collected from the 39 message writers. Each message had a mean of 1.2 codes (SD=0.68); an average of 7.6 words (SD=7.2); and an average Flesh-Kincaid grade level of 4.5. Codes were grouped into four larger themes (Table 2): attitudes and expectations (e.g., secondhand smoke is harmful to others, I want to quit for my children); improvements in quality of life (e.g., live longer, senses improve); seeking help (e.g., talking to doctors, online research); and behavioral strategies (e.g., avoidance, substitution, distraction).
Table 2.
Coding of peer- and expert-written messages by readiness to quit smoking, %a
| Ready to quit scenario N= 1,482 | Not ready to quit scenario N = 1,404 | p-value | |
|---|---|---|---|
| Behavioral Strategies | 57.5 | 25.6 | |
| Behaviors (e.g., remove triggers) | 22.1 | 12.2 | <0.05 |
| Distraction/Substitution (e.g., chew gum) | 23.8 | 5.8 | <0.05 |
| Avoidance (e.g., stay away from smokers) | 11.6 | 7.6 | <0.05 |
| Seeking Help | 20.3 | 17.7 | |
| Talk to Doctor (e.g., medicine safety) | 0.9 | 1.2 | 0.49 |
| Seek Help (e.g., group therapy) | 1.7 | 3.4 | <0.05 |
| Treatments (e.g., Rx, NRT) | 3.3 | 1.2 | <0.05 |
| Social Support (e.g., quit with a friend) | 13.9 | 9.3 | <0.05 |
| Online Research (e.g., search for tips) | 0.5 | 2.6 | <0.05 |
| Attitudes and Expectations | 15.6 | 37.9 | |
| Positive Expectations (e.g., more energy) | 1.6 | 6.3 | <0.05 |
| Negative Expectations (e.g., initial cough) | 0.5 | 18.1 | <0.05 |
| Attitudes/Beliefs (e.g., commit to change) | 10.9 | 7.0 | <0.05 |
| Family (e.g., quit for child) | 2.4 | 3.1 | 0.25 |
| 2nd hand smoke (e.g., harm to others) | 0.2 | 3.4 | <0.05 |
| Improvements in Quality of Life | 22.6 | 36.5 | |
| Life (e.g., live longer) | 2.8 | 4.1 | 0.06 |
| Breathing (e.g., breathe better) | 0.6 | 2.6 | <0.05 |
| Health (e.g., no lung cancer) | 8.8 | 13.4 | <0.05 |
| Sense of taste/smell (e.g., food tastes better) | 0.5 | 1.1 | 0.08 |
| Aesthetics or Appearance (e.g., white teeth) | 2.6 | 4.2 | 0.02 |
| Money (e.g., save more) | 7.3 | 11.1 | <0.05 |
Message codes not exclusive. Multiple codes per messages was allowed, with each message having an average of 1.2 codes (SD = 0.68).
Messages written to someone ready to quit differed from those given to someone not ready to quit (Table 2). For those not ready to quit, the messages focused more on expectations around a quit attempt and how quitting would change an individual’s quality of life (37.9% and 36.5% of messages from those not ready to quit, respectively). In contrast, for those ready to quit, the messages focused predominantly on behavioral strategies to use when quitting (57.6% of messages from those not ready to quit). Of note, one of the largest variations occurred with the mention of negative expectations, (e.g., “You have to go into it knowing there will be challenges and triggers…that you will have to overcome the addiction by fighting the temptation,”) present in 18% of messages in response to those not ready to quit, but nearly absent when writing to those ready to quit.
Many S2S messages were not directly quotable. Examples of messages that are not directly quotable are “breathe better” or “live longer.” Although these messages were important to quantify the frequency of themes mentioned by message writers, the wording was not of sufficient strength and clarity to include in an intervention to motivate cessation. Based on the review, 3.9% of the messages were chosen as directly quotable and eligible for inclusion in the intervention (2.97% were advice to someone ready to quit and 0.93% were advice to someone not ready to quit.) In all, 57 smoker-written messages were selected for Phase 2.
Website Visit Comparison
A total of 655 smokers participated in the Decide2Quit.org study website. The length of time each smoker participated was different (M=179.80 days, SD=106.83, median=171). The mean number of expert messages sent per smoker was 26 (SD=15), while the mean number of S2S messages sent was 14 (SD=7). A total of 1044 return visits occurred. Of these visits, 405 (38.8%) occurred on days when no messages were sent, and 639 (61.2%) occurred on days when the smoker received automated, tailored e-mail messages. The mean proportion of days per smoker when messages (either a peer or an expert) were sent out was 32 (SD=13).
A total of 17,169 expert messages were sent, and 1.75% of messages were followed by return visits. In contrast, 9028 S2S messages were sent, and 3.70% of S2S messages were followed by return visits. This doubling of return visits was significant (p<0.05). In multivariable analysis, S2S messages were more likely to generate a return visit (OR=2.03, 95% CI=1.74, 2.35), compared with the expert-written messages. The effect remained after adjusting for time-from-registration and for age, gender, baseline smoking status, and routine use of the Internet (e.g., e-mail, gaming). There were significant interactions of the effect of the message with the time-from-registration (p<0 .001). It was found that the advantage of peer versus expert messages was accentuated over time in a dose-dependent time. As the time interval from registration increased (e.g., 0–30, 30–90) the peer message effect increased (Table 3). There were also significant interactions of the effect of the message with the message codes (p <0.001). Comparing codes in expert and S2S messages, expert messages that resulted in visits had more “biomedical” codes (avoidance, behavioral strategies, health), while peer messages had more “social” and “real-life” codes (expectations, money, quality of life, attitudes and friends; Figure 2).
Table 3.
Effect Messages had on Return Visits Stratified by Time Periods
| Time period, days | Proportion of Messages Triggering Return Visits | Unadjusted OR (95% CI) | |
|---|---|---|---|
| S2S | Expert | ||
| 0–14 | 6.85 | 8.07 | 0.84 (0.63, 1.12) |
| 15–30 | 2.66 | 2.36 | 1.13 (0.69, 1.85) |
| 31–90 | 1.13 | 0.95 | 1.19 (0.80, 1.78) |
| 91–120 | 5.43 | 1.60 | 3.55 (1.83, 6.89) |
| > 120 | 9.69 | 3.11 | 3.34 (2.52, 4.42) |
S2S, smoker-to-smoker
Figure 2.
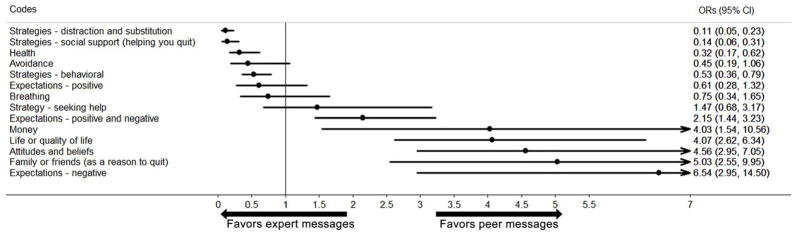
Forest Plot of the Effect of S2S and Expert Message Code on Return Visits
S2S, smoker-to-smoker
Discussion
The study demonstrated that peers can generate tailored messages that map to important constructs within behavioral theories. Moreover, the study demonstrated a strong association between delivering these S2S messages and a key engagement endpoint in the study (participation in the web-assisted tobacco intervention). Smokers varied the content they wrote in the messages in response to the scenarios. The resulting content aligned with the behavioral concepts of SCT. Not all S2S-generated messages created were directly usable. However, the volume of messages (2886 S2S messages) allowed selection of a subset of S2S messages on a variety of motivational themes. The S2S study is the first to “crowdsource” the writing of tailored motivational messages for a web-assisted tobacco intervention.
As maintaining engagement in web-assisted tobacco interventions is challenging, yet critical to intervention fidelity and subsequent cessation, these results provide interesting insights for future directions. In particular, they highlight how persuasive messages may maintain engagement, especially if the content is deemed by smokers to be realistic and authentic to their experiences and struggles with quitting. Smoking-cessation outcomes for web-assisted tobacco interventions have been associated with the number of visits,42 number of website sections viewed43 and amount of time spent on the website.44 These persuasive messages may increase the likelihood of these outcomes.
As demonstrated, Decide2Quit.org engagement was limited on days without pushed e-mail messages. The majority of return visits (61.3%) occurred on days messages were sent, even though these were a minority of the total days. In the Phase 2 evaluation, the peer-written S2S messages resulted in an increased number of visits as compared with expert messages. In the initial time periods, the increase was marginal. However, after 90 days, there was a noticeable difference between the two in their ability to trigger return visits. Longitudinal engagement of users in a web-assisted intervention is a huge challenge. Developing additional peer messages may be one strategy that could be used. This ability of the S2S messages to improve longitudinal engagement may be due to the S2S messages being “in a smoker’s own words” and reflecting shared or real-world experiences of smokers and allowing other smokers to more easily identify with the message content.
To test this further, D2Q return visits were assessed by the motivational content codes. Interestingly, the codes seemed to divide in what is favored in S2S and expert messages. Codes that were favored in S2S messages included expectations, money, quality of life, attitudes and friends. All of these codes represent the more “social” and “real-life” aspects of smoking cessation and represent the day-to-day issues associated with smoking cessation and the social and interpersonal influences on quitting. Such codes align with the concepts of SCT in which the physical and social environment influences individual behavior change.
These results indicate that peer-generated content reflects these important concepts and suggest that such content may increase engagement with smoking-cessation efforts more than other types of content. Comparatively, the motivational content codes favored more in experts included the more “biomedical” codes of strategies (e.g., avoidance) and health. It suggests that peer-written content reflecting more the social interactions and aspects of quitting could better enhance the impact of the web-assisted tobacco intervention on subsequent smoking cessation. Although additional research may be needed, this provides important insights into future ways to communicate about smoking cessation to smokers and the message content components that may be more successful.
Limitations
This study has limitations including that peer-written messages were of mixed quality with some mapping better to key behavioral concepts than others. Future studies could benefit from recruiting peer writers from various sources, such as the local community or even social networks on the Internet. This could allow for a larger sample size and more variation in messages collected. By recruiting from various resources, another limitation of this study may be addressed. The study cohort was small and predominately white (82.1%) and this likely has an influence on the peer-written messages in that they may not be generalizable to all races and ethnicities. In addition, the actual messages were likely influenced by the framing of the scenarios. Inclusion of additional scenarios or reframing of the current scenarios could lead to soliciting a larger variety of directly quotable messages. Several messages that were not directly quotable because of their wording were excluded. Providing clearer instructions to message writers might have averted this issue.
Another limitation was that fewer peer-written S2S messages were sent to smokers than expert messages, mainly because there had been fewer peer-written messages selected to send. As this resulted in more opportunities to participate after expert messages, this unbalance should bias the results towards the expert messages, and the observed effect of the peer-written messages may be underestimated. Additionally, the analyses assessing website participation by visits on days the messages were sent may not account for a delayed effect of later website visits. Thus, the remarkable effect of participation following S2S and expert messages may actually be underestimated.
Conclusion
Additional research is needed to refine methods for directly collecting intervention content from the target audience and to evaluate the impact of peer-generated content versus expert-generated content on cessation outcomes.
Acknowledgments
Funding for these studies was received from the National Cancer Institute, grant R01 CA129091, and the National Institute of Dental and Craniofacial Research, grants U01 DE16746, U01 DE16747, and U19 DE22516.
Appendix A. QUITPROMO Scenarios
Scenarios
READY
-
1
Phillip is a young man who is ready to quit smoking.
-
2
Daphne is a young woman who is ready to quit smoking.
-
3
Henry is a middle-aged man who is ready to quit smoking.
-
4
Leslie is a middle-aged woman who is ready to quit smoking.
NOT READY
-
5
Brian is a young man who is not ready to quit smoking.
-
6
Nicole is a young woman who is not ready to quit smoking.
-
7
Dennis is a middle-aged man who is not ready to quit smoking.
-
8
Margaret is a middle-aged woman who is not ready to quit smoking.
Each of the questions below will be duplicated under each of the eight scenarios.
Questions for READY TO QUIT
~Example scenario for Phillip, a young man who is ready to quit smoking.~
Before the Quit Day
{Phillip} is planning to quit but has not set a quit date. Think about what you did to prepare to quit smoking. What would you say to {Phillip} as he is getting ready to quit?
When getting ready to quit smoking, one of the most important things {Phillip} can do is __________.
Many people think of reasons why they want to quit before to them actually quitting. What would you tell {Phillip} to encourage him to quit smoking?
For {Phillip}, some good reasons for quit smoking are _______ and __________.
When tempting situations arise, it is often hard for people to continue in their quit attempt. Think about what {Phillip} can do to stay focused on quitting.
Thinking about ________ can help {Phillip} stay focused on quitting.
To help {Phillip} stay focused quitting, he can ________________.
Set a Quit Day
Our young man, {Phillip}, is now ready to set a quit date. Quitting is easier for people who prepare before their quit day. Think about some of the things {Phillip} can do to get ready for his quit day.
Before his quit day, {Phillip} can __________________.
{Phillip} may find it helpful to ___________________.
Help of friends and family is important for people when they are quitting. Think about how your friends and family may have helped you when you quit.
{Phillip} can ask people around him to help him by_________________.
On the Quit Day
It is now 8 o’clock in the morning on {Phillip}’s quit day. What should he do? Items in your environment often serve as reminders to smoke and may make it more difficult to quit. When you quit smoking, what items did you find necessary to remove from your environment to keep you from smoking?
When {Phillip} is preparing to quit, he may find it helpful to remove _________________.
Quitting day is a big change for people. What are some of the things that {Phillip} can do on his quit day to help him quit.
On {Phillip}’s quit day, he can ___________.
Some people seek help in stopping smoking such as from doctors, quit-lines, or medication. What help would you recommend {Phillip} use on his quit day?
To help {Phillip} quit he could ___________.
Immediately after Quit Day
Yesterday {Phillip} quit smoking! The days right after quitting are often most difficult for many people. What are some of the things {Phillip} can do to keep from smoking?
The first week after {Phillip}’s quit day, he can ____________________ to keep from smoking.
Quitting smoking can involve breaking many small habits such as having a cigarette with coffee or taking multiple cigarette breaks outside the office. Sometimes it is necessary to find other things to do to keep your mind off smoking. What are some things {Phillip} can do in place of smoking (such as chewing gum or having tea instead of coffee)?
Instead of smoking, {Phillip} can ___________.
Some people find certain situations and activities remind them of smoking such as going out at night with friends. What are some things {Phillip} can do to avoid smoking in these activities or situations?
When {Phillip} is around situations and activities that make him want to smoke he can ___________.
Long-term
{Phillip} quit smoking over 6 months ago and has not smoked yet! After you’ve quit smoking, it is important to find ways to keep from smoking. What are ways to help {Phillip} stay smoke-free?
In order to remain smoke-free, {Phillip} can ______________.
Remembering your reasons for wanting to quit can help you stay quit. What reasons can help {Phillip} stay smoke-free?
Reasons such as ______________ may help {Phillip} to stay smoke free.
Staying smoke-free is a huge step and your friends and family can be a big help. After his quit day how might {Phillip}’s friends and family help him stay smoke-free?
{Phillip}’s friends and family may help him stay smoke-free by______________.
Quitting smoking can be difficult. What can {Phillip} do to avoid slips or relapses?
To avoid having a slip or relapse {Phillip} can______________.
If {Phillip} were to smoke a cigarette after he quit, he could______________ to help him get back on track.
Questions for NOT READY
~Example scenario for Brian, a young man who is not ready to quit smoking.~
Many people think of reasons why they want to quit before they actually quit. What are some of the things that may encourage {Brian} to quit smoking?
One reason {Brian} may want to quit smoking is ________. This may benefit his life by________________.
One immediate change {Brian} may notice from quitting smoking is ___________.
Thinking about ________ can help {Brian} stay focused on quitting.
To help {Brian} stay focused on quitting, he can ________________.
Smoking affects all aspects of a person’s life. It is important to think about the effects smoking has on you and those around you. What effects might {Brian} notice in his life?
Smoking may negatively impact {Brian}’s life by _______________________.
Smoking may negatively impact the people around {Brian} by __________________.
Quitting smoking is hard. Think about some of the difficulties you had when you tried to stop smoking. What challenges might Brain face in quitting?
Some of the problems {Brian} may have in quitting are ______________, ____________, and __________. To overcome these problems, he can ______________, _________, and ___________.
Family and friends can play a big role in quitting smoking. Think about things your family and friends did to help you stop smoking. Did they also do things that made it more difficult for you to stop smoking? How can {Brian} get his family and friends involved in his quit attempt?
{Brian}can ask his family and friends to help him quit smoking by ______________________________________________________.
If {Brian}’s family and friends are making quitting smoking more difficult for him he can_____________________________________________.
Since {Brian} has not decided to quit smoking it sounds like he might benefit from learning more about smoking and quitting smoking.
What are some things you would suggest {Brian} do to learn more?______________________________________________________
Smoking can be a very expensive habit. Did you think about how much money you would save when you were quitting smoking?
What would you encourage {Brian} to think about regarding the cost of smoking?__________________________________________________________
It sounds like {Brian} is not quite ready to quit. Sometimes it is difficult to make that leap.
What made you quit?________________________________________
Appendix B

Footnotes
The National Dental PBRN Collaborative Group and QUIT PRMO Collaborative Group consists of practitioners, faculty, and staff who contributed to this activity. For a list of members: nationaldentalpbrn.org/publication.php.
Trial registration: This study is registered at www.clinicaltrials.gov NCT00797628 (web-delivered provider intervention for tobacco control [QUIT-PRIMO]) and NCT01108432 (DPBRN Hygienists Internet Quality Improvement in Tobacco Cessation [HiQuit]).
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fiore MC, Croyle RT, Curry SJ, Cutler CM, Davis RM, Gordon C, et al. Preventing 3 million premature deaths and helping 5 million smokers quit: a national action plan for tobacco cessation. Am J Public Health. 2004 Feb;94(2):205–10. doi: 10.2105/ajph.94.2.205. [Research Support, U.S. Gov’t, P.H.S.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lancaster T, Stead LF. Self-help interventions for smoking cessation. Cochrane Database Syst Rev. 2005;(3):CD001118. doi: 10.1002/14651858.CD001118.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Strecher VJ. Computer-tailored smoking cessation materials: a review and discussion. Patient Educ Couns. 1999 Feb;36(2):107–17. doi: 10.1016/s0738-3991(98)00128-1. [DOI] [PubMed] [Google Scholar]
- 4.Sciamanna CN, Ford DE, Flynn JA, Langford C. An evidence-based interactive computer program to assist physicians in counseling smokers to quit. MD computing: computers in medical practice. 1999 Sep-Oct;16(5):54–60. [Research Support, U.S. Gov’t, P.H.S.] [PubMed] [Google Scholar]
- 5.Bental DS, Cawsey A, Jones R. Patient information systems that tailor to the individual. Patient Educ Couns. 1999 Feb;36(2):171–80. doi: 10.1016/s0738-3991(98)00133-5. [Research Support, Non-U.S. Gov’t Review] [DOI] [PubMed] [Google Scholar]
- 6.Augustson E, Bright M, Babb S, Malarcher A, Rodes R, Beistle D, et al. Increase in Quitline Calls and Smoking Cessation Website Visitors During a National Tobacco Education Campaign- March 19-June 10, 2012. Morbidity and Mortality Weekly Report. 2012;61(34):667–70. [PubMed] [Google Scholar]
- 7.Kreuter MW, Farrell DW, Olevitch LR, Brennan LK. Customizing Communication with Computer Technology. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2000. Tailoring Health Messages. [Google Scholar]
- 8.Shiffman S, Paty JA, Rohay JM, Di Marino ME, Gitchell J. The efficacy of computer-tailored smoking cessation material as a supplement to nicotine polacrilex gum therapy. Arch Intern Med. 2000 Jun 12;160(11):1675–81. doi: 10.1001/archinte.160.11.1675. [DOI] [PubMed] [Google Scholar]
- 9.Brug J, Steenhuis I, van Assema P, de Vries H. The impact of a computer-tailored nutrition intervention. Prev Med. 1996 May-Jun;25(3):236–42. doi: 10.1006/pmed.1996.0052. [DOI] [PubMed] [Google Scholar]
- 10.Strecher V. Developing a tool for evaluating the quality of print-based health education materials. Atlanta, GA: DHHS, Public Health Service, CDC; 1994. [Google Scholar]
- 11.Prochaska JO, DiClemente CC, Velicer WF, Rossi JS. Standardized, individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychol. 1993 Sep;12(5):399–405. doi: 10.1037//0278-6133.12.5.399. [DOI] [PubMed] [Google Scholar]
- 12.Campbell MK, DeVellis BM, Strecher VJ, Ammerman AS, DeVellis RF, Sandler RS. Improving dietary behavior: the effectiveness of tailored messages in primary care settings. Am J Public Health. 1994 May;84(5):783–7. doi: 10.2105/ajph.84.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bull FC, Kreuter MW, Scharff DP. Effects of tailored, personalized and general health messages on physical activity. Patient Educ Couns. 1999 Feb;36(2):181–92. doi: 10.1016/s0738-3991(98)00134-7. [DOI] [PubMed] [Google Scholar]
- 14.Kreuter MW, Strecher VJ. Do tailored behavior change messages enhance the effectiveness of health risk appraisal? Results from a randomized trial. Health Educ Res. 1996 Mar;11(1):97–105. doi: 10.1093/her/11.1.97. [DOI] [PubMed] [Google Scholar]
- 15.Marcus BH, Emmons KM, Simkin-Silverman LR, Linnan LA, Taylor ER, Bock BC, et al. Evaluation of motivationally tailored vs. standard self-help physical activity interventions at the workplace. Am J Health Promot. 1998 Mar-Apr;12(4):246–53. doi: 10.4278/0890-1171-12.4.246. [DOI] [PubMed] [Google Scholar]
- 16.An LC, Schillo BA, Saul JE, Wendling AH, Klatt CM, Berg CJ, et al. Utilization of smoking cessation informational, interactive, and online community resources as predictors of abstinence: cohort study. J Med Internet Res. 2008;10(5):e55. doi: 10.2196/jmir.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lenert L, Munoz RF, Perez JE, Bansod A. Automated e-mail messaging as a tool for improving quit rates in an internet smoking cessation intervention. J Am Med Inform Assoc. 2004 Jul-Aug;11(4):235–40. doi: 10.1197/jamia.M1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suggs LS, McIntyre C. Are we there yet? An examination of online tailored health communication. Health Educ Behav. 2009 Apr;36(2):278–88. doi: 10.1177/1090198107303309. [DOI] [PubMed] [Google Scholar]
- 19.Dijkstra A, De Vries H. The development of computer-generated tailored interventions. Patient Educ Couns. 1999 Feb;36(2):193–203. doi: 10.1016/s0738-3991(98)00135-9. [DOI] [PubMed] [Google Scholar]
- 20.Kukafka R, Lussier YA, Patel VL, Cimino JJ. Developing tailored theory-based educational content for WEB applications: illustrations from the MI-HEART project. Stud Health Technol Inform. 2001;84(Pt 2):1474–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Kok G, Schaalma H, Ruiter RA, van Empelen P, Brug J. Intervention mapping: protocol for applying health psychology theory to prevention programmes. J Health Psychol. 2004 Jan;9(1):85–98. doi: 10.1177/1359105304038379. [DOI] [PubMed] [Google Scholar]
- 22.Ashing-Giwa K. Health behavior change models and their socio-cultural relevance for breast cancer screening in African American women. Women Health. 1999;28(4):53–71. doi: 10.1300/J013v28n04_04. [DOI] [PubMed] [Google Scholar]
- 23.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 24.Kelly CM, Baker EA, Brownson RC, Schootman M. Translating research into practice: using concept mapping to determine locally relevant intervention strategies to increase physical activity. Eval Program Plann. 2007 Aug;30(3):282–93. doi: 10.1016/j.evalprogplan.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999 Winter;9(1):10–21. [PubMed] [Google Scholar]
- 26.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003 Apr;30(2):133–46. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 27.Kreuter MW, Green MC, Cappella JN, Slater MD, Wise ME, Storey D, et al. Narrative communication in cancer prevention and control: a framework to guide research and application. Ann Behav Med. 2007 Jun;33(3):221–35. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- 28.Hinyard LJ, Kreuter MW. Using narrative communication as a tool for health behavior change: a conceptual, theoretical, and empirical overview. Health Educ Behav. 2007 Oct;34(5):777–92. doi: 10.1177/1090198106291963. [DOI] [PubMed] [Google Scholar]
- 29.Houston TK, Cherrington A, Coley HL, Robinson KM, Trobaugh JA, Williams JH, et al. The art and science of patient storytelling-harnessing narrative communication for behavioral interventions: the ACCE project. J Health Commun. 2011 Aug;16(7):686–97. doi: 10.1080/10810730.2011.551997. [DOI] [PubMed] [Google Scholar]
- 30.Houston TK, Allison JJ, Sussman M, Horn W, Holt CL, Trobaugh J, et al. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann Intern Med. 2011 Jan 18;154(2):77–84. doi: 10.7326/0003-4819-154-2-201101180-00004. [DOI] [PubMed] [Google Scholar]
- 31.Bandura A. Social Foundations of Thought and Action: a social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 32.Howe J. Wired. 2006. The Rise of Crowdsourcing. [Google Scholar]
- 33.Brabham D. Crowdsourcing as a Model for Problem Solving. The International Journal of Research into New Media Technologies. 2008;14(1):75–90. [Google Scholar]
- 34.Swan M. Crowdsourced health research studies: an important emerging complement to clinical trials in the public health research ecosystem. J Med Internet Res. 2012;14(2):e46. doi: 10.2196/jmir.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sadasivam RS, Allison JJ, Ray MN, Ford DE, Houston TK. Using a Resource Effect Study Pre-Pilot to Inform a Large Randomized Trial: The Decide2Quit.Org Web-Assisted Tobacco Intervention. AMIA Annu Symp Proc. 2012;2012:789–98. [PMC free article] [PubMed] [Google Scholar]
- 36.Houston TK, Sadasivam RS, Ford DE, Richman J, Ray MN, Allison JJ. The QUIT-PRIMO provider-patient Internet-delivered smoking cessation referral intervention: a cluster-randomized comparative effectiveness trial: study protocol. Implement Sci. 2010;5:87. doi: 10.1186/1748-5908-5-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Google AdWords. 2011 www.adwords.google.com.
- 38.Fiore M, Jaen C, Baker T, Bailey W, Benowitz N, Curry S, et al. Clinical Practice Guideline. Rockville, MD: DHHS. Public Health Service; May, 2008. Treating Tobacco Use and Dependence: 2008 Update. [Google Scholar]
- 39.DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol. 1991 Apr;59(2):295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- 40.Guo G, Zhao H. Multilevel Modeling for Binary Data. Annual Review of Sociology. 2000;26(1):441–62. [Google Scholar]
- 41.Rabe-Hesketh S, Skrondal A, Pickles A. Reliable estimation of generalized linear mixed models using adaptive quadrature. Stata Journal. 2002;2(1):1–21. [Google Scholar]
- 42.Saul JE, Schillo BA, Evered S, Luxenberg MG, Kavanaugh A, Cobb N, et al. Impact of a statewide Internet-based tobacco cessation intervention. J Med Internet Res. 2007;9(3):e28. doi: 10.2196/jmir.9.4.e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Strecher VJ, McClure J, Alexander G, Chakraborty B, Nair V, Konkel J, et al. The role of engagement in a tailored web-based smoking cessation program: randomized controlled trial. J Med Internet Res. 2008;10(5):e36. doi: 10.2196/jmir.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cobb NK, Graham AL, Bock BC, Papandonatos G, Abrams DB. Initial evaluation of a real-world Internet smoking cessation system. Nicotine Tob Res. 2005 Apr;7(2):207–16. doi: 10.1080/14622200500055319. [DOI] [PMC free article] [PubMed] [Google Scholar]


