Abstract
Adolescents, who have a parent with Huntington Disease (HD), not only are at genetic risk for HD but also are witness to its onset and devastating clinical progression as their parent declines. To date, no mechanism has been developed to direct health care providers to the atypical adolescent experiences of these teens. The purpose of this report is to describe the process of developing the HD-Teen Inventory clinical assessment tool. Forty-eight teens and young adults from 19 U.S. states participated in the evaluation of the HD-Teen Inventory tool. Following item analysis, the number of items was reduced and item frequency and reaction scales were combined, based on the strong correlation (r = .94). The resultant tool contains 15 inventory and 2 open-ended response items. The HD-Teen Inventory emerged as a more compact and efficient tool for identifying the most salient concerns of at-risk teens in HD families in research and/or clinical practice.
Keywords: Huntington disease, adolescence, HD-Teen Inventory, field test
Introduction
Adolescence is commonly recognized as the developmental period during which an individual transitions between being a child and becoming an adult (Holmbeck, 2002; Smetana, Campione-Barr, & Metzger, 2006). Current research suggests that for this transition to be successful, teens need ongoing and secure parental attachment (Hair, Moore, Garrett, Ling, & Cleveland, 2008). Thus, health providers caring for teens must be aware of issues affecting both teens and their parents since both can affect the teen’s risk for transition difficulties.
One group of adolescents that needs focused attention includes teens with parents who have Huntington Disease (HD). Research reveals these teens can have atypical, complex, and often painful adolescent and family experiences, which increases their risk for a difficult transition through adolescence (Duncan et al., 2007, 2008; Keenan, Miedaybrodzka, van Teigjlingen, McKee, & Simpson, 2007; Keenan, van Teijlingen, McKee, Miedzybrodzka, & Simpson, 2009; Sparbel et al., 2008; Williams, Ayres, Specht, Sparbel, & Klimek, 2009a). Nevertheless, assessing this group of teens and clinical follow-up is particularly challenging, because HD families often carefully conceal their situation, making it difficult to be aware of potential problems (Quaid et al., 2008).
Background
Huntington disease (HD) is an inherited, neuropsychiatric disease involving progressive, involuntary and voluntary motor disability, a decline in cognitive capability, and psychiatric disturbances (Sturrock & Leavitt, 2010; Warby, Graham, & Hayden, 2010). The mean onset of clinical symptoms is 30 to 50 years of age; and after onset, the median survival time is 17 to 20 years (Roos, 2010). The average age at death for an adult with HD is 55 years of age.
Adolescents who have a parent with HD typically witness the onset of their parent’s symptoms, the disease progression, and their parent’s decline and eventual death. To date, there is no cure or life-extending intervention for the individual with HD (Richards, 2008). While having a parent with a life-altering and limiting disease is difficult for any teen, symptom progression in the HD parent can be especially disruptive to the process of secure parental attachment, often placing the teen in the role of caregiver rather than receiver.
Affected individuals may present with neurologic psychiatric or cognitive changes. Chorea, an involuntary movement disorder involving irregular jerking of limbs, face, or trunk, is present in more than 90% of individuals (Sturrock & Leavitt, 2010). The choreic movements are continuously present during waking hours, leading to increased caloric needs that are difficult to keep up with. In the early stages of HD, clinical manifestations include subtle changes in coordination, minor involuntary movements, and difficulty in mental planning, irritability, and depression (Cummins, Eggert, Pruitt, & Collins, 2011). In the middle stage, chorea becomes more prominent, voluntary activity becomes increasingly difficult, and dysphagia emerges, along with intermittent outbursts of aggressive behaviors and social disinhibition. In the late stages of HD, motor disability becomes severe and the individual is totally dependent.
In addition, because HD is inherited in an autosomal dominant manner, teens in HD families face an additional challenge as they discover their own genetic risk for the disease (Sturrock & Leavitt, 2010). The inheritance of HD follows an autosomal dominant pattern, meaning each offspring of an individual with HD has a 50%, or 50-50, chance of inheriting the disease. Although genetic testing for HD is available to “at risk” individuals, it is not offered to teens until the individual reaches 18 years of age, the age at which they can give their own informed consent.
Although these teens’ genetic risk to develop HD is already fixed, their developmental and health trajectories are not. Accordingly, through qualitative interviews and focus groups, their experiences have been explored in-depth, highlighting the need to identify teens who can be facing difficult challenges and provide support (Duncan et al., 2007, 2008; Keenan et al., 2007, 2009; Sparbel et al., 2008; Williams et al., 2009a). Nevertheless, no mechanism has yet been developed that allows clinicians or researchers to readily access these teen experiences in the clinical setting. To address this shortfall, we developed, field-tested, and revised, a novel, clinical inventory tool—the HD-Teen Inventory (HD-TI). Here, we report the development of the HD-TI and findings from the field test.
Method
This section begins with a brief overview of the process to develop items for the HD-TI, followed by a discussion of the field test and subsequent revision of the HD-TI as it was transitioned to its current format as a clinical tool.
Development of the HD-TI
The development of the HD-TI began within a larger study focusing on the needs of family members of individuals with HD linked with the PREDICT-HD study (Paulsen et al., 2006; Williams, 2001). In the first phase of the larger study, data from focus groups were used to develop items. The focus group data and analysis with teens (Sparbel et al., 2008; Williams et al., 2009a) and adult family members (Williams & Ayres, 2007; Williams et al., 2007, 2009b) are reported elsewhere (Skirton, Williams, Barnette, & Paulsen, 2010; Williams, Skirton, Barnette, & Paulsen, 2012). Here, we focus on the final stage of evaluation and the transition of the HD-TI to its final format (Figure 1).
Figure 1.
Sequenced,3-phase evaluative process used in developing the HD-TI
Field Test
The HD-TI items were identified from the first phase qualitative analysis of data from six focus groups that involved 32 teens at five HD Centers across the United States and Canada (Sparbel et al., 2008; Williams et al., 2009a). To assure the initial items were clear and relevant; we validated the item content using nine experts in HD, family and/or pediatric clinical management, or research, as well as 9 teens who participated in the initial focus groups. The resultant HD-TI contained 29 Personal Concerns items and two open-ended questions. The openended questions asked respondents to identify (a) the top-ranked concern from the items listed and (b) any item that was missing that we needed to know about.
The next step was to field test the HD-TI in a new sample to identify potential sources of problems in terms of item concepts, response format, and/or admin- istration (Groves et al., 2009). For this study, the research team was particularly interested in fine-tuning the HD-TI, to make it user-friendly and ensure it cap- tured only the aspects of the teens’ experiences that are unique in HD families by carving these aspects out from the larger experience of adolescence. Of particular concern was the inclusion of teen preferences. This concern was rooted in the evidence-based practice movement’s emphasis on the application of best research evidence to clinical care in conjunction with the preferences and wishes of the patients to which the evidence is being applied. Clinical assessment tools developed using this approach are more likely to direct clinician’s attention to those items most important to patients, which in this case were teens in HD families (Gilgum, 2004; Morse et al., 1998).
The study was approved by the University of Iowa Institutional Review Board (IRB). The sampling goal was to obtain equal distribution of teens (14 to 17 years of age) and young adults (18 to 30 years of age). The two groups were purposively sought not only to ascertain what concerns are unique to teens currently living in families with HD but also to identify concerns that persist over time in the memory of young adults recalling their teen years. Eligible participants (a) had a family member with HD, (b) could communicate in English, and (c) were 14 to 30 years of age. The study was announced through the University of Iowa HD Registry and Huntington Disease Society of America (HDSA). Participants received their choice of either a phone card or an iTunes gift card for participating.
Forty-eight teens and young adults from 19 different U.S. states participated. Of the 48 participants, 66.7% were female and 91.7% were White. The mean age was 18.8 years (SD = 4.41). Twenty three (47.9%) were teens (14 to 17 years old) and 21 (43.8%) were young adults (18 to 30 years old).
Findings
In the initial version of the HD-TI, each respondent was asked to indicate two things: (a) the frequency with which each of the 29 items occurred and (b) their personal reaction. For example, one item was I worry I will develop HD. Respondents first indicated how frequently this concern occurred in the past month (0 = never occurred at any time, to 4 = several times a week, daily, or more). They were then asked to share their personal reaction, in terms of how much this concern bothers them (0 = not at all, to 4 = extremely). For each item, an overall index score was also calculated to represent the product of these two ratings (frequency × reaction). Internal consistency measures and 95% confidence intervals were computed using the ScoreRel CI program (Barnette, 2005). All values were well above common standards used to assess internal consistency: (a) frequency (α = .96; CI [.94, .97]), (b) personal reaction (α = .96; CI [.95, .98]), and (c) overall index score (α = .96; CI [.94, .97]).
Items were ranked by statistical mean (M). The top-ranked item was I worry I will develop HD (M = 2.50), with 76% reporting this concern occurred any- where from once a month to several times a day. The second ranked item, It is difficult to distinguish HD from the person (M = 2.36), followed close behind, with more than 66% of respondents reporting this concern also occurred any- where from once a month to several times a day. Items identified by intensity/reaction scores were also ranked by statistical mean. Of note, was the extremely strong correlation between item frequency means and the reaction/intensity means (r = .94). Also of note was a clear delineation of item frequency between the top 14 and remaining 15 items.
Items were further analyzed by examining differences between the teens’ responses and the experiences young adults recalled from their teen years. Using Fisher Exact tests, 16 items had significantly (p < .05) higher frequencies in the young adults recalling their teen experiences. Fifteen of the 16 items also had significantly higher intensity/reaction scores (p < .05). Twelve of the 16 items were already among the 14 top-ranked teen group items, validating their prevalence and importance in teen’s lives. Females reported six concerns significantly more often (p < .05) than their male counterparts. However, because there was a 2:1 female to male ratio in the numbers of participants, male respondents were examined as a subgroup to ensure their experiences were being not masked by the larger female presence. The team was reassured as the top-ranked male concerns, across both teens and young adults, were found to be identical to the overall ranking of items.
The final evaluative step compared top-ranked items to the two open-ended questions. Of the 48 participants, 31 (62.5%) responded. Three concerns were mentioned most often and were already identified in the top-ranked 14 items: (a)I worry that I will develop HD (10 comments), (b) I feel worried that my quality time with him or her is running out (6 comments), and (c) I feel no one knows what I am going through (6 comments). Seven (22%) of the 48 participants indicated a concern they felt was missing: having an intimate relationship.
To understand how concerns about intimacy had not been included in the original items, the research team returned to the transcripts and analysis from the Phase 1 teen focus groups. A close evaluation revealed intimacy was identified as an important teen concern, but the team felt it was a concern common to most teens, not unique to teens in HD families, and therefore had not been included. However, after close rereading and write-in comments during the field test, the teens’ concerns about becoming intimate went beyond typical adolescent concerns about sexual and/or intimate relationships as these teens were concerned about becoming intimate because they did not yet know their genetic HD-risk status. Therefore, the decision was made to add this item to the HD-TI, using the participants’ written responses to craft it.
Refining the HD-TI
The first step in refining the HD-T was to establish whether the internal consistency of the HD-T would be compromised if, out of the original 29, only the 14 top-ranked items were included. The Cronbach α for the 14 items remained high at .93 (frequency) and .94 (reaction). Second, because of the extremely strong correlation between frequency and reaction scores (r = .94), the research team felt that either score could be used. Furthermore, the participants suggested collapsing scaled responses into binomial response categories (yes/no) was more user-friendly. Having binomial categories also ensured male responses, which scaled lower than females, were represented equally. Furthermore, other researchers are beginning to report that teens prefer categorical responses over Likert-type scales (Flicker et al., 2010; Gallo, 2010).
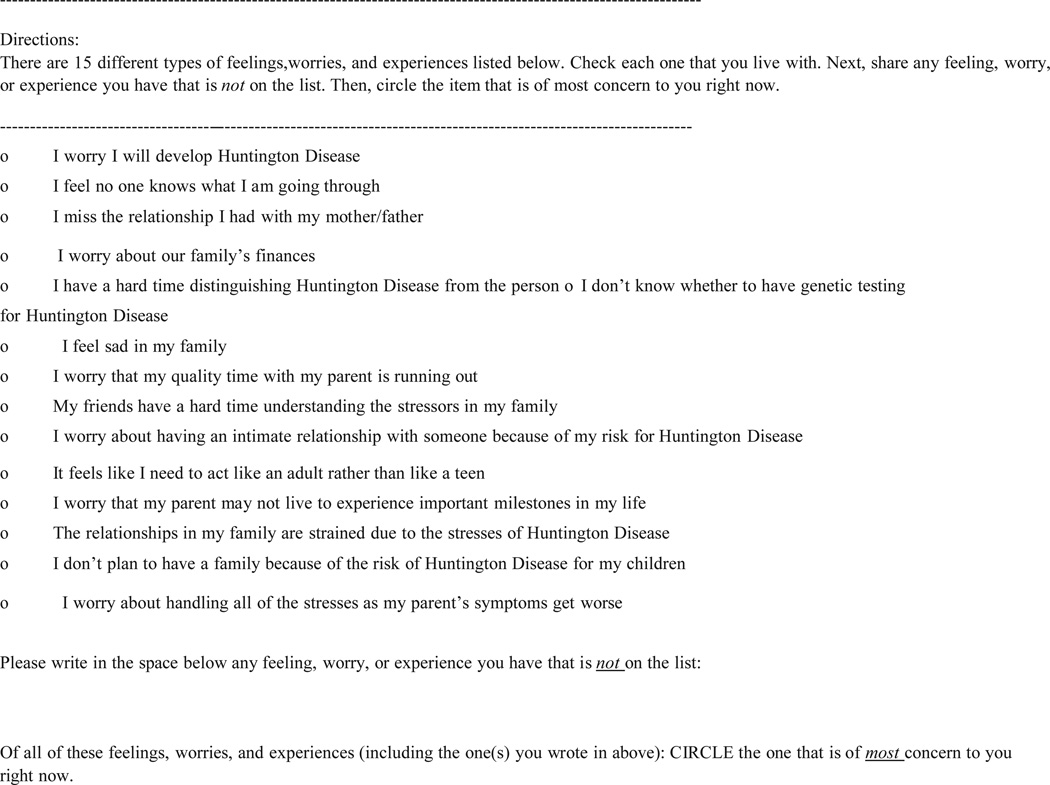
After field testing, the final format that emerged for the HD-TI is a targeted, 15-item categorical response inventory, with two open-ended questions that allow for individuation and continued evolution (Figure 2).
Figure 2.
HD Teen Inventory (HD-TI)
Summary
The research team used a carefully sequenced, evaluative process that placed teens at the forefront at each stage, thus producing a clinical inventory tool that captures the unique aspects of teens in HD families. This is particularly important because while individuals directly affected by HD receive health care from specialists, the adolescents within these families typically receive their health care from primary care providers who may be unaware that these teens have specific risks that can impede their transition through adolescence. The process used in developing the HD-TI may be relevant to other researchers seeking to capture experiences of teens in families with other adult-onset and/ or progressive chronic conditions that could interfere with a teen’s ability to maintain secure parental attachment during adolescence.
The HD-TI emerged from field testing as a more compact and efficient tool for assessing the most salient concerns of at-risk teens in HD families. The open-ended questions provided formative comments, which not only validated but also revealed an important omission. The open-ended questions were retained to capture individual experiences that may not be anticipated and to create a mechanism through which the tool can continue to evolve. By adding an item about intimacy, the HD-TI was further enhanced. The final inventory format is easy to administer, can be completed within the time constraints of clinical practice, and provides health care providers and researchers with the ability to identify sources of personal concerns for teens growing up in families with members who have HD. Awareness of these concerns is an essential first step in building supportive and health promoting interventions for this population.
Acknowledgments
The authors would like to acknowledge the entire HD Family Research Team, site coordinators, and participants.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by an NIH/NINR Grant (R01NR07079) to Janet K. Williams and linked with Jane S. Paulsen’s NINDS Grant (R0140068), NIMH Grant (R0101579), the Roy J. Carver Trust Medicine Research Initiative, Howard Hughes Medical Institute, and a CHDI Foundation Grant.
Biographies
Martha Driessnack, PhD, PNP-BC, RN, is an assistant professor at the College of Nursing, The University of Iowa, Iowa City, IA, USA.
Janet K.Williams, PhD, RN, FAAN, is the Kelting Professor of Nursing at the College of Nursing, The University of Iowa, Iowa City, IA, USA.
J. Jackson Barnette, PhD, is a professor of biostatistics & informatics at the Colorado School of Public Health, University of Colorado–Denver, Denver, CO, USA.
Kathleen J. Sparbel, PhD, FNP-BC, RN, is a clinical assistant professor at the College of Nursing, University of Illinois–Chicago, Chicago, IL, USA.
Jane S. Paulsen, PhD, is professor of psychiatry, neurology, psychology, and neurosciences at the Carver College of Medicine, The University of Iowa, Iowa City, IA, USA.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Barnette J. ScoreRel CI: A Excel program for computing confidence intervals of commonly used score reliability coefficients. Educational and Psychological Measurement. 2005;65:980–983. [Google Scholar]
- Cummins A, Eggert J, Pruitt R, Collins JS. Huntington disease: Implications for practice. Nurse Practitioner. 2011;36(2):41–47. doi: 10.1097/01.NPR.0000392796.01760.e2. [DOI] [PubMed] [Google Scholar]
- Duncan RE, Gillam L, Savulescu J, Williamson J, Rogers JG, Delatycki M. “Holding your breath”: Interviews with young people who have undergone predictive genetic testing for Huntington disease. American Journal of Medical Genetics, Part A. 2007;143A:1984–1989. doi: 10.1002/ajmg.a.31720. [DOI] [PubMed] [Google Scholar]
- Duncan RE, Gillam L, Savulescu J, Williamson R, Rogers JG, Delatycki M. “You’re one of us now”: Young people describe their experiences of predictive genetic testing for Huntington disease (HD) and familial adenomatous polyposis (FAP) American Journal of Medical Genetics, Part C, Seminars in Medical Genetics. 2008;148C(1):47–55. doi: 10.1002/ajmg.c.30158. [DOI] [PubMed] [Google Scholar]
- Flicker S, Guta A, Larkin J, Flynn S, Fridkin A, Travers R, Layne C. Survey design from the ground up: Collaboratively creating the Toronto Teen Survey. Health Promotion Practice. 2010;11(1):112–122. doi: 10.1177/1524839907309868. [DOI] [PubMed] [Google Scholar]
- Gallo A. Teens with and without genetic conditions: Focus group findings about appropriateness and feasibility of data collection methods; Paper presented at the Midwest Research Nursing Society Conference; Kansas City, MO. 2010. Apr 8–11, [Google Scholar]
- Gilgum JF. Qualitative methods and the development of clinical assessment tools. Qualitative Health Research. 2004;14(7):1008–1019. doi: 10.1177/1049732304266819. [DOI] [PubMed] [Google Scholar]
- Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourarangeau R. Survey methodology. 2nd ed. Hoboken, NJ: John Wiley; 2009. [Google Scholar]
- Hair EC, Moore KA, Garrett SB, Ling T, Cleveland K. The continued importance of quality parent–adolescent relationships during late adolescence. Journal of Research on Adolescence. 2008;18:187–200. [Google Scholar]
- Holmbeck GN. A developmental perspective on adolescent health and illness: An introduction to special issues. Journal of Pediatric Psychology. 2002;27:409–415. doi: 10.1093/jpepsy/27.5.409. [DOI] [PubMed] [Google Scholar]
- Keenan KF, Miedzybrodzka Z, van Teijlingen E, McKee L, Simpson SA. Young people’s experiences of growing up in a family affected by Huntington’s disease. Clinical Genetics. 2007;71(2):120–129. doi: 10.1111/j.1399-0004.2006.00702.x. [DOI] [PubMed] [Google Scholar]
- Keenan KF, van Teijlingen E, McKee L, Miedzybrodzka Z, Simpson SA. How young people find out about their family history of Huntington’s disease. Social Science & Medicine. 2009;68:1892–1900. doi: 10.1016/j.socscimed.2009.02.049. [DOI] [PubMed] [Google Scholar]
- Morse JM, Hutchinson S, Penrod J. From theory to practice: The development of assessment guides from qualitatively derived theory. Qualitative Health Research. 1998;8:329–340. [Google Scholar]
- Paulsen JS, Hayden M, Stout JC, Langbehn DR, Aylward E, Ross CA, Penziner E. Preparing for preventive clinical trials: The Predict-HD study. Archives of Neurology. 2006;63:883–890. doi: 10.1001/archneur.63.6.883. [DOI] [PubMed] [Google Scholar]
- Quaid KA, Sims SL, Swenson MM, Harrison JM, Moskowitz C, Stepanov N, Wetphal BJ. Living at risk: Concealing risk and preserving hope in Huntington disease. Journal of Genetic Counseling. 2008;17(1):117–128. doi: 10.1007/s10897-007-9133-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards FH. Predictive genetic testing of adolescents for Huntington disease: A question of autonomy and harm. American Journal of Medical Genetics, Part A. 2008;146A:2443–2446. doi: 10.1002/ajmg.a.32477. [DOI] [PubMed] [Google Scholar]
- Roos RAC. Huntington’s disease: A clinical review. Orphanet Journal of Rare Diseases. 2010;5:40. doi: 10.1186/1750-1172-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skirton H, Williams JK, Barnette JJ, Paulsen JS. Huntington disease: Families’ experiences of healthcare services. Journal of Advanced Nursing. 2010;66:500–510. doi: 10.1111/j.1365-2648.2009.05217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smetana JG, Campione-Barr N, Metzger A. Adolescent development in interpersonal and societal contexts. Annual Reviews in Psychology. 2006;57:255–284. doi: 10.1146/annurev.psych.57.102904.190124. [DOI] [PubMed] [Google Scholar]
- Sparbel KJ, Driessnack M, Williams JK, Schutte DL, Tripp-Reimer T, McGonigal-Kenney M, Paulsen JS. Experiences of teens living in the shadow of Huntington Disease. Journal of Genetic Counseling. 2008;17:327–335. doi: 10.1007/s10897-008-9151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturrock A, Leavitt BR. The clinical and genetic features of Huntington disease. Journal of Geriatric Psychiatry and Neurology. 2010;23:243–259. doi: 10.1177/0891988710383573. [DOI] [PubMed] [Google Scholar]
- Warby SC, Graham RK, Hayden MR. Huntington disease [Last updated, April 22, 2010] GeneReviews. 2010 Retrieved from http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=huntington.
- Williams JK. Family health after predictive HD testing. 2001 Retrieved from http://projectreporter.nih.gov/reporter.cfm.
- Williams JK, Ayres L. “I’m like you”: Establishing and protecting common ground in focus groups with Huntington disease caregivers. Journal of Research in Nursing. 2007;12:655–664. [Google Scholar]
- Williams JK, Ayres L, Specht J, Sparbel K, Klimek ML. Caregiving by teens for family members with Huntington disease. Journal of Family Nursing. 2009a;15:273–294. doi: 10.1177/1074840709337126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JK, Hamilton R, Nehl C, McGonigal-Kenney M, Schutte DL, Sparbel K, Paulsen JS. “No one sees the difference”: Family members’ perceptions of changes in persons with preclinical Huntington disease. American Journal of Human Genetics, Part B Neuropsychiatric Genetics. 2007;144B:636–641. doi: 10.1002/ajmg.b.30479. [DOI] [PubMed] [Google Scholar]
- Williams JK, Skirton H, Barnette JJ, Paulsen JS. Huntington disease caregiver personal concerns. Journal of Advanced Nursing. 2012;68(1):137–146. doi: 10.1111/j.1365-2648.2011.05727.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JK, Skirton H, Paulsen JS, Tripp-Reimer T, Jarmon L, McGonigal-Kenney M, Honeyford J. The emotional experiences of family carers in Huntington disease. Journal of Advanced Nursing. 2009b;65:789–798. doi: 10.1111/j.1365-2648.2008.04946.x. [DOI] [PMC free article] [PubMed] [Google Scholar]