Abstract
Background
Little is known about how often contextual factors such as patient preferences and competing priorities impact prescribing of guideline-recommended medications, or about the extent to which these factors are documented in medical records and available to performance measurement systems.
Methods
Mixed-methods study of 295 veterans age 50 years and older in 4 VA health care systems who had systolic heart failure and were not prescribed a beta blocker and/or an ACE inhibitor (ACE-I) or angiotensin receptor blocker (ARB). Reasons for non-treatment were identified from clinic notes and from interviews with 62 primary care clinicians caring for these patients. These reasons were classified using a published taxonomy.
Results
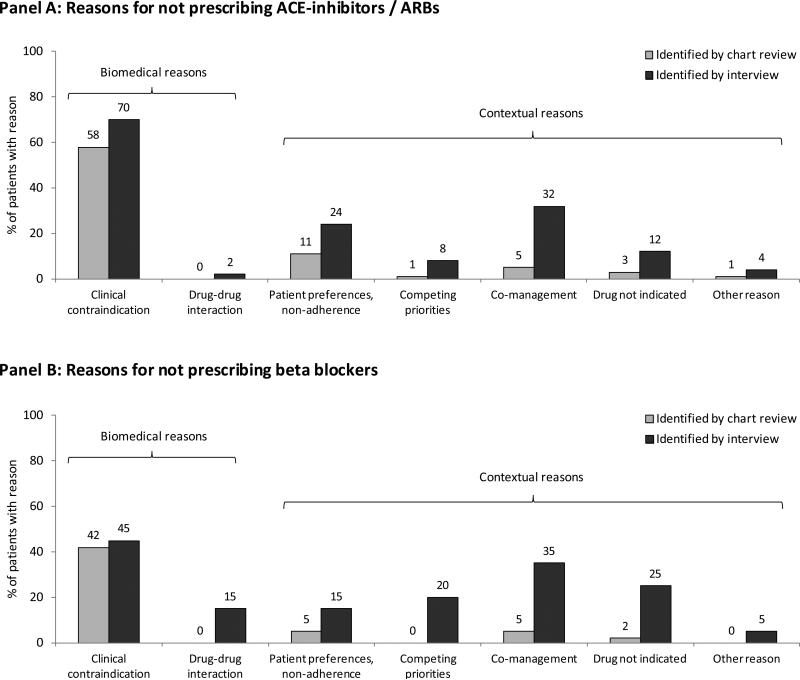
Among 295 patients not receiving guideline-recommended drugs for heart failure, chart review identified biomedical reasons for non-prescribing in 42-58% of patients and contextual reasons in 11-17%. Clinician interviews identified twice as many reasons for non-prescribing as chart review (mean 1.6 vs. 0.8 reasons per patient, P < .001). In these interviews, biomedical reasons for non-prescribing were cited in 50-70% of patients, and contextual reasons in 64-70%. The most common contextual reasons were co-management with other clinicians (32-35% of patients), patient preferences and non-adherence (15-24%), and clinician belief that the medication is not indicated in the patient (12-20%).
Conclusions
Contextual reasons for not prescribing ACE-I/ARBs and beta blockers are present in two-thirds of patients with heart failure who did not receive these medications, yet are poorly documented in medical records. The structure of medical records should be improved to facilitate documentation of contextual reasons for not providing guideline-recommended care.
Keywords: Guideline adherence, heart failure, drug prescribing, performance measurement
INTRODUCTION
Quality assessment systems have recognized the need to account for “exceptions” - patients for whom a given quality measure is not appropriate.7, 10-13 The vast majority of research in this area has focused on clinical contraindications or history of intolerance to a recommended medication. Other reasons for not adhering to a guideline recommendation, such as patient refusal, limited opportunities for care coordination, and competing priorities, are widely recognized as important by clinicians and policy-makers.14-15 However, little is known about how often these contextual issues account for failure to meet performance measurement targets, or about which factors predominate in real-world clinical settings.
We used a combination of chart review and clinician interviews to evaluate clinician reasons for not providing guideline-recommended medications to adults with heart failure. Our primary objective was to assess why clinicians did not prescribe guideline-recommended medications to these patients, with a particular focus on contextual factors. As a secondary objective, we evaluated the extent to which contextual reasons for non-prescribing are documented in the medical record, and thus might be measurable in performance measurement systems.
METHODS
Sample
We studied adults 50 years and older in 4 Department of Veterans Affairs (VA) health care systems who had heart failure with reduced left ventricular ejection fraction (LVEF) and who were not prescribed an angiotensin converting enzyme inhibitor (ACE-I) or angiotensin-receptor blocker (ARB) and/or a beta blocker. Research assistants conducted screening chart reviews on 2,846 patients identified by administrative data as having heart failure and not taking an ACE-I/ARB or beta blocker as of November 2009 to July 2010. Of these, 295 patients (10%) met all inclusion and exclusion criteria. The most common exclusion criteria were the patient not being a regular user of VA services (876 patients), and having preserved or unknown LVEF (950 patients; see Appendix, supplemental digital content 1 for details).
Chart reviews
Research assistants and a research nurse conducted a two-tier, comprehensive chart review. Reasons for not prescribing an ACE-I/ARB and/or a beta blocker were assessed based on a published taxonomy.19 This taxonomy includes “biomedical reasons” for not receiving guideline-recommended medications for heart failure (e.g., clinical contraindications to drug therapy) and “contextual reasons,” which include the patient's life circumstances and goals as well as challenges in health care delivery (e.g., patient attitudes, competing priorities, lack of coordinated care). To be coded as a reason for non-prescribing, we required an explicit or strongly implicit statement that linked the decision not to prescribe to a specific reason for that decision (see Appendix, supplemental digital content 1 for more details). To assess the reliability of coding of reasons for non-prescribing, in a subset of 40 charts a physician reviewer followed the same procedures as the study nurse to identify and code reasons for non-prescribing. The two independent reviewers had full or partial agreement on reasons for non-prescribing in 35 of 40 subjects (88%).
Interviews
We invited all 133 staff clinicians who provided primary care for patients in the chart review cohort and were still practicing in VA to participate in interviews. Of these, 65 (49%) consented and completed interviews. Interviews revealed that 2 patients were taking both ACE-I/ARBs and beta blockers, and additional chart review identified 1 patient taking both medications, leaving 62 eligible clinician interviews.
In the interviews, we asked each clinician open-ended questions and probes designed to elicit their reasons for not prescribing ACE-I/ARBs and/or beta blockers to a patient in the chart review cohort who was under their care. Results of the interview were summarized into a narrative. The principal investigator and a pair of research assistants independently reviewed the narrative and coded reasons for non-prescribing following the same taxonomy employed in the chart review. After excluding a test set, the reviewers obtained matching answers in 51 of 54 clinician interviews. Disagreements were resolved by consensus.
Analyses were performed using Stata 11 (StataCorp, College Station, TX). This research was approved by the institutional review boards of the San Francisco, South Texas, Iowa City, and Connecticut VA Health Care Systems and their affiliated universities.
RESULTS
Characteristics of study patients and clinicians
Among 295 patients, mean age was 74 years, and 98% were men (Table 1). Overall, 243 patients (82%) were not taking ACE-Is / ARBs and 84 (28%) were not taking beta blockers; an overlapping 32 patients (11%) were taking neither medication. Most non-users of ACE-I/ARBs (203; 84%) had previously been prescribed an ACE-I or ARB. Similarly, 61 (73%) non-users of beta blockers had previously been prescribed a beta blocker.
Table 1.
Characteristics of patients and clinicians
| Patients | N(%) N=295 |
|---|---|
| Age (years) | |
| 50-64 | 70 (24) |
| 65-80 | 118 (40) |
| 80 and older | 107 (36) |
| Male sex | 290 (98) |
| Race | |
| White | 187 (63) |
| Black | 19 (6) |
| Other | 8 (3) |
| Not stated | 81 (27) |
| Qualifying LVEF* | |
| <30% | 107 (36) |
| 30-40% | 172 (58) |
| Qualitative value | 16 (5) |
| Comorbid conditions | |
| Coronary heart disease | 211 (72) |
| Diabetes | 122 (41) |
| Chronic lung disease | 110 (37) |
| Atrial fibrillation | 108 (37) |
| Depression | 109 (37) |
| Cancer (non-prostate) | 35 (12) |
| Dementia | 25 (8) |
| Time since last primary care visit | |
| < 2 months | 67 (22) |
| 2-6 months | 166 (56) |
| 7-12 months | 39 (13) |
| >1 year | 15 (5) |
| No primary care visits | 8 (3) |
| Time since last cardiology visit | |
| < 2 months | 35 (12) |
| 2-6 months | 54 (18) |
| 7-12 months | 32 (11) |
| >1 year | 65 (22) |
| No cardiology visits | 109 (37) |
| Co-managed with any non-VA clinician? | |
| Yes | 120 (41) |
| No | 146 (49) |
| Unsure | 29 (10) |
| Study site | |
| Site 1 | 65 (22) |
| Site 2 | 93 (32) |
| Site 3 | 57 (19) |
| Site 4 | 80 (27) |
| Clinicians interviewed | N (%) N=62 |
|---|---|
| Male sex | 30 (48%) |
| Professional status | |
| Staff Physician | 54 (87%) |
| Nurse Practitioner | 8 (13%) |
| Specialty | |
| General Internal Medicine | 38 (61%) |
| Geriatrics | 11 (18%) |
| Family Medicine | 10 (16%) |
| Cardiology or other | 3 (5%) |
| Years since graduated from professional school (median, IQR) | 17 (IQR 12,25) |
| Days per week in clinic (median, IQR) | 5 (IQR 3.5,5) |
LVEF that qualified the patient as eligible for the study. Some patients had qualitative documentation of “moderately” or “severely” depressed LVEF but no numeric LVEF value recorded in the medical record.
The 62 patients that were the focus of interviews had similar characteristics as the 233 patients who were not discussed in clinician interviews, but had visited their primary care clinician more recently than non-interview patients (median 72 vs. 103 days, P=.04; see Supplemental Digital Content Appendix 3).
Reasons for not prescribing guideline-recommended medications
Chart review
Overall, 158 (65%) non-users of ACE-I/ARBs had one or more documented reasons for not receiving these medications, and 41 (49%) non-users of beta blockers had one or more reasons for not receiving a beta blocker. The prevalence of documented reasons for non-prescribing ranged from 43% to 80% of patients across the four study sites. There were differences in the distribution of age, race, and frequency of cardiology contact between patients at the different study sites. However, after controlling for these and other factors there remained a nearly two-fold difference across sites in the rate of documenting reasons for non-prescribing (see Appendix, supplemental digital content 2).
Biomedical reasons for non-prescribing were documented in 141 (58%) non-users of ACE-I/ARBs and 35 (42%) non-users of beta blockers (Figure 1). The most commonly cited contraindications to ACE-I/ARBs were renal insufficiency (59 of 141 patients, 42%); hypotension (53 patients, 38%), and hyperkalemia (29 patients, 21%). The most commonly cited contraindications to beta blockers were bradycardia (14 of 35 patients, 40%), hypotension (9 patients, 26%), and respiratory disease or symptoms (8 patients, 24%). Many patients had more than one contraindication cited.
Figure 1. Reasons for not prescribing guideline-recommended medications for heart failure.
Panel A shows reasons for not prescribing ACE-I/ARBs identified in 243 chart reviews (grey bars) and 50 clinician interviews (black bars) for patients not taking these medications. Panel B shows reasons for not prescribing beta blockers identified in 84 chart reviews (grey bars) and 20 clinician interviews (black bars) for patients not taking these medications.
Biomedical reasons included clinical contraindications to medication therapy; and avoiding drug-drug interactions. Contextual reasons included patient preferences about, adherence to, or misuse of medications; competing priorities, whereby the treating clinician prioritized management of other conditions over heart failure management; co-management with other clinicians (e.g., perception that another clinician was responsible for decisions on heart failure management); clinician belief that the medication(s) was not indicated; and other reasons.
We also evaluated the chart for evidence of biomedical contraindications to ACE-I/ARBs and beta blockers, even if they were not cited by the treating clinician(s) as a reason for not prescribing. These contraindications were present in 20-27% of patients who had no clinician-documented reasons for non-prescribing (Table 2).
Table 2.
Biomedical contraindications identified in the medical record
| Patients not taking ACE-I or ARB | Patients not taking beta blocker | |||
|---|---|---|---|---|
| Item | All patients N (%) N=243 | Patients who had no reasons for non-prescribing documented in the medical record by treating clinicians N (%) N=85 | All patients N (%) N=84 | Patients who had no reasons for non-prescribing documented in the medical record by treating clinicians N (%) N=44 |
| Medication allergy listed in allergy field* | 12 (5) | 0 (0) | 8 (10) | 1 (2) |
| Medication allergy listed in quasi-templated section of note* | 45 (19) | 2 (2) | 7 (8) | 1 (2) |
| Angioedema | 4 (2) | 0 (0) | -- | -- |
| Renal artery stenosis | 12 (5) | 0 (0) | -- | -- |
| Most recent creatinine >=2.5 mg/dl | 32 (13) | 11 (13) | -- | -- |
| Most recent potassium > 5.5 mEq/l | 3 (1) | 2 (2) | -- | -- |
| High degree AV block or sick sinus syndrome without pacemaker | -- | -- | 1 (1) | 0 (0) |
| Chronic lung disease - moderate to severe*† | -- | -- | 20 (24) | 10 (23) |
| Systolic blood pressure <90 mm Hg at most recent clinic visit | 7 (3) | 3 (4) | 3 (4) | 2 (5) |
| Any of the above criteria | 87 (36) | 17 (20) | 29 (35) | 12 (27) |
Data reported in this table were derived from templated and quasi-templated areas of the electronic medical record, and were included regardless of whether clinicians cited the condition as a reason for not prescribing the guideline-recommended drug.
The second and fourth column present results among patients for whom the treating clinician(s) did not document any reason in the medical record as justification for not prescribing the medication. For example, among 85 patients not taking ACE inhibitors from whom the clinicians did not provide any free-text notation as to why they were not prescribing this medication, 11 had a serum creatinine >=2.5 mg/dl. In these cases one might infer that renal insufficiency could have been a reason for avoiding the medication, even though clinicians did not state this explicitly.
Allergy field = distinct area within VA's electronic medical record for recording allergy information; “Allergy listed in quasi-templated section of note” = allergy listed as free text notation within body of note (e.g., under medications in typical progress note format); Moderate or severe chronic lung disease = FEV1 < 80% or qualitative description of lung disease equivalent to “moderate” or worse. Cough not included as a contraindication, since most patients with cough on ACE-inhibitors can tolerate ARBs.
Expanding the definition of chronic lung disease to include any such disease (not just disease of moderate or worse severity) doubled the percentage of non-beta blocker users having this condition from 24% to 48%.
Contextual reasons for not being prescribed ACE-I/ARBs were documented in 42 of 243 patients (17%) not taking ACE-I/ARBs and 9 of 84 (11%) not taking beta blockers (Figure 1). Most of these patients also had biomedical contraindications documented. Only 17 patients not taking ACE-I/ARBs and 6 patients not taking beta blockers had contextual reasons cited as the sole reason for not prescribing.
Interviews
In clinician interviews, all clinicians provided at least one reason for not prescribing, and many stated more than one reason, with a mean of 1.6 reasons cited per patient (compared with 0.8 reasons per patient identified on chart review, P<.001). Among 50 patients not taking ACE-I/ARBs, clinicians cited biomedical reasons for not prescribing in 35 (70%), and contextual reasons in 32 (64%); 17 patients (34%) had both biomedical and contextual reasons cited. Results were similar for the 20 patients not taking beta blockers, for whom 10 (50%) had biomedical reasons cited and 14 (70%) had contextual reasons cited.
The most common type of contextual reason for not prescribing was co-management with other clinicians (Figure 1). Among the 21 patients for whom co-management was cited as a reason for nonprescribing, co-management issues occurred with non-VA clinicians (11 patients), VA clinicians (8 patients), and both (2 patients). Deferring decision-making to other clinicians and difficulty communicating with them were commonly cited as contributing factors.
Another common contextual reason for non-prescribing was patient attitudes toward medication use and non-adherence, cited in 12 (24%) not taking ACE-I/ARBs and 3 (15%) not taking beta blockers (2 patients were prescribed neither drug). For at least 9 of these 13 patients, clinicians invoked patients’ general dislike of medications, non-adherence, and lack of followup as reasons for non-prescribing.
Most clinicians felt confident that they made the correct decision in not prescribing ACE-I/ARBs or beta blockers: 49 of 57 (86%) clinicians answering this question stated that they were moderately or very confident about their decision not to prescribe.
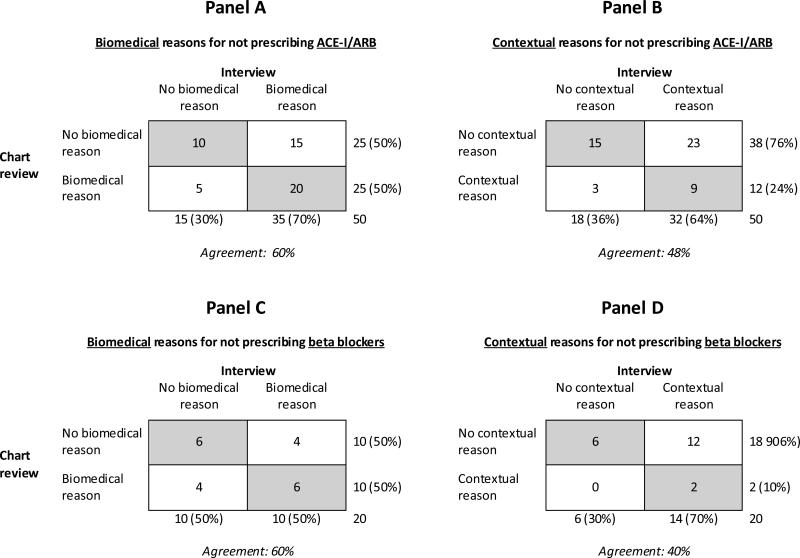
Agreement between reasons for non-prescribing identified by chart review and by interview
There was imperfect agreement between the types of reasons for non-prescribing identified by chart review and by interview (Figure 2). This lack of agreement reflected limited sensitivity of the chart for identifying reasons for non-prescribing – but also situations where the chart identified reasons that were not elicited in the interview. This included situations where the interviewed clinician did not appear to be aware of reasons for non-prescribing that other clinicians had clearly documented in the medical record (see Appendix, supplemental digital content 2).
Figure 2. Correspondence between reasons for non-prescribing identified in interviews vs. by chart review.
The panels show the correspondence between reasons for non-prescribing identified in structured chart review and clinician interviews for 62 patients (50 not prescribing ACE-I/ARB and 20 not prescribed beta blockers, with 8 patients prescribed neither medication). Panels A and B show the correspondence of reasons for not prescribing ACE-I/ARBs identified in chart review and interviews. Panels C and D show the correspondence of reasons from chart review and interviews for not prescribing beta blockers.
DISCUSSION
In this study, both biomedical and contextual factors were commonly invoked as reasons for not prescribing ACE-Is, ARBs, and beta blockers to veterans with heart failure. Clinicians commonly documented in the medical record that they were withholding these medications due to biomedical contraindications. Contextual reasons for withholding therapy were documented much less frequently, being invoked in 11-17% of patients not receiving these medications. Yet, when clinicians were directly asked in an interview setting, contextual reasons for not prescribing ACE-I/ARBs and beta blockers were cited in up to 70% of patients not receiving these drugs.
The low rate at which contextual factors were documented in the medical record is not surprising, given similar findings from prior studies.1, 3, 5-6, 21-23 However, it has been difficult to determine to what extent these contextual factors are truly uncommon or are simply undocumented.19, 24-25 Our findings from clinician interviews that contextual factors were responsible for as much non-prescribing as biomedical factors suggests that performance measurement systems, most of which focus on biomedical exceptions, address only half of the issue of non-prescribing of guideline-recommended medications. This fosters a misalignment of physician incentives to provide context-sensitive care.
Our results add credence to the argument that efforts to improve care quality should place greater attention on contextual factors. One potential strategy is to develop performance measurement systems that allow physicians to directly report both biomedical and contextual exceptions in a seamless and clinically sensible manner.26 These strategies have been largely successful in the United Kingdom's Quality and Outcomes Framework and U.S. Medicare's Physician Quality Reporting System. In these settings, exceptions have been identified in a substantial proportion of patients who otherwise would fail to meet performance targets, with little evidence that clinicians are abusing the system.2-9, 13, 26
While direct exception reporting could help to better assess quality of care, the most important use of such systems may be providing a means to improve care.14-15, 27 Most biomedical and contextual contraindications to medication therapy are relative, not absolute. Exception reporting may thus work best when tied to programs that can address the underlying barrier. For example, reporting in an electronic system that a patient is not prescribed a beta blocker due to COPD could call up educational materials and a treatment algorithm to help physicians prescribe in these challenging settings, and if necessary facilitate referral to a specialty clinic. Reporting of co-management issues could trigger mechanisms to facilitate better communication between clinicians. Such granular information could also support point-of-care systems to help individualize guideline recommendations according to the clinical circumstances and goals of individual patients.20, 28-30
Our study has several limitations. The VA has its own electronic medical record and performance measurement systems, and serves a predominantly male and socioeconomically disadvantaged population.31 However, VA provides care to more than 6% of older Americans,32-33 and the multisite nature of this study supports the generalizability of the findings. It is also important to note that we did not attempt to judge the appropriateness of reasons for non-prescribing. Our results should be interpreted as identifying reasons cited by clinicians for not following guidelines and not the actual quality of care these patients received. Finally, our study focused on patients who were regular users of VA care. Substantial numbers of patients with heart failure may fail to receive guideline-recommended medications because they have limited access to health care, representing an important (but different) focus for improving care quality.
Measuring and improving quality of care needs to account for the full range of reasons why patients may not receive guideline-recommended care, not just those which are convenient to measure or relate to biomedical factors. It is imperative to find better ways of measuring and addressing these contextual reasons, both to recognize when they are appropriate reasons for withholding therapy from a patient, and to remedy barriers that may be overcome to provide patients high-quality care.
Supplementary Material
ACKNOWLEDGEMENTS
Support: Supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (IIR 06-080-02 and CHF QUERI-04-326) and by the National Institute on Aging and the American Federation for Aging Research (1K23-AG030999)
The funders had no role in study design, data collection, analysis, interpretation, or the decision to publish this manuscript.
Footnotes
Disclosure
The authors do not have any conflicts of interest or financial relationships related to the content of this manuscript. The lead author had full access to and takes full responsibility for the integrity of the data. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Michael A. Steinman, HSR&D Research Enhancement Award Program, San Francisco VA Medical Center and the University of California, San Francisco; San Francisco VA Medical Center Box 181G; 4150 Clement St; San Francisco, CA 94121.
Liezel Dimaano, University of California, San Francisco; c/o UCSF School of Medicine, Dean's Office; 513 Parnassus Ave; San Francisco, CA 94143-0410; Liezel.Dimaano@ucsf.edu.
Carolyn A. Peterson, Department of Psychology, University of Oregon ; Straub Hall 1227; University of Oregon; Eugene, OR 97403; carolynapeterson@yahoo.com.
Paul A. Heidenreich, Palo Alto VA Health Care System and Stanford University; VA Palo Alto Medical Center; 111C Cardiology; 3801 Miranda Avenue; Palo Alto, CA 94304; Paul.Heidenreich@va.gov.
Sara J. Knight, VA HSR&D Service and Associate Professor of Psychiatry and Urology, University of California, San Francisco; VA HSR&D Central Office; 810 Vermont Ave., NW; Washington, DC, 20420; sara.knight@va.gov.
Kathy Z. Fung, San Francisco VA Medical Center; San Francisco VA Medical Center, Box 181G; 4150 Clement St; San Francisco, CA 94121; kathy.fung@va.gov.
Peter J. Kaboli, Comprehensive Access and Delivery Research and Evaluation (CADRE) Center, Iowa City VA Healthcare System and the University of Iowa Carver College of Medicine; Iowa City VA Medical Center; 601 Highway 6 West; Iowa City, IA 52246-2208; Peter.Kaboli@va.gov.
REFERENCES
- 1.Baker DW, Persell SD, Thompson JA, et al. Automated review of electronic health records to assess quality of care for outpatients with heart failure. Ann Intern Med. 2007 Feb 20;146(4):270–277. doi: 10.7326/0003-4819-146-4-200702200-00006. [DOI] [PubMed] [Google Scholar]
- 2.Persell SD, Dolan NC, Friesema EM, Thompson JA, Kaiser D, Baker DW. Frequency of inappropriate medical exceptions to quality measures. Ann Intern Med. 2010 Feb 16;152(4):225–231. doi: 10.7326/0003-4819-152-4-201002160-00007. [DOI] [PubMed] [Google Scholar]
- 3.Kmetik KS, O'Toole MF, Bossley H, et al. Exceptions to outpatient quality measures for coronary artery disease in electronic health records. Ann Intern Med. 2011 Feb 15;154(4):227–234. doi: 10.7326/0003-4819-154-4-201102150-00003. [DOI] [PubMed] [Google Scholar]
- 4.Steinman MA, Harlow JB, Massie BM, Kaboli PJ, Fung KZ, Heidenreich PA. Age and receipt of guideline-recommended medications for heart failure: a nationwide study of veterans. J Gen Intern Med. 2011 Oct;26(10):1152–1159. doi: 10.1007/s11606-011-1745-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kerr EA, Smith DM, Hogan MM, et al. Building a better quality measure: are some patients with ‘poor quality’ actually getting good care? Med Care. 2003 Oct;41(10):1173–1182. doi: 10.1097/01.MLR.0000088453.57269.29. [DOI] [PubMed] [Google Scholar]
- 6.Persell SD, Wright JM, Thompson JA, Kmetik KS, Baker DW. Assessing the validity of national quality measures for coronary artery disease using an electronic health record. Arch Intern Med. 2006 Nov 13;166(20):2272–2277. doi: 10.1001/archinte.166.20.2272. [DOI] [PubMed] [Google Scholar]
- 7.Doran T, Fullwood C, Reeves D, Gravelle H, Roland M. Exclusion of patients from pay-for-performance targets by English physicians. N Engl J Med. 2008 Jul 17;359(3):274–284. doi: 10.1056/NEJMsa0800310. [DOI] [PubMed] [Google Scholar]
- 8. [December 6, 2012];Physician Consortium for Performance Improvement (PCPI). Physician Consortium for Performance Improvement (PCPI) position statement. Specification and categorization of measure exclusions: Recommendations to PCPI work groups. 2008 http://www.amaassn.org/resources/doc/cqi/exclusions053008.pdf.
- 9.Doran T, Kontopantelis E, Fullwood C, Lester H, Valderas JM, Campbell S. Exempting dissenting patients from pay for performance schemes: retrospective analysis of exception reporting in the UK Quality and Outcomes Framework. BMJ. 2012;344:e2405. doi: 10.1136/bmj.e2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jha AK, Joynt KE, Orav EJ, Epstein AM. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med. 2012 Apr 26;366(17):1606–1615. doi: 10.1056/NEJMsa1112351. [DOI] [PubMed] [Google Scholar]
- 11.Center for Medicare and Medicaid Services [December 6, 2012];Physician Quality Reporting System. 2012 http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.html.
- 12.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003 May 29;348(22):2218–2227. doi: 10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- 13.Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006 Jul 27;355(4):375–384. doi: 10.1056/NEJMsa055505. [DOI] [PubMed] [Google Scholar]
- 14.Weiner SJ, Schwartz A, Weaver F, et al. Contextual errors and failures in individualizing patient care: a multicenter study. Ann Intern Med. 2010 Jul 20;153(2):69–75. doi: 10.7326/0003-4819-153-2-201007200-00002. [DOI] [PubMed] [Google Scholar]
- 15.Fraenkel L, Fried TR. Individualized medical decision making: necessary, achievable, but not yet attainable. Arch Intern Med. 2010 Mar 22;170(6):566–569. doi: 10.1001/archinternmed.2010.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andrus MR, Loyed JV. Use of beta-adrenoceptor antagonists in older patients with chronic obstructive pulmonary disease and cardiovascular co-morbidity: safety issues. Drugs Aging. 2008;25(2):131–144. doi: 10.2165/00002512-200825020-00005. [DOI] [PubMed] [Google Scholar]
- 17.Viswanathan M, Golin CE, Jones CD, et al. Interventions to Improve Adherence to Self-administered Medications for Chronic Diseases in the United States: A Systematic Review. Ann Intern Med. 2012 Sep 11; doi: 10.7326/0003-4819-157-11-201212040-00538. [DOI] [PubMed] [Google Scholar]
- 18.Steinman MA, Sudore RL, Peterson CA, Harlow JB, Fried TR. Influence of patient age and comorbid burden on clinician attitudes toward heart failure guidelines. Am J Geriatr Pharmacother. 2012 Jun;10(3):211–218. doi: 10.1016/j.amjopharm.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steinman MA, Patil S, Kamat P, Peterson C, Knight SJ. A taxonomy of reasons for not prescribing guideline-recommended medications for patients with heart failure. Am J Geriatr Pharmacother. 2010 Dec;8(6):583–594. doi: 10.1016/S1543-5946(10)80007-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kerr EA, Lucatorto MA, Holleman R, Hogan MM, Klamerus ML, Hofer TP. Monitoring performance for blood pressure management among patients with diabetes mellitus: too much of a good thing? Arch Intern Med. 2012 Jun 25;172(12):938–945. doi: 10.1001/archinternmed.2012.2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bart BA, Gattis WA, Diem SJ, O'Connor CM. Reasons for underuse of angiotensin-converting enzyme inhibitors in patients with heart failure and left ventricular dysfunction. Am J Cardiol. 1997 Apr 15;79(8):1118–1120. doi: 10.1016/s0002-9149(97)00060-x. [DOI] [PubMed] [Google Scholar]
- 22.Bertoni AG, Duren-Winfield V, Ambrosius WT, et al. Quality of heart failure care in managed Medicare and Medicaid patients in North Carolina. Am J Cardiol. 2004 Mar 15;93(6):714–718. doi: 10.1016/j.amjcard.2003.11.053. [DOI] [PubMed] [Google Scholar]
- 23.Kerr EA, Krein SL, Vijan S, Hofer TP, Hayward RA. Avoiding pitfalls in chronic disease quality measurement: a case for the next generation of technical quality measures. Am J Manag Care. 2001 Nov;7(11):1033–1043. [PubMed] [Google Scholar]
- 24.Phillips SM, Marton RL, Tofler GH. Barriers to diagnosing and managing heart failure in primary care. Med J Aust. 2004 Jul 19;181(2):78–81. doi: 10.5694/j.1326-5377.2004.tb06178.x. [DOI] [PubMed] [Google Scholar]
- 25.Fuat A, Hungin AP, Murphy JJ. Barriers to accurate diagnosis and effective management of heart failure in primary care: qualitative study. Bmj. 2003 Jan 25;326(7382):196. doi: 10.1136/bmj.326.7382.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDonald R, Roland M. Pay for performance in primary care in England and California: comparison of unintended consequences. Ann Fam Med. 2009 Mar-Apr;7(2):121–127. doi: 10.1370/afm.946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heisler M, Hogan MM, Hofer TP, Schmittdiel JA, Pladevall M, Kerr EA. When more is not better: treatment intensification among hypertensive patients with poor medication adherence. Circulation. 2008 Jun 3;117(22):2884–2892. doi: 10.1161/CIRCULATIONAHA.107.724104. [DOI] [PubMed] [Google Scholar]
- 28.Eddy DM, Adler J, Patterson B, Lucas D, Smith KA, Morris M. Individualized guidelines: the potential for increasing quality and reducing costs. Ann Intern Med. 2011 May 3;154(9):627–634. doi: 10.7326/0003-4819-154-9-201105030-00008. [DOI] [PubMed] [Google Scholar]
- 29.O'Connor PJ. Adding value to evidence-based clinical guidelines. Jama. 2005 Aug 10;294(6):741–743. doi: 10.1001/jama.294.6.741. [DOI] [PubMed] [Google Scholar]
- 30.Kent DM, Hayward RA. Limitations of applying summary results of clinical trials to individual patients: the need for risk stratification. JAMA. 2007 Sep 12;298(10):1209–1212. doi: 10.1001/jama.298.10.1209. [DOI] [PubMed] [Google Scholar]
- 31.Nelson KM, Starkebaum GA, Reiber GE. Veterans using and uninsured veterans not using Veterans Affairs (VA) health care. Public Health Rep. 2007 Jan-Feb;122(1):93–100. doi: 10.1177/003335490712200113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Federal Interagency Forum on Aging Related Statistics [December 6, 2012];Indicator 29. Use of health care services. http://www.agingstats.gov/Main_Site/Data/2012_Documents/Health_Care.aspx.
- 33.United States Census Bureau [December 6, 2012];Table 7. Resident population by sex and age: 1980 to 2010. http://www.census.gov/compendia/statab/2012/tables/12s0007.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.