Diabetic nephropathy is a major complication of both type 1 and type 2 diabetes and the leading cause of end-stage renal disease worldwide. Strict glycemic control and renin-angiotensin system inhibition delay the progression of diabetic nephropathy but do not prevent end-stage renal disease. Thus, identification of novel pathogenic mechanisms and targetable pathways is needed to change the outcome of the disease.
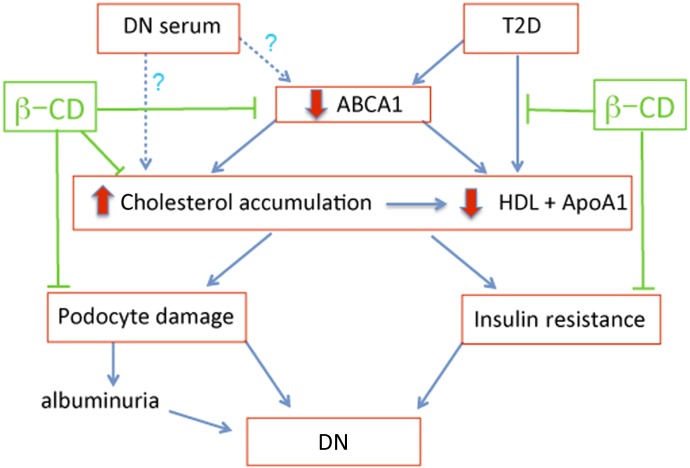
In this issue, Merscher-Gomez et al. (1) report that cholesterol accumulation in podocytes plays a pathogenic role in diabetic nephropathy and provide evidence of the beneficial effect of targeting this pathway. Using a cell assay, the authors show that serum from patients with diabetic nephropathy (as opposed to that of diabetic patients without nephropathy) induces abnormal accumulation of cholesterol in human podocytes in culture, which is associated with downregulation of the cholesterol transporter ABCA1, increased apoptosis, cell blebbing, and loss of caveolin phosphorylation. Notably, these changes are prevented by exposure to methyl-β-cyclodextrin (methyl-β-CD), an oligosaccharide that mobilizes cholesterol from lipid rafts. Microarray and PCR analysis of human biopsies from a cohort of type 2 diabetic patients confirmed ABCA1 downregulation in diabetic nephropathy. In addition, Merscher-Gomez et al. used a type 2 diabetic mouse model carrying homozygous leptin mutation on insulin-resistant genetic background (BTBR: ob/ob) (2) to target this pathway, and found that long-term parenteral methyl-β-CD administration improves albuminuria and mesangial expansion, as well as insulin resistance and obesity (Fig. 1).
FIG. 1.
Exposure to serum from diabetic nephropathy (DN) patients or type 2 diabetic (T2D) patients induces ABCA1 downregulation, cholesterol accumulation, podocyte damage, and insulin resistance leading to albuminuria and DN progression. Methyl-β-CD (β-CD) causes cholesterol efflux, prevents podocyte damage, and rescues the insulin secretion defect. ApoA1, apolipoprotein A1.
Cholesterol is synthesized from acetyl-coenzyme A by most cells and imported from circulating LDL by receptor-mediated endocytosis. Unlike fatty acid metabolism, cholesterol is not oxidized completely to carbon dioxide; instead, it is actively transported out of the cell by ATP-binding cassette transporters A1 (ABCA1) and G1 (ABCG1). ABCA1, a major regulator of cholesterol homeostasis, mediates cholesterol efflux from endothelial cells, β-cells, adipocytes, and podocytes to circulating apolipoprotein acceptors (HDL) (1,3,4). HDL completes the so-called reverse cholesterol transport by delivering cholesterol to the liver, where it can be secreted into bile and excreted in the feces (3). Loss-of-function mutations of ABCA1 cause Tangier disease, an extremely rare recessive disorder associated with HDL deficiency and accelerated atherosclerosis (5). Humans with heterozygous ABCA1 mutations have HDL deficiency and abnormal β-cell function due to impaired glucose-stimulated insulin secretion (6). ABCA1-deficient mice mimic the human phenotype and show defects in caveolae processing and budding from the Golgi network, where caveolin 1 is retained (7). ABCA1 deficiency in β-cells leads to impaired insulin granule exocytosis and impaired proinsulin processing (8,9). ABCA1 localizes to caveolae and interacts with caveolin 1 (10). Moreover, caveolin 1 is a positive regulator of ABCA1 function that increases cholesterol trafficking to the plasma membrane, thereby enhancing cholesterol efflux (11); in turn, ABCA1 induces caveolin 1 phosphorylation. The scaffolding domain of caveolin 1 interacts with multiple signaling proteins anchored in caveolae: nitric oxide synthase, G-coupled protein receptors, Src family kinases, and receptor tyrosine kinases, including the insulin receptor (12). Caveolin-1 amplifies insulin signaling by preventing proteasomal degradation of the insulin receptor and modulating GLUT transporter function (12). Caveolin-1–deficient mice develop insulin resistance, illustrating its important role in energy metabolism (13).
Abnormalities in lipid metabolism and lipid accumulation in the diabetic kidney are well described, including cholesterol accumulation and ABCA1 downregulation (14,15). These changes are thought to contribute to diabetic nephropathy progression through ROS, vascular endothelial growth factor, and transforming growth factor-β pathways (14). Downregulation of ABCA1 has also been detected in leukocytes and macrophages from type 2 diabetic patients, correlating with hyperglycemia, HgA1c, and HDL levels (16). The benefit of cholesterol synthesis inhibition (statins) on diabetic nephropathy progression rate is considered modest at best. Merscher-Gomez et al. (1) targeted cholesterol accumulation in human podocytes by stimulating cholesterol efflux, thereby probably modulating signaling in caveolae, where caveolin-1, ABCA1, and insulin receptors (as well as other signaling molecules) physically and functionally interact, resulting in improved podocyte and diabetic nephropathy phenotype (Fig. 1). Cyclodextrins are cyclic oligosaccharides with a hydrophilic outer surface and a relatively hydrophobic central cavity that function as potent artificial cholesterol acceptors. The number of sugar rings (α = 6, β = 7, γ = 8) determines the hydrophobic cavity size, while hydroxyl and methyl modifications influence their binding kinetics and cytotoxicity (17). β-Cyclodextrins form dimers and inclusion complexes with cholesterol, allowing manipulation of cholesterol in biomembranes (18,19). Methyl-β-CD increases cholesterol efflux from cells rapidly without large changes in the cell membrane bilayer structure, although decreased invagination of clathrin-coated pits and flattening of caveolae, which were reversible, were detected by electron microscopy (20). Exposure of pancreatic β-cells to methyl-β-CD increases glucose-induced insulin exocytosis without altering insulin sensitivity (21), as shown by Merscher-Gomez et al. (1) using human islets. Moreover, cholesterol depletion with methyl-β-CD rescues the insulin exocytosis defect in β-cells lacking ABCA1, suggesting that cholesterol accumulation is directly responsible for the β-cell insulin secretion defect (9). Cyclodextrins are used in the food industry as emulsifiers and by the pharmaceutical industry as excipients aimed to increase aqueous solubility, oral absorption of hydrophobic drugs, and drug delivery, although they may also reduce the apparent permeability of the drug, a so-called solubility–permeability interplay (22). Hydroxy- and methyl-β-CDs are considered nontoxic for rodents, dogs, and humans; are well tolerated (23); and have received FDA approval for the treatment of Niemann-Pick and Tangier diseases. α-Cyclodextrin was shown to induce modest weight loss in obese type 2 diabetic and in overweight nondiabetic patients, associated with modest but significant decreases in total cholesterol, LDL, apolipoprotein A, and insulin levels without change in glycemia (24).
Although the findings by Merscher-Gomez et al. (1) suggesting that methyl-β-CD may be a useful treatment for diabetic nephropathy are promising, identification of the diabetic nephropathy patients’ serum component that elicits cholesterol accumulation in podocytes (β-cells and others) remains elusive. Further mechanistic studies are needed to understand how methyl-β-CD–mediated cholesterol removal alters specific cell functions, signaling pathways, caveolae-dependent internalization, and clathrin-dependent endocytosis. Such studies will be informative on pleiotropic effects of cyclodextrins, potential toxic effects, and for novel drug designs. Given that methyl-β-CDs may remove cholesterol from both raft and nonraft domains of cell membranes, as well as alter intracellular membranes and plasma cholesterol distribution (19,25), in vivo pharmacodynamics and functional effects should also be determined in acute and long-term settings, including advanced diabetic nephropathy, for safety concerns.
ACKNOWLEDGMENTS
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 3817.
REFERENCES
- 1.Merscher-Gomez S, Guzman J, Pedigo CE, et al. FinnDiane Study Group Cyclodextrin protects podocytes in diabetic kidney disease. Diabetes 2013;62:3817–3827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hudkins KL, Pichaiwong W, Wietecha T, et al. BTBR ob/ob mutant mice model progressive diabetic nephropathy. J Am Soc Nephrol 2010;21:1533–1542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Attie AD. ABCA1: at the nexus of cholesterol, HDL and atherosclerosis. Trends Biochem Sci 2007;32:172–179 [DOI] [PubMed]
- 4.Wang N, Silver DL, Thiele C, Tall AR. ATP-binding cassette transporter A1 (ABCA1) functions as a cholesterol efflux regulatory protein. J Biol Chem 2001;276:23742–23747 [DOI] [PubMed]
- 5.Bodzioch M, Orsó E, Klucken J, et al. The gene encoding ATP-binding cassette transporter 1 is mutated in Tangier disease. Nat Genet 1999;22:347–351 [DOI] [PubMed] [Google Scholar]
- 6.Vergeer M, Brunham LR, Koetsveld J, et al. Carriers of loss-of-function mutations in ABCA1 display pancreatic beta-cell dysfunction. Diabetes Care 2010;33:869–874 [DOI] [PMC free article] [PubMed]
- 7.Orsó E, Broccardo C, Kaminski WE, et al. Transport of lipids from Golgi to plasma membrane is defective in tangier disease patients and Abc1-deficient mice. Nat Genet 2000;24:192–196 [DOI] [PubMed] [Google Scholar]
- 8.Brunham LR, Kruit JK, Pape TD, et al. Beta-cell ABCA1 influences insulin secretion, glucose homeostasis and response to thiazolidinedione treatment. Nat Med 2007;13:340–347 [DOI] [PubMed] [Google Scholar]
- 9.Kruit JK, Wijesekara N, Fox JE, et al. Islet cholesterol accumulation due to loss of ABCA1 leads to impaired exocytosis of insulin granules. Diabetes 2011;60:3186–3196 [DOI] [PMC free article] [PubMed]
- 10.Lin YC, Ma C, Hsu WC, Lo HF, Yang VC. Molecular interaction between caveolin-1 and ABCA1 on high-density lipoprotein-mediated cholesterol efflux in aortic endothelial cells. Cardiovasc Res 2007;75:575–583 [DOI] [PubMed] [Google Scholar]
- 11.Fu Y, Hoang A, Escher G, Parton RG, Krozowski Z, Sviridov D. Expression of caveolin-1 enhances cholesterol efflux in hepatic cells. J Biol Chem 2004;279:14140–14146 [DOI] [PubMed] [Google Scholar]
- 12.Cohen AW, Combs TP, Scherer PE, Lisanti MP. Role of caveolin and caveolae in insulin signaling and diabetes. Am J Physiol Endocrinol Metab 2003;285:E1151–E1160 [DOI] [PubMed] [Google Scholar]
- 13.Cohen AW, Razani B, Wang XB, et al. Caveolin-1-deficient mice show insulin resistance and defective insulin receptor protein expression in adipose tissue. Am J Physiol Cell Physiol 2003;285:C222–C235 [DOI] [PubMed] [Google Scholar]
- 14.Proctor G, Jiang T, Iwahashi M, Wang Z, Li J, Levi M. Regulation of renal fatty acid and cholesterol metabolism, inflammation, and fibrosis in Akita and OVE26 mice with type 1 diabetes. Diabetes 2006;55:2502–2509 [DOI] [PubMed] [Google Scholar]
- 15.Zhou H, Tan KC, Shiu SW, Wong Y. Cellular cholesterol efflux to serum is impaired in diabetic nephropathy. Diabetes Metab Res Rev 2008;24:617–623 [DOI] [PubMed] [Google Scholar]
- 16.Patel DC, Albrecht C, Pavitt D, et al. Type 2 diabetes is associated with reduced ATP-binding cassette transporter A1 gene expression, protein and function. PLoS One 2011;6:e22142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kiss T, Fenyvesi F, Bácskay I, et al. Evaluation of the cytotoxicity of beta-cyclodextrin derivatives: evidence for the role of cholesterol extraction. Eur J Pharm Sci 2010;40:376–380 [DOI] [PubMed] [Google Scholar]
- 18.López CA, de Vries AH, Marrink SJ. Molecular mechanism of cyclodextrin mediated cholesterol extraction. PLOS Comput Biol 2011;7:e1002020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.López CA, de Vries AH, Marrink SJ. Computational microscopy of cyclodextrin mediated cholesterol extraction from lipid model membranes. Sci Rep 2013;3:2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodal SK, Skretting G, Garred O, Vilhardt F, van Deurs B, Sandvig K. Extraction of cholesterol with methyl-beta-cyclodextrin perturbs formation of clathrin-coated endocytic vesicles. Mol Biol Cell 1999;10:961–974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hao M, Head SW, Gunawardana SC, et al. Direct effect of cholesterol in insulin secretion: a novel mechanism for pancreatic beta-cell dysfunction. Diabetes 2007;56:2328–2338 [DOI] [PubMed] [Google Scholar]
- 22.Beig A, Agbaria R, Dahan A. Oral delivery of lipophilic drugs: the tradeoff between solubility increase and permeability decrease when using cyclodextrin-based formulations. PLoS One 2013;8:e68237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gould S, Scott RC. 2-Hydroxypropyl-beta-cyclodextrin (HP-beta-CD): a toxicology review. Food Chem Toxicol 2005;43:1451–1459 [DOI] [PubMed] [Google Scholar]
- 24.Comerford KB, Artiss JD, Jen KL, Karakas SE. The beneficial effects of α-cyclodextrin on blood lipids and weight loss in healthy humans. Obesity (Silver Spring) 2011;19:1200–1204 [DOI] [PubMed] [Google Scholar]
- 25.Zidovetzki R, Levitan I. Use of cyclodextrins to manipulate plasma membrane cholesterol content: evidence, misconceptions and control strategies. Biochim Biophys Acta 2007;1768:1311–1324 [DOI] [PMC free article] [PubMed]