Abstract
Children with attention-deficit/hyperactivity disorder (ADHD) are at increased risk for the development of depression, with evidence that peer and academic difficulties mediate predictions of later depression from ADHD. The present study hypothesized that parent-child relationship difficulties may be an additional potential mediator of this association. Academic, peer, and parent-child functioning were tested as mediators of the association of attention problems and depression in two distinctly different, yet complementary samples. Study 1 was a cross-sectional sample of 230 5–10 year-old children with and without ADHD. Study 2 was a prospective longitudinal sample of 472 youth followed prospectively from birth to age 20 at risk for depression. Despite differences in age, measures, and designs, both studies implicated peer and parent-child problems as unique mediators of depressive symptoms, although academic difficulties did not uniquely mediate the ADHD-depression association. Further, inattention symptoms, but not hyperactivity, predicted depressive symptoms via the disruption of interpersonal functioning. The inclusion of oppositional defiant disorder into models impacted results, and supported its independent role in parent-child problems. Implications include support for interventions that target interpersonal competence, which may effectively reduce the risk of depression among children with ADHD.
Keywords: ADHD, depression, peer problems, peer rejection, parent-child relationship
The association between attention-deficit/hyperactivity disorder (ADHD) and depression has been well-documented across epidemiological and clinical samples of children and adolescents (e.g., Anderson, Williams, McGee, & Silva, 1987; Biederman, Newcorn, & Sprich, 1991; Biederman et al., 2008). Given that ADHD typically precedes the onset of depression (American Psychiatric Association, 2000), studies of the association of ADHD and depression have focused on ADHD-related impairments or failure-related mediators (i.e., academic and peer failure), such that depression may follow from ADHD-related demoralization (Biederman, Mick, & Faraone, 1998). The dual-failure model proposes that both academic and peer problems, resulting from disruptive behavior problems, contribute to the development of depression (e.g., Patterson & Stoolmiller, 1991). Similar to the dual-failure model, Cole’s (1990) competency based model asserts that negative feedback obtained from failure is a pathway to depression.
Children with ADHD typically fare worse academically and socially than their non-ADHD counterparts (e.g., Hoza, Waschbusch, Owens, Pelham, & Kipp, 2001), and attention problems typically precede academic problems (e.g., Smart, Sanson, & Prior, 1996). Academic problems mediated the association of attention problems with depression measured two years later, even after controlling for baseline conduct problems and academic performance (Herman, Lambert, Ialongo, & Ostrander, 2007). Peer relationships are also reliably disrupted in children with ADHD (Henker & Whalen, 1999), and approximately half of children from the Multimodal Treatment Study of Children with ADHD were sociometrically rejected (Hoza et al., 2005). Both academic and peer impairment are known to predict depressive symptoms (e.g., McCarty et al., 2008; Seroczynski, Cole, & Maxwell, 1997). In children ages 6–9, others’ appraisals of social competence were found to mediate the association of ADHD and depression (Ostrander, Crystal & August, 2006).
Interpersonal difficulties, defined broadly, are associated with risk for depression across development (e.g., Rudolph et al., 2000). Thus, in addition to peer relationships, the parent-child relationship may be relevant to depression risk in children with ADHD. The majority of extant research on parent-child relationships and child outcomes focused primarily on its association with ADHD symptoms, rather than the development of psychopathology in other domains. In one notable exception, Ostrander and Herman (2006) found that parent management, a measure of parenting behavior, fully explained the association between ADHD and depression in young children, but not in older children.
Families of children with ADHD are characterized by poor parent-child relationships, including greater conflict, problematic child behavior, and poorer parenting practices (Barkley, Fischer, Edelbrock, & Smallish, 1991; Johnston & Mash, 2001). Children with ADHD are also thought to require greater parental effort than those without ADHD (Barkley, Anastopoulos, Guevremont, & Fletcher, 1992), which may disrupt normative parenting behavior (Anastopoulos, Shelton, DuPaul, & Guevremont, 1993). Longitudinal evidence suggests that child ADHD may precede both parent-child rejection and hostility (Lifford, Harold, & Thapar, 2008; 2009), and problematic parent-child interactions, specifically, have uniquely predicted depression and antisocial behavior (Eberhart & Hammen, 2006; Patterson, DeBaryshe, & Ramsey, 1989). There is also evidence that parent-child problems increase the risk for depression among children with ADHD (Johnston & Mash, 2001; Ostrader & Herman, 2006).
Because ADHD is associated with multiple domains of impairment, multiple potential mediators must be evaluated simultaneously. In particular, the parent-child relationship has been largely omitted in understanding the progression from ADHD to depression. Accordingly, the present investigation addressed these concerns directly by examining the role of three potential mediators in the association between ADHD and depression. Specifically, we used structural equation modeling (SEM) to examine whether ADHD symptoms predicted academic problems, peer problems, and parent-child problems, and whether these three facets further predicted individual differences in depressive symptoms. To our knowledge, this is the first study to use SEM and multiple mediation to examine the independent effect of each mediator. In addition, to more clearly examine the independent role of attention problems over and above oppositional defiant disorder (ODD), secondary models included both ADHD and ODD/aggression factors, given their frequent overlap (Biederman et al., 1991) and the association of ODD with poorer interpersonal functioning and increased depression risk (Capaldi, 1991; Panak & Garber, 1992).
Study 1 consisted of a cross-sectional sample of children ages 5–10, oversampled for children who met full diagnostic criteria for ADHD. This sample yielded multi-method measures of ADHD symptom dimensions that permitted separate examination of the role of inattention vs. hyperactivity in their association with depressive symptoms. Previous studies of ADHD and depression have typically ignored this distinction, even when examined dimensionally (e.g., Seymour et al., 2012). This may mask important differences in symptom domains (e.g., inattention was a better predictor of internalizing problems than hyperactivity [Willcutt et al., 2012]). Study 2 is a prospective longitudinal study of the offspring of depressed and never-depressed mothers, and thus constitutes an enriched sample of individuals at high risk for depression. This large sample allowed testing of whether childhood attention problems conferred risk for interpersonal difficulties in adolescence and, in turn, depression in the transition to adulthood. These time points are significant developmentally as adolescent interpersonal difficulties are known predictors of psychosocial problems (e.g., poorer romantic relationship quality; Katz, Hammen, & Brennan, 2013) and psychopathology (e.g., depression; Eberhart & Hammen, 2006). Furthermore, age 20 was an appropriate age for assessing depression as the twenties is a common age range for initial onset of major depression (Kessler et al., 2010). Additionally, given the known sex differences in ADHD prevalence (Szatmari, Offord, & Boyle, 1989), as well as sex differences in depression prevalence (Piccinelli & Wilkinson, 2000), we included sex as both a covariate in our analyses and a moderator of associations in our final models.
Study 1
Method
Participants
Recruitment and procedures for this sample have been described previously (Humphreys, Mehta, Lee, 2012; Shemmassian & Lee, 2012). In brief, two hundred thirty children with (n = 120) and without (n = 110) ADHD, ages 5–10 (M = 7.39, SD = 1.12), 71% male, and their families, were recruited. Forty-seven percent of the sample was Caucasian, 8% African-American, 9% Hispanic, 3% Asian, 21% mixed, and 12% as Other or missing. All study procedures were approved by the UCLA Institutional Review Board.
Measures
Diagnostic Interview Schedule for Children, 4th edition (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000)
We administered the computerized DISC-IV to each parent. We separately analyzed the 18 Diagnostic and Statistical Manual for Mental Disorders (DSM-IV) ADHD symptoms (9 inattention and 9 hyperactivity). Test-retest reliability for ADHD from the DISC ranged from .51 to .64 in the DSM-IV field trials (Lahey et al., 1994), and there is strong evidence for the predictive validity and sensitivity to treatment effects of the DISC-IV (Pelham, Fabiano, & Massetti, 2005). The DISC also provided the number of ODD symptoms endorsed (0–8).
Disruptive Behavior Disorder Rating Scale (DBD; Pelham, Gnagy, Greenslade, & Milich, 1992)
Parents rated DSM-IV DBD symptoms with response options ranging from 0 for “not at all” to 3 for “very much.” The 18 symptoms that comprise DSM-IV ADHD were summed to create dimensional measures of inattention and hyperactivity symptoms, which were split into odd and even item scales. The eight ODD symptoms were also obtained via the DBD rating scale and split into odd and even item scales. Evidence of validity of the DBD has been shown in previous studies of school-age children with ADHD (Owens & Hoza, 2003).
Child Behavior Checklist 6–18 (CBCL; Achenbach & Rescorla, 2001)
The 113-item rating scale completed by the parent yielded measures of child psychopathology. Responses were scored on a 3-point scale, from 0 for “not true” to 2 for “very true or often true.” The CBCL was normed on a large sample of children ages 6–18 and possesses excellent test-retest and interrater reliability, as well as adequate to excellent internal consistency (Achenbach & Rescorla, 2001). We utilized the total score from the withdrawn/depressed narrow-band subscale as our measures of depression. This scale has been shown to have adequate internal consistency and test-retest reliability (Achenbach & Rescorla, 2001), and discriminated youths with major depressive disorder or dysthymia from youths without these diagnoses (Ebesutani et al., 2010).
The Wechsler Individual-Achievement Test - Second Edition (WIAT-II; Wechsler 2002)
The Word Reading and Math Reasoning subtests of the WIAT-II were utilized to estimate academic achievement. The Word Reading subtest assesses phonemic awareness and reading fluency whereas Math Reasoning assesses computational knowledge and the calculation of word problems. Standard scores for both subtests were z-scored and summed to create a composite measure of academic achievement.
Dishion Social Preference Scale (Dishion, 1990)
This is a three-item (five-point metric) parent-completed measure of peer acceptance, rejection, and being ignored. We estimated negative social preference, our measure of peer problems, by subtracting the rejection rating from the acceptance rating, which is consistent with prior work (Lee & Hinshaw, 2006; Shemmassian & Lee, 2012).
Parenting Stress Index: Short Form (PSI-SF; Abidin, 1995)
The Parent-Child Dysfunctional Interaction subscale assesses parental perception that the child does not meet expectations and that interactions with the child are not reinforcing. This subscale consists of 12 items rated from 1 for “strongly disagree” to 5 for “strongly agree.” Higher scores indicated more parent-child dysfunction. Psychometric properties for the PSI have been previously shown to be adequate (Abidin, 1995).
Data Analytic Procedures
Initial data compilation and analysis was completed using PASW (18.0) software. Our general data analytic approach consisted of SEM to assess associations among constructs that are corrected for biases attributable to random error and construct-irrelevant variance (Bollen, 1989) on standardized variables. We used SEM to simultaneously compare the unique contribution of peer problems, academic achievement, and parent-child problems as mediators of the association of ADHD and depression. Given the substantial variability in scales of the observed variables, these were converted to z-scores prior to conducting analyses to facilitate the interpretability of results. To account for non-normality in multiple variables, robust maximum likelihood procedures in Mplus (Muthén & Muthén 1998–2010) were used to obtain model estimates.
Goodness-of-fit of the initial and alternate models was assessed with the maximum-likelihood χ2 statistic, the Comparative Fit Index (CFI), the standardized root mean square residual (SRMR), and the root mean squared error of approximation (RMSEA). The CFI ranges from 0 to 1 and reflects the improvement in fit of a hypothesized model over a model of complete independence among the measured variables. Values approaching .95 or greater are desirable for the CFI. The RMSEA is a measure of fit per degrees of freedom, controlling for sample size. Values of .06 or less for RMSEA and values of .08 for SRMR indicate a relatively good fit (Hu & Bentler, 1999).
To interrogate the potential separate effects of ADHD symptoms, latent variables for inattention and hyperactivity were created. To provide a sufficient number of independent indicators for each latent variable, the two DBD symptom dimension scores were divided into odd-item and even-item composites (Kelloway, 1998). These separate indicators, along with the number of inattention and hyperactivity symptoms from the DISC, comprised the three indicators for each inattention and hyperactivity latent factor. The same procedure was used to create an ODD latent factor.
Results
Descriptive statistics and bivariate correlations among ADHD, ODD, mediator, and depression variables are presented in Table 1. Significant positive associations were observed among all measures of ADHD. Additionally, all ADHD variables showed significant positive associations with peer problems and parent-child problems, whereas four of the six ADHD variables were associated with (poorer) academic achievement. Peer problems and parent-child problems were both significantly associated with depression, whereas academic achievement was not. Five of the six ADHD variables were significantly associated with depression.
Table 1.
Correlation Matrix for Structural Equation Modeling Variables for Study 1
| Variable | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | −.09 | −.03 | −.17* | −.003 | .02 | −.07 | −.13 | −.13 | .03 | −.03 | .06 | −.06 | .13 | .11 |
| 2. Sex (Male = 1) | 1 | .10 | .17** | .10 | .05 | .08 | .15* | .14* | .08 | .14* | .11 | .04 | −.01 | −.03 |
| 3. DISC IN symptoms | 1 | .58*** | 42*** | .78*** | .79*** | .62*** | .56*** | .37*** | .38*** | .31*** | −.25*** | .32*** | .28*** | |
| 4. DISC HI symptoms | 1 | 61*** | .60*** | .58*** | .84*** | .85*** | .53*** | .63*** | .28*** | −.11 | .23*** | .13 | ||
| 5. DISC ODD symptoms | 1 | .42*** | .37*** | .51*** | .53*** | .71*** | .67*** | .24*** | .001 | .33*** | .29*** | |||
| 6. DBD IN symptom score (odd items) | 1 | .89*** | .74*** | .67*** | .49*** | .53*** | .39*** | −.29*** | .43*** | .31*** | ||||
| 7. DBD IN symptom score (even items) | 1 | .75*** | .68*** | .47*** | .52*** | .32*** | −.24*** | .35*** | .26*** | |||||
| 8. DBD HI symptom score (odd items) | 1 | .88*** | .58*** | .68*** | .32*** | −.16* | .34*** | .16* | ||||||
| 9. DBD HI symptom score (even items) | 1 | .59*** | .69*** | .32*** | −.11 | .32*** | .18** | |||||||
| 10. DBD ODD symptom score (odd items) | 1 | .81*** | .28*** | .02 | .46*** | .40*** | ||||||||
| 11. DBD ODD symptom score (even items) | 1 | .33*** | −.04 | .46*** | .31*** | |||||||||
| 12. Peer Problems | 1 | −.03 | .32*** | .36*** | ||||||||||
| 13. Academic Achievement | 1 | −.10 | −.03 | |||||||||||
| 14. Parent-Child Problems | 1 | .42*** | ||||||||||||
| 15. Depression | 1 | |||||||||||||
| Means (SD) or % | 71 % | 4.53 (3.14) | 3.39 (3.07) | 2.16 (2.39) | 6.62 (4.22) | 4.79 (3.33) | 5.50 (4.12) | 4.04 (3.39) | 3.57 (2.77) | 2.68 (2.52) | 0.96 (1.20) | 0 (0.91) | 21.56 (6.61) | 1.61 (2.01) |
Note: DISC = Diagnostic Interview Schedule for Children. IN = inattention. HI = hyperactivity/impulsivity. DBD = Disruptive Behavior Disorder Rating Scale.
p < .05.
p < .01.
p < .001.
Proposed Structural Model
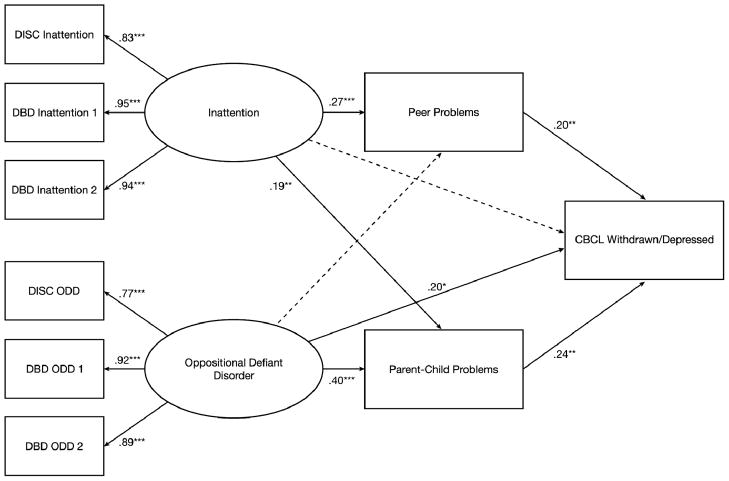
Covariates in the model included participant sex and age. To examine the indirect effect of inattention and hyperactivity symptom dimensions on depression via multiple mediators, depression was regressed on peer problems, academic achievement, and parent-child problems, which was in turn regressed on the two latent ADHD symptom dimensions, set to covary. This initial model had suboptimal fit (χ2(41) =114.17, p < .001, CFI = .96, SRMR = .04, RMSEA = .09). Academic achievement was unrelated to depression, and the paths from hyperactivity to all mediators and to depression were not statistically significant. As a result, the model was reevaluated after removing both academic achievement and hyperactivity. This model (Figure 1) provided a good fit that was also more parsimonious (χ2(16) = 31.00, p = .01, CFI = .98, SRMR = .04, RMSEA = .06). There were significant associations between inattention and both peer problems and parent-child problems, which were, in turn, significantly associated with depression. The point estimate of the indirect effect of the inattention latent factor on depression was .08 (SE = .03), p = .003 for peer problems and .13 (SE = .04), p < .001 for parent-child problems, indicating that both measures of interpersonal disturbance independently significantly mediated this association. The direct effect of inattention on depression was no longer significant over and above the variables reflecting interpersonal problems.
Figure 1.
Model of the association of ADHD inattention with depression as mediated by peer rejection and parent-child problems (N = 229) Note: DISC = Diagnostic Interview Schedule for Children. DBD = Disruptive Behavior Disorder Rating Scale. CBCL = Child Behavior Checklist. Standardized parameter estimations are shown; errors and covariances not shown. Nonsignificant paths are represented by dotted lines. ***p < .001.
Inclusion of Oppositional Defiant Disorder
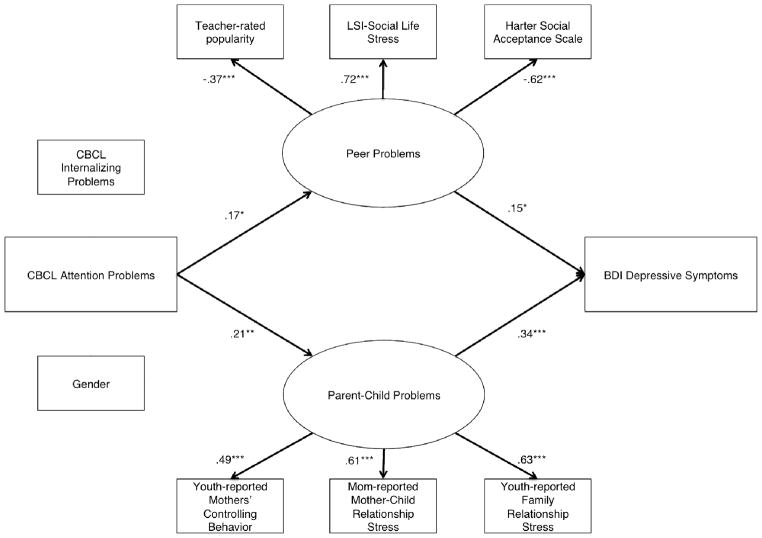
Given the frequent overlap between ADHD and ODD and the relevance of ODD to the mediators and outcome assessed, we examined the above model with the inclusion of latent ODD as an additional predictor. The latent ODD and inattention factors were allowed to covary, as were the ODD and inattention scales from the DISC. Though the model RMSEA fell slightly above the standard thresholds for acceptable fit, (χ2(36) = 68.17, p = .001, CFI = .97, SRMR = .04, RMSEA = .062), the results suggested independent effects of both inattention and ODD (Figure 2). While only ODD had a significant direct effect on depression, both inattention and ODD demonstrated indirect effects via peer problems and parent-child problems on depression, although the effect was marginal for ODD via peer problems. The point estimate of the indirect effect of the inattention latent factor on depression was .06 (SE = .03), p = .04 for peer problems and .04 (SE = .02), p = .05 for parent-child problems, whereas the point estimate of the indirect effect of the ODD latent factor on depression was .04 (SE = .02), p = .095 for peer problems and .10 (SE = .04), p = .01 for parent-child problems.
Figure 2.
Model of the association of both ADHD inattention and oppositional defiant disorder with depression as mediated by peer rejection and parent-child problems (N = 229) Note: DISC = Diagnostic Interview Schedule for Children. DBD = Disruptive Behavior Disorder Rating Scale. CBCL = Child Behavior Checklist. Standardized parameter estimations are shown; errors and covariances not shown. Nonsignificant paths are represented by dotted lines. * p < .05. ** p < .01. ***p < .001.
Moderation by Sex
Sex differences in the initial multiple mediation model were first examined by evaluating the difference in model fit between a model in which all paths were constrained to be equal across sex compared to a model in which all pathways were free to vary. Satorra-Bentler χ2 difference testing revealed no difference in model fit between the more restrictive and less restrictive models (χ2diff (7) = 3.57, p = .83). Second, there were no significant differences between boys and girls for any path coefficients or indirect effects.
Moderation by sex was then explored in the model where ODD was included as a predictor. The Satorra-Bentler χ2 test revealed a marginally significant difference in model fit between the more restrictive and less restrictive models (χ2diff (11) = 17.92, p = .08). Specifically, ODD predicted parent-child problems more strongly for girls than for boys (unstandardized difference = 0.47, p < .05; β = .56, SE = .08, p < .001 for females; β = .35, SE = .08, p < .001 for males). ODD also predicted peer problems for females (β = .47, SE = .16, p < .01); however, this pathway was nonsignificant for males (β = .09, SE = .10, p = .34). Another significant sex difference was found where parent-child problems significantly mediated the association between ODD and depression for females (estimate = 0.39, SE = 0.14, p < .01), but not for males (estimate = 0.07, SE = 0.04, p = .12).
Study 1 Discussion
The results of Study 1 suggest that both peer and parent-child difficulties independently mediated the association between inattention and depressive symptoms. The results affirm the importance of interpersonal difficulties in the prediction of depression. However, contrary to expectations, academic achievement was not a significant mediator. These findings were not moderated by the child’s sex. The inclusion of ODD in the model revealed that both inattention and ODD were independent indirect predictors of depression via both peer problems and parent-child problems. These findings are in concert with previous evidence that ADHD was associated with depression similarly in young children (ages 6–9) with and without comorbid ODD (see Ostrander et al., 2006). Additionally, the consequences of ODD were more significant for girls than boys, with girls experiencing more peer problems, parent-child problems, and, indirectly depression, as a function of their ODD. While these results are notable, the cross-sectional design and lack of youth self-report are notable limitations.
Study 2
It is unknown whether the associations between attention problems, interpersonal difficulties, and depression are robust across development, and whether Study 1 findings would replicate using measures of depression symptoms commonly used in clinical studies (i.e., Beck Depression Inventory) and using different, but more diverse, measures of academic, parent-child, and peer functioning. Study 2 attempted to replicate and extend the findings of Study 1 in a longitudinal high-risk community sample where children of depressed mothers were overrepresented. Children in this sample were followed from birth to age 20, allowing for assessment across development and by multiple informants (i.e., self, mother, and teacher).
Method
Participants
Participants were 472 individuals (44% male; age 20 years) from Queensland, Australia followed from birth to age 20. These individuals were part of a larger birth cohort study, the Mater-University Study of Pregnancy (Keeping et al., 1989), designed to examine how conditions during pregnancy affect children’s development up to age 5. Of the over 7,000 mother-child pairs who participated in the original study, 815 were selected for follow-up at youth age 15. For further information regarding procedures of sample recruitment and screening, see Hammen, Shih, and Brennan (2004). Of these participants, 706 (87% of the sample) were retained for follow up at youth age 20. Attrition was largely due to refusal to participate or failure to be located or scheduled. The sample for the present analyses consisted of the 472 individuals who, in addition to having self- and maternal-reported data, also had teacher-reported data on social functioning when youth were 15 years old, which allowed for a more complete assessment of interpersonal functioning at age 15. This subsample did not differ from the original sample of 815 on childhood attention problems (t(764) = −1.00, p = .31), depression diagnosis by age 15 (x2(1) = 0.04, p = .92), or any age 15 indicators of interpersonal functioning included in the current model. However, the current sample had lower levels of academic difficulties (e.g., class failures, school withdrawal) at age 15 than those not included in the current sample (t(656) = 4.80, p < .001).
Procedure
At participants’ age 5, mothers completed rating scales pertaining to their health, attitudes, parenting style, and children’s behavior, including selected questions from the CBCL (Achenbach, 1991).
At ages 15 and 20, participants and their mothers completed extensive interview and questionnaire sessions. Participants all gave informed consent, or assent in the case of minors, and the relevant institutional review/ethics panels of the University of Queensland, UCLA, and Emory University approved the research protocols.
At age 15, participants and mothers were also asked permission to allow researchers to collect information from participants’ teachers. Participating teachers completed the Teacher’s Report Form (Achenbach, 1991) and an additional questionnaire regarding academic and social functioning of the participant.
Measures
Age 5 Behavior and Emotion Problems
At youth age 5, mothers completed a modified version of the CBCL (Achenbach, 1991) regarding their children’s emotional states and behaviors. This abbreviated version of the CBCL was developed by Najman et al. (1997) and included 33 of the 118 items from the full length CBCL. Such items were selected based on resource constraints in order to reduce participant burden. Reliability estimates indicate that the psychometric properties of the modified CBCL are similar to those of the full version. For example, scores on the shortened version of the Externalizing scale of the CBCL are strongly correlated with scores from the full version (r = .94; Najman et al., 1997). Three scales of the modified CBCL were relevant to the current study: Attention Problems, Aggression, and Internalizing scales.
Age 15 Academic Problems
Academic problems were assessed at age 15 using the academic stress section of the UCLA Life Stress Interview (LSI; Hammen & Brennan, 2001). The LSI is a semi-structured interview that assesses stress in various domains of functioning, including social relationships, family relationships, and school or work. For each domain, trained interviewers query the participant about his or her functioning. The interviewers then determine a rating of stress/functioning on the basis of participants’ reports, with scores ranging from 1 to 5, with half points permitted. In the case of academic functioning, a score of 1 reflects “superior performance in all areas: honors,” and a score of 5 is given when an individual is “doing very poorly academically, has failed 3 or more subjects, has full-time placement in special classes, or has dropped out of school for academic reasons.” Reliabilities for this measure were based on independent judges’ ratings of 88 audiotaped interviews. In the full sample of individuals followed to age 15, the intraclass correlation for ratings on this measure was .94. Scores on this measure were significantly correlated with teacher reports of participants’ academic performance in their own class at r = .56 (see Adrian & Hammen, 1993 and Rao, Hammen, & Daley, 1999 for more information regarding the psychometric properties of the Life Stress Interview).
Age 15 Peer Problems
Impairment in peer relationships was assessed at age 15 using teacher-report data, interview data from the LSI, and self-report data. In the current analyses, these three indicators of social impairment were used to create a latent factor of peer problems.
Teachers were asked to describe the participant’s age 15 functioning, including one item on the youth’s popularity with peers rated from 1 (not at all popular) to 7 (extremely popular). This item served as one indicator of peer problems.
Information about participants’ social functioning was also assessed using the “Social Life” domain of the LSI. Participants were queried about the size of their social circle, quality of social relationships, and frequency of social interaction. As with all domains of the LSI, interviewers gave participants a score from 1 to 5. A score of 1 reflects a social life including many friends, frequent engagement in social activities, and no conflict in social situations, and a score of 5 is indicative of no friends, rejection by peers, or frequent and severe conflict with friends or acquaintances. The intraclass correlation for reliability on this measure was .63. Supporting the validity of this measure, significant correlations have been found between the LSI-Social Life scores and ratings of peer acceptance/rejection and popularity assessed by homeroom teachers (see Hammen, Brennan, & Keenan-Miller, 2008).
Thirdly, participants were asked to complete the Self-Perception Profile for Adolescents (Harter, 1988). Used in the current study was the Social Acceptance subscale of this measure, which consists of five items (each rated on a scale from 1 to 4) regarding perceived acceptance by peers, ease of making friends, and likeability.
Age 15 Parent-Child Problems
Parent-child problems were assessed using three different measures at age 15: 1) chronic stress in the mother-child relationship domain of the LSI administered to participants’ mothers, 2) chronic stress in the family domain of the LSI administered to participants, and 3) participant reports of mothers’ controlling parenting behaviors. These three measures were used as indicators of an underlying latent variable of parent-child problems.
First, the LSI was conducted with participants’ mothers during the age 15 assessment. The domain of the LSI that assessed parent-child relationship stress queried mothers about the quality of the parent-child relationship, including closeness, conflict, and the child’s compliance with rules. On the behaviorally anchored 1–5 scoring scale, a score of 1 represents an exceptionally close and effective parenting relationship with minimal chronic stress and a 5 represents a poor parent-child relationship marked by conflict and poor monitoring or control over the youth. The intraclass correlation of reliability among raters was .82.
Participants also completed a domain of the LSI regarding their family relationships, including factors such as closeness, communication, and conflict resolution. A score of 1 represents an exceptional quality relationship with all members of the family while a score of 5 reflects markedly poor relationship quality and significant problems. The intraclass correlation of inter-rater reliability was .84.
Participants additionally completed the Psychological Control subscale of the Children’s Report of Parental Behavior Inventory (CRPBI; Schluderman & Schluderman, 1988). This scale includes items such as “wants to control whatever I do,” and “is always trying to change me.” CRPBI subscales have shown good reliability and convergent validity (e.g., parental overinvolvement; Safford, Alloy, & Pieracci, 2007).
Age 20 Depressive Symptoms
Participants’ depressive symptoms were assessed at age 20 using the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996). The BDI-II is a well-validated and widely used 21-item self-report measure of depressive symptomatology. Questions cover symptoms of depression including low mood, appetite changes, and suicidal ideation, among others.
Results
Proposed Structural Model
Descriptive statistics and bivariate correlations among all observed variables are presented in Table 2. To test study hypotheses, we evaluated a multiple mediation model based on childhood attention problems directly predicting depressive symptoms in early adulthood and indirectly predicting depressive symptoms via peer problems, academic functioning, and parent-child problems. Academic problems were included in the model as an observed variable whereas both peer problems and parent-child problems were included as latent factors with three indicators each, as explained in the Methods section. As with Study 1, all observed variables were converted to z-scores prior to analyses to facilitate interpretation of results. To account for non-normality in several variables, robust maximum likelihood procedures were utilized to obtain model estimates.
Table 2.
Correlation Matrix for Study 2 Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CBCL Attention Problems | 1 | .62*** | .63*** | .22*** | .16** | −.04 | −.10* | .05 | .18*** | .13** | .12** | −.09* |
| 2. CBCL Aggression | 1 | .56*** | .22*** | .14** | −.08† | −.12* | .13** | .25*** | .16** | .18*** | −.05 | |
| 3. CBCL Internalizing Problems | 1 | .18*** | .15** | .02 | −.06 | .13** | .11* | .10* | .13** | −.01 | ||
| 4. LSI Academic Problems | 1 | .17*** | −.09† | −.30*** | .20*** | .26*** | .24*** | .19*** | −.16** | |||
| 5. LSI Social Stress | 1 | −.46*** | −.23*** | .20*** | .10* | .14** | .17*** | −.03 | ||||
| 6. Harter Social Acceptance | 1 | .25*** | −.06 | −.01 | −.08 | −.13** | .07 | |||||
| 7. Teacher-reported Popularity | 1 | −.09† | −.18*** | −.17*** | −.16*** | .10* | ||||||
| 8. Youth-reported Family Stress | 1 | .40*** | .29*** | .28*** | .09† | |||||||
| 9. Mother-reported Mother-Child Stress | 1 | .29*** | .21*** | .02 | ||||||||
| 10. Youth-reported Maternal Controlling Behavior | 1 | .19*** | −.08† | |||||||||
| 11. Depressive Symptoms | 1 | .18*** | ||||||||||
| 12. Sex (Female = 1) | 1 | |||||||||||
| Means (SD) or % | 3.49 (2.38) | 6.90 (3.88) | 4.66 (3.27) | 2.54 (0.86) | 2.28 (0.48) | 15.67 (3.07) | 4.55 (1.20) | 2.34 (0.56) | 2.20 (0.50) | 16.78 (4.13) | 6.94 (8.58) | 44% male |
Note. CBCL = Child Behavior Checklist. LSI = Life Stress Interview.
p < 0.10,
p < 0.05,
p < 0.01,
p < 0.001.
Multiple Mediation
To examine peer problems, academic problems, and parent-child problems as mediators of the association between youth attention problems and early adult depressive symptoms, the full proposed structural model was evaluated. The model controlled for child’s sex and internalizing symptoms at age 5, which diminished the possibility that any effects of age 5 attention problems on later depression were merely a result of initial comorbidity of attention problems and internalizing difficulties at age 5.
Though the model was an acceptable fit to the data by some fit statistics (CFI = .90, SRMR = .50), the RMSEA (.064) was slightly higher than the acceptable cutoff. The chi-square test statistic was significant (χ2(34) = 99.84, p < .001); however, chi-square test statistics are often significant with large samples. Parameter estimates revealed that, whereas attention problems predicted all three mediators, depressive symptoms were only predicted by peer and parent-child problems. Consistent with Study 1, academic problems were unrelated to later depressive symptoms (β = .05, SE = .06, p = .43). For this reason, the academic problems variable was excluded from the model.
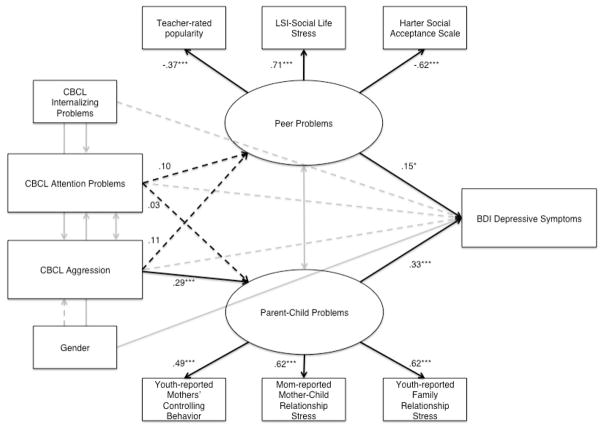
When the model was re-evaluated without academic problems (i.e., peer problems and parent-child problems as the two mediators), the model adequately fit the data (χ2(28) = 71.59, p < .001, CFI = .93, SRMR = .04, RMSEA = .058) (see Figure 3). The direct path from childhood attention problems to adult depressive symptoms was nonsignificant. Attention problems significantly predicted peer problems and parent-child problems, which in turn, significantly predicted depressive symptoms. Analyses revealed a significant specific indirect effect of attention problems on depressive symptoms via parent-child problems (point estimate = .07, SE = .03, p < .05). In addition, there was a marginal specific indirect effect of attention problems on depressive symptoms via peer problems (point estimate = .03, SE = .01, p = .08)1.
Figure 3.
Final model of the association between age 5 attention problems and age 20 depressive symptoms. Model excludes academic problems due to nonsignificant pathways in the original model. Model includes peer problems and parent-child problems as mediators, as well as age 5 internalizing problems and sex as statistical controls. Note: CBCL = Child Behavior Checklist. LSI = Life Stress Interview. BDI = Beck Depression Inventory. Standardized parameter estimates are shown. Parameter estimates unrelated to study hypotheses are excluded from the figure for ease of readability. Nonsignificant paths are represented by dotted lines. †p < 0.10, *p < .05, **p < .01, ***p < .001.
Inclusion of Oppositional Defiant Disorder
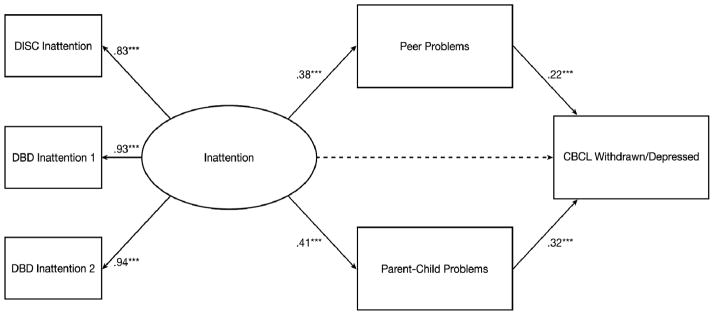
To account for co-occurring ODD/aggression in predictions of impaired interpersonal functioning and subsequent depression symptoms, we reproduced the aforementioned multiple mediation model, except we included childhood aggression as a second predictor of the two mediators and outcome variable (Figure 4). This model adequately fit the data (χ2(32) = 78.59, p < .001, CFI = .95, SRMR = .04, RMSEA = .056). In contrast to the first multiple mediation model, attention problems did not significantly predict peer problems or parent-child problems. Childhood aggression, however, significantly predicted parent-child problems but not peer problems. Examination of indirect effects revealed that parent-child problems significantly mediated the association of childhood aggression and adult depressive symptoms (β = .10, SE = .04, p < .01). No further mediation was supported and neither childhood inattention nor childhood aggression directly predicted age 20 depressive symptoms.
Figure 4.
Final model of the association between age 5 attention problems, age 5 aggression, and age 20 depressive symptoms. Model includes peer problems and parent-child problems as mediators, as well as age 5 internalizing problems and sex as statistical controls. Note: CBCL = Child Behavior Checklist. LSI = Life Stress Interview. BDI = Beck Depression Inventory. Standardized parameter estimates are shown. Parameter estimates unrelated to study hypotheses are excluded from the figure for ease of readability. Nonsignificant paths are represented by dotted lines. *p < .05, **p < .01, ***p < .001.
Moderation by Sex
Satorra-Bentler χ2 tests evaluated potential sex differences. In the model with attention problems as the only predictor, there was no significant difference in model fit (χ2diff (8) = 12.48, p = .13). However, the path from parent-child problems to depressive symptoms differed across sex (unstandardized difference = 0.68, p < .05), such that parent-child problems significantly predicted depressive symptoms for girls (β = .77, SE = .20, p < .001), but not for boys (β = .10, SE = .21, p = .65). There were no significant differences in indirect effect point estimates across sex.
For the multiple mediation model in which both childhood attention problems and aggression were included as predictors, the Satorra-Bentler χ2 revealed a marginally significant difference between the restricted and unrestricted models (χ2diff (13) = 21.36, p = .07). Further analysis revealed a significant difference between males and females in the relationship between aggression and parent-child problems (unstandardized difference = 0.22, p < .05), such that parent-child problems were predicted by childhood aggression for females (β = .43, SE = .10, p < .001), but not for males (β = .13, SE = .09, p = .14). Additionally, depression was predicted by parent-child problems for females (β = .45, SE = .09, p < .001), but not for males (β = .06, SE = .14, p = .67). Overall, the indirect path from aggression to depression via parent-child problems was significant for females (estimate = .23, SE = .08, p < .01), but not for males (estimate = .01, SE = .02, p = .70).
Study 2 Discussion
As in Study 1, multiple mediation analyses revealed that academic functioning was not a significant unique mediator in the association between attention problems and depression. However, adolescent peer and parent-child problems each predicted later depressive symptoms and were predicted by early attention problems. Parent-child problems significantly mediated the relationship between attention problems and depression whereas peer problems marginally significantly mediated this relationship. Notably, when childhood aggression, a proxy for ODD symptoms, was included in the model, attention problems no longer predicted these mediators. Instead, childhood aggression significantly predicted parent-child problems, and, in turn, adulthood depression symptoms. This nonsignificant effect of attention problems when accounting for childhood aggression differs from the findings of Study 1. Finally, parent-child problems significantly predicted depression for females but not for males, and childhood aggression was only predictive of parent-child problems for females. This suggests that the significant mediating role of parent-child problems in the full sample may reflect the relatively strong relationship between these variables among females.
General Discussion
Using two independent but complementary samples, we explored the association between attention problems and depression, with particular consideration of the interpersonal and functional impairments that may contribute to the development of depressive symptoms among children with elevated inattention. Study 1 examined the mediating roles of peer problems, academic achievement, and parent-child problems in the concurrent association of ADHD and depression in a sample of school-aged children with and without ADHD. The use of rigorous and reliable measures of ADHD symptoms allowed for the separate examination of inattention vs. hyperactivity symptoms, as well as ODD symptoms, and their unique associations with academic and psychosocial impairment as well as depressive symptoms. Study 2 also examined peer, academic, and parent-child problems in a prospective longitudinal sample of children followed from birth to age 20 whose mothers disproportionately had clinical depression histories. The sample allowed for exploration of the ADHD-depression relationship and its mediating factors across three time points, spanning from early childhood to young adulthood, and included multiple informants on child’s behavior and a well-validated measure of depressive symptoms.
We believe the most substantial finding is that, in both samples, parent-child problems significantly mediated the relationship between attention problems and depression, over and above the potential effects of both peer and academic domains. Thus, dual-failure models of externalizing problems and later depression appear to be omitting this important factor. Previous literature showed elevated rates of parent-child problems in parents of children with comorbid ADHD and depression (Deault, 2010), an association between ADHD and parent-child problems (e.g., Barkley et al., 1991), and an association between parent-child problems and depression (e.g., McLeod, Weisz, & Wood, 2007). Given the stress associated with parenting a child with ADHD (Barkley et al., 1992), these parents may have difficulty implementing effective parenting strategies, have greater conflict with their children, and convey greater rejection and hostility to their children (Johnston & Mash, 2001; Lifford et al., 2008; Lifford et al., 2009). In turn, stressful conflict and perceived lack of support from parents may contribute to the onset of depressive symptoms (e.g., Stice, Ragan, & Randall, 2004). Further research is needed to determine the specific components of parent-child problems that may be responsible for the relationship between ADHD and depression.
Peer problems significantly mediated the ADHD-depression relationship in Study 1 and marginally significantly mediated the ADHD-depression relationship in Study 2. Thus, beyond the well-established peer difficulties among children with ADHD (Hoza et al., 2005), difficulties with peer relationships may contribute to depressive symptoms (see Hirschfield et al., 2000 for a review). Children with ADHD frequently overestimate their social competence and functioning in other domains, a phenomenon known as positive illusory bias (see Owens, Goldfine, Evangelista, Hoza, & Kaiser, 2007, for a review). Such inflated positive self-perceptions may serve as a double-edged sword: on the one hand, these perceptions may inhibit children’s ability to incorporate critical feedback from others in order to change their social behaviors and improve their relationships (Colvin & Block, 1994). On the other hand, positive self-perceptions protect children with ADHD from the development of depression (McQuade, Hoza, Murray-Close, Waschbusch, & Owens, 2011). Notably, positive illusory bias is not found among children with comorbid depression (Hoza, Waschbusch, Pelham, Molina, & Milich, 2004), potentially making this subgroup more attuned to negative peer relationships. It may be that as children become increasingly proficient at understanding how others view them, the protective effect associated with the positive illusory bias may be replaced by more stable negative self-schemas. One notable limitation of both studies was the lack of parallel self-report and observer-report measures to allow for a comparison between self-appraisal of interpersonal functioning and actual interpersonal functioning. The discrepancy between one’s cognitions about social functioning and one’s actual social performance may be crucial to the development of depression.
Interestingly, neither study found that academic functioning significantly mediated the association of ADHD and depression when peer problems and parent-child problems were treated as simultaneous mediators. Yet, there are limitations in both studies’ measures of academic functioning, as both standardized assessment and youth interview are unlikely to perfectly capture school performance. Additionally, parent-report was used for all variables included in Study 1, with the exception of academic achievement, reducing the likelihood of shared variance due to methodological issues alone. However, validation data supported the use of the LSI in Study 2, as academic performance scores were corroborated by teacher reports. It should be noted that in Study 1, although academic functioning was associated with attention problems, it was uncorrelated with depression. This is counter to existing literature (Herman, Lambert, Reinke, & Ialongo, 2008), and the use of a measure that assesses ability rather than actual classroom performance may underlie this finding. In Study 2, academic functioning was correlated with both attention and depression measures, yet, in the full model when other, correlated variables were also included, academic functioning did not uniquely predict depression or the ADHD-depression relationship. Previous work has also documented a relative weakness of academic competence as a mediator of child problems to depression compared to peer problems (e.g., Blechman, McEnroe, Carella, & Audette, 1986; Patterson & Stoolmiller, 1991). Future studies will benefit from multi-informant measures of academic performance to confirm this domain’s secondary role to interpersonal difficulties in predictions of depressive symptoms.
Study 1 also separately examined inattention and hyperactivity to determine the relative contribution to interpersonal problems and depression. Inattention, but not hyperactivity, was related to peer problems, parent-child problems, and depression symptoms. Meta-analytic evidence suggests that while hyperactivity is more strongly associated with negative peer regard than inattention, social isolation is more strongly associated with inattention than hyperactivity (Willcutt et al., 2012). As social withdrawal has predicted risk for depressive symptoms by way of peer difficulties (e.g., Katz, Conway, Hammen, Brennan, & Najman, 2011), it is possible that there is a similar trajectory for children with attention problems. Given that SEM included predictors examined simultaneously, it is possible that the effect of inattention resulted in the non-significant association between hyperactivity and relevant outcomes, despite significant bivariate correlations between hyperactivity and both peer problems and parent-child problems.
The present study also explored the independent roles of ADHD and ODD in the development of depression. Results from Study 1 suggest that only ODD is a direct predictor of depression. However, inattention remained an important independent indirect predictor of depression through peer and parent-child problems. ODD, on the other hand, demonstrated a significant indirect effect on depression via parent-child problems and a marginal effect via peer problems. The impact of aggression in Study 2 was less clear. The inclusion of baseline aggression resulted in the loss of a significant indirect effect of attention problems on depression, and neither inattention nor aggression demonstrated a significant indirect effect via peer problems. Only parent-child problems remained a significant mediator of the aggression to depression association. Clearly the potential role of ODD/aggression in studies of ADHD remains an important issue in developmental psychopathology, and the present studies provide further evidence that inattention is an important risk factor for depression independent of ODD, but that the inclusion of conduct problems may complicate the ability to obtain direct effects from ADHD. Though distinguishing the independent roles of ADHD and ODD remains an important theoretical question, there is increasing evidence that individuals with ADHD+ODD comorbidity are at the highest risk for a number of negative outcomes (e.g., Carlson, Tamm, & Gaub, 1997; Humphreys & Lee, 2011).
No sex differences were found in the relationship between ADHD and interpersonal problems or indirect effects of ADHD on depression by way of interpersonal problems. However, both studies revealed significant sex differences in the indirect effect of ODD on depression through parent-child problems, such that ODD symptoms predicted these negative outcomes more strongly for females than for males. Though the rate of ODD is lower in girls compared to boys (Lahey, Miller, Gordon, & Riley, 1999), girls with conduct problems are more likely to have comorbid disorders (Robins, 1986), known as the “gender paradox.” It may be that parent-child relationships are more central to the development of comorbidity, including depression, in girls with elevated ODD symptoms. Study 2 also found a significant sex difference in the effect of parent-child relationship problems on depressive symptoms where parent-child problems significantly predicted depressive symptoms among females, but not males. This is consistent with previous literature suggesting that females are more likely than males to develop depression in response to interpersonal difficulties (see Leadbeater, Blatt, & Quinlan, 1995). In light of meta-analytic evidence that males are much more likely to meet diagnostic criteria for ADHD and that females with ADHD have more co-occurring internalizing symptoms (Gershon, 2002), these associations may be sex specific.
Overall, similar findings were noted of the ADHD-depression relationship and its mediators in two complementary samples. Study 1 was limited by its cross-sectional design, but included rigorous measures of ADHD, including separate tests of inattention and hyperactivity. Although Study 2 had a single measure of attention problems, it was strengthened by its prospective design spanning multiple developmental stages, data from multiple informants, and reliable and valid measurement of depressive symptoms. Thus, for the most part, where each study was lacking, the other study improved on those limitations. Despite potentially important differences in the etiology and presentation of child-, adolescent-, and adult-onset depression (e.g., Kaufman, Martin, King, & Charney, 2001), both final models suggested that ADHD may affect depression at different developmental stages via similar mechanisms. Additionally, though it is unclear at what age elevated depression levels presented, it is significant that the indirect effect of attention problems on depression via parent-child problems remained following the stringent inclusions of both baseline and age 15 depression measures.
Several important limitations should be considered, including the exclusive use of maternal reports of attention problems in both studies. Maternal psychopathology, such as depression, has been found to predict negatively biased reports of child ADHD symptoms and behavior problems (Chi & Hinshaw, 2002). On the other hand, emotionally healthy mothers tend to underestimate their children’s emotional and behavioral problems, relative to children’s self-reports (Najman et al., 2001). In addition, though there were efforts in Study 2 to control for relevant baseline predictors, we were unable to include baseline peer functioning in our models as other studies have done (i.e., Herman et al., 2008). Importantly, Herman and colleagues (2008) documented a link between academic competence and depression after controlling for baseline depression, peer relations, attention problems, and conduct problems. The rigorous inclusion of baseline covariates in future research would provide the most conservative test for examining mediation of the ADHD-depression relationship.
One further limitation was the length of time that elapsed between the age 15 and age 20 assessments in Study 2. It may be the case that five years is too long to expect mood-related consequences to persist secondary to interpersonal or academic difficulties. For example, failing a class in high school, though likely to negatively affect mood in the short-term, may have little effect on long-term mental health outcomes. This five-year period between assessments may be at least partially responsible for the contrast between our nonsignificant findings related to academic difficulties and the significant findings of previous research on the dual failure model (e.g., Patterson & Stoolmiller, 1991). An alternative consideration, proposed by Cole (1991) is that the value placed on academic functioning may decline in adolescence, as interpersonal factors increase in salience. In this case, despite the association between ADHD and poorer academic functioning, it is less likely that (negative) self-schema is tied to this domain. The changing priorities across development suggest that the mediators of the association between attention problems and depression should change over development, deemphasizing the role of failure related to academic and parent-child domains and prioritizing peer domains.
The two complementary studies included in this report provide significant evidence that peer problems and parent-child problems, but not academic functioning, play an important role in the relationship between attention problems and depression. Thus, these two aspects of interpersonal functioning may be central targets of intervention for children with ADHD. In line with both failure and competency models, treatment programs that emphasize improving competence may be particularly useful in children with ADHD (e.g., The Incredible Years; Webster-Stratton, 1992). Outcome research from this program found that child internalizing scores decreased following treatment (Webster-Stratton & Herman, 2008), which indicates that such treatment programs may be promising for addressing depression in children with disruptive behavior problems.
Footnotes
This multiple mediation model was re-run controlling for maternal depression, which had no effect on the pattern or significance of study findings. Additionally, this model was re-run controlling for age 15 depressive symptoms. While parent-child problems remained a significant mediator of the relationship between attention problems and depression, peer problems no longer met criteria for mediation in this case.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/pas
References
- Abidin RR. Parenting Stress Index. 3. Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- Achenbach TM. Integrative guide to the 1991 CBCL, YSR, and TRF profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Adrian C, Hammen C. Stress exposure and stress generation in children of depressed mothers. Journal of Consulting and Clinical Psychology. 1993;61(2):354–359. doi: 10.1037/0022-006X.61.2.354. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Anastopoulos A, Shelton T, DuPaul G, Guevremont D. Parent training for attention deficit hyperactivity disorder: its impact on parent functioning. Journal of Abnormal Child Psychology. 1993;21:581–96. doi: 10.1007/BF00916320. [DOI] [PubMed] [Google Scholar]
- Anderson JC, Williams S, McGee R, Silva PA. DSM-III disorders in preadolescent children: Prevalence in a large sample from the general population. Archives of General Psychiatry. 1987;44:69–76. doi: 10.1001/archpsyc.1987.01800130081010. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Anastopoulos AD, Guevremont DC, Fletcher KE. Adolescents with ADHD: Mother-adolescent interactions, family beliefs and conflicts, and maternal psychopathology. Journal of Abnormal Child Psychology. 1992;20:263–288. doi: 10.1007/BF00916692. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: III. Mother-child interactions, family conflicts and maternal psychopathology. Journal of Child Psychology and Psychiatry. 1991;32:233–255. doi: 10.1111/j.1469-7610.1991.tb00304.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Biederman J, Ball SW, Monuteaux MC, Mick E, Spencer TJ, McCreary M, Faraone SV. New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:426–434. doi: 10.1097/CHI.0b013e31816429d3. [DOI] [PubMed] [Google Scholar]
- Biederman J, Mick E, Faraone SV. Depression in attention deficit hyperactivity disorder (ADHD) children: “True” depression or demoralization? Journal of Affective Disorders. 1998;47:113–122. doi: 10.1016/S0165-0327(97)00127-4. [DOI] [PubMed] [Google Scholar]
- Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. The American Journal of Psychiatry. 1991;148:564–577. doi: 10.1176/ajp.148.5.564. [DOI] [PubMed] [Google Scholar]
- Blechman EA, McEnroe MJ, Carella ET, Audette DP. Childhood competence and depression. Journal of Abnormal Psychology. 1986;95:223–227. doi: 10.1037/0021-843X.95.3.223. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York, NY: John Wiley; 1989. [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: I. Familial factors and general adjustment at grade 6. Development and Psychopathology. 1991;3:277–300. doi: 10.1017/S0954579400005319. [DOI] [PubMed] [Google Scholar]
- Carlson CL, Tamm L, Gaub M. Gender differences in children with ADHD, ODD, and co-occurring ADHD/ODD identified in a school population. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(12):1706–1714. doi: 10.1097/00004583-199712000-00019. [DOI] [PubMed] [Google Scholar]
- Chi TC, Hinshaw SP. Mother-child relationships of children with ADHD: The role of maternal depressive symptoms and depression-related distortions. Journal of Abnormal Child Psychology. 2002;30:387–400. doi: 10.1023/A:1015770025043. [DOI] [PubMed] [Google Scholar]
- Cole DA. Relation of social and academic competence to depressive symptoms in childhood. Journal of Abnormal Psychology. 1990;99(4):422–429. doi: 10.1037/0021-843X.99.4.422. [DOI] [PubMed] [Google Scholar]
- Cole DA. Preliminary support for a competency-based model of depression in children. Journal of Abnormal Psychology. 1991;100(2):181–190. doi: 10.1037/0021-843X.100.2.181. [DOI] [PubMed] [Google Scholar]
- Colvin CR, Block J. Do positive illusions foster mental health? An examination of the Taylor and Brown formulation. Psychological Bulletin. 1994;116:3–20. doi: 10.1037/0033-2909.116.1.3. [DOI] [PubMed] [Google Scholar]
- Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD) Child Psychiatry and Human Development. 2010;41:168–192. doi: 10.1007/s10578-009-0159-4. [DOI] [PubMed] [Google Scholar]
- Dishion TJ. Family ecology of boys’ peer relations in middle childhood. Child Development. 1990;61:874–892. doi: 10.1111/j.1467-8624.1990.tb02829.x. [DOI] [PubMed] [Google Scholar]
- Eberhart NK, Hammen CL. Interpersonal predictors of onset of depression during the transition to adulthood. Personal Relationships. 2006;13:195–206. doi: 10.1111/j.1475-6811.2006.00113.x. [DOI] [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura B, Chorpita B, Higa-McMillan C, Weisz J. Concurrent validity of the Child Behavior Checklist DSM-oriented scales: Correspondence with DSM diagnoses and comparison to syndrome scales. Journal of Psychopathology and Behavioral Assessment. 2010;32:373–384. doi: 10.1007/s10862-009-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon J. A meta-analytic review of gender differences in ADHD. Journal of Attention Disorders. 2002;5(3):143–154. doi: 10.1177/108705470200500302. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Depressed adolescents of depressed and nondepressed mothers: tests of an interpersonal impairment hypothesis. Journal of Consulting and Clinical Psychology. 2001;69(2):284–294. doi: 10.1037/0022-006X.69.2.284. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Keenan-Miller D. Patterns of adolescent depression to age 20: the role of maternal depression and youth interpersonal dysfunction. Journal of Abnormal Child Psychology. 2008;36:1189–1198. doi: 10.1007/s10802-008-9241-9. [DOI] [PubMed] [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72(3):511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Harter S. Unpublished manuscript. University of Denver; 1988. Manual for the Self-Perception Profile for Adolescents. [Google Scholar]
- Henker B, Whalen CK. The child with attention-deficit/hyperactivity disorder in school and peer settings. In: Quay HC, Hogan AE, editors. Handbook of disruptive behavior disorder. Plenum; New York: 1999. pp. 157–178. [Google Scholar]
- Herman KC, Lambert SF, Ialongo NS, Ostrander R. Academic pathways between attention problems and depressive symptoms among urban African American children. Journal of Abnormal Child Psychology. 2007;35:265–274. doi: 10.1007/s10802-006-9083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman KC, Lambert SF, Reinke WM, Ialongo NS. Low academic competence in first grade as a risk factor for depressive cognitions and symptoms in middle school. Journal of Counseling Psychology. 2008;55(3):400–410. doi: 10.1037/a0012654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfield MD, Montgomery SA, Keller MB, Kasper S, Schatzberg AF, Möller H, Bourgeois M. Social functioning in depression: a review. Journal of Clinical Psychiatry. 2000;61(4):268–275. doi: 10.4088/JCP.v61n0405. [DOI] [PubMed] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, Arnold LE. What aspects of peer relationships are impaired in children with ADHD? Journal of Consulting and Clinical Psychology. 2005;73:411–423. doi: 10.1037/0022-006X.73.3.411. [DOI] [PubMed] [Google Scholar]
- Hoza B, Gerdes AC, Hinshaw SP, Arnold LE, Pelham WE, Jr, Molina BS, Wigal T. Self-perceptions of competence in children with ADHD and comparison children. Journal of Consulting and Clinical Psychology. 2004;72(3):382–391. doi: 10.1037/0022-006X.72.3.382. [DOI] [PubMed] [Google Scholar]
- Hoza B, Waschbusch DA, Pelham WE, Molina BSG, Milich R. Attention-deficit/hyperactivity disordered and control boys’ responses to social success and failure. Child Development. 2000;71:432–446. doi: 10.1111/1467-8624.00155. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Humphreys KL, Lee SS. Risk taking and sensitivity to punishment in children with ADHD, ODD, ADHD+ ODD, and controls. Journal of Psychopathology and Behavioral Assessment. 2011;33(3):299–307. doi: 10.1007/s10862-011-9237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Mehta N, Lee SS. Association of parental ADHD and depression with externalizing and internalizing dimensions of child psychopathology. Journal of Attention Disorders. 2012;16:267–275. doi: 10.1177/1087054710387264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston C, Mash EJ. Families of children with attention-deficit/hyperactivity disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/A:1017592030434. [DOI] [PubMed] [Google Scholar]
- Katz SJ, Conway CC, Hammen CL, Brennan PA, Najman JM. Childhood social withdrawal, interpersonal impairment, and young adult depression: A mediational model. Journal of Abnormal Child Psychology. 2011;39:1227–1238. doi: 10.1007/s10802-011-9537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz SJ, Hammen CL, Brennan PA. Maternal depression and the intergenerational transmission of relational impairment. Journal of Family Psychology. 2013;27:86–95. doi: 10.1037/a0031411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeping JD, Najman JM, Morrison J, Western JS, Andersen MJ, Williams GM. A prospective longitudinal study of social, psychological, and obstetrical factors in pregnancy: Response rates and demographic characteristics of the 8,556 respondents. British Journal of Obstetrics and Gynaecology. 1989;96:289–297. doi: 10.1111/j.1471-0528.1989.tb02388.x. [DOI] [PubMed] [Google Scholar]
- Kelloway EK. Using LISREL for structural equation modeling: A researcher’s guide. SAGE Publications, Incorporated; 1998. [Google Scholar]
- Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA, Stein DJ. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: Results from the WHO World Mental Health Survey Initiative. Depression and Anxiety. 2010;27:351–364. doi: 10.1002/da.20634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Martin A, King RA, Charney D. Are child-, adolescent-, and adult-onset depression one and the same disorder? Biological Psychiatry. 2001;49(12):980–1001. doi: 10.1016/S0006-3223(01)01127-1. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, McBurnett K, Biederman J. DMS-IV field trials for attention deficit hyperactivity disorder in children and adolescents. American Journal of Psychiatry. 1994;151(11):1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Miller TL, Gordon RA, Riley AW. Developmental epidemiology of the disruptive behavior disorders. In: Quay HC, Hogan AE, editors. Handbook of disruptive behavior disorders. New York: Kluwer Academic/Plenum Publishers; 1999. [Google Scholar]
- Leadbeater BJ, Blatt SJ, Quinlan DM. Gender-linked vulnerabilities to depressive symptoms, stress, and problem behaviors in adolescents. Journal of Research on Adolescence. 1995;5:1–29. doi: 10.1207/s15327795jra0501_1. [DOI] [Google Scholar]
- Lee SS, Hinshaw SP. Predictors of adolescent functioning in girls with attention deficit hyperactivity disorder (ADHD): The role of childhood ADHD, conduct problems, and peer status. Journal of Clinical Child and Adolescent Psychology. 2006;35:356–368. doi: 10.1207/s15374424jccp3503_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifford KJ, Harold GT, Thapar A. Parent-child relationships and ADHD symptoms: a longitudinal analysis. Journal of Abnormal Child Psychology. 2008;36:285–96. doi: 10.1007/s10802-007-9177-5. [DOI] [PubMed] [Google Scholar]
- Lifford KJ, Harold GT, Thapar A. Parent-child hostility and child ADHD symptoms: A genetically sensitive and longitudinal analysis. The Journal of Child Psychology and Psychiatry. 2009;50:1468–1476. doi: 10.1111/j.1469-7610.2009.02107.x. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Mason WA, Kosterman R, Hawkins JD, Lengua LJ, McCauley E. Adolescent school failure predicts later depression among girls. Journal of Adolescent Health. 2008;43:180–187. doi: 10.1016/j.jadohealth.2008.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod BD, Weisz JR, Wood JL. Examining the association between parenting and childhood depression: A meta-analysis. Child Psychology Review. 2007;27:986–1003. doi: 10.1016/j.cpr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- McQuade JD, Hoza B, Murray-Close D, Waschbusch DA, Owens JS. Changes in self-perceptions in children with ADHD: A longitudinal study of depressive symptoms and attributional style. Behavior Therapy. 2011;42:170–182. doi: 10.1016/j.beth.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- Najman JM, Behrens BC, Andersen M, Bor W, O’Callaghan M, Williams GM. Impact of family type and family quality on child behavior problems: A longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1357–1365. doi: 10.1097/00004583-199710000-00017. [DOI] [PubMed] [Google Scholar]
- Najman JM, Williams GM, Nikles J, Spence S, Bor W, O’Callaghan M, Shuttlewood GJ. Bias influencing maternal reports of child behaviour and emotional state. Social Psychiatry and Psychiatric Epidemiology. 2001;36:186–194. doi: 10.1007/s001270170062. [DOI] [PubMed] [Google Scholar]
- Ostrander R, Crystal DS, August G. Attention deficit-hyperactivity disorder, depression, and self- and other-assessments of social competence: A developmental study. Journal of Abnormal Child Psychology. 2006;34(6):773–787. doi: 10.1007/s10802-006-9051-x. [DOI] [PubMed] [Google Scholar]
- Ostrander R, Herman KC. Potential cognitive, parenting, and developmental mediators of the relationship between ADHD and depression. Journal of Consulting and Clinical Psychology. 2006;74:89–98. doi: 10.1037/0022-006X.74.1.89. [DOI] [PubMed] [Google Scholar]
- Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM. A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clinical Child and Family Psychology Review. 2007;10(4):335–351. doi: 10.1007/s10567-007-0027-3. [DOI] [PubMed] [Google Scholar]
- Panak WF, Garber J. Role of aggression, rejection, and attributions in the prediction of depression in children. Development and Psychopathology. 1992;4:145–165. doi: 10.1017/S0954579400005617. [DOI] [Google Scholar]
- Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44:329–335. doi: 10.1037/0003-066X.44.2.329. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Stoolmiller M. Replications of a dual failure model for boys’ depressed mood. Journal of Consulting and Clinical Psychology. 1991;59:491–498. doi: 10.1037/0022-006X.59.4.491. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Jr, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Jr, Fabiano GA, Massetti GM. Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):449–476. doi: 10.1207/s15374424jccp3403_5. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression Critical review. The British Journal of Psychiatry. 2000;177(6):486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Rao U, Hammen C, Daley SE. Continuity of depression during the transition to adulthood: a 5-year longitudinal study of young women. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(7):908–915. doi: 10.1097/00004583-199907000-00022. [DOI] [PubMed] [Google Scholar]
- Robins LN. The consequences of conduct disorder in girls. Development of antisocial and prosocial behavior. 1986:385–414. [Google Scholar]
- Rudolph KD, Hammen C, Burge D, Lindberg N, Herzberg D, Daley SE. Toward an interpersonal life-stress model of depression: the developmental context of stress generation. Development and Psychopathology. 2000;12:215–234. doi: 10.1017/s0954579400002066. [DOI] [PubMed] [Google Scholar]
- Safford SM, Alloy LB, Pieracci A. A comparison of two measures of parental behavior. Journal of Child and Family Studies. 2007;16(3):375–384. doi: 10.1007/s10826-006-9092-3. [DOI] [Google Scholar]
- Schludermann S, Schludermann E. Unpublished manuscript. University of Manitoba; Winnipeg, Canada: 1988. Shortened Child Report of Parent Behavior Inventory (CRPBI-30): Schludermann Revision. [Google Scholar]
- Seroczynski AD, Cole DA, Maxwell SE. Cumulative and compensatory effects of competence and incompetence on depressive symptoms in children. Journal of Abnormal Psychology. 1997;106:586–597. doi: 10.1037/0021-843X.106.4.586. [DOI] [PubMed] [Google Scholar]
- Seymour KE, Chronis-Tuscano A, Halldorsdottir T, Stupica B, Owens K, Sacks T. Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. Journal of Abnormal Child Psychology. 2010;40:595–606. doi: 10.1007/s10802-011-9593-4. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–39. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shemmassian SK, Lee SS. Comparing four methods of integrating parent and teacher symptom ratings of attention-deficit/hyperactivity disorder (ADHD) Journal of Psychopathology and Behavioral Assessment. 2012;34:1–10. doi: 10.1007/s10862-011-9262-5. [DOI] [Google Scholar]
- Smart D, Sanson A, Prior M. Connections between reading disability and behavior problems: Testing temporal and causal hypotheses. Journal of Abnormal Child Psychology. 1996;24:363–383. doi: 10.1007/BF01441636. [DOI] [PubMed] [Google Scholar]
- Stice E, Ragan J, Randall P. Prospective relations between social support and depression: Differential direction of effects for parent and peer support? Journal of Abnormal Psychology. 2004;113:155–159. doi: 10.1037/0021-843X.113.1.155. [DOI] [PubMed] [Google Scholar]
- Szatmari P, Offord DR, Boyle MH. Ontario Child Health Study: prevalence of attention deficit disorder with hyperactivity. Journal of Child Psychology and Psychiatry. 1989;30(2):219–223. doi: 10.1111/j.1469-7610.1989.tb00236.x. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Herman KC. The impact of parent behavior-management training on child depressive symptoms. Journal of Counseling Psychology. 2008;55(4):473–484. doi: 10.1037/a0013664. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C. The incredible years. Seattle: 1992. [citerad dec. 2007]. URL http://www.incredibleyears.com. [Google Scholar]
- Wechsler DL. Wechsler Individual Achievement Test-II. San Antonio, Tex: Psychological Corporation; 2002. [Google Scholar]
- Willcutt EG, Nigg JT, Pennington BF, Solanto MV, Rohde LA, Tannock R, Lahey BB. Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. Journal of Abnormal Psychology. 2012 doi: 10.1037/a0027347. [DOI] [PMC free article] [PubMed] [Google Scholar]