Summary
We sought to determine the effect of hydration on the criteria for chronic cerebrospinal venous insufficiency (CCSVI), a proposed hypothesis for the etiology of multiple sclerosis (MS). Sixteen subjects (11 MS and 5 controls) were asked to fast overnight. The following morning, 2 CCSVI ultrasound examinations were performed: 1 in the mildly dehydrated state, and another 30–45 minutes after rehydrating with 1.5 L of Gatorade. Seven subjects fulfilled CCSVI criteria in the dehydrated state. Of these, 5 (71%) no longer fulfilled CCSVI criteria after rehydration. One additional subject met CCSVI criteria only after rehydration. Hydration status has a substantial effect on CCSVI criteria, suggesting that the sonographic findings of CCSVI may represent a physiologic rather than pathologic state.
The chronic cerebrospinal venous insufficiency (CCSVI) hypothesis posits that abnormalities in the extracranial venous outflow contribute to the pathogenesis of multiple sclerosis (MS),1,2 although results from different groups vary widely.3–5 A key method used for assessment of CCSVI involves ultrasound of the internal jugular veins (IJVs), vertebral veins (VVs), and deep cerebral veins (DCVs); catheter venography is not as widely used in CCSVI assessments due to its invasive technique.6 Two or more of 5 subcriteria must be met to fulfill the criteria for CCSVI: 1) reflux in IJVs or VVs, 2) reflux in the DCVs, 3) stenosis of IJV, 4) no flow detected in IJVs or VVs, and 5) reverted postural flow.1
To date, no studies have investigated the relation between volume status and CCSVI. There is anecdotal evidence, both from patients and from experience of clinicians, that people with MS tend to be more dehydrated than the general population. Drinking less fluid can help patients self-manage neurogenic bladder symptoms. By measuring urine osmolality, one study demonstrated that 42% of subjects with MS were not adequately hydrated.7 Our goal was to evaluate the effect of hydration status on CCSVI ultrasound results.
METHODS
Standard protocol approvals, registrations, and patient consents
The study was reviewed and approved by the Cleveland Clinic Institutional Review Board. All participants provided written informed consent to participate.
Patients
Sixteen subjects (11 subjects with MS and 5 healthy controls) were recruited from an ongoing CCSVI study. Participants were required to have met 0–4 CCSVI subcriteria1 on their previous CCSVI ultrasound.
Study design
CCSVI ultrasound assessment1 was performed by a single trained sonographer and over-read by a vascular ultrasound physician familiar with CCSVI assessment, both of whom were blinded to disease status and number of CCSVI subcriteria previously met during the separate CCSVI study from which patients were recruited.
CCSVI subcriteria 1, 3, 4, and 5 were assessed. DCV reflux was not assessed in this hydration study since transcranial Doppler examination in the main study has been consistently negative for reflux. After a 12-hour fast, including abstention from fluids, a baseline “dehydrated” CCSVI ultrasound was performed. Patients were then asked to drink 1.5 L of Gatorade over 30–45 minutes, and a second “rehydrated” ultrasound was subsequently performed. Inferior vena cava (IVC) cross-sectional area (CSA) was measured during both studies, and change in IVC CSA was used as a quantitative marker for change in hydration status.
Data analysis
Changes in subcriteria 1, 3, 4, and 5 between the dehydrated and rehydrated states were recorded. The maximal change in CSA was recorded, regardless of whether it occurred in the right or left IJV. Two-tailed paired t tests were used to compare changes between the 2 hydration states. Because of the small sample size, outlier values were not used in the statistical calculations.
RESULTS
Sixteen subjects were recruited: 11 subjects with MS (9 relapsing-remitting MS, 2 primary progressive MS) and 5 healthy controls. Overall, there were 5 men and 11 women, with an average age of 54.9 years.
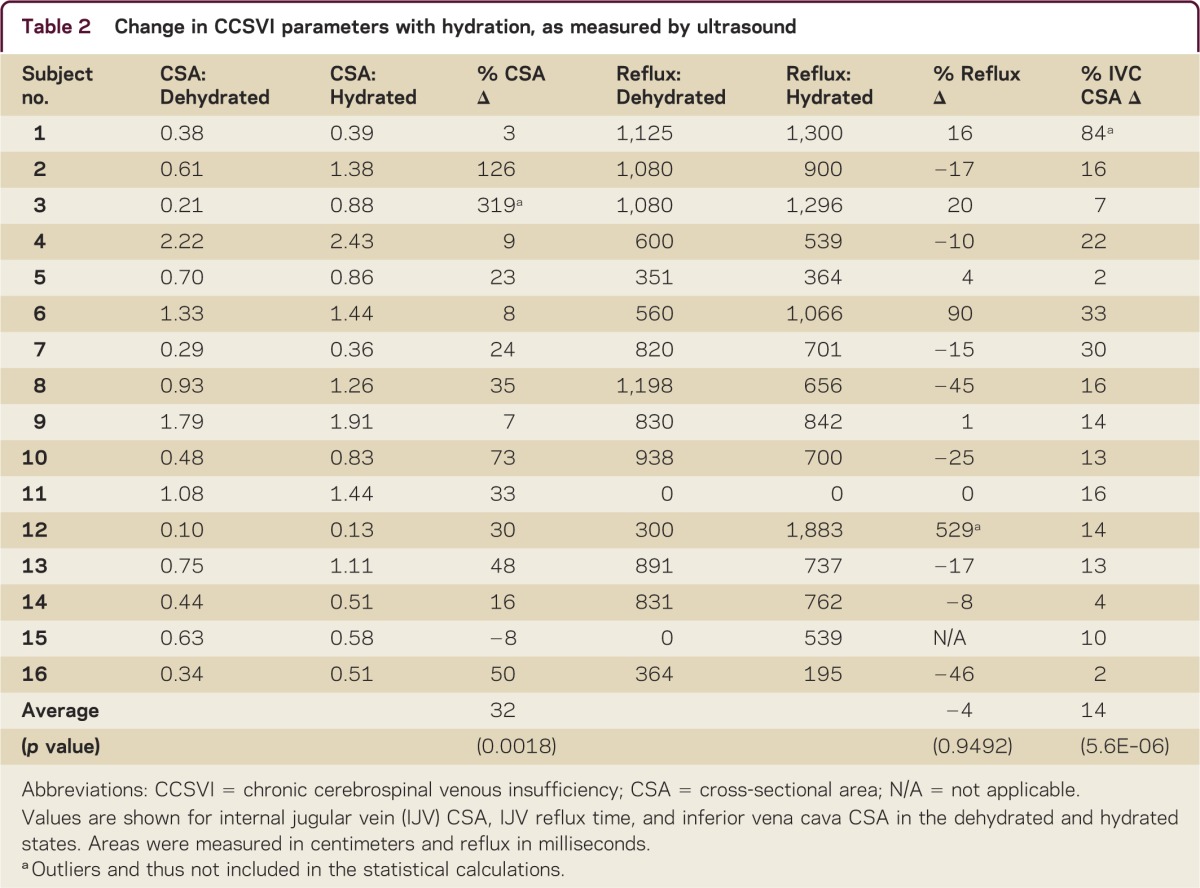
Seven subjects fulfilled the CCSVI criteria in the dehydrated state. Of these, 5 (71%) no longer fulfilled CCSVI criteria after rehydration (table 1). One additional subject met CCSVI criteria only after rehydration. The most common change in criteria was losing the stenosis subcriterion, followed by a change in reflux time. Rehydration decreased reflux time in 8 subjects and increased it in 7; the average change in reflux over all subjects was not significant (table 2). One subject had reverted postural control that normalized with hydration, whereas another had reverted postural control induced by hydration. In 3 subjects, flow became detectable in one vertebral vein in the supine position with rehydration. In 2 of these subjects, there was no detectable flow in one vertebral vein in the upright position despite rehydration, thus not changing subcriterion 4. After rehydration, IVC CSA increased on average by 14% (p = 5.6 × 10−6) and IJV CSA increased on average by 32% (p = 0.0018) (table 2).
Table 1.
Individual CCSVI classification of the 16 subjects in the 2 hydration states
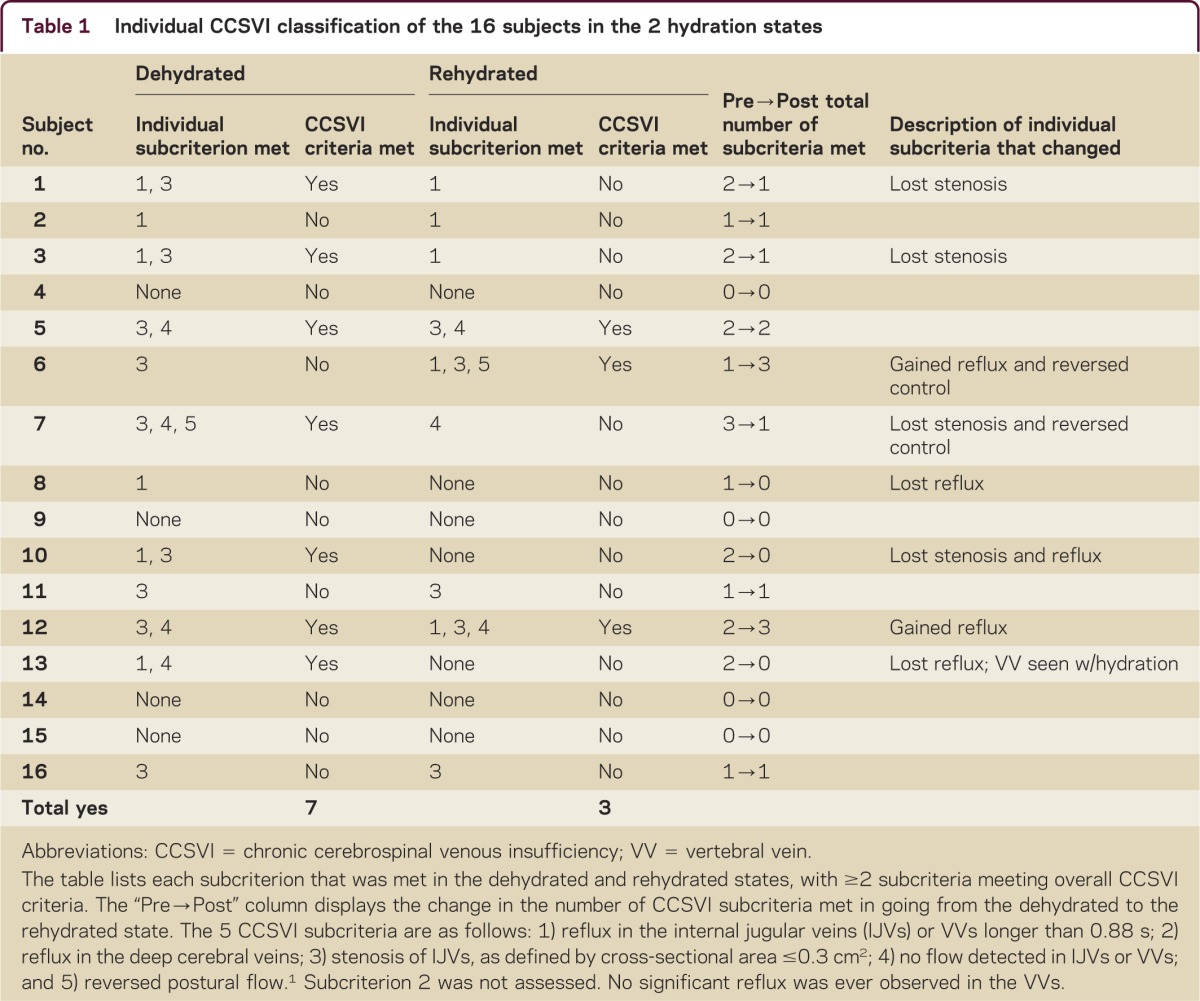
Table 2.
Change in CCSVI parameters with hydration, as measured by ultrasound
DISCUSSION
Studies of CCSVI have yielded conflicting results,3–5 although a meta-analysis of 8 studies suggested a correlation between CCSVI and MS.5 Because the venous system is a low pressure and high compliance system, it is particularly affected by hydration status, and so we hypothesized that hydration may play a substantial role in CCSVI ultrasound assessments. We found that 71% of subjects who met CCSVI criteria while dehydrated no longer met CCSVI criteria after rehydration. Since patients with MS often prefer to drink less fluid because of bladder dysfunction, our results suggest that at least some of the differences between patients with MS and controls without MS in previous CCSVI studies may be explained by differential hydration between patients with MS and controls without MS. We could not draw definite conclusions from our sample size about the effect of hydration on CCSVI within MS subgroups. To our knowledge, no other study has investigated the effect of hydration on MS subgroups or on CCSVI.
Our observations suggest that the sonographic findings of CCSVI may not represent a pathologic state but instead may represent a physiologic state in which hydration status plays a substantial role. When interpreting CCSVI ultrasound findings, care must be taken to recognize the potential effect from patient hydration status.
STUDY FUNDING
Supported by a grant from the Cleveland Clinic Research Program Committee (RPC grant 2010-1074) and a Research Grant (RC 1004-A-5) from the National MS Society (USA).
DISCLOSURES
C.I. Diaconu reports no disclosures. R.J. Fox serves on scientific advisory boards for Biogen Idec and Novartis; serves on the editorial boards of Neurology® and Multiple Sclerosis; serves as a consultant for Allozyne, Avanir, Biogen Idec, Novartis, Questcor, EMD Serono, and Teva Neurosciences; and receives research support from Novartis and the National MS Society. A. Grattan reports no disclosures. A. Rae-Grant has received speaker honoraria from Novartis, Avanir, Biogen Idec, and Teva Neurosciences for speaking; serves on the Evidence Review Team for Neurology; receives publishing royalties for Handbook of Multiple Sclerosis (Springer Healthcare, 2010), Comprehensive Review of Clinical Neurology (Wolters Kluwer, 2012), and 5 Minute Consult in Neurology (Wolters Kluwer, 2012); serves on the speakers' bureau for Biogen Idec; and receives research support from the NIH and the National MS Society. M. Lu has received research support from the National MS Society. H. Gornik serves on an internal DSMB for Roy Greenberg IDE; serves on the editorial board of Vascular Medicine and Current Treatment Options in Cardiovascular Medicine; is author on patents re: Non-invasive diagnosis of lower extremity peripheral artery disease by oscillometric means (license fee payments received) and Remote monitoring of anticoagulation (royalty payments received); serves as Medical Director, Non-Invasive Vascular Laboratory, Cleveland Clinic; and receives research support from Theravasc, Astra-Zeneca, and the NIH/NHLBI. E.S.H. Kim received consulting fees from Philips; received grant support from the American College of Cardiology supported by GE, as well as grant support directly from GE; reviews vascular ultrasound (15% clinical effort) at the Cleveland Clinic Non-Invasive Vascular Laboratory; and receives research support from the Multiple Sclerosis Society. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Zamboni P, Galeotti R, Menegatti E, et al. Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis. J Neurol Neurosurg Psychiatry 2009;80:392–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zamboni P, Galeotti R, Menegatti E, et al. A prospective open-label study of endovascular treatment of chronic cerebrospinal venous insufficiency. J Vasc Surg 2009;50:1348–1358 [DOI] [PubMed] [Google Scholar]
- 3.Doepp F, Paul F, Valdueza JM, Schmierer K, Schreiber SJ. No cerebrocervical venous congestion in patients with multiple sclerosis. Ann Neurol 2010;68:173–183 [DOI] [PubMed] [Google Scholar]
- 4.Zivadinov R, Marr K, Cutter G, et al. Prevalence, sensitivity, and specificity of chronic cerebrospinal venous insufficiency in MS. Neurology 2011;77:138–144 [DOI] [PubMed] [Google Scholar]
- 5.Laupacis A, Lillie E, Dueck A, et al. Association between chronic cerebrospinal venous insufficiency and multiple sclerosis: a meta-analysis. CMAJ 2011;183:E1203–E1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simka M, Ludyga T, Latacz P, Kazibudzki M. Diagnostic accuracy of current sonographic criteria for the detection of outflow abnormalities in the internal jugular veins. Phlebology 2013;28:285–292 [DOI] [PubMed] [Google Scholar]
- 7.Collett J, Dawes H, Cavey A, et al. Hydration and independence in activities of daily living in people with multiple sclerosis: a pilot investigation. Disabil Rehabil 2011;33:1822–1825 [DOI] [PubMed] [Google Scholar]


