Abstract
Objective. To determine the impact of performing critical-thinking and reflection assignments within interdisciplinary learning teams in a biochemistry course on pharmacy students’ and prospective health professions students’ collaboration scores.
Design. Pharmacy students and prospective medical, dental, and other health professions students enrolled in a sequence of 2 required biochemistry courses. They were randomly assigned to interdisciplinary learning teams in which they were required to complete case assignments, thinking and reflection exercises, and a team service-learning project.
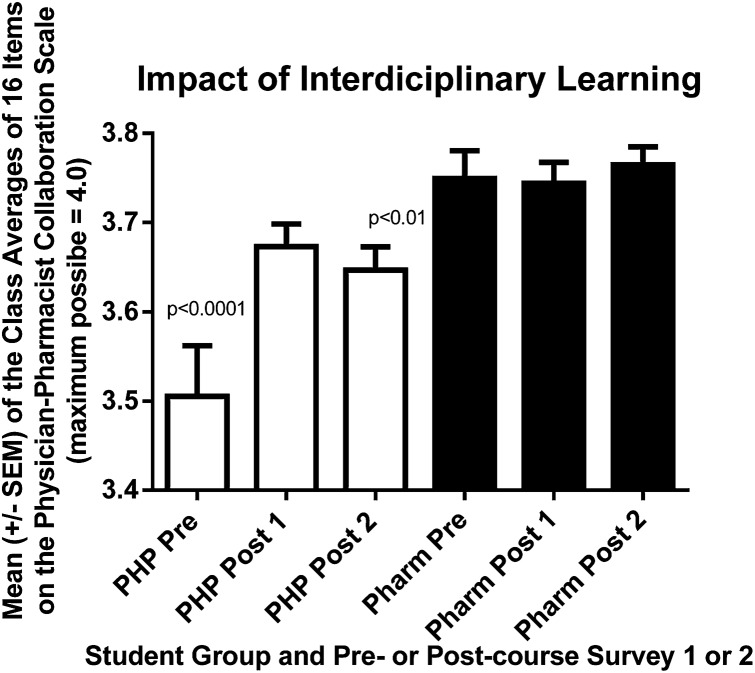
Assessment. Students were asked to complete the Scale of Attitudes Toward Physician-Pharmacist Collaboration prior to the first course, following the first course, and following the second course. The physician-pharmacist collaboration scores of prospective health professions students increased significantly (p<0.001).
Conclusions. Having prospective health professions students work in teams with pharmacy students to think and reflect in and outside the classroom improves their attitudes toward physician-pharmacist collaboration.
Keywords: interprofessional education, interdisciplinary education, health profession students, pharmacy students, medical students, dental students, empathy, service learning, biochemistry
INTRODUCTION
Interdisciplinary collaboration and teamwork are part of the professional behaviors of healthcare providers and promote patient safety and positive outcomes.1-9 Pharmacists collaboration with physicians fosters optimal drug-therapy selection, improved patient drug-therapy adherence and self-care skills, enhanced communication about drug interactions,10,11 and cost-effective use of medication with fewer medication errors.12,13
Pharmacists are trained and expected to collaborate with physicians and other healthcare professionals in patient-centered education and care. Thus, pharmacist-physician collaboration and interprofessional education are encouraged in dental, medical, and pharmacy schools.14 Training in each of these professions is, to a large extent, specialized, so interprofessional collaboration should improve therapeutic outcomes and optimize patient care. The growing urgency for this collaboration stems in part from rapid advancements in dental, medical, and pharmaceutical sciences which increase the probability of drug interactions and drug-related morbidity. These advancements also likely contribute to higher chances of medical errors and rising health care costs. These complexities led Schellens and associates15 to conclude that “rational and tailored drug therapy cannot be implemented in its full width when the discipline is applied only by physicians.”
Based on characteristics desirable in collaborations among healthcare professionals, Hojat and Gonnella designed16 an instrument to measure pharmacy and medical students’ attitudes toward interprofessional collaboration.17,18 These characteristics included accountability, communication, education, and shared decisions and responsibilities.17,19,20 Ultimately, 3 reliable factors emerged for the instrument: responsibility and accountability, shared authority, and interprofessional education.16-18 These authors and VanWinkle and colleagues later validated this instrument.17,18
At Midwestern University, we used the instrument to show that even a single workshop exercise to foster understanding between medical and pharmacy students led to a small improvement in their physician-pharmacist collaboration scores.21 We also found, however, that the collaboration scores of pharmacy students significantly exceeded those of medical students, and that this difference persisted even though medical students’ scores improved after participating in the workshop. The effect size for the difference between pharmacy and medical students’ collaboration scores was of crucial practical importance.17,21 Consequently, we designed this pilot study to determine whether the collaboration scores of prospective medical, dental, and other health professions students could be raised to those of pharmacy students simply by having these students work regularly with pharmacy students in interdisciplinary learning teams to complete critical-thinking and reflection exercises, case assignments, and a service-learning project during 2 required 10-week biochemistry courses. In our prior study, prospective health professions students took the same biochemistry courses as pharmacy students, but the 2 groups of students worked in their own discipline-specific teams rather than on interdisciplinary ones.
Also in the prior study, the physician-pharmacist collaboration scores of prospective health professions students’ mirrored those of medical students.21 Since the prospective health professions students in the present study were enrolled with pharmacy students in the same biochemistry courses, it was relatively easy for us to design activities in the courses in which these 2 groups of students worked together within integrated teams. We conducted this study to determine whether the physician-pharmacist collaboration scores of prospective health professions students would increase by a crucially important amount after working regularly with pharmacy students to perform critical thinking and reflection in interdisciplinary learning teams during a sequence of 2 required biochemistry courses.22
DESIGN
The pharmacy students and prospective health professions students enrolled in a series of 2 required 10-week biochemistry courses in fall quarter 2012 and winter quarter 2013. Course content in the fall term focused primarily on metabolism and application of related laboratory tests such as complete blood count and comprehensive metabolic panel. The course included 30 lecture hours and 8 team workshop exercises (Table 1). A sample workshop exercise is shown in Appendix 1. The fall course also included 4 team discussion/reflection sessions.
Table 1.
Workshop Topics for Teams of Students in Biochemistry Courses
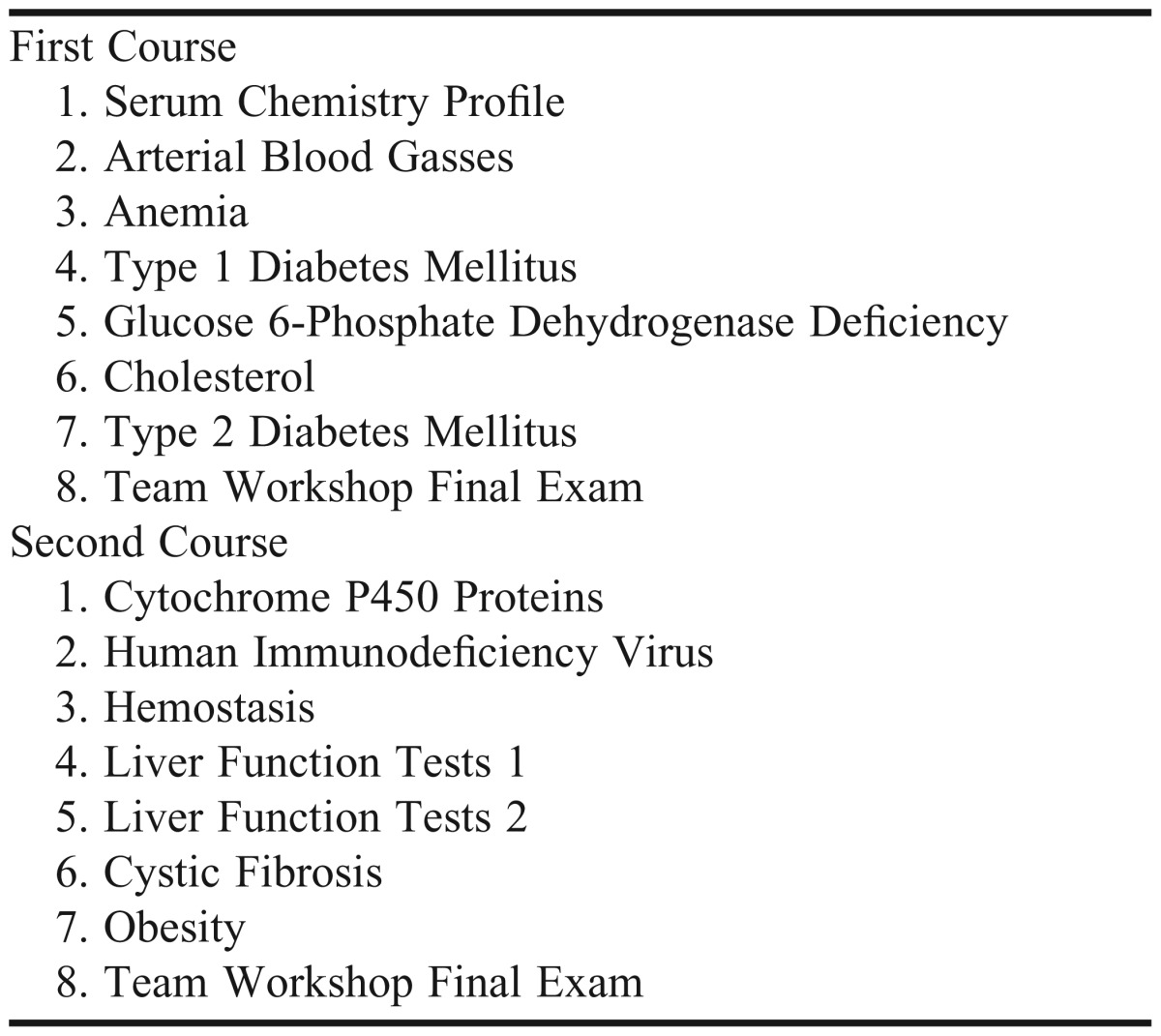
Content of the second course focused on cell biology, genetics, nutrition, and application of pertinent clinical laboratory data. The second course was composed of 40 lecture hours, 8 team workshop exercises (Table 1), a team service-learning project, and 3 team discussion/reflection sessions concerning the project. Teams were expected to begin planning a team service-learning project in the first course for completion during the second course.
At the beginning of the first course students were randomly assigned to interdisciplinary teams of 1 to 3 (usually 2) prospective health professions students and 4 to 6 pharmacy students. Students completed workshop exercises within their teams during regularly scheduled, 50-minute class sessions. Teams also were required to schedule seven 60-minute discussion and reflection sessions at times of their choosing, but they had to be at regular intervals throughout the fall and winter quarters.
The 4 discussions during the fall quarter concerned some aspect of the difficulties and rewards of healthcare professions, health professions education, and life. Students were free to select their own topics or use ones that were suggested (see sample topic in Appendix 1). Written discussion minutes and reflections were submitted by teams at regular intervals throughout the fall and winter quarters and graded based on the amount of critical thinking and reflection exhibited as we defined previously.23 Grades ranged from 80% (thinking and reflection but not critical thinking and reflection exhibited) to 100% (extensive critical thinking and reflection exhibited). Grades assigned by independent assessors for critical reflection (ie, the course director and another faculty member) correlate well (r=0.92) as we report elsewhere.24
In the second course, much of the reflection was expected to be inspired by experiences in the team service-learning project. Teams were expected to choose a project producing experiences they could integrate with biochemistry course content (eg, diabetes coach or service to provide nutrition to those in need). Each team was expected to perform a combined total of approximately 27 hours of service. Most teams divided the work so that each team member contributed about 4 hours of service to the project. Teams met 3 times during the quarter in which the project was performed to discuss their projects and student members’ critical thinking and reflections about their contributions to the project and related issues. Written minutes and individual and team reflections were submitted for grading. The projects were graded based on the amount of critical thinking and reflection exhibited as we have defined and discussed previously.23,24 The project grade contributed a total of 16% toward students’ final grades. In summary, students’ teamwork in the series of 2 required biochemistry courses included completion of 16 biochemistry workshop exercises, 7 team critical-thinking and reflection assignments, and 1 team service-learning project.
EVALUATION AND ASSESSMENT
All students enrolled in the course (212 pharmacy students and 82 prospective health professions students) were invited to complete the Scale of Attitudes Toward Physician-Pharmacist Collaboration17 immediately prior to the introduction to the courses (pre-course survey) and just after the final examinations of the first course (post-course survey 1) and the second course (post-course survey 2). Students were asked to mark their survey forms with a unique 4-digit or letter identifications (ID) code of their choice so that their scores on the pre-course survey could be matched to their scores on the post-course surveys for more powerful statistical analysis. We also asked students to complete the Jefferson Scale of Empathy (HPS-Version for administration to pharmacy students22) prior to the introduction to the courses and after completion of the second course.
The average age of the pharmacy students was 23 years (range 19 to 44 years) and 66% were female. Approximately 51% of the students were Caucasian, 41% were Asian, 5% were Hispanic, 2% were African American, and 1% was other/not reported. The average age of the prospective health professions students was 24 years (range 21 to 31 years) and 37% were female. Approximately 66% were Caucasian, 27% were Asian, 5% were Hispanic, and 2% were other/not reported.
The prospective health professions students were pursuing either a master of arts in biomedical sciences or master of biomedical sciences degree in order to improve their applications to medical, dental, or other health professions colleges and schools. The prospective health professions students in the present study overwhelmingly aspired to become either medical physicians (57%) or dental physicians (35%). The remaining students expressed desires for careers as physician assistants (2%), biomedical research scientists (5%), or pharmacists (1%).
Statistical analyses were performed using GraphPad Prism 5 Software, Inc (LaJolla, CA). We determined the mean and median collaboration scores for each group of students at each time the survey was administered. The distributions of these collaboration scores deviated significantly from Gaussian distributions and were skewed dramatically toward the highest possible values (D’Agostino and Pearson omnibus normality test).21 Consequently, analysis of variance (ANOVA) could not be used to compare mean values of the survey scores obtained at different times or for different groups. Instead, median survey scores were compared statistically using the Kruskal-Wallis Test with Dunn’s Multiple Comparison Test.
When survey scores could be matched for the same individual using their unique ID code, the series of matched scores were compared using repeated measures ANOVA with Newman-Keuls Multiple Comparison Test. An effect size 25,26 value was also calculated from these matched samples of student data, because only the differences among matched scores need to form Gaussian distributions; the values themselves need not do so. This repeated measures ANOVA yielded the pertinent r value using GraphPad Prism 5 Software, and the r value equals the effect size (ES) value.26
We also compared the collaboration scores that had been obtained each time the survey was administered for each class of students as a whole. To determine class survey scores, we calculated the average score of the class for each of the 16 survey items. We then calculated the mean of these 16 average scores. These mean values were compared using repeated measures ANOVA with Newman-Keuls Multiple Comparison Test, as the averages for each item could be paired on an item-by-item basis. The distributions of the 16 average scores also followed Gaussian distributions (D’Agostino and Pearson omnibus normality test). This study was reviewed and found to fulfill the criteria for exemption by the Midwestern University Institutional Review Board.
Team Critical Thinking and Reflection
All 40 interdisciplinary student-learning teams in the biochemistry courses displayed some critical thinking and reflection in at least 1 of their 7 written team reflection and discussion papers, and 32 of the 40 teams performed such thinking and reflection numerous times in at least 1 of their papers (ie, grade of >95%). Our definition of critical reflection required that students recognize how their thoughts and behavior did not match their humanistic and professional values and consider and plan how to better align their values and behavior.23,24 The latter realization was by far the most frequent outcome of students’ critical thinking and reflection. For example, in thinking about the sometimes poor treatment of elderly patients in nursing homes, one student remarked that they often times neglect the way they make elderly persons feel at work (a retail pharmacy) because they are impatient with them when the older person counts out their payment from their change purse. Similarly, another team of students came to realize that even with the stress of professional training, they need to learn to work in interdisciplinary teams now, because the stakes and stress will only be higher later when they are working in their chosen healthcare professions.
Team Service Learning Projects
The 40 teams of students selected a variety of service-learning projects. Eight teams attempted to educate the public at some combination of pharmacies, grocery stores, shopping malls, universities, and the YMCA about health-related issues such as hypertension, influenza (and other) vaccines, diabetes, or good nutrition. Similarly, 7 teams volunteered at rehabilitation centers, retirement homes, soup kitchens, or a holiday outreach to underserved children. By far the most teams (25) volunteered at an organization that distributed food to undernourished children overseas. Other volunteers at these food distribution sites frequently included adult community members and their children. Consequently, many of the student teams came to realize that community cooperation as well as interprofessional collaboration are needed to best care for the health of others.
Impact of Team Critical Thinking, Reflection, and Service Learning
Of the 212 first-year pharmacy students enrolled in the course, 99% completed the pre-course survey on physician-pharmacist collaboration, 95% completed the post-course 1 survey, and 77% completed the post-course survey 2. Of the 82 prospective health professions students, 100% completed the pre-course survey, 90% completed the post-course 1 survey, and 82% completed the post-course 2 survey. The scores of 56% of the prospective health professions students who completed the post-course survey 2 could be matched to both their post-course survey 1 score and their pre-courses survey score for more powerful pair-wise statistical analysis.
There was a significant increase in the physician-pharmacist collaboration scores of prospective health professions students from a median of 57 out of a maximum possible score of 64 on the first day of class to median scores of 61 and 60 at the ends of the first and second biochemistry courses, respectively (p=<0.001). The first of these median scores (57) was significantly lower than each of the median scores for pharmacy students (p<0.001), while the other 2 median scores for prospective health professions students were not significantly different from those of pharmacy students. No significant change was observed in the collaboration scores of pharmacy students (median scores of 61, 62, and 63 for the pre-course survey, post-course survey 1, and post-course survey 2, respectively).
Analysis of matched prospective health professions student samples was also highly significant. These matched data samples reflected the total data samples well, with median scores for the sequence of 3 surveys of 56, 60, and 60, respectively (p <0.001 for increases in median post-course survey 1 and 2 scores). The ES (r) value for the latter increase was 0.44. When a greater proportion of prospective health professions students’ post-course survey 1 scores could be paired to their pre-course survey scores, this ES value was 0.60.
The increase in prospective health professions students’ collaboration scores was attributed especially to items 2, 7, 8, and 11 of the scale. When the median values for each of the 16 items on the scale obtained on the pre-course survey were compared to the median values of each of the 16 items on the post-course surveys 1 and 2, significant increases in scores were observed for items 2 and 7 (p<0.01) and for items 8 and 11 (p<0.05), but not for the other items.
We also compared the collaboration scores, obtained each time the survey was administered, for each class of students as a whole. When we compared the means of the class averages for each of the 16 items obtained for the prospective health professions class in the pre-course survey, to those obtained in each of the post-course surveys, the improvements in mean score of the prospective health professions students was highly significant (p<0.001, Figure 1). Thus, there was an increase in the average value of almost every item on the collaboration survey instrument for the prospective health professions students (not solely on items 2, 7, 8, and 11). The repeated measures ANOVA used to assess these data (Figure 1) also yielded an ES (r) value of 0.72 for the improvement in the prospective health professions class scores. Moreover, the pharmacy class scored significantly higher than did the prospective health professions class every time the survey was administered (p<0.01). For the smallest difference between the classes on the post-course survey 1 (Figure 1), the ES (r) value for the difference between the prospective health professions students and the pharmacy students was 0.62. (There was no significant change in the pharmacy students’ scores over the course of the study (Figure 1).
Figure 1.
Changes in pharmacy (Pharm) and prospective healthcare professions (PHP) students’ class physician-pharmacist collaboration scores in association with completing critical thinking and reflection assignments in interdisciplinary learning teams. The total collaboration scores for the classes as wholes can be calculated by multiplying the means of the 16 items shown in the figure by 16.
Nevertheless, pharmacy students’ empathy scores increased significantly from a mean of 109.9±12.7 on pre-course survey to a mean of 112.8±15.7 on post-course survey 2 (p=0.045). When the class average scores on each of the 20 items of the Jefferson Empathy Scale were assessed using a paired t test for each pair of 20 items, the increase in the empathy score was also significant (p=0.027). In the later case, the ES (r) value for the class as a whole was 0.48. No change was observed in the empathy scores of individual prospective health professions students or in their group as a whole between the pre-course survey and post-course survey 2.
DISCUSSION
Prospective health professions students’ physician-pharmacist collaboration scores increased to near those of pharmacy students when these students worked together on interdisciplinary learning teams to perform critical thinking and reflection. This increase was most apparent when the mean change in scores was assessed on the basis of the health professions students class as a whole (Figure 1). The collaboration scores of pharmacy students also increased, although this increase was not significant. Pharmacy students were, however, likely influenced through completion of critical-thinking and reflection exercises in teams with prospective health professions students. Pharmacy students and the class as a whole had significantly higher empathy scores at the end of the biochemistry courses than at the beginning. The ES (r) value for this change by the class as a whole was of crucial practical importance.25,26
We attribute the lack of a significant change in the collaboration scores of pharmacy students to their scores already being near the maximum possible score prior to beginning the biochemistry courses. As a class, the pharmacy students were eager to collaborate before their training had begun (Figure 1). Consequently, significant increases in the median and mean scores were more difficult to realize. Also, teams were composed of more pharmacy students (usually 5 or 6) than prospective health professions students (usually 2), so pharmacy students may have had more impact on prospective health professions students than vice versa. Most prospective health professions students also were receptive to interprofessional education efforts even before the biochemistry courses began (median individual prospective health professions students’ scores on the 3 education items on the collaboration survey instrument were equal to the maximum possible score of 12), suggesting they were ready to learn the importance of collaboration.
In a prior study, we found that even a single interprofessional workshop to improve mutual understanding led to small but significant improvements in the collaboration scores of medical, prospective health profession students, and pharmacy students.21 The demographics of prospective health-professions students in this prior study were virtually the same as those of students in the present study. In the prior study, the total collaboration scores of students did not change until the interprofessional workshop took place halfway through the students’ second course in biochemistry. In spite of improvements in scores after this single workshop, medical and prospective health professions students’ scores remained well below the scores of pharmacy students, and this difference between pharmacy and prospective health professions or medical students was of crucial practical importance.21
Building on our previous findings, we designed the present study to determine whether the collaboration scores of prospective health professions students would increase to nearer those of pharmacy students if they worked together regularly with pharmacy students to think and reflect in interdisciplinary learning teams. Prior to this study, prospective health professions students took the same biochemistry courses as pharmacy students, but the 2 groups of students worked in their own discipline-specific teams rather than on interdisciplinary ones. In response to this change in team composition, the collaboration scores of prospective health professions students not only increased, but the scores increased by an amount considered to be of near crucial practical importance25 equivalent to reducing the death rate from 72% under control conditions to 28% under experimental conditions.26 The impact of regular critical thinking and reflections by interdisciplinary teams was even more profound when the class, rather than individual students, was viewed as the subject of study. Hence, the prospective health professions class as a whole became considerably more eager to collaborate, at least according to its collaboration survey scores.
The forces mitigating against such changes in the scores of prospective health professions students may be powerful. As we discussed previously,17 the “principle of least interest” may apply also to differences in the collaboration scores of pharmacy and prospective health professions students. According to this principle, proposed by Waller and Hill in the context of family relations,27 those in a more powerful position historically, are less likely to express eagerness for collaborative relationships with others who are lower in the power hierarchy.17 The principle was likely in operation in several studies of interactions between nurses and physicians.28-33 In the case of students, pharmacy and social work students expressed more positive attitudes toward interprofessional collaboration than did medical students.34 In one study, however, Turkish medical students demonstrated a more positive attitude toward collaboration than did nursing students.35
Despite the possible force of the principle of least interest, we show that prospective health professions students, the vast majority of whom aspire to become medical or dental physicians, could be influenced to become significantly more eager to collaborate with pharmacists simply through working regularly with pharmacy students to perform critical-thinking and reflection exercises in biochemistry learning teams. Whether medical and dental students can be moved in the same way will require further research. Similarly, whether the attitudes of practicing medical and dental physicians towards collaboration with pharmacists will improve the more they work together toward common goals also still must be determined.
This work together needs to include projects in which different healthcare professionals (or healthcare professional students) share authority and responsibility so they can come to trust one another and establish more equal relationships.36 Such shared authority and responsibility is easier to include in projects during training. In addition, prospective health professions students may be even more impressionable than medical or dental students, as they are one step further removed from their goals to be medical or dental physicians. Perhaps by designing courses to move students to become eager to collaborate at the earliest possible times in their training, we can inspire them to continue to collaborate more effectively throughout their careers.
These investigations did not include randomly assigned control groups, but we did establish in a previous study that the physician-pharmacist collaboration scores of control groups of prospective health professions students, medical students, and pharmacy students did not increase when they did not work together in interprofessional teams.21 Moreover, 4 of the prospective health professions students in the present study are striving to become biomedical research scientists and 1 wants to become a pharmacy student. However, students who want to be scientists may be less likely to be enthusiastic about physician-pharmacist collaboration than are prospective medical or dental students, while the prospective pharmacy student likely had a high collaboration score before the biochemistry course began. Consequently, survey results from the latter 5 students likely made the observed changes in health professions students collaboration scores somewhat less dramatic.
Prospective health professions students were, however, outnumbered by pharmacy students on teams. Accordingly, how students’ scores are affected when team membership is more balanced or even skewed in the reverse direction needs to be determined. Moreover, the single institution nature of the present findings and the focus on prospective health professions students limits the ability to generalize the observations. This study and our previous studies need to be expanded to medical and dental students and repeated at other institutions.
CONCLUSIONS
Working regularly with pharmacy students on exercises and assignments to perform critical thinking and reflection in biochemistry courses improved the physician-pharmacist collaboration scores of prospective health professions students. This increase was of crucial practical importance both when individual students and the class as a whole was the subjects of study. Future goals include raising and maintaining the collaboration scores of medical and dental students to or near those of pharmacy students.
Appendix 1. Sample Workshop Exercise – G6PD Deficiency
Objective – To understand the biochemical basis and consequences of G6PD deficiency
- I. Glucose 6-Phosphate Dehydrogenase (G6PD)
- A. Glucose 6-phosphate dehydrogenase catalyzes the rate-limiting step in the hexose monophoshate pathway, the reduction of NADP+ to NADPH.
- 1. NADPH is needed to maintain glutathione in its reduced form.
- 2. Reduced glutathione can chemically detoxify H2O2 produced in response to oxidant stress.
- B. Glucose 6-phosphate dehydrogenase is required in erythrocytes for production of NADPH; other cells have additional pathways to produce NAPDH.
- II. Oxidant Stress and Erythrocytes
- A. Erythrocytes carry oxygen, a very potent oxidizing agent. Certain drugs, infections and fava beans can induce additional oxidant stress.
- B. If H2O2 is not detoxified, it will oxidize proteins and lipids and damage cells. Erythrocytes will lyse and hemolytic anemia will result.
- III. Basis of Glucose 6-Phosphate Dehydrogenase Deficiency
- A. There are more than 400 genetic variants (mutations) in the G6PD enzyme that result in an abnormality in the activity or concentration of G6PD.
- 1. There are 4 major classes of G6PD deficiency.
- 2. Clinical symptoms correlate to the residual enzyme activity.
- B. G6PD Deficiency is the most common human enzyme deficiency, affecting an estimated 400 million individuals worldwide, particularly those in regions where malaria is endemic.
- 1. Most prevalent in Africa, affecting up to 20% of the population.
- 2. Affects 4-30% of the population in Mediterranean regions.
- 3. Also found in Southeast Asia.
- C. The gene for G6PD is carried on the X chromosome. Inheritance follows an X-linked pattern, with many more males than females affected.
- 1. Females with 1 copy of a mutant G6PD gene are carriers.
- 2. Males with 1 copy of a mutant G6PD gene express the trait.
- IV. Signs and Symptoms of G6PD Deficiency
- A. Most individuals with G6PD deficiency have no signs or symptoms unless they experience a strong oxidant stress.
- B. Neonatal jaundice is observed in many newborns with G6PD deficiency.
Case
A 45 year-old, African American male, Alfred Carter Jr., presents with sudden onset of jaundice, pallor, dark urine, abdominal and back pain, shortness of breath and fatigue. Although the patient is serving a 30-year prison sentence, he is currently in the hospital receiving intravenous recombinant urate oxidase (rasburicase, 0.2 mg/kg) once daily in preparation for his first cycle of chemotherapy for stage IIB Burkitt lymphoma. His second of six daily rasburicase treatments was yesterday. The purpose of raspuricase treatment is to lower the plasma uric acid (urate) concentration. The patient’s current laboratory data and his data prior to beginning treatment are shown in the table below. Further studies show that the patient has a short-lived (deficient) form of glucose-6-phosphate dehydrogenase A (i.e., G6PD-A-).
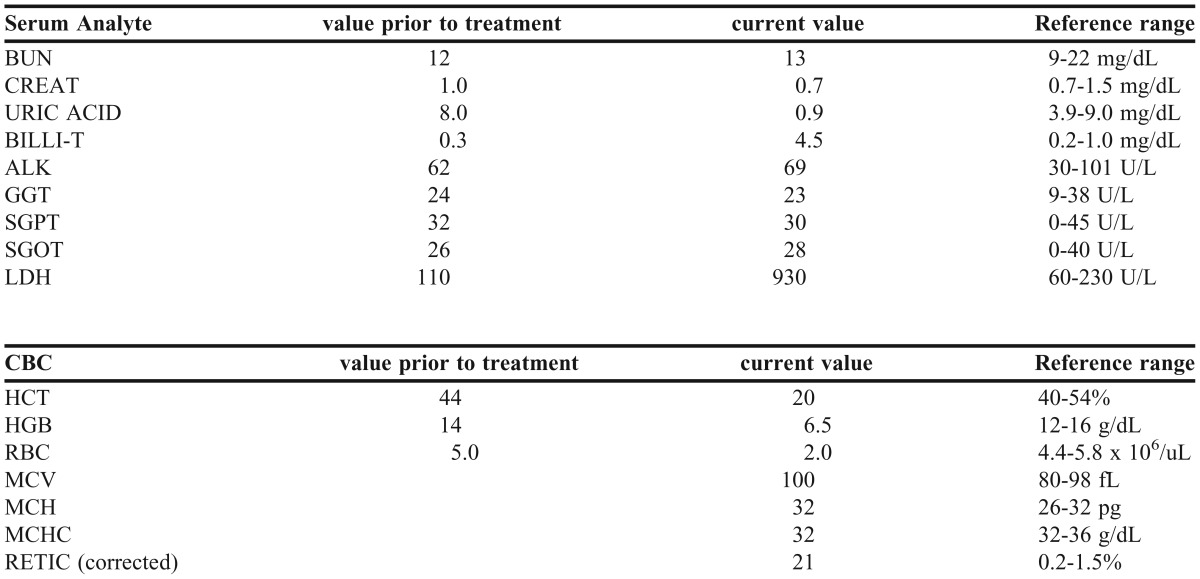
1. Was the patient’s serum uric acid (urate) concentration successfully lowered in preparation for his chemotherapy? Please explain your answer briefly.
2. Below is the two-step reaction catalyzed by urate oxidase. Explain why the reaction posed an oxidant stress to the patient’s red blood cells.
-
urate ➝ H2O2 + intermediates
intermediates ➝ allantoin + CO2
3. Urate (uric acid) is also considered to be a major antioxidant in human blood where it acts as an efficient scavenger of highly reactive oxygen species. Explain how the change in the patient’s serum (and plasma) urate concentration along with the urate oxidase-catalyzed reaction above might have acted synergistically to produce a large oxidant stress to Alfred’s red blood cells.
4. Was the patient anemic before or after rasburicase treatment? If he was anemic at either or both of these times, describe the mechanism(s) by which his anemia likely developed.
5. If he has anemia, how should it be treated?
6. Which of the patient’s signs and symptoms are consistent with problems sometimes associated with a G6PD deficiency?
7. What are the underlying reasons for these signs and symptoms?
8. This patient is 45 years of age. Is it unusual that he was not diagnosed with a G6PD deficiency sooner? Explain.
9. The patient has two sons. Their mother does not carry the gene encoding G6PD-A-. Are his children and future grandchildren at risk for G6PD deficiency? If yes, which ones and why? If not, why not?
10. Use Google Scholar or PubMed to identify two other drugs or foods the patient should avoid. (Please cite your reference(s).)
Possible topic for your next Team Discussion/Reflection.
Assume you are part of the team of healthcare professionals treating Mr. Carter. What biases do you or members of your biochemistry team have against Mr. Carter that might adversely affect his treatment? How will you or members of your biochemistry team begin to mitigate these biases?
REFERENCES
- 1.Baldwin D. Some historical notes on interdisciplinary and interprofessional education and practice in the USA. J Interprofl Care. 2007;21(suppl 1):23–37. doi: 10.1080/13561820701594728. [DOI] [PubMed] [Google Scholar]
- 2.Veloski J, Hojat M. Measuring specific elements of professionalism: empathy, teamwork, and lifelong learning. In: Stern TD, editor. Measuring Medical Professionalism. Oxford: Oxford University Press; 2006. pp. 117–145. [Google Scholar]
- 3.Fagin CM. Collaboration between nurses and physicians: no longer a choice. Acad Med. 1992;67(5):295–303. doi: 10.1097/00001888-199205000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Papa PA, Rector C, Stone C. Interdisciplinary collaborative training for school-based health professionals. J Sch Health. 1998;68(10):415–419. doi: 10.1111/j.1746-1561.1998.tb06320.x. [DOI] [PubMed] [Google Scholar]
- 5.Clemmer TP, Spuhler VJ, Berwick DM, Nolan TW. Cooperation: the foundation of improvement. Ann Intern Med. 1998;128(12):1004–1009. doi: 10.7326/0003-4819-128-12_part_1-199806150-00008. [DOI] [PubMed] [Google Scholar]
- 6.Poulton BC, West MA. Effective multidisciplinary teamwork in primary health care. J Adv Nurs. 1993;18(6):918–925. doi: 10.1046/j.1365-2648.1993.18060918.x. [DOI] [PubMed] [Google Scholar]
- 7.Nkansah NT, Brewer JM, Connors R, Shermock KM. Clinical outcomes of patients with diabetes mellitus receiving medication management by pharmacists in an urban private physician practice. Am J Health Syst Pharm. 2008;65(2):145–149. doi: 10.2146/ajhp070012. [DOI] [PubMed] [Google Scholar]
- 8.Carter BL, Bergus GR, Dawson JD, et al. A cluster randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. J Clin Hypertens. 2008;10(4):260–271. doi: 10.1111/j.1751-7176.2008.07434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kiel PJ, McCord AD. Pharmacist impact on clinical outcomes in a diabetes disease management program via collaborative practice. Ann Pharmacother. 2005;39(11):1828–1832. doi: 10.1345/aph.1G356. [DOI] [PubMed] [Google Scholar]
- 10.McDonough RP, Doucette WR. Dynamics of pharmaceutical care: developing collaborative working relationships between pharmacists and physicians. J Am Pharm Assoc. 2001;41(5):682–692. [Google Scholar]
- 11.Brock KA, Doucette WR. Collaborative working relationships between pharmacists and physicians: an exploratory study. J Am Pharm Assoc (Wash). 2004;44(3):358–365. doi: 10.1331/154434504323063995. [DOI] [PubMed] [Google Scholar]
- 12.Sweeney MA. Physician-pharmacist collaboration: a millennial paradigm to reduce medication errors. J Am Osteopath Assoc. 2002;102(12):678–681. [PubMed] [Google Scholar]
- 13.Davies JG, Horne R, Bennett J, Stott R. Doctors, pharmacists and the prescribing process. Br J Hosp Med. 1994;52(4):167–170. [PubMed] [Google Scholar]
- 14.Zillich AJ, Milchak JL, Carter BL, Doucette WR. Utility of a questionnaire to measure physician-pharmacist collaborative relationships. J Am Pharm Assoc. 2006;46(4):453–458. doi: 10.1331/154434506778073592. [DOI] [PubMed] [Google Scholar]
- 15.Schellens JHM, Grouls R, Guchelaar HJ, et al. The Dutch model for clinical pharmacology: collaboration between physician- and pharmacist-clinical pharmacologist. Br J Clin Pharmacol. 2008;66(1):146–147. doi: 10.1111/j.1365-2125.2008.03156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hojat M, Gonnella JS. An instrument for measuring pharmacist and physician attitudes toward collaboration: preliminary psychometric data. J Interprof Care. 2011;25(1):66–72. doi: 10.3109/13561820.2010.483368. [DOI] [PubMed] [Google Scholar]
- 17.Van Winkle LJ, Fjortoft N, Hojat M. Validation of an instrument to measure pharmacy and medical students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2011;75(9) doi: 10.5688/ajpe759178. Article 178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hojat M, Spandorfer J, Isenberg GA, Vergare MJ, Fassihi R, Gonnella JS. Psychometrics of the scale of attitudes toward physician–pharmacist collaboration: A study with medical students. Med Teach. 2012;34(12):e833–e837. doi: 10.3109/0142159X.2012.714877. [DOI] [PubMed] [Google Scholar]
- 19.Coluccio M, Maguire P. Collaborative practice: becoming a reality through primary nursing. Nurs Adm Q. 1983;7(4):59–63. [PubMed] [Google Scholar]
- 20.Braggs JG, Schmitt MH. Collaboration between nurses and physicians about care decisions. Image J Nurs Sch. 1988;20(3):145–149. doi: 10.1111/j.1547-5069.1988.tb00055.x. [DOI] [PubMed] [Google Scholar]
- 21.Van Winkle LJ, Bjork BC, Chandar N, et al. Inter-professional workshop to improve mutual understanding between pharmacy and medical students. Am J Pharm Educ. 2012;76(8) doi: 10.5688/ajpe768150. Article 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fjortoft N, Van Winkle LJ, Hojat M. Measuring empathy in pharmacy students. Am J Pharm Educ. 2011;75(6):Article 109. doi: 10.5688/ajpe756109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Winkle LJ, Robson C, Chandar N, et al. Use of poems written by physicians to elicit critical reflection by students in a medical biochemistry course. J Learn Through Arts. 2011;7(1):Number 1. [Google Scholar]
- 24.Van Winkle LJ, La Salle S, Richardson L, et al. Challenging medical students to confront their biases: a case study simulation approach. Med Sci Educ. 2013;23(2):217–224. [Google Scholar]
- 25.Hojat M, Xu G. A visitor’s guide to effect size: statistical versus practical significance of research findings. Adv Health Sci Educ. 2004;9(3):241–249. doi: 10.1023/B:AHSE.0000038173.00909.f6. [DOI] [PubMed] [Google Scholar]
- 26.Rosenthal R, Rubin DB. A simple, general purpose display of magnitude of experimental effect. J Educ Psychol. 1982;74(2):166–169. [Google Scholar]
- 27.Waller W, Hill R. The Family: A Dynamic Interpretation. New York: Dryden Press; 1951. [Google Scholar]
- 28.Hojat M, Gonnella JS, Nasca TJ, et al. Comparisons of American, Israeli, Italian and Mexican physicians and nurses on the total and factor scores of the Jefferson Scale of Attitudes toward physician-nurse collaborative relationships. Int J Nurs Stud. 2003;40(4):427–435. doi: 10.1016/s0020-7489(02)00108-6. [DOI] [PubMed] [Google Scholar]
- 29.Garber JS, Madigan EA, Click ER, Fitzpatrick JJ. Attitudes toward collaboration and servant leadership among nurses, physicians and residents. J Interprof Care. 2009;23(4):331–340. doi: 10.1080/13561820902886253. [DOI] [PubMed] [Google Scholar]
- 30.Sterchi SL. Perceptions that affect physician-nurse collaboration in the preoperative setting. AORN J. 2007;86(1):45–57. doi: 10.1016/j.aorn.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 31.Jones TS, Fitzpatrick JJ. CRNA-physician collaboration in anesthesia. AANA J. 2009;77(6):431–436. [PubMed] [Google Scholar]
- 32.Taylor CL. Attitudes toward physician-nurse collaboration in anesthesia. AANA J. 2009;77(5):343–348. [PubMed] [Google Scholar]
- 33.Hansson A, Arvemo T, Marklund B, Gedda B, Mattsson B. Working together- primary care doctors’ and nurses’ attitudes to collaboration. Scand J Public Health. 2010;38(1):78–85. doi: 10.1177/1403494809347405. [DOI] [PubMed] [Google Scholar]
- 34.Curran VR, Sharpe D, Forristall J, Flynn K. Attitudes of health sciences students toward interprofessional teamwork and education. Learn Health Soc Care. 2008;7(3):146–156. [Google Scholar]
- 35.Ardahan M, Akcasu B, Engin E. Professional collaboration in students of medicine faculty and school of nursing. Nurse Educ Today. 2010;30(4):350–3554. doi: 10.1016/j.nedt.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 36.Zillich AJ, McDonough RP, Carter BL, Doucette WR. Influential characteristics of physician/pharmacist collaborative relationships. Ann Pharmacother. 2004;38(5):764–770. doi: 10.1345/aph.1D419. [DOI] [PubMed] [Google Scholar]