Abstract
Objective. To implement an active-learning approach in a pharmacotherapy course sequence in the second year (P2) and third (P3) year of a doctor of pharmacy (PharmD) program and determine whether the pedagogical changes correlated with retention of core content in the fourth year (P4).
Design. Class sessions were transitioned from slides-based lectures to discussion-based active-learning pedagogy.
Assessment. A comprehensive examination was created and administered to assess student retention of therapeutic topics taught. Students demonstrated significantly improved overall scores on questions derived from the active-learning pedagogy used in Pharmacotherapy II and III compared to those derived from Pharmacotherapy I in which content was delivered by lecture.
Conclusion. The use of active-learning strategies over lecture-based methods in pharmacotherapy courses resulted in higher retention of core content. Students’ performance in areas taught using the discussion-based methodology was superior to that which was taught using lecture-based slide presentations.
Keywords: pedagogy, active learning, assessment, advanced pharmacy practice experience, pharmacotherapy
INTRODUCTION
The combination of the changing face of pharmacy education and the influx of new pharmacy programs demands curriculum innovations to assure the profession’s future competency, resulting in the increase of active-learning pedagogies.1-4 Due to the quantity of interpretations in the literature, choosing the most applicable active-learning strategy for student engagement proves cumbersome. The implementation of active-learning strategies may be facilitated with the application of core concepts. Among these, defining the requirements for student participation in meaningful activities, engaging students in the learning process, and evaluating their participation have utmost significance. This contrasts a traditional lecture style of unilateral learning (eg, students passively receive information from faculty).5,6
Literature supports the use of active-learning pedagogies in pharmacy education. Hogan and Lundquist surveyed graduating pharmacy students to evaluate their perceptions of preparedness for advanced pharmacy practice experiences (APPEs) and the effectiveness of problem-based learning in their preparation. Students found the use of problem-based learning to be an appropriate tool in preparing themselves to perform above average during APPEs.7 Dolder and colleagues measured the effect over time of a 2-year, problem-based learning sequence on the skills, knowledge, and abilities it was designed to enhance and develop. Students worked in groups to complete 4 problem-based learning (PBL) cases each semester. Case solutions were documented through the use of standardized answer sheets comprising 6 questions that addressed the course learning objectives (hypotheses, learning issues to investigate, how hypotheses ruled in or out, primary problem identification, plan, and goals). Students received a total score and 3 predetermined sub-item scores (ie, bioinformatics, knowledge and reasoning, and application). Total and sub-item scores significantly improved for each semester compared with baseline; however, a performance ceiling was observed among semesters 2, 3, and 4. The improvements demonstrated in all measured areas of performance were consistent with the ability of PBL to affect a variety of academic achievement areas.8
The American Association of Colleges of Pharmacy Curricular Change Summit Supplement addressing competencies for the future in the professional curriculum encouraged faculty members to “extensively implement active-learning strategies that will improve retention of knowledge, thinking abilities, and problem-solving, and foster development of professional traits.”3 Recommendations from this study, as well as an additional summit supplement addressing roles of innovation in education delivery, are consistent with the 2004 revisions of the Center for the Advancement of Pharmaceutical Education guidelines in addressing pharmacy practice competencies and are supportive of the need for interactive curricula with less focus on information storage and retrieval.2,3,9,10 The Accreditation Council for Pharmacy Education standards stipulate that active-learning strategies be used throughout curricula to foster student learning and achievement of outcomes.11
Traditional lecture styles facilitate rote memorization and result in students forgetting information following an examination. Student attention and retention have been shown to be affected during a traditional 60-minute lecture. Student attention span is approximately 15 minutes with lecture-based pedagogy.5,12 Substantial decline in student retention of information presented after the first 10 minutes of lecture has also been documented. This decline continues throughout the 60-minute period with the lowest percentage of information retained being presented during the last 10 minutes.13 Active learning requires students’ participation in the classroom and helps them to become more responsible for their own learning. Evidence supports the use of active learning to stimulate higher-order thinking and improve student motivation to learn.5 Ruhl and colleagues evaluated short- and long-term retention following the implementation of 1 active-learning strategy (the pause procedure) in a study involving 72 undergraduate students. The strategy involved interrupting a 45-minute lecture with 2-minute breaks during which students worked in pairs to clarify their notes. Short-term retention was assessed by a free-recall exercise and long-term retention by a multiple-choice examination given 1.5 weeks after the last of 5 lectures used in the study. Results were compared with a control group who experienced the traditional lecture format. Short-term and long-term retention of lecture material were higher in the group using the active-learning approach.14
In 2008, Kelley and colleagues designed an interactive competency-based assessment that P4 students at The Ohio State University underwent prior to APPEs. The examination was case-based, covering 9 major health/medical topics and the top 200 prescribed medications of 2006. This assessment evaluated student confidence preexamination and postexamination.15 In 2010, Alston and colleagues created an Annual Skills Mastery Assessment (ASMA) at Wingate University used to test abilities at the end of each academic year. Each ASMA was multiple choice and faculty development included training on writing higher-order items based on Bloom’s Taxonomy. Care was given to diversify content to cover a broad range of disease states relevant to the student year (P1, P2, P3, P4). Each ASMA was considered high stakes but had no sole bearing on student progress; however, concerns raised were followed by appropriate remediation.16
This study was conducted at the University of Charleston School of Pharmacy. It describes an assessment tool built with varying levels of Bloom’s Taxonomy to evaluate student retention of concepts taught using active-learning strategies vs those taught using traditional pedagogy.17 Studies evaluating the effect of active learning on longitudinal knowledge retention assessed through examination are lacking in the pharmacy literature. The objective of this study was to determine if a systematic change in teaching methodology from a lecture-based to an active-learning, student-centered pedagogy between P2 and P3 correlated with increased retention of core pharmacotherapy content in P4 students. We detail the design, development, implementation, and assessment of a novel approach to integrating active-learning strategies into an advanced therapeutics course and the impact on student retention of core concepts.
DESIGN
Students in the class of 2012 were given a comprehensive examination during their fourth year to determine retention of pharmacotherapy concepts. This comprehensive examination was not a routine assessment in the school’s pharmacy curriculum and was used only in this class of students who had experienced 2 different teaching pedagogies during their second- and third-year pharmacotherapy courses. This assessment was administered to measure the effectiveness of the school’s new active-learning pedagogy vs the traditional pedagogy being used. The new active-learning strategies implemented during P3 pharmacotherapy courses were intended to improve students’ ability to recall and apply material in the fourth year; thus, the examination focused on retention as a marker of success.
Key learning objectives for the pharmacotherapy course sequence were for students, upon completion, to be able to: describe the incidence, clinical presentation, and diagnostic process of selected disease states; use pertinent diagnostic and laboratory tests for directing drug therapy; apply sociologic and economic considerations when determining a drug therapy plan; use interdisciplinary skills that direct appropriate selection of nonpharmacologic and pharmacologic therapies; understand mechanisms and proper usage of prescription and nonprescription medications; develop strategies to increase patient understanding, motivation, and adherence to treatment plans; identify and prevent drug-related problems; effectively monitor, assess, and optimize therapeutic plans; and apply current practice guidelines to therapeutic recommendations.
The fourth-year students (N=70) had been exposed to the traditional teaching methodology in their Pharmacotherapy I course. They experienced the change in pedagogy starting with their Pharmacotherapy II course and carrying through Pharmacotherapy III. Content within each pharmacotherapy course was unique. The first sequence included cardiovascular, renal, immunologic, and bone and joint disorders. The second sequence covered respiratory, gastrointestinal, neurologic, endocrine, and psychiatric disorders. The last sequence covered infectious disease, oncology, special populations, and nonprescription medication topics. Content in the pharmacotherapy sequence did not change with implementation of the new pedagogy. Pharmacotherapy I content was delivered using traditional lectures with slide presentations involving little dialogue with students. This was the method in which all previous students had been taught pharmacotherapy at the school. Students did not engage in the material prior to class. Instead, instructors taught the information in class via lectures, leaving students with little time for application of the material. Students demonstrated that they could memorize the slide content and perform well on examinations, but during the following year in the experiential education setting, they had difficulty recalling and applying information from the previous pharmacotherapy courses. Feedback and evaluations requested from our experiential department confirmed the student’s challenges with application of knowledge.
During fall semester 2010, faculty members began implementation of the reconstructed pharmacotherapy course sequence starting with Pharmacotherapy II as it is delivered in the fall, whereas Pharmacotherapy I and III are delivered in the spring. This teaching method was different from the slides-based lectures previously used in the Class of 2012 first Pharmacotherapy course. Therefore, the class of 2012 had already completed Pharmacotherapy I, taught using the traditional pedagogy, before the changes to the course sequence began. Experiencing this transition from the traditional pedagogy to the active-learning pedagogy is what made this class of students the best subjects for this study.
As part of the course reconstruction, the course coordinators created an instructor guide, the contents of which were agreed upon by all faculty members teaching in the course sequence. Faculty members used the instructor guide to help facilitate consistency in mechanisms of content delivery and student expectations during class sessions. Students were assigned preparatory readings and given individual readiness assessment tests (IRATs) prior to the lecture. Although faculty members agreed upon using IRATs as an effective tool to assess student readiness for class, they required excessive faculty time to conduct and grade, and added an administrative burden to these team-taught courses. Thus, the IRATs were abandoned shortly after implementing the new pedagogy.
Once class sessions began, instructors used a randomized list to call on students to participate in class discussion. Students were required to answer questions directed at them to demonstrate their ability to apply the material they had studied. Instructors designed questions to cover key concepts to meet ability-based outcomes for each class session. They had the flexibility to administer questions creatively using their choice of in-class activities (eg, games, puzzles, patient cases; not slides or lectures) to help students demonstrate their ability to apply material in the class setting. Students earned class-participation points for correctly answering questions when called upon during class. Students were given 8 chances to earn these participation points through instructor-facilitated questioning in class. Each student was called upon for points for this purpose 8 times throughout the semester. Additional comments and questions were encouraged; however, only those directed by the instructor resulted in points earned. Class-participation points comprised approximately 20% of the course grade, while team cases and online secure examinations accounted for the remaining 80% of the grade in the P3 pharmacotherapy courses. The University of Charleston’s Institutional Review Board approved this study. Statistical evaluation was completed using SPSS Version 16.0 (SPSS Inc, Chicago, IL). Groups were compared using the student t test.
EVALUATION AND ASSESSMENT
Course coordinators created a 100-item comprehensive examination, with 30 questions on the content of each of the 3 pharmacotherapy courses. (Responses to the 10 additional questions included in the examination are not reported here as they had no relevance to this study.) The pharmacotherapy course coordinators reviewed previous examination material from their courses and selected the 30 questions based on levels in Bloom’s Taxonomy and acceptable item statistics for each question.6 Each coordinator selected 10 questions from Bloom’s Taxonomy level of knowledge, comprehension, and application, respectively. This was done to maintain consistency in the difficulty level of questions for each of the 3 courses.
In December 2011 (after completion of 5 of their 8 required APPEs), 70 students completed the comprehensive examination. Examsoft (ExamSoft Worldwide, Inc, Dallas, TX) was used to administer the secure examination and students were given 2 hours to complete it. Although there were no outlined consequences if a student did not take the examination, all students in the class completed it. SPSS Version 16.0 (SPSS Inc, Chicago, IL) was used to analyze results for significance.
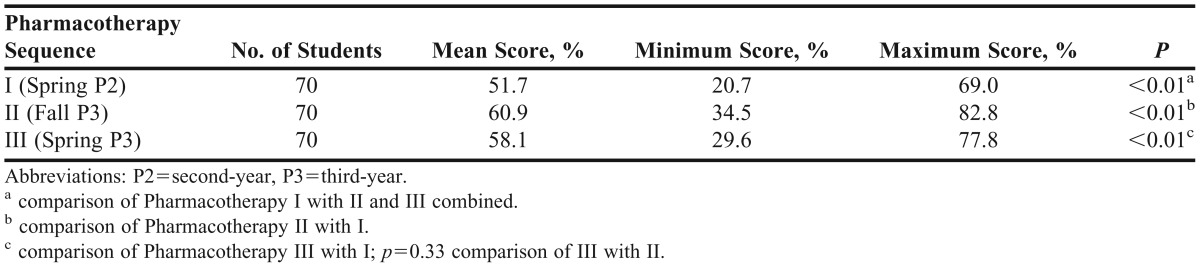
Students demonstrated significantly better overall mean scores on questions derived from the active-learning pedagogy used in Pharmacotherapy II and III than on those derived from Pharmacotherapy I in which content was delivered by lecture (p<0.01 for Pharmacotherapy I vs III, p<0.01 for Pharmacotherapy I vs II). There was no significant difference in overall student performance on questions derived from courses using the new pedagogy (p=0.33 for Pharmacotherapy II vs III) (Table 1).
Table 1.
Class of 2012 Assessment Scores Based on Content Year for Active-Learning Format Versus Lecture-based Format
The 11 faculty members involved in team-teaching Pharmacotherapy II in 2010 were surveyed at the beginning and end of the semester to determine faculty attitudes toward teaching using active-learning methods. The pre-semester survey resulted in a 100% response rate while the followup survey achieved a 45% response rate. Prior to using the new pedagogy, respondents anticipated that more time would be required to prepare for each active-learning class session but that students would be more engaged with the material and would learn more applicable content. One hundred percent of faculty members responding to the survey agreed that student outcomes would improve with implementation of the new pedagogy. Comments reflected some hesitation regarding changes but willingness to attempt new methods to potentially increase student learning. Responses to the followup survey reflected that initial thoughts of the instructors did not change. They reported a perceived slight increase in time spent preparing for classes using the new teaching method. However, they were pleased with the level of student engagement and apparent learning of applicable content. Incorporating active-learning strategies into a large class setting proved feasible and acceptable among faculty members who undertook this change. This pedagogy change and subsequent assessment did not require additional resources (financial or personnel). Faculty members have adopted this new pedagogy in subsequent annual offerings of this pharmacotherapy sequence. Other faculty members have implemented aspects of this pedagogy throughout the curriculum.
Initial student perspectives were mixed. Based upon course evaluations, students reported that they did retain material better and felt more comfortable with the content taught using the active-learning pedagogy. Complaints included a hesitancy to assume responsibility for completion of reading assignments (sometimes reading assignments were perceived as voluminous), requests to use slides again (overall resistance to change), and difficulty re-organizing personal time management to facilitate adequate pre-class preparation (while balancing other course workload). As students matured throughout their final year, they reported a greater appreciation for the new pedagogy. Exit interview data (collected annually from graduates of the University of Charleston School of Pharmacy’s program) reflected a gratitude for having experienced the change in teaching methods. As assessed in focus groups of this class, many graduates reported having a greater sense of responsibility and capability for self-learning.
DISCUSSION
Transitioning third-year pharmacotherapy courses from a traditional lecture-style andragogy to an active-learning andragogy style resulted in pharmacy students retaining course material/content better in their P4 year. Active-learning strategies are an important element when promoting critical-thinking and problem-solving skills.11,18 Active learning allows students to become more involved in the classroom setting with a better understanding of the key concepts and improved content retention.
Our efforts were put toward a class of 70 students. A randomized listing of the students was used by each faculty member to determine which students were to be called on during each class session. This list helped to assess student preparedness and ensure the inclusion of each student equally throughout the semester. Although the faculty members saw an improvement in student confidence and willingness to participate during each semester, the amount of content discussion among the students could have been increased. However, the balance between delivery and discussion of new content was difficult to achieve. Faculty members stressed the importance of students preparing for class, asking questions about difficult content, and participating in the discussion during class, thereby placing responsibility for learning on the student.
Initial barriers for faculty members included creation of new lecture material in order to incorporate student-directed reading assignments and student-centered in-class activities. Many of our faculty members had been teaching certain topics for quite some time, so the change in lecture material and presentation style added an increased workload compared to that which was planned in advance. Newer faculty members had less of a barrier as they were expected to begin working on lecture materials and it was already assumed they would need more time for preparation. For students, 1 initial barrier was thought to be the increased amount of required reading in order to adequately prepare for each class session. Many students voiced concerns of “teaching themselves” vs having an improved learning environment. However, once examination time came, students seemed more prepared. Some stated they spent less time cramming for the examination and more time reviewing what they had already read, prepared for, and discussed. The students expressed the change in format as a major strength. Verbal and informal student feedback throughout each semester allowed faculty members to stay motivated to teach in a different style in order to provide students with a better outcome (ie, a greater retention of knowledge).
Because questions remained among faculty members as to the value of active learning in terms of student retention of material, the assessment tool described in the Evaluation and Assessment section was constructed and administered to students who had experienced both pedagogical strategies throughout the pharmacotherapy course sequence. Because the examination revealed positive results in the way of increased knowledge retained, we hope that the curriculum committee at the University of Charleston will continue to consider implementing active-learning methods beyond the pharmacotherapy sequence. Based on verbal feedback from students, students would also advocate the active-learning model as they commented on their success in ability to not only learn the material for the first time, but also to have a deeper understanding of the material. In addition, active learning should be viewed as a positive change in classrooms and curriculum nationwide. Faculty members may choose from multiple active-learning styles to engage their students, so implementing such changes in instructional method can be done with minimal effort and resources.
In creating the comprehensive assessment, old examination questions from Pharmacotherapy I, II, and III were reviewed and included in the content to ensure the major concepts from each course were covered adequately. Other than minor changes made to some questions to correct statistics, grammar, or typographical errors, essentially the same set of examination questions that had been given to this group of students when they completed the courses the previous year were included in the comprehensive assessment, leaving no way to rule out recall of the test questions as the reason for their higher scores rather than knowledge retention of course content. When looking at the time between the pharmacotherapy sequence and the examination, recall was most possible for the latest content delivered and tested (ie, Pharmacotherapy III).
Because of delays in obtaining the archived questions from the Pharmacotherapy I examination, the comprehensive assessment was administered more than halfway through the experiential year. Thus, some students may have completed more difficult practice experiences prior to the assessment compared to other students and because of the knowledge gained during these APPEs, they may have performed better on the comprehensive assessment. Another limitation related to the delay in administering the assessment was that some students may have been studying for the North American Pharmacist Licensure Examination (NAPLEX) and could have skewed the results in favor of a larger amount of knowledge retained.
Although not technically part of the evaluation of our study, investigators were interested in evaluating the NAPLEX score results for this cohort of students. There was a 7.5% increase in first time pass rate of the NAPLEX among those graduates who had experienced the change in pedagogy when compared to the average of all previous graduates from this program. While these results may have been influenced by other factors, it is worthy of mention and further evaluation.
SUMMARY
A change in pedagogy from a lecture-based format to an active-learning format initiated during the second course of a 3-course pharmacotherapy series resulted in improved student retention of course content. By developing and administering a comprehensive assessment, we quantified students’ gain in knowledge retention when comparing active-learning strategies to the traditional lecture format. Student evaluations and preceptor surveys point to our graduates having a greater sense of responsibility, and better retention of information and capacity for self-learning, because of incorporating the active-learning pedagogy.
ACKNOWLEDGMENTS
The authors thank their colleagues for contributing information and assistance in assessing this pedagogical change. Dr. Sandra Bowles was instrumental in quality assurance measures, such as student focus groups. Dr. Bowles and Dr. Travis White collaborated with us on the survey of faculty attitudes toward teaching. Dr. David Latif provided statistical support.
REFERENCES
- 1.Knapp DA, Knapp DE. Attributes of colleges and schools of pharmacy in the United States. Am J Pharm Educ. 2009;73(5):Article 96. doi: 10.5688/aj730596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blouin R, Riffee W, Robinson E, et al. AACP curricular change summit supplement: roles of innovation in education delivery. Am J Pharm Educ. 2009;73(8):Article 154. doi: 10.5688/aj7308154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jungnickel RP, Kelley KW, Hammer DP, Haines ST, Marlowe KF. AACP curricular change summit supplement: addressing competencies for the future in the professional curriculum. Am J Pharm Educ. 2009;73(8):Article 156. doi: 10.5688/aj7308156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steward DW, Brown SD, Clavier CW, Wyatt J. Active learning processes used in US pharmacy education. Am J Pharm Educ. 2011;75(4):Article 68. doi: 10.5688/ajpe75468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prince M. Does active learning work? A review of the research. J Eng Educ. 2004;93(3):223–231. [Google Scholar]
- 6.Bonwell CC, Eison JA. Washington DC. George Washington University; 1991. Active learning: creating excitement in the classroom. ASHEERIC Higher Education Report No. 1. http://www.eric.ed.gov/PDFS/ED340272.pdf. Accessed April 11, 2013. [Google Scholar]
- 7.Hogan S, Lundquist LM. The impact of problem-based learning on students’ perceptions of preparedness for advanced pharmacy practice experiences. Am J Pharm Educ. 2006;70(4):Article 82. doi: 10.5688/aj700482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dolder CR, Olin JL, Alston GL. Prospective measurement of a problem-based learning course sequence. Am J Pharm Educ. 2012;76(9):Article 179. doi: 10.5688/ajpe769179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Association of Colleges of Pharmacy. Educational Outcomes 2004. Alexandria VA: Center for the Advancement of Pharmaceutical Education Outcomes. 2004 http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed September 10, 2013. [Google Scholar]
- 10.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education, Pharmacy Practice Educational Outcomes and Objectives Supplements Task Forces. Pharmacy practice supplemental education outcomes based on CAPE. 2004 http://www.aacp.org/resources/education/Documents/PharmacyPracticeDEC006.pdf . Accessed February 1, 2013. [Google Scholar]
- 11.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree, guidelines version 2.0. Adopted. January 23, 2011 http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed February 1, 2013. [Google Scholar]
- 12.Wankat P. The effective efficient professor. Boston, MA: Allyn and Bacon; 2002. teaching, scholarship, and service. [Google Scholar]
- 13.Hartley J, Davies I. Note taking: a critical review. Program Learn Educ Technol. 1978;15(3):207–224. [Google Scholar]
- 14.Ruhl K, Hughes, Schloss P. Using the pause procedure to enhance lecture recall. Teach Educ Spec Educ. 1987;10(1):14–18. [Google Scholar]
- 15.Kelley KA, Demb A. A progress assessment to evaluate pharmacy students’ knowledge prior to beginning advanced pharmacy practice experiences. Am J Pharm Educ. 2008;72(4):Article 88. doi: 10.5688/aj720488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alston GL, Love BL. Development of a reliable, valid annual skills mastery assessment examination. Am J Pharm Educ. 2010;74(5):Article 80. doi: 10.5688/aj740580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bloom BS, Englehart MD, Furst EJ, Hill WH, Krathwohl DR. Taxonomy of Education Objectives. Handbook 1: The Cognitive Domain. New York, NY: Longman; 1956. [Google Scholar]
- 18.Stanger-Hall KF, Lang S, Maas M. Facilitating learning in large lecture classes: testing the “teaching team” approach to peer learning. CBE Life Sci Educ. 2010;9(4):489–503. doi: 10.1187/cbe.09-12-0093. [DOI] [PMC free article] [PubMed] [Google Scholar]


