Abstract
Colleges and schools of pharmacy are incorporating more team-based learning (TBL) into their curriculum. Published resources are available to assist instructors with implementing TBL and describing it in the health professions literature. The 7 core elements include: team formation, readiness assurance, immediate feedback, sequencing of in-class problem solving, the 4 “S” structure for developing team application exercises (significant problem, same problem, specific answer choice, simultaneous reporting), incentive structure, and peer evaluation. This paper summarizes best practices related to implementation of TBL in pharmacy education, including courses taught using teaching teams.
Keywords: team-based learning, team formation, readiness assurance test, learning, peer evaluation, team taught course
INTRODUCTION
Team-based learning is a form of cooperative learning that creates an environment that allows learners to develop higher levels of learning (ie, application, analysis, evaluation, creativity). To accomplish these goals, the instructor must embrace the 4 essential principles of TBL: (1) properly form and maintain groups; (2) hold students accountable for individual and team work; (3) provide frequent and timely feedback; and (4) design team assignments to promote learning and team development.1 Each of these areas can offer challenges to course instructors and have resulted in variability among TBL practitioners. One particular challenge is courses that use multiple instructors.
Pharmacy education uses teaching teams so students may learn from content experts. Implementation of TBL in a team-teaching environment provides additional procedural considerations that may not occur in courses with only one instructor. Of the published reports of implementing TBL in pharmacy education, 10 of 12 (83.3%) programs had incorporated teaching teams.2-13
Following adoption of TBL in health sciences education, published reports on TBL have increased. Haidet et al published guidelines to assist instructors with implementing TBL and describing it in the literature.14 This publication also identifies 7 core elements of TBL that should be incorporated into published reports on TBL implementation to ensure appropriate comparisons among results.14 The 7 core elements include: team formation, readiness assurance, immediate feedback, sequencing of in-class problem solving, the 4 “S” structure in developing team application exercises (significant problem, same problem, specific answer choice, simultaneous reporting), incentive structure, and peer evaluation.14
The purpose of this manuscript is to summarize best practices related to implementation of TBL in pharmacy education, including courses taught using teaching teams. The report also summarizes the 7 core elements of TBL as defined by Haidet and colleagues. Special considerations for team taught courses also are discussed.
TEAM FORMATION
Once the decision to use TBL is made, the course director needs to form TBL teams. In doing so, the director should consider how teams will be selected, team size, and permanence, because each of these factors has implications for team functionality and learning outcomes. The goal is to create functional teams whose members communicate and negotiate well, make equitable contributions, and achieve the learning outcomes, rather than dysfunctional teams, which suffer from internal fighting, nonparticipation, and/or a “divide and conquer” approach that negates peer learning.15 The course director should select the teams (rather than allowing students to select their teams) because it can be done in advance, which facilitates material preparation. When selecting the teams, the instructor should seek faculty and staff input to identify undesirable student groupings such as couples, clicks, or social organization affiliations.
When selecting the students, the instructor should create heterogeneous teams (vs homogeneous) to expose students to peers who have different backgrounds and experiences, thereby preparing them for future interprofessional practice. The simplest heterogeneous selection option is random assignment, which can be achieved by grouping students alphabetically, using a table of random digits, drawing names out of a hat, or having students count off by a number. Random assignment is easy and fast, but the disadvantage is that it is difficult to control for clicks, or organization affiliations. Course directors wanting more control over team selection could use ability grouping based on students’ grade point average, course grades, class rank, pharmacy experience, and/or acceptance into honor societies such as Rho Chi or Phi Lambda Sigma. Results of course knowledge or skill-assessments, or personality or learning style inventory results, such as the Myers Briggs Type Indicator (MBTI), the Keirsey Temperament Sorter (KTS-II), the Strengths Finder, the Pharmacists’ Inventory of Learning Styles (PILS), the Kolb Learning Style Inventory, or the Visual, Aural, Read/Write, Kinesthetic Questionnaire (VARK), could also be used.16-18 Using personality or learning style inventories when constructing teams can help instructors emphasize team and leadership dynamics. However, selecting the tool can be challenging as they can be costly, have a time-consuming process for administration and/or scoring, or require special training. Overall, random assignment is the least time consuming and may yield similar learning outcomes to teams formed using ability grouping.
A team size of 4 to 7 students is recommended to promote greater student participation in the activity and learning.19 Studies on team size have found that students have the most positive experiences and perform the best in teams of this size.20 While larger teams may offer more diversity, they may also encourage more social loafing. Because TBL activities require team consensus, odd-numbered teams may best facilitate decision-making when the team is split on the decision. One caution is in large classes such as a class of 150 students, teams of 4 to 5 students can result in 30 to 40 teams, which may be difficult to supervise alone. Teams of 5 to 7 students result in 20 to 30 teams. In addition, class time and classroom structure (eg, seating arrangements) may not accommodate large numbers of teams.
Team permanence is the third consideration when forming teams. Research on team development suggests that teams should work together for at least 40 hours in order to move through the Tuckman stages of team formation (forming, storming, norming, and performing).1,21 Achieving 40 hours of teamwork would require that most TBL teams remain together for the entire course and possibly the entire year to promote optimal team performance. More frequent team member changes would cause the team to restart the team formation cycle each time. Directors of courses that are taught simultaneously and both use TBL (regardless of learning method used or assignments given for the teams to complete) should consider using the same teams.
Course directors should discuss their plans for student teamwork with all of the course instructors to establish support for the team formation process. The course director and instructors can work together to construct the teams and the same teams should be used throughout the course, semester, or year to promote team formation, productivity, and peer learning.
READINESS ASSURANCE PROCESS
Course design and planning should start with the end in mind, ie, what should students have learned after the completion of the course or session? This approach, sometimes called “backward design,” should be used when developing TBL materials, including the Readiness Assurance Process.22-25 Team-based learning naturally facilitates integrated course design as the learning goals, learning experiences, and feedback and assessment support each other. Once the content expert has determined the final learning outcomes, he/she should design a team application exercise that will help learners achieve those outcomes through practice, feedback, and assessment. The team application exercise determines the content of the readiness assurance test (RAT). The RAT should be designed to ensure that the learners are prepared to apply the content to solve meaningful problems in the team assignment.25
Although it should require a relatively small segment of class time, the readiness assurance process is an important component of a TBL session. It connects the learner’s pre-class preparation to the team assignment/application. The readiness assurance process also provides the opportunity for peer teaching and immediate feedback to individual students and the team. The process allows the learner and instructor to identify and immediately address gaps or misconceptions.
Parmalee and Michaelsen24 describe 5 key outcomes of the readiness assurance process: (1) effective and efficient content coverage; (2) development of teams and teamwork skills; (3) student learning value of considering input from diverse sources; (4) development of self-study and life-long learning skills; and (5) optimal use of class time. The readiness assurance process should take place in the classroom, not prior to the class session. This ensures that peer teaching takes place instead of students dividing the questions to answer individually.
Within the TBL literature, the usual number of multiple-choice questions for the RAT is 10 to 20.25 Published reports of TBL in pharmacy education include a range of 5 to 15 multiple-choice questions per RAT.2,4,5,7,9,12 The number of questions depends on the allocated class time, course content, and number of topics per TBL session. Regardless of these situational factors, the RAT and pre-class preparation should be driven by learning objectives. The duration of time allotted for the RAT will then depend on the number of questions included. The course instructor should allow 1 minute for each question on the RAT.
The course director should develop learning objectives to guide students’ pre-class preparation, which may include a reading assignment, class notes, pre-session lectures, or primary literature. The objectives and RAT questions should assess the learner’s understanding of important key points, not minor details.24,25 The RAT questions should be written at lower levels of Bloom’s Taxonomy (ie, remember, understand, apply). The learners will work through the relevant details and higher levels of Bloom’s Taxonomy (ie, analyze, evaluate, create) later in well-designed team application exercises. One of the challenges to instructors is the ability to identify the major concepts that will allow students to understand and engage in the team application exercises.
Depending on the size of the class and other logistical concerns, individual and team RAT answers may be submitted via scantrons, individual or team answer sheets, an audience response system,25-27 or Immediate Feedback Assessment Teaching (IF-AT) forms. The IF-AT forms (Epstein Educational Enterprises, Cincinnati, OH) are an effective way to engage students in the team RAT process. These forms are multiple-choice (4 to 5 answer choices) and give the student immediate feedback on their answer. It also allows for partial credit to be earned as the team continues to work toward the correct answer.25,28-29 Partial credit can be awarded based on the number of attempts teams used to answer the question. The number of attempts teams needed to answer the question correctly can be determined by the number of answer choices that were “scratched” to reveal the correct answer, which is marked with a star.30 For courses not able to use the IF-AT forms, partial credit could be awarded by allowing teams to distribute points to each answer choice they are considering. For example, if there are 4 answer choices, the question would be worth 4 points. The team could distribute points to 1, 2, 3, or 4 answer choices. Teams who are confident about their answer choice will place all of the points on 1 answer choice. Teams who are debating between 2 answer choices may evenly distribute points between 2 answer choices. Teams who cannot narrow down the answer choices may place 1 point on each answer choice.
Students should complete the RAT individually and as a team. After the team RAT, the instructor should facilitate a brief review of the RAT. This discussion allows the instructor to address any misconceptions, answer student questions, and provide immediate, corrective feedback. Instructors may determine what RAT questions to review based on individual or team responses, or conversations they hear during the team RAT discussions. Because peer teaching has likely occurred, these discussions do not necessarily need to review each question.25
Ideally, teams should have the opportunity to appeal a RAT question.1 This appeals process provides students with a sense of fairness (ie, opportunity to earn credit for incorrectly answered questions, and the opportunity for focused restudy and animated discussion). It also encourages a high level of student engagement, and helps the instructor to revise questions for future course offerings.1,24 Teams should be encouraged to re-write a question if it is misleading, or to justify, verbally or in writing, why the answer they selected is correct.1,25 The verbal or written justification should be based on either the tertiary or primary literature. Only the team that appeals should earn credit for their answer, and it should be given for both their team and individual grades.24 The appeal process motivates all learners to critically evaluate their performance and the quiz as they seek to develop and communicate evidence-based appeals.
Appeals may be conducted in class or after class, with both approaches having pros and cons. The immediacy and energy of an appeal in class promotes learning and team engagement, but it uses class time and does not engage teams who are not participating in the appeal. Appeals that are submitted out of class require teams to meet outside of their regular class time, but allows them more time to carefully think through their appeal.25
When multiple instructors participate in the same course, each one must/should follow the same procedure for conducting readiness assurance tests. The course director should communicate the procedure with all instructors prior to their first in-class TBL session, and provide them with a quick reference guide outlining procedures. We also recommend that instructors who do not have experience leading a TBL session observe a colleague prior to their sessions to have a better understanding of timing and classroom procedures. When consistent procedures are followed, students become accustomed to the process, which lowers the administrative burden for less familiar instructors.
DEVELOPING TEAM APPLICATION EXERCISES
The in-class team application exercises are intended to build on the basic level of understanding gained through the readiness assurance process and provide opportunities for higher-order thinking and the development of noncognitive skills such as teamwork and communication. The creation of these application exercises thus becomes a critical part of the TBL process.
Developing team application exercises (ie, in-class cases) that foster interaction and promote learning are both essential and challenging.24,31 These team application exercises are based on the 4 S’s, significant, same, specific, and simultaneous. Some of the variability among TBL practitioners relates to their interpretation/application of the 4 S’s as well as to whether team application exercises will contribute to the course grade.
The first of the 4 S’s is significant – the problems that students solve should be significant, that is, could students see themselves being challenged with this problem as a pharmacist? The best cases typically are practice-based and focused on major, overarching concepts. Focusing on smaller details risks leaving gaps in student learning and may not address key learning objectives. However, these finer details can be addressed as “pearls” during the course of the discussion. Because the learning objectives are focused on higher-order learning, the cases should allow learners to justify their answers. The ability to justify answers helps promote critical-thinking and meta-cognition, skills essential to higher levels of learning32 and are further promoted if they are more integrated either between courses (eg, foundational and clinical science)4,13 or within a course (eg, inclusion of prior material).33 Given that team application exercises need be significant, focused on major learning objectives, and potentially integrative, it is highly recommended that cases be peer-reviewed. This review ensures all the appropriate information is included; the cases address key learning points; and the answer choices are reasonable along a continuum of possibilities.
Specific choices and the simultaneous reporting of these choices are the other important elements for developing team application exercises. A key choice instructors have to make is whether the case should be multiple-choice format or open-ended (eg, SOAP [subjective, objective, assessment, plan] note, progress note, case report forms, presentations).13,34 Within the original construct of TBL, multiple-choice team application exercises are the preference because they require a specific choice, allowing easier simultaneous reporting among the teams. This simultaneous reporting can be accomplished by having students hold up letters corresponding to the teams’ answer choice or using audience response systems.8,27,35 The alternative to the multiple-choice question is open-ended team application exercises. The advantage with this format is that it presents a more realistic clinical application. The disadvantage of this format is the challenge of simultaneous reporting. Some practitioners have accomplished simultaneous reporting in smaller classes by using technology or large Post-it notes and a “gallery walk” where students can view the others teams’ work.1,13 Both multiple-choice and open-ended format share a common disadvantage of being difficult to write, especially at higher levels of learning where students are expected to apply, analyze, synthesize, and/or evaluate information.
The final area is whether the team application exercises contribute to the course grade. Most instructors who use TBL grade team application exercises, which is consistent with the original literature on TBL.36 The grading varies from a grade on a continuous numerical scale to pass/fail to contribution to class participation. The grading may assess each team’s selection of the correct answer, and/or its justification or rationale for the answer chosen. When grading the team application exercises based on justification, a grading rubric should be developed.
Developing Team Application Exercises in Team Taught Courses
Team taught courses pose an interesting dilemma when developing team application exercises. Course directors should develop in-class procedures for the total amount of time teams are given to answer the questions for each case/scenario and for the total amount of time that is provided for simultaneous reporting and inter-team discussion. Some instructors may prefer teams to complete all cases and questions prior to simultaneous reporting and inter-team discussion, while others may prefer teams to work on 1 case at a time. To maintain consistency in the course, the course director should determine the process to be used in advance and communicate that with all course instructors. Similarly, with the RAT in-class procedures, the course director should provide this process in writing to course instructors.
Having multiple instructors in the same course also is ideal for incorporating content from multiple areas, such as merging basic science with clinical sciences, or presenting students with patients who have multiple problems of various origins. Although multiple instructors may develop a case, all content experts may not need to be present for the in-class TBL session.
FACILITATION SKILLS
The instructor’s ability to properly facilitate team learning in small or large classroom settings is essential to the overall success of the TBL session. One of the key things that sets TBL apart from other active-learning strategies is that 1 course instructor can facilitate a session, regardless of class size.2,14 The instructor will have multiple responsibilities throughout the session to ensure the learning process is occurring through intra- and inter-team discussion. The most important skill for the facilitator is the ability to encourage teams to verbalize their rationales during large group discussions to achieve the predetermined learning objectives.1 The facilitator’s role is to serve as the content expert for the focused discussions that will follow the RAT and team application exercises and also to provide a framework for the implementation of the session.25 The framework for implementation can be broken into 3 components: social, administrative or organizational, and intellectual or knowledge base.37 Having a solid framework will help to ensure that student engagement is properly managed. The components of the framework often overlap and each will be briefly described below.
The facilitator will need to create and maintain an open and interactive environment in which teams feel safe and comfortable interacting with one another. To accomplish this goal, the facilitator’s responsibilities include: setting the tone for the session, encouraging interactivity, inviting responses from teams, asking probing questions when necessary, and acknowledging the individual contributions made by the teams.37
The administrative or organizational role of the facilitator is to establish the rules for the session, keep discussions focused on meeting the learning objectives, monitor the discussions by walking around the room during the TBL session, and invite participation from teams who do not appear to be actively engaged in the discussion.37 Providing students with an outline of the timing of each component of TBL (individual and team RAT, team application exercises, etc) will assist in keeping the TBL session moving towards completion.
Unlike other learning strategies where facilitators provide learners with feedback and guidance regarding their reasoning but are not necessarily content experts, instructors who serve as facilitators for TBL activities are expected to be content-experts for their respective sessions, able to anticipate and address learner’s questions and misconceptions as they arise during the session.25 Using the “backward design” and starting with the end in mind, the intellectual role of the facilitator is to assist team members in achieving predetermined learning objectives.25,37 The intellectual responsibilities of the facilitator are to stimulate student thinking by phrasing appropriate questions, make connections to objectives and practical application when necessary, provide informative feedback, and summarize key points.37 Proper facilitation of the focused discussion that occurs upon spontaneous reporting following the team RAT or team application exercises requires the instructor to have a thorough understanding of the learning objectives outlined for the students.
There are 2 main points of discussion that occur in a TBL session: (1) at the conclusion of the RAT process and (2) during inter-team discussions of the team application exercises. Immediate feedback provides students the opportunity for engagement with both course content and their peers.14 The intra-team discussion benefits students who have misinterpreted course materials by helping them understand their misconceptions prior to consolidation into long term memory.1 Prior to moving on to the application exercises, the facilitator should gauge the entire classes’ understanding of the core concepts that were assessed during the readiness assurance process. The facilitator can provide additional insight on content, but only after all teams have had the opportunity to explain their thinking.
Once a conceptually based, challenging, relevant team application exercise is constructed, the time allowed to complete a case varies. The original model suggests 8 minutes for intra-team discussion followed by a brief inter-team discussion.2 The time to complete the team application exercise can be dictated by the number of questions within each case but can range from 3 to 15 minutes.8,12 Many practitioners of TBL use cases with 3 to 5 multiple-choice questions.7,12 The time for inter-team discussion can vary from 8 to 30 minutes depending on the complexity of the case, thoroughness of discussion, or allowing a “time for telling” for areas where there is a lack of knowledge.12 In one study, the time to complete a case was pared down throughout the semester to eventually reach a 5-minute time point, a time period typically encountered with patient counseling.38 Tan and colleagues used 3 minutes for groups to work on team application exercises.35 Parmelee and colleagues found students feel the time limit for team application exercises should not be longer than 2.5 hours and the instructor’s role is to keep the discussion moving along.25
Specific techniques to promote inter-team discussions are described in the literature.1 Table 1 summarizes useful facilitator techniques. Simultaneous reporting of answers provides a foundation for productive discussion because this is the first opportunity for students to see how their thinking contrasts with that of other teams.1
Table 1.
Tips for Facilitating a Discussion Using Team-Based Learning
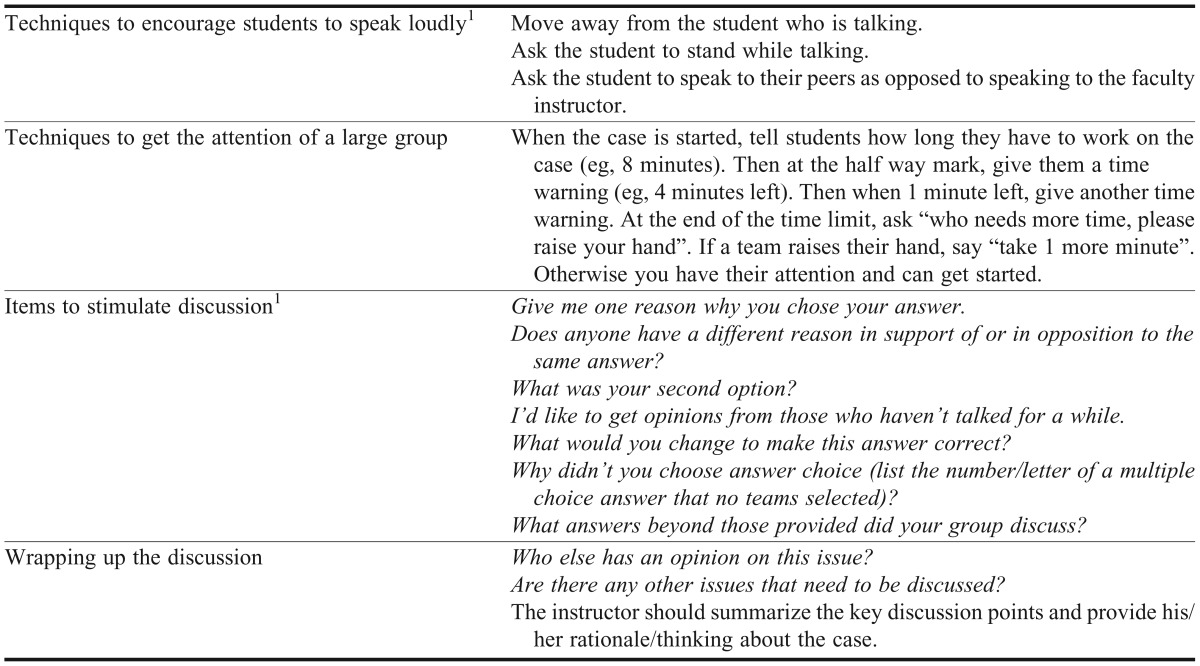
Each instructor will develop his/her own style for facilitating the TBL session. However, it is important to maintain some consistent procedures in the classroom. For example, instructors may be asked to provide a summary of all discussion points at the end of the inter-team discussion to assist students with identifying key concepts. For instructors who have not previously taught using TBL, in-class observation can assist them with identifying successful facilitation strategies.
PEER EVALUATION
Peer evaluation is an important component of TBL because it helps students to develop the team skills and attitudes they will need as future pharmacists practicing in collaborative health care environments.12 The most important consideration in incorporating a peer evaluation system is for the instructor first to decide what goals he or she hopes to achieve through peer evaluation, and then to choose or develop a peer evaluation system that achieves those goals. Depending on the system implemented, peer evaluation has the potential to provide helpful feedback to team members regarding their interpersonal and team skills, ensure individual accountability, prevent “social loafing” during team activities, and promote team effectiveness by accelerating the team’s progress through the stages of team formation. Peer evaluation also can be structured to help develop students’ skills in providing instructive feedback.1
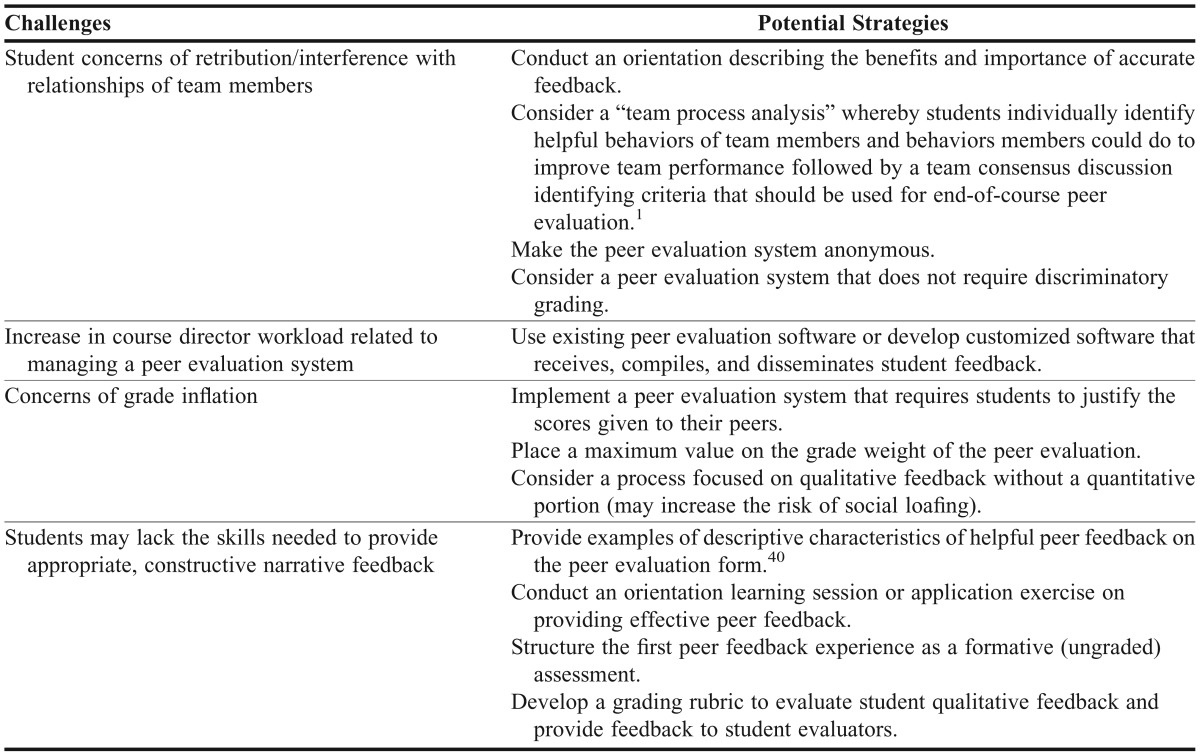
Despite the potential benefits, many educators have encountered challenges when attempting to incorporate peer evaluation into their course. Some students express dissatisfaction with peer evaluation systems and believe it interferes with their relationships with fellow learners.1,31 Students may fear retribution from classmates or be reluctant to give teammates a “below average” grade, leading to potential inflation of peer evaluation scores. In one study, students on a clinical clerkship expressed dissatisfaction with a peer evaluation system that required discriminatory grading, citing that all team members contributed equally.39 Also, students may not have the skills to provide appropriate, constructive narrative feedback because evaluation skills are not intuitive; they must be learned. Incorporating a peer evaluation system also can add a significant workload on course directors. A substantial amount of time may be required to obtain peer feedback, evaluate it (if applicable), compile, and return the feedback to the students. Table 2 provides potential strategies for addressing some of the challenges related to peer evaluation.
Table 2.
Potential Strategies for Overcoming Challenges Related to Peer Evaluation
Several peer evaluation methods have been developed to address the achievement of goals related to peer evaluation while minimizing the challenges. Some examples of peer evaluation systems, include the Michaelsen method which forces students to discriminate among the performance of team members; the Fink method, in which students are given 100 points to divide among team members resulting in a multiplier that is used to adjust the overall course grade for a particular student; and the Koles method which incorporates both a required quantitative and qualitative section.1 Instructors will need to decide if the students will assign an overall single quantitative score to team members (eg, Michaelsen method) or provide students with specific domains for evaluation (eg, Koles method). Instructors have included a variety of assessment domains for the quantitative section, including cooperative learning skills, self-directed learning, interpersonal skills, preparation, participation, leadership, attitude, confidence, and professionalism.1,2 Some TBL educators have suggested involving students in setting the grade weight for the peer evaluation component as well as designing the peer evaluation instrument as familiarity with and ownership of assessment criteria tends to foster peer assessment validity.31,41 Regardless of the method used, in order to promote accountability, Michaelsen and Fink emphasize that the peer evaluation system must be capable of: (1) accommodating teams of different sizes; (2) accurately reflecting the work of the team members; and (3) making a significant impact on the course grade.1
Once a peer evaluation system is developed, instructors must carefully consider how often to conduct peer evaluations and what processes will be used to collect information. In deciding upon the frequency of evaluation, the actual amount of time students have spent in a team must be considered. As discussed above, teams should work together for at least 40 hours in order to begin “performing.” In addition, frequent peer evaluation may lead to “survey fatigue,” and disrupt team development by validating the role of a dominant team member early in the semester.1,31 Many published studies of TBL in pharmacy education conducted peer evaluations 1 to 2 times during the semester, 1 of which was a formative assessment.2,7,8,12 While peer evaluations can be conducted via paper responses, instructors have also used Web-based applications such as iPeer (University of British Columbia) and SparkPLUS (University of Technology Sydney) which provide a variety of capabilities such as self-evaluations and peer evaluations, custom rubric creation, and student reminders.
The peer evaluation process is typically conducted by the course director, so having multiple instructors in the same course does not typically require additional considerations. However, if peer evaluation is being used in multiple courses simultaneously, the course directors should develop a strategy for peer evaluation that can be used for all courses to avoid students developing survey fatigue and confusion over the various instruments and courses. This can be particularly helpful when the same student teams are used for multiple courses. One goal of peer evaluation is to assist students with development of teamwork skills and provide a process to allow students to reflect on their contributions to the team. Peer evaluation may not need to be conducted in every course if the same student teams are used in more than 1 course.
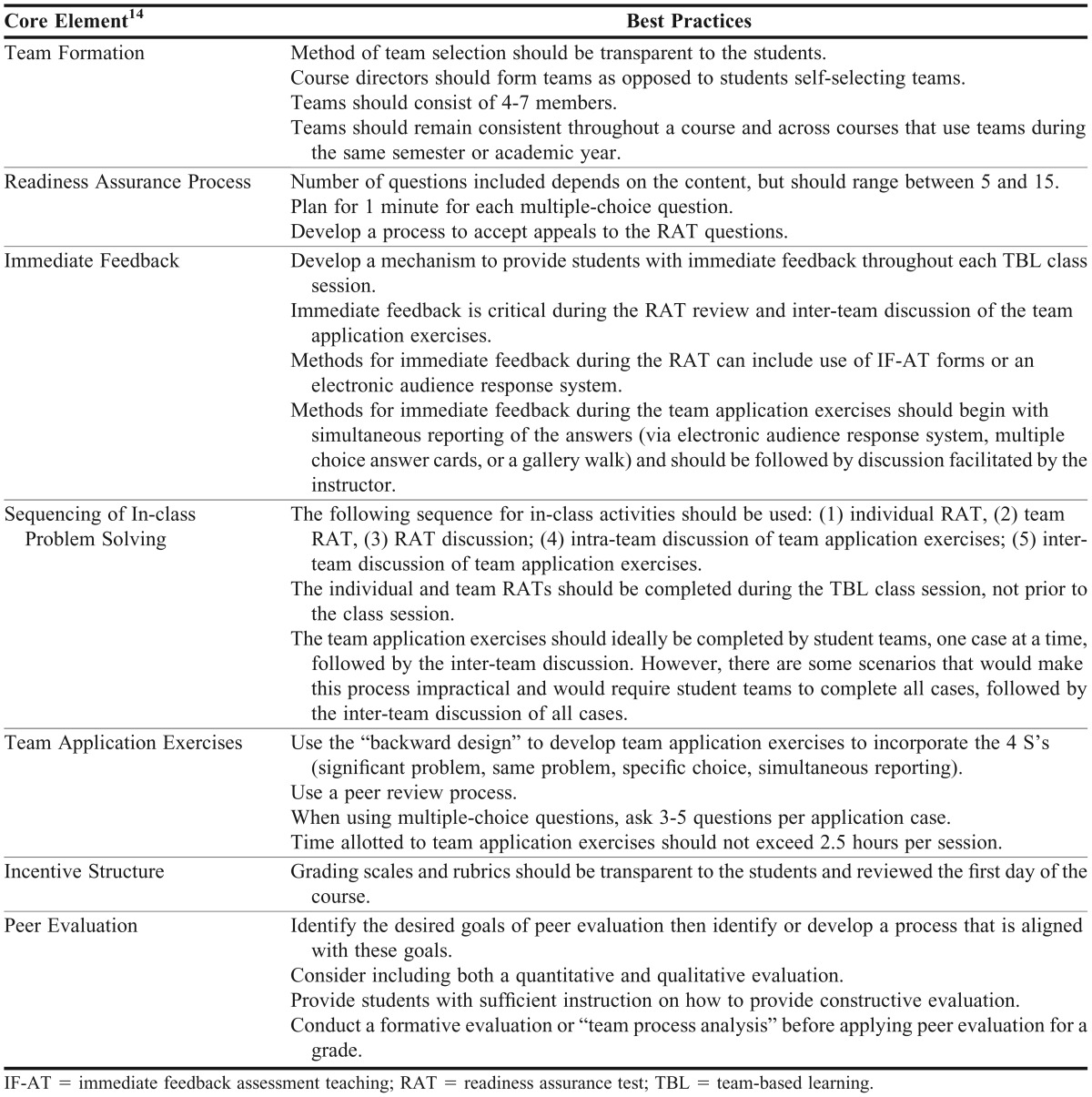
CONCLUSION
Team-based learning is growing in popularity among colleges and schools of pharmacy and variations have been reported anecdotally and within the literature. While there are opportunities to individualize the TBL process, some fundamental components should remain intact: the readiness assurance process, in-class team application exercises that allow for simultaneous reporting that emphasizes major learning objectives, and immediate feedback for content, process (eg, thinking skills), and student development (eg, working in teams). The authors discussed some additional challenges with team-taught courses such as communication, consistency, and coordination. Table 3 provides a summary of recommendations for each of the 7 core elements of TBL.
Table 3.
Summary of Team-Based Learning Best Practices
REFERENCES
- 1.Michaelsen LK, Parmelee DX, McMahon KK, Levine RE. Team-based learning for health professions education. Sterling, VA: Stylus Publishing, LLC; 2008. [Google Scholar]
- 2.Letassy NA, Fugate SE, Medina MS, Stroup JS, Britton ML. Using team-based learning in an endocrine module taught across two campuses. Am J Pharm Educ. 2008;72(5):Article 103. doi: 10.5688/aj7205103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poirier TI, Butler LM, Devraj R, Gupchup GV, Santanello C, Lynch JC. A cultural competency course for pharmacy students. Am J Pharm Educ. 2009;73(5):Article 81. doi: 10.5688/aj730581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beatty SJ, Kelley KA, Metzger AH, Bellebaum KL, McAuley JW. Team-based learning in therapeutics workshop sessions. Am J Pharm Educ. 2009;73(6):Article 100. doi: 10.5688/aj7306100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conway SE, Johnson JL, Ripley TL. Integration of team-based learning strategies into a cardiovascular module. Am J Pharm Educ. 2010;74(2):Article 35. doi: 10.5688/aj740235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Devraj R, Butler LM, Gupchup GV, Poirier TI. Active-learning strategies to develop health literacy knowledge and skills. Am J Pharm Educ. 2010;74(8):Article 137. doi: 10.5688/aj7408137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zingone MM, Franks AS, Guirguis AB, George CM, Howard-Thompson A, Heidel RE. Comparing team-based and mixed active-learning methods in an ambulatory care elective course. Am J Pharm Educ. 2010;74(9):Article 160. doi: 10.5688/aj7409160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grady SE. Team-based learning in pharmacotherapeutics. Am J Pharm Educ. 2011;75(7):Article 136. doi: 10.5688/ajpe757136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Persky AM, Pollack GM. A modified team-based learning physiology course. Am J Pharm Educ. 2011;75(10):Article 204. doi: 10.5688/ajpe7510204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gallegos PJ, Peeters JM. A measure of teamwork perceptions for team-based learning. Curr Pharm Teach Learn. 2011;3(1):30–35. [Google Scholar]
- 11.Redwanski J. Incorporating team-based learning in a drug information course covering tertiary literature. Curr Pharm Teach Learn. 2012;4(3):202–206. [Google Scholar]
- 12.Persky AM. The impact of team-based learning on a foundational pharmacokinetics course. Am J Pharm Educ. 2012;76(2):Article 31. doi: 10.5688/ajpe76231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolluru S, Roesch DM, de la Fuente AA. A multi-instructor, team-based, active-learning exercise to integrate basic and clinical sciences content. Am J Pharm Educ. 2012;76(2):Article 33. doi: 10.5688/ajpe76233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haidet P, Levine RE, Parmelee DX, et al. Guidelines for reporting team-based learning activities in the medical and health sciences education literature. Acad Med. 2012;87(3):292–299. doi: 10.1097/ACM.0b013e318244759e. [DOI] [PubMed] [Google Scholar]
- 15.McKeachie WJ, Svinicki M. Teaching Tips. 13th ed. New York, NY: Houghton Mifflin; 2011. pp. 198–200. [Google Scholar]
- 16.Medina MS. Teaching self-concept and self-esteem in a clinical communications course. Am J Pharm Educ. 2006;70(5):Article 99. doi: 10.5688/aj700599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Romanelli F, Bird E, Ryan M. Learning styles: a review of theory, application, and best practices. Am J Pharm Educ. 2009;73(1):Article 9. doi: 10.5688/aj730109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Austin Z. Development and validation of the pharmacists’ inventory of learning styles. Am J Pharm Educ. 2004;68Article 37(2) [Google Scholar]
- 19.Davis BG. Tools for Teaching. 2nd ed. San Francisco, CA: Jossey-Bass; 2009. pp. 190–206. [Google Scholar]
- 20.Feichtner SB, Davis EA. Why some groups fail: a survey of students' experiences with learning groups. J Manag Educ. 1984;9(4):58–73. [Google Scholar]
- 21.Tuckman BW. Developmental sequence in small groups. Psychol Bull. 1965;63(6):384–399. doi: 10.1037/h0022100. [DOI] [PubMed] [Google Scholar]
- 22.Fink D. Creating Significant Learning Experiences: An Integrated Approach to Designing College Course. San Francisco, CA: Jossey-Bass; 2004. [Google Scholar]
- 23.Wiggins G, McTighe JH. Understanding by Design. 2nd ed. Alexandria, VA: Association for Supervision and Curriculum Development; 2005. Backward design; pp. 13–34. [Google Scholar]
- 24.Parmalee DX, Michaelsen LK. Twelve tips for doing effective team-based learning. Med Teach. 2012;32(2):118–122. doi: 10.3109/01421590903548562. [DOI] [PubMed] [Google Scholar]
- 25.Parmelee D, Michaelsen LK, Cook S, Hudes P. Team-based learning: a practical guide: AMEE Guide No. 65. Med Teach. 2012;34(5):e275–e287. doi: 10.3109/0142159X.2012.651179. [DOI] [PubMed] [Google Scholar]
- 26.Pileggi R, O’Neill PN. Team-based learning using an audience response system: an innovative method of teaching diagnosis to undergraduate dental students. J Dent Educ. 2008;72(10):1182–1188. [PubMed] [Google Scholar]
- 27.Medina MS, Medina PJ, Wanzer D, Wilson J, Er N, Britton ML. Use of an audience response system (ARS) in a dual campus classroom environment. Am J Pharm Educ. 2008;72(2):Article 38. doi: 10.5688/aj720238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Epstein ML, Epstein BB, Brosvic GM. Immediate feedback during academic testing. Psychol Rep. 2001;88(3 Pt 1):889–894. doi: 10.2466/pr0.2001.88.3.889. [DOI] [PubMed] [Google Scholar]
- 29.Epstein ML, Brosvic GM. Students prefer the immediate feedback assessment technique. Psychol Rep. 2002;90(3 Pt 2):1136–1138. doi: 10.2466/pr0.2002.90.3c.1136. [DOI] [PubMed] [Google Scholar]
- 30.Persky AM, Pollack GM. Using answer-until-correct examinations to provide immediate feedback to students in a pharmacokinetics course. Am J Pharm Educ. 2008;72(4):Article 83. doi: 10.5688/aj720483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Michaelsen LK, Sweet M, Parmelee DX, editors. New Directions for Teaching and Learning: Team-Based Learning: Small-Group Learning’s Next Big Step. San Francisco, CA: Jossey-Bass; 2008. pp. 69–78. [Google Scholar]
- 32.Halpern DF. In: Analyzing arguments. Thought Knowledge: An Introduction to Critical Thinking. 4th ed. Halpern DF, editor. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. pp. 1–38. [Google Scholar]
- 33.Schwartz DL, Bransford JD. A time for telling. Cognition Instruct. 1998;16(4):475–522. [Google Scholar]
- 34.Mody SK, Kiley J, Gawron L, Garcia P, Hammond C. Team based learning: a novel approach to medical student education in family planning. Contraception. 2012 doi: 10.1016/j.contraception.2012.07.012. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 35.Tan NC, Kandiah N, Chan YH, Umapathi T, Lee SH, Tan K. A controlled study of team-based learning for undergraduate clinical neurology education. BMC Med Educ. 2011;11(1):91. doi: 10.1186/1472-6920-11-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Michaelsen LK, Knight AB, Fink LD. Team-based learning: a transformative use of small groups. Westport, CT: Praeger; 2002. [Google Scholar]
- 37.Wang Q. Student-facilitators’ roles in moderating online discussions. Br J Educ Technol. 2008;39(5):859–874. [Google Scholar]
- 38.Ferreri SP, O’Connor SK. Redesign of a large lecture course into a small-group learning course. Am J Pharm Educ. 2013;77(1):Article 13. doi: 10.5688/ajpe77113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levine RE, Kelly A, Karakoc T, Haidet P. Peer evaluations in a clinical clerkship: students’ attitudes, experiences, and correlations with traditional assessments. Acad Psychiatry. 2007;31(1):19–24. doi: 10.1176/appi.ap.31.1.19. [DOI] [PubMed] [Google Scholar]
- 40.Michaelsen LK, Schultheiss EE. Making feedback helpful. J Manag Educ. 1989;13(1):109–113. [Google Scholar]
- 41.Falchikov N, Goldfinch J. Student peer assessment in higher education: a meta-analysis comparing peer and teacher marks. Rev Educ Res. 2000;70(3):287–322. [Google Scholar]


