Abstract
Objective
Prior studies have shown a significant but modest association between mental disorders and violence and an increased risk in the presence of co-occurring substance use disorders. Categorical diagnoses, however, have limited utility when assessing dynamic risk state over time. This study used data from the MacArthur Violence Risk Assessment Study to examine the relationship of symptom levels and alcohol use to violence in repeated observations within two diagnostic groups.
Methods
Participants with a primary categorical diagnosis of depression (N=386) or a psychotic disorder (N=201) were identified. Subscale scores for affective or positive symptoms from the Brief Psychiatric Rating Scale and self-reported alcohol consumption were tested in panel logistic models over five ten-week intervals for their concurrent and lagged relationship to violence. An interaction term between each type of symptom and alcohol use was also tested.
Results
In models including the amount of alcohol consumed and symptom levels, a high level of affective symptoms was associated with violence during the next follow-up period only for participants with depression. There was a significant interaction between alcohol use and affective symptoms for participants with depression.
Conclusions
The relationship of symptoms and alcohol use to community violence should be considered in the context of the individual’s primary diagnosis. Further characterization of interactions between symptoms and substance use in relation to violent behavior may allow for more effective assessment of risk state and interventions for violence prevention.
Approximately 4.9 million non-lethal violent incidents occur annually in the United States (1). Although the vast majority of these incidents involve persons with no major mental disorder, social policy and law have focused on preventing violence by individuals with mental illness through civil commitment and mandated community treatments (2). These allow for involuntary confinement or supervision of persons with mental illness who, because of active symptoms, pose a danger to themselves or others. Psychopathology is thus accepted as a relevant criterion in violence prevention efforts, and yet the conditional probability of violence by diagnosis remains unclear (3).
Markers of violence might not function in the same way across different diagnostic groups. Studies in the inpatient setting suggest that symptom constellations associated with an act of violence differ according to diagnosis (4), but little is known about whether this is the case in the community. Characterization of a link between mental illness and violence thus requires consideration of two approaches: a categorical one, separating cases according to diagnostic class, and a dimensional one that examines dynamic fluctuation in risk markers such as symptom levels (5).
Previous studies of mental disorders and violence have focused particular attention on psychotic disorders (6,7). Evidence is mixed about whether individuals with chronic psychotic disorders as a group have an elevated disease-attributable risk of violence, especially after estimates are adjusted for substance use (8–13). Meanwhile, relatively little attention has been devoted to the study of violence risk among individuals with affective disorders, who also frequently have co-occurring substance use disorders (14). Depression is associated with an elevated risk of suicide, but there has been little research on violence toward others among patients with depression (15–18).
Previous studies have examined the relationship between symptom levels and violence, but generally without using diagnosis as a grouping variable (19–21). For example, hostility was found to be a significant predictor of violence across diagnoses in a sample of individuals at high risk of violence (22), whereas delusions were not associated with violence when examined across multiple diagnostic groups (23). In another investigation, co-occurring substance use and non-compliance with medications were associated with violence across mental diagnoses (24), suggesting that increased symptoms may elevate risk.
This study examined symptom levels and alcohol use among persons with either depression or a psychotic disorder, to assess whether these dynamic indicators exerted similar effects on violence risk within each diagnostic group. We examined data from the MacArthur Violence Risk Assessment Study (2), a large-scale investigation that followed psychiatric patients in the community for one year after hospital discharge. As previously reported, participants with depression had the same rate of violence as the overall patient sample, and participants with schizophrenia had a significantly lower rate of violence (2). The MacArthur study data set allows for the examination of the role of symptoms and alcohol use in a defined sample of psychiatric patients, with repeated observations over a one-year period after hospitalization. We hypothesized that reported alcohol use would have a similar impact in both groups of participants and that symptoms most characteristic of each disorder would be significantly related to the risk of community violence.
Methods
Study participants
A sample of 1,136 patients admitted to acute inpatient psychiatric facilities in three cities was recruited for the study between 1992 and 1995 (8). Eligibility criteria have been previously described (2,8). After complete description of the study to the participants, written informed consent was obtained. Institutional review board approval was obtained for this secondary analysis of the data set.
At baseline and follow-up interviews every ten weeks for one year, the participant designated a collateral informant with whom the participant had at least weekly contact. Arrest and rehospitalization records were also available. The study included interviews with participants who were hospitalized or incarcerated at the time of follow-up.
Baseline measures
Demographic variables
The participant’s age and gender were recorded during the baseline interview. Other baseline measures are described elsewhere (2,8).
Categorical diagnoses
The DSM-III-R Checklist (25,26) was administered at the baseline interview. Participants were coded on each of 17 categorical diagnoses. DSM-III-R Checklist diagnoses were compared with medical record diagnoses, and a primary diagnosis was assigned based on the most clinically significant syndrome. Data for participants with a primary diagnosis of either depression or a psychotic disorder (schizophrenia, schizoaffective disorder, brief reactive psychosis, schizophreniform disorder, delusional disorder, or psychotic disorder not otherwise specified) were included in this study.
Repeated measures
Symptom levels
The Brief Psychiatric Rating Scale (BPRS), an 18-item instrument scored on a 7-point scale (27,28), was completed at each follow-up. Subscales for affective symptoms and positive symptoms of psychosis were defined in accordance with a meta-analysis of the BPRS factor structure (29) after confirmation of subscale loadings within the overall sample. The depressive-anxiety symptoms (“affective”) score was the sum of scores on the following items: anxiety, guilt, depression, and somatic preoccupation. The positive symptoms (“positive”) subscale was the sum of scores on the following items: unusual thought content, conceptual disorganization, hallucinatory behavior, and grandiosity.
Alcohol consumption
Participants were asked the amount of beer, wine, and liquor they had consumed during the week preceding each follow-up interview. In keeping with prior studies defining binge drinking as five drinks on one day (30), amounts of alcohol consumption in the previous week were coded as none, one to nine drinks (fewer than two binge days, or one to two drinks per day), ten to 34 drinks (fewer than seven binge days, or five drinks per day), 35–69 drinks (fewer than ten per day), and 70 or more drinks.
Violence
At each follow-up interview, a revised version of the Conflict Tactics Scale (31,32) was used to ask participants and collateral informants about the participant’s involvement in violence during the previous ten weeks. Violence was defined as an aggressive act that resulted in physical injury, sexual assault, an assaultive act involving the use of a deadly weapon, or a threat made with a weapon in hand. The presence or absence of at least one act of violence was coded on the basis of a previously described algorithm for reconciling participant and collateral reports (2).
Statistical analyses
Violence outcomes at each assessment point were binary. Multivariate panel logistic regression models using maximum likelihood estimation were examined to assess relationships between symptom levels and alcohol use with concurrent violence (at time t) or lagged violence (at time t+1) as the dependent variable. Models included the five assessment times as repeated measures, with age and gender as fixed factors and the amount of alcohol consumed in the week prior to the interview and either affective or positive symptom subscales on the BPRS as time-varying covariates. Random-effects models allowed the inclusion of cases with incomplete follow-up data or no variation in the outcome variable (no violence).
Two sets of models were examined to assess the conditional effect within each diagnostic group of symptom levels and alcohol use: one set represented the relationship between symptom levels, alcohol use, and the multiplicative interaction between each type of symptom and alcohol use at time t and the occurrence of at least one incident of violence during the same period (violence at time t); the other set of models represented the lagged relationship between symptom levels, alcohol use, and the multiplicative interaction between each type of symptom and alcohol use at time t and the occurrence of at least one incident of violence during the subsequent period (violence at time t+1). Violence at time t was also included in these latter models to control for the effect of recent violence on future violence (30). Each set of models tested affective and positive symptoms separately and together.
BPRS symptom-level scores, the five-level alcohol use variable, and interaction terms were initially tested as continuous variables in panel logistic models. [Tables concerning violence at time t and at time t+1 are included in an online supplement to this article at ps.psychiatryonline.org.] In bivariate analyses, individuals consuming one to nine drinks in the week before the interview had the same odds of concurrent or lagged violence as individuals with no alcohol consumption, whereas participants consuming ten to 34 drinks, 35–69 drinks, or ≥70 drinks had significantly higher odds of violence than those with no alcohol consumption. In an alternative approach that allowed visualization of interaction term results, models were therefore constructed using categorization of the variables as follows: BPRS affect scores of <12 or ≥12 and alcohol use <10 drinks or ≥10 drinks per week. Both methods indicated the same patterns of statistical significance regarding affective symptoms. Due to nonlinearity of the relationship between positive symptoms and violence, additional analyses were performed, with BPRS positive symptom scores categorized as <8, 8–11, and ≥12, corresponding to mild, moderate, and marked levels of severity, respectively (33).
Confirmatory subscale loadings of the 18-item BPRS were conducted for 1,136 participants in EQS, version 6.1. Descriptive analyses were conducted in SAS, version 9.2, and regression analyses were conducted in Stata SE, version 10 on each of the two mutually exclusive diagnostic groups.
Missing data in the selected sample
Twenty demographic and other baseline variables that were significant predictors of violence in the initial MacArthur study analyses were used to examine patterns of missing data. Student’s t tests or chi square statistics were used to assess differences on these variables between participants present and missing at each time point within each diagnostic group.
Participants with depression who were missing at follow-up interviews differed significantly from those present (on more than two of 20 variables, or >10%), with differences generally in the direction expected for a higher risk of violence. Given that data were not missing at random, sensitivity analyses were performed within each diagnostic group to compare model differences among participants with at least one community follow-up; participants with no consecutive missed follow-ups; and participants present at all follow-ups. Although estimates differed in each of the above models, patterns of significance (at p<.05) were stable in models of affective symptoms and varied slightly in models of positive symptoms. Results are reported for participants who had at least one follow-up interview.
Results
Primary diagnosis at discharge
Of 1,136 participants in the Mac-Arthur study, 688 (61%) had a primary diagnosis of either depression (N=443) or a psychotic disorder (N= 245). Participants with no follow-up data (57 of 443 participants with depression [13%] and 44 of 245 participants with a psychotic disorder [18%]) were excluded from the analyses reported here. Participants with a psychotic disorder thus included 115 of 201 (57%) with schizophrenia and 55 of 201 (27%) with schizoaffective disorder. Of 386 remaining participants with depression, 152 (39%) also had a diagnosis of alcohol abuse or alcohol dependence, as did 67 (33%) of the 201 participants with a psychotic disorder.
Prevalence of violence overall and at each follow-up
Of the 587 participants included, 110 of 386 (29%) individuals with depression had at least one episode of violence in the year after discharge, compared with 32 of 201 (16%) individuals with a psychotic disorder (p<.001). The prevalence of violence in each follow-up period for each group is shown in Table 1.
Table 1.
Prevalence of violence at follow-up within one year among participants, by diagnostic category
| With ≥1 follow-up interview |
Violent acts in year after discharge |
Violent acts in each 10-week period after discharge |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| None |
1 |
2 |
3–4 |
Time 1 |
Time 2 |
Time 3 |
Time 4 |
Time 5 |
||||||||||||
| Disordera | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
| Depression | 386 | 87 | 276 | 72 | 88 | 23 | 16 | 4 | 6 | 2 | 46 | 13 | 34 | 10 | 21 | 7 | 24 | 8 | 15 | 5 |
| Psychotic | 201 | 82 | 169 | 84 | 18 | 9 | 12 | 6 | 2 | 1 | 15 | 8 | 6 | 3 | 9 | 6 | 13 | 8 | 5 | 3 |
Primary diagnosis
Study population
Participants with a primary diagnosis of depression were younger and more likely than those with a psychotic disorder to be white and female and to have more years of education. Demographic and other baseline information for the 587 participants in the analyses is shown in Table 2.
Table 2.
Demographic and baseline characteristics associated with violence among persons discharged with depression or a psychotic disorder and followed in the community for one year
| Selected sample (N=587) |
Depression (N=386) |
Psychotic disorder (N=201) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any violence at 1 year |
Any violence at 1 year |
Any violence at 1 year |
||||||||||
| Variable | N | % | OR | 95% CI | N | % | OR | 95% CI | N | % | OR | 95% CI |
| Demographic and historical | ||||||||||||
| Age (M±SD years) | 30±6.2 | .99 | .96–1.02 | 29.5±6.1 | 1.00 | .96–1.04 | 31.1±6.3 | 1.00 | .94–1.06 | |||
| Male gender | 322 | 55 | 1.47* | 1.00–2.16 | 191 | 50 | 1.63* | 1.04–2.55 | 131 | 65 | 1.74 | .74–4.10 |
| White | 396 | 67 | .67* | .45–.99 | 292 | 76 | .55* | .33–.89 | 104 | 52 | .50 | .23–1.09 |
| Education | ||||||||||||
| <12 years | 159 | 27 | — | — | 95 | 25 | — | — | 64 | 32 | — | — |
| High school graduate | 227 | 39 | .64 | .41–1.01 | 147 | 38 | .59 | .35–1.02 | 80 | 40 | .63 | .26–1.51 |
| >12 years | 199 | 34 | .44* | .27–.72 | 143 | 37 | .35* | .20–.63 | 56 | 28 | .56 | .21–1.52 |
| Past property arrest | 172 | 29 | 1.85* | 1.24–2.75 | 102 | 26 | 2.09* | 1.30–3.38 | 70 | 35 | 1.83 | .85–3.93 |
| Past violence arrest | 101 | 17 | 1.99* | 1.25–3.15 | 62 | 16 | 1.61 | .91–2.84 | 39 | 19 | 3.76* | 1.66–8.54 |
| Past arrest frequency (N=496) | ||||||||||||
| 0 times | 275 | 55 | — | — | 194 | 60 | — | — | 81 | 48 | — | — |
| Once or twice | 101 | 20 | 2.81* | 1.61–4.87 | 62 | 19 | 3.40* | 1.76–6.58 | 39 | 23 | 2.06 | .73–5.85 |
| ≥3 times | 120 | 24 | 4.27* | 2.57–7.10 | 70 | 22 | 6.19* | 3.33–11.50 | 50 | 29 | 2.53 | .98–6.53 |
| Past arrest seriousness (N=485) | ||||||||||||
| None | 275 | 57 | — | — | 194 | 61 | — | — | 81 | 49 | — | — |
| Minor, drugs | 116 | 24 | 2.42* | 1.41–4.16 | 70 | 22 | 3.65* | 1.94–6.88 | 46 | 28 | .98 | .31–3.11 |
| Rape, assault | 83 | 17 | 5.09* | 2.91–8.88 | 47 | 15 | 5.93* | 2.94–11.96 | 36 | 22 | 4.52* | 1.71–11.94 |
| Murder | 11 | 2 | 7.97* | 2.31–27.46 | 9 | 3 | 12.37* | 2.92–52.43 | 2 | 1 | .00 | — |
| Seriousness of childhood abuse (N=515) |
||||||||||||
| None | 15 | 3 | — | — | 6 | 2 | — | — | 9 | 5 | — | — |
| Verbal: yelling, threatening, lecturing, verbal abuse |
13 | 3 | — | — | 8 | 2 | — | — | 5 | 3 | — | — |
| Material: withholding of privileges, grounding, expulsion from home, additional chores |
160 | 31 | 1.04 | .28–3.90 | 105 | 30 | 1.40 | .156–12.61 | 55 | 33 | .78 | .14–4.32 |
| Neglect: withholding of basic needs, isolation |
26 | 5 | 1.47 | .32–6.83 | 11 | 3 | 2.86 | .24–33.90 | 15 | 9 | .88 | .12–6.58 |
| Spanking | 40 | 8 | .85 | .19–3.82 | 32 | 9 | 1.15 | .11–11.78 | 8 | 5 | .50 | .04–6.86 |
| Physical: hitting, punching, kicking, choking |
72 | 14 | 1.24 | .31–4.90 | 54 | 16 | 2.11 | .23–19.48 | 18 | 11 | .21 | .02–2.65 |
| Weapons use: including hitting with object |
176 | 34 | 1.63 | .44–6.03 | 119 | 34 | 2.73 | .31–24.12 | 57 | 34 | .66 | .12–3.68 |
| Sexual abuse | 13 | 3 | 9.00* | 1.60–50.69 | 13 | 4 | 11.25 | .97–130.22 | 0 | — | — | — |
| Frequency of childhood abuse | ||||||||||||
| Never | 124 | 21 | 70 | 18 | 54 | 27 | ||||||
| Once or twice | 68 | 12 | .89 | .40–1.98 | 42 | 11 | 1.51 | .59–3.88 | 26 | 13 | .18 | .02–1.46 |
| Sometimes | 196 | 33 | 1.34 | .76–2.37 | 134 | 35 | 1.58 | .76–3.29 | 62 | 31 | .95 | .37–2.45 |
| Frequently | 113 | 19 | 2.17* | 1.18–3.98 | 83 | 22 | 3.03* | 1.41–6.50 | 30 | 15 | .68 | .19–2.38 |
| Most of the time | 85 | 15 | 2.40* | 1.26–4.57 | 56 | 15 | 3.37* | 1.49–7.64 | 29 | 14 | 1.15 | .37–3.56 |
| Father’s drug use (N=545) | 107 | 20 | 1.55 | .98–2.47 | 81 | 23 | 1.52 | .90–2.57 | 26 | 14 | 1.22 | .42–3.52 |
| Father’s arrest history (N=518) | 190 | 37 | 1.97* | 1.31–2.95 | 137 | 39 | 1.84* | 1.15–2.94 | 53 | 32 | 2.15 | .94–4.91 |
| Mother’s drug use (N=573) | 61 | 11 | 1.24 | .68–2.24 | 42 | 11 | 1.30 | .66–2.58 | 19 | 10 | .96 | .26–3.50 |
| Head injury (N=516) | 392 | 76 | 1.99* | 1.28–3.08 | 267 | 78 | 1.76* | 1.05–2.93 | 125 | 72 | 2.46* | 1.01–6.02 |
| Clinical | ||||||||||||
| Imagined violence screen (yes) (N=585) |
174 | 30 | 1.79* | 1.21–2.67 | 124 | 32 | 1.46 | .92–2.32 | 50 | 25 | 2.83* | 1.28–6.24 |
| Total Novaco Anger Scale score (M±SD)a |
165±29 | 1.02* | 1.01–1.03 | 167±27 | 1.02* | 1.01–1.03 | 161±32 | 1.02* | 1.01–1.04 | |||
| Used substances ≥5 times in past 2 months (N=585) |
292 | 50 | 2.54* | 1.71–3.78 | 197 | 51 | 2.70* | 1.70–4.31 | 95 | 47 | 2.09 | .96–4.54 |
| Violence in past 2 months | 82 | 14 | 1.66* | 1.30–2.12 | 56 | 15 | 1.59* | 1.19–2.13 | 26 | 13 | 1.87* | 1.18–2.96 |
| Involuntary status on admission | 159 | 27 | 1.68* | 1.12–2.52 | 94 | 24 | 2.35* | 1.44–3.83 | 65 | 32 | .94 | .42–2.13 |
| Contextual: percentage of mental health professionals in social network (M±SD) |
12±15 | .17* | .04–.75 | 11±14 | .17 | .03–1.04 | 14±18 | .3 | .03–3.67 | |||
Possible scores range from 73 to 244, with higher scores indicating higher levels of anger.
p>.05
Study variables
Participants with depression had higher mean±SD ratings on the BPRS affective subscale (10.7±5.0 on a scale of 4–28, with higher scores indicating more severe symptoms) than participants with a psychotic disorder (8.5±4.7). Participants with a psychotic disorder had higher ratings on the BPRS positive subscale (7.7±4.4 on a scale of 4–28, with higher scores indicating more severe symptoms) than participants with depression (5.0±2.1). Group differences were significant at p<.001. There was no significant group difference in amount of alcohol consumed.
Correlates of violence in a 10-week period
The presence or absence of a violent incident at time t and time t+1 and demographic variables (age and gender), affective and positive symptom scores, and alcohol levels were examined (not shown). Violence at time t and at time t+1 was significantly associated (p<.001) in each group of participants, and violence at time t was associated with the amount of alcohol consumed at time t (p<.001). Amount of alcohol consumed at time t was also significantly related to violence at time t+1 for both groups (p≤.001).
Multivariate panel logistic models
Panel logistic models using either continuous or categorized study variables both showed distinctive patterns in main effects for each diagnostic group. Among participants with depression, violence at time t was associated with both affective symptoms (odds ratio [OR]=1.07, SE=.03, 95% confidence interval [CI]=1.03–1.12) and positive symptoms (OR= 1.23, SE=.06, CI=1.12–1.34) as well as with alcohol use (OR=1.55, SE=.14, CI=1.30–1.85) at time t. Among participants with a psychotic disorder, positive symptoms (OR=1.11, SE=.05, CI=1.03–1.21) and alcohol use (OR=1.58, SE=.26, CI=1.14–2.19) were associated with violence at time t. The interaction of symptoms and alcohol use was not significant in either group. Table 3 shows results of analyses using the categorized variables, which mirror results using the continuous affective symptom variables.
Table 3.
Violence at time t predicted by variables at time t among persons discharged with depression or a psychotic disorder
| BPRS affectivea |
BPRS positivea |
Affective and positive |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depression (N=385; 1,575 observations) |
Psychotic (N=200; 820 observations) |
Depression (N=383; 1,513 observations) |
Psychotic (N=199; 808 observations) |
Depression (N=383; 1,511 observations) |
Psychotic (N=199; 807 observations) |
|||||||
| Variableb | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Age | .99 | .95–1.03 | .98 | .91–1.05 | 1.00 | .96–1.04 | .97 | .91–1.04 | .99 | .95–1.03 | .97 | .91–1.04 |
| Male | 1.56 | .96–2.51 | 1.51 | .57–4.00 | 1.39 | .88–2.21 | 1.25 | .50–3.13 | 1.5 | .93–2.40 | 1.24 | .49–3.11 |
| Affective score | ||||||||||||
| ≥12 | 2.00* | 1.30–3.07 | 1.27 | .54–2.98 | 1.79* | 1.15–2.76 | .97 | .41–2.29 | ||||
| Positive score | ||||||||||||
| 8–11 | 2.36* | 1.22–4.56 | 2.39 | .99–5.78 | 2.06* | 1.06–4.02 | 2.40 | .98–5.86 | ||||
| Positive score | ||||||||||||
| ≥12 | 4.30* | 1.57–11.79 | 3.13* | 1.23–7.99 | 3.81* | 1.36–10.67 | 3.17* | 1.21–8.30 | ||||
| Alcohol ≥10 drinks per week |
3.37* | 2.09–5.42 | 3.62* | 1.51–8.66 | 3.41* | 2.13–5.47 | 3.65* | 1.55–8.59 | 3.32* | 2.07–5.34 | 3.65* | 1.55–8.59 |
| Within-subject correlation (ρ) |
.26 | .14–.42 | .42 | .23–.65 | .22 | .11–.40 | .36 | .17–.61 | .23 | .11–.40 | .36 | .17–.61 |
BPRS, Brief Psychiatric Rating Scale
Time t for affective score, positive score, and alcohol use
p>.05
The panel logistic models showed different patterns for lagged effects. Among participants with depression, violence at time t+1 was associated with violence at time t (OR=3.51, SE=1.32, CI=1.68–7.34) and with affective symptoms (OR=1.08, SE=.04, CI=1.01–1.16) and alcohol use (OR=2.66, SE=.78, CI=1.50–4.73) at time t; there was a significant negative interaction of alcohol use and affective symptoms (OR=.95, SE=.02, CI=.91–.99). Among participants with psychotic disorders, violence at time t+1 was significantly associated with alcohol use only (OR=1.59, SE=.29, CI=1.11–2.28).
Table 4 shows results of analyses with the categorized variables. Among participants with depression, again, violence at time t+1 was associated with violence at time t and with high alcohol use and a high level of affective symptoms (BPRS affective score ≥12) at time t, with a significant negative (OR<1) interaction of alcohol use and affective symptoms. Among participants with psychotic disorders, however, violence at time t+1 was significantly associated with a moderate level (BPRS positive score 8–11) but not a high level (score ≥12) of positive symptoms and with alcohol use. Interaction terms between each symptom type and alcohol use were not significant for participants with a psychotic disorder.
Table 4.
Violence at time t+1 predicted by variables at time t among persons discharged with depression or a psychotic disorder
| BPRS affectivea |
BPRS positivea |
Affective and positive |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depression (N=349; 1,129 observations) |
Psychotic (N=182; 586 observations) |
Depression (N=347; 1,092 observations) |
Psychotic (N=182; 581 observations) |
Depression (N=347; 1,090 observations) |
Psychotic (N=182; 580 observations) |
|||||||
| Variableb | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Age | 1.01 | .97–1.06 | .99 | .92–1.06 | 1.02 | .97–1.07 | .98 | .92–1.05 | 1.01 | .97–1.06 | .98 | .92–1.05 |
| Male | 1.30 | .74–2.28 | 1.27 | .49–3.29 | 1.14 | .64–2.02 | 1.14 | .47–2.78 | 1.25 | .71–2.23 | 1.13 | .46–2.77 |
| Violence | 3.91* | 1.96–7.80 | 2.48 | .59–10.46 | 3.55* | 1.73–7.28 | 2.75 | .65–11.59 | 3.82* | 1.89–7.71 | 2.71 | .64–11.43 |
| Affective score | ||||||||||||
| ≥12 | 2.51* | 1.28–4.93 | 1.01 | .38–2.68 | 2.38* | 1.20–4.74 | .84 | .32–2.20 | ||||
| Positive score | ||||||||||||
| 8–11 | 1.17 | .46–2.93 | 2.86* | 1.17–6.99 | 1.09 | .44–2.70 | 2.97* | 1.19–7.45 | ||||
| Positive score | ||||||||||||
| ≥12 | 2.68 | .74–9.73 | 1.02 | .29–3.51 | 2.37 | .67–8.43 | 1.07 | .30–3.78 | ||||
| Alcohol ≥10 drinks per week |
6.90* | 3.04–15.66 | 4.15* | 1.63–10.59 | 3.44* | 1.82–6.52 | 3.74* | 1.53–9.10 | 6.78* | 2.96–15.54 | 3.82* | 1.55–9.43 |
| Affective × alcohol |
.24* | .08–.75 | .22* | .07–.70 | ||||||||
| Within-subject correlation (ρ) |
.06 | .00–.86 | .22 | .03–.74 | .11 | .01–.57 | .11 | .00–.90 | .07 | .00–.76 | .12 | .00–.88 |
BPRS, Brief Psychiatric Rating Scale
Time t for affective score, positive score, and alcohol use
p>.05
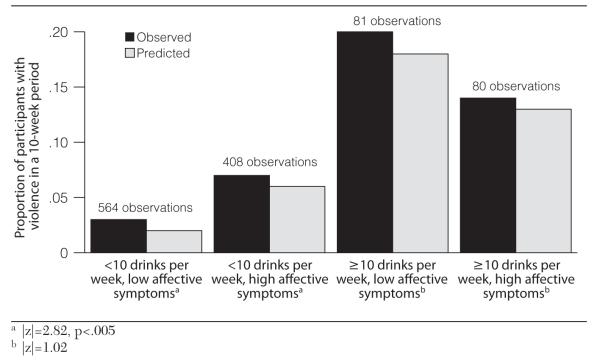
Figure 1 illustrates, with analyses using dichotomous variables, the consistently observed interaction between affective symptoms and alcohol use in relation to violence at time t+1 for participants with depression. Affective symptom levels had a significant effect on violence at low (but not at high) levels of alcohol use. Although there was a main effect for alcohol use, the difference between the low and high affective symptom classes was significant only at a lower level of drinking (p<.005).
Figure 1.
Relationship of affective symptoms and alcohol with violence among participants with depression
Figure 1 thus shows that for participants with depression and low alcohol use, affective symptoms were associated with an increased probability of violence, and higher levels of alcohol use were associated with violence at any affective symptom level. A negative multiplicative interaction term indicates here that although alcohol use and affective symptoms each increased the risk of violence, together they increased risk less than alcohol alone in this diagnostic group (34).
Discussion
In this study, affective symptoms and alcohol use were associated with concurrent and future violence of participants with depression. The relationship of positive symptoms and alcohol use to violence of participants with a psychotic disorder was less evident. There was a significant negative interaction between affective symptoms and alcohol use as predictors of subsequent violence of participants with depression, and there was no appreciable interaction between alcohol use and either type of symptom for participants with a psychotic disorder.
Recent past violence (within the past ten weeks) was a strong predictor of violence by participants with depression, but not by participants with a psychotic disorder. This suggests that the adage indicating past violence as the best predictor of future violence (2) may not hold equally across diagnostic groups, at least in the relatively short interval of a ten-week follow-up period. The finding within this time frame is nonetheless most relevant for ongoing clinical management and attention to violence risk in different diagnostic groups. Wide confidence intervals for the participants with a psychotic disorder resulted from a low rate of violence in this group. Although positive symptom findings are somewhat consistent with previous large cross-sectional studies (21,35), the effect of recent prior violence in this sample of participants with a psychotic disorder is inconclusive.
Substance use has been consistently and strongly associated with violence (8,36), but evidence about the dynamics of this link is still limited (30). Prior studies of violence demonstrated a moderate association between a diagnosis of a mental disorder and violence and an elevated risk when associated with a co-occurring substance use disorder (8,11,21,37). Our findings suggest further that dimensions of symptoms and the amount of alcohol use are also salient to dynamic risk of violence, perhaps more so than categorical diagnoses.
Our focus in this study on affective symptoms of depression and positive symptoms of psychosis was guided by a primary aim of examining specific effects within diagnostic groups. Many of the anergic symptoms of depression, such as blunted affect, social isolation, and psychomotor slowing, are represented in another subscale of the BPRS, but we did not test this subscale because these symptoms overlap with negative symptoms of psychosis (38). Furthermore, our analyses did not test the effects of participants’ medication or adherence to it. Alcohol may, for instance, increase the sedating effects of antipsychotic medication, thus decreasing the individual’s propensity for aggression in social situations. These findings thus point to future investigations of violence risk of patients with depression, to examine additional variables (such as anergic symptoms, childhood antisocial conduct, and medication compliance), previously characterized in studies focused on patients with schizophrenia (35, 39,40).
Two caveats should be noted regarding time course. First, prior studies on the larger MacArthur Violence Risk Study sample demonstrated that adjusting for time at risk does not significantly affect the risk estimates (2). There was, however, an overall pattern of decreased rates of violence over the one-year study period for participants with depression, suggesting that factors relating to this decrease would be useful to examine. Second, although a ten-week interval is reasonable for examining clinically significant change in the evolution of primary psychiatric symptoms in specific diagnoses, the interval is long for studying effects of alcohol (30). Further characterization of a relationship between symptom fluctuation and alcohol use would require a fine-grained analysis using repeated measures at shorter intervals.
Conclusions
The results of this study suggest that violence risk among patients with psychotic disorders may function in a substantially different manner from the way it unfolds among patients with depression, in terms of both predictors and mechanisms. We selected two groups characterized by distinctive symptoms in order to contrast the effects within diagnostic categories. Examining a larger array of symptoms and how they map onto a set of other diagnoses, such as bipolar disorder or personality disorders, merits further study. Our results indicate that examination of the relationship between symptoms and violence across broad samples of patients does not appear sufficiently nuanced to give us clinically useful tests of this phenomenon. More appropriate tests require conditional assessment of different symptom types in the context of the individual’s disorder.
Whereas suicide risk is routinely assessed with particular vigilance in clinical practice with depressed patients, their risk of harm to others is less commonly the focus of assessment and treatment. Our findings suggest that affective symptoms are associated with risk of harm to others and that this risk is further increased when patients with depression use alcohol. Just as we regularly assess suicidality with a focused aim of prevention in this population, increased attention to the assessment of violence risk associated with depression may afford an additional opportunity for prevention and improvement of quality of life.
Supplementary Material
Acknowledgments and disclosures
During the preparation of the manuscript, Dr. Yang was supported by grant T32 MH16804 from the National Institute of Mental Health and by the U.S. Department of Veterans Affairs (VA), Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment. Contents do not represent the views of the VA or the U.S. government. Dr. Yang thanks Kevin Kim, Ph.D., Candice Odgers, Ph.D., and Ada Youk, Ph.D., for valuable advice during data analysis and Bruno Falissard, M.D., Ph.D., for insightful comments on the manuscript.
Dr. Mulvey is a shareholder in COVR, Inc., which distributes Classification of Violence Risk (COVR) through Psychological Assessment Resources, Inc.
Footnotes
The other authors report no competing interests.
Contributor Information
Dr. Suzanne Yang, Veterans Integrated Service Network (VISN) 4 Mental Illness Research, Education and Clinical Center (MIRECC), VA Pittsburgh Healthcare System, 7180 Highland Dr., Pittsburgh, PA 15206 (yangs@upmc.edu). She is also with the Western Psychiatric Institute and Clinic and the Law and Psychiatry Program, University of Pittsburgh.
Dr. Edward P. Mulvey, Western Psychiatric Institute and Clinic and the University of Pittsburgh School of Medicine.
Dr. Thomas A. Loughran, Department of Criminology, University of Maryland, College Park.
Dr. Barbara H. Hanusa, Center for Health Equity Research and Promotion and the VISN 4 MIRECC, VA Pittsburgh Healthcare System.
References
- 1.Rand MR. Criminal Victimization, 2008. US Department of Justice; Washington, DC: 2009. [Google Scholar]
- 2.Monahan J, Steadman HJ, Silver E, et al. Rethinking Risk Assessment: The MacArthur Study of Mental Disorder and Violence. Oxford University Press; New York: 2001. [Google Scholar]
- 3.Mulvey EP, Lidz CW. Clinical prediction of violence as a conditional judgment. Social Psychiatry and Psychiatric Epidemiology. 1998;33(suppl 1):S107–S113. doi: 10.1007/s001270050218. [DOI] [PubMed] [Google Scholar]
- 4.McNiel DE, Binder RL. The relationship between acute psychiatric symptoms, diagnosis, and short-term risk of violence. Hospital and Community Psychiatry. 1994;45:133–137. doi: 10.1176/ps.45.2.133. [DOI] [PubMed] [Google Scholar]
- 5.Douglas KS, Skeem JL. Violence risk assessment: getting specific about being dynamic. Psychology, Public Policy, and Law. 2005;11:347–383. [Google Scholar]
- 6.Douglas KS, Guy LS, Hart SD. Psychosis as a risk factor for violence to others: a meta-analysis. Psychological Bulletin. 2009;135:679–706. doi: 10.1037/a0016311. [DOI] [PubMed] [Google Scholar]
- 7.Taylor PJ. When symptoms of psychosis drive serious violence. Social Psychiatry and Psychiatric Epidemiology. 1998;33(suppl 1):S47–S54. doi: 10.1007/s001270050209. [DOI] [PubMed] [Google Scholar]
- 8.Steadman HJ, Mulvey EP, Monahan J, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Archives of General Psychiatry. 1998;55:393–401. doi: 10.1001/archpsyc.55.5.393. [DOI] [PubMed] [Google Scholar]
- 9.Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2009;66:152–161. doi: 10.1001/archgenpsychiatry.2008.537. [DOI] [PubMed] [Google Scholar]
- 10.Arseneault L, Moffitt TE, Caspi A, et al. Mental disorders and violence in a total birth cohort: results from the Dunedin study. Archives of General Psychiatry. 2000;57:979–986. doi: 10.1001/archpsyc.57.10.979. [DOI] [PubMed] [Google Scholar]
- 11.Eronen M, Angermeyer MC, Schulze B. The psychiatric epidemiology of violent behaviour. Social Psychiatry and Psychiatric Epidemiology. 1998;33(suppl 1):S13–S23. doi: 10.1007/s001270050205. [DOI] [PubMed] [Google Scholar]
- 12.Fazel S, Gulati G, Linsell L, et al. Schizophrenia and violence: systematic review and meta-analysis. PLoS Medicine. 2009;6:e1000120. doi: 10.1371/journal.pmed.1000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fazel S, Langstrom N, Hjern A, et al. Schizophrenia, substance abuse, and violent crime. JAMA. 2009;301:2016–2023. doi: 10.1001/jama.2009.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 15.Modestin J, Hug A, Ammann R. Criminal behavior in males with affective disorders. Journal of Affective Disorders. 1997;42:29–38. doi: 10.1016/s0165-0327(96)00093-6. [DOI] [PubMed] [Google Scholar]
- 16.Beal CA, Kroner DG, Weekes JR. Persecutory ideation and depression in mild violence among incarcerated adult males. International Journal of Offender Therapy and Comparative Criminology. 2003;47:159–170. doi: 10.1177/0306624X03252173. [DOI] [PubMed] [Google Scholar]
- 17.Graz C, Etschel E, Schoech H, et al. Criminal behaviour and violent crimes in former inpatients with affective disorder. Journal of Affective Disorders. 2009;117:98–103. doi: 10.1016/j.jad.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Fazel S, Lichtenstein P, Grann M, et al. Bipolar disorder and violent crime: new evidence from population-based longitudinal studies and systematic review. Archives of General Psychiatry. 2010;67:931–938. doi: 10.1001/archgenpsychiatry.2010.97. [DOI] [PubMed] [Google Scholar]
- 19.Gray NS, Hill C, McGleish A, et al. Prediction of violence and self-harm in mentally disordered offenders: a prospective study of the efficacy of HCR-20, PCL-R, and psychiatric symptomatology. Journal of Consulting and Clinical Psychology. 2003;71:443–451. doi: 10.1037/0022-006x.71.3.443. [DOI] [PubMed] [Google Scholar]
- 20.Amore M, Menchetti M, Tonti C, et al. Predictors of violent behavior among acute psychiatric patients: clinical study. Psychiatry and Clinical Neurosciences. 2008;62:247–255. doi: 10.1111/j.1440-1819.2008.01790.x. [DOI] [PubMed] [Google Scholar]
- 21.Swanson J, Estroff S, Swartz M, et al. Violence and severe mental disorder in clinical and community populations: the effects of psychotic symptoms, comorbidity, and lack of treatment. Psychiatry. 1997;60:1–22. doi: 10.1080/00332747.1997.11024781. [DOI] [PubMed] [Google Scholar]
- 22.Skeem JL, Schubert C, Odgers C, et al. Psychiatric symptoms and community violence among high-risk patients: a test of the relationship at the weekly level. Journal of Consulting and Clinical Psychology. 2006;74:967–979. doi: 10.1037/0022-006X.74.5.967. [DOI] [PubMed] [Google Scholar]
- 23.Appelbaum PS, Robbins PC, Monahan J. Violence and delusions: data from the MacArthur Violence Risk Assessment Study. American Journal of Psychiatry. 2000;157:566–572. doi: 10.1176/appi.ajp.157.4.566. [DOI] [PubMed] [Google Scholar]
- 24.Swartz MS, Swanson JW, Hiday VA, et al. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. American Journal of Psychiatry. 1998;155:226–231. doi: 10.1176/ajp.155.2.226. [DOI] [PubMed] [Google Scholar]
- 25.Janca A, Helzer J. DSM-III-R Criteria Checklist. Diagnostic Interview Schedule Newsletter. 1990;1990:7–17. [Google Scholar]
- 26.Hudziak JJ, Helzer JE, Wetzel MW, et al. The use of the DSM-III-R Checklist for initial diagnostic assessments. Comprehensive Psychiatry. 1993;34:375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- 27.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports. 1962;10:799–812. [Google Scholar]
- 28.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale (BPRS): recent developments in ascertainment and scaling. Psychopharmacology Bulletin. 1988;24:97–99. [PubMed] [Google Scholar]
- 29.Shafer A. Meta-analysis of the Brief Psychiatric Rating Scale factor structure. Psychological Assessment. 2005;17:324–335. doi: 10.1037/1040-3590.17.3.324. [DOI] [PubMed] [Google Scholar]
- 30.Mulvey EP, Odgers C, Skeem J, et al. Substance use and community violence: a test of the relation at the daily level. Journal of Consulting and Clinical Psychology. 2006;74:743–754. doi: 10.1037/0022-006X.74.4.743. [DOI] [PubMed] [Google Scholar]
- 31.Straus MA, Gelles RJ, Smith C. Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. Transaction Publishers; New Brunswick, NJ: 1990. [Google Scholar]
- 32.Lidz CW, Mulvey EP, Gardner W. The accuracy of predictions of violence to others. JAMA. 1993;269:1007–1011. [PubMed] [Google Scholar]
- 33.Leucht S, Kane JM, Kissling W, et al. Clinical implications of Brief Psychiatric Rating Scale scores. British Journal of Psychiatry. 2005;187:366–371. doi: 10.1192/bjp.187.4.366. [DOI] [PubMed] [Google Scholar]
- 34.Swanson JW, Holzer CE., III Violence and ECA data. Hospital and Community Psychiatry. 1991;42:954–955. doi: 10.1176/ps.42.9.954. [DOI] [PubMed] [Google Scholar]
- 35.Swanson JW, Swartz MS, Van Dorn RA, et al. A national study of violent behavior in persons with schizophrenia. Archives of General Psychiatry. 2006;63:490–499. doi: 10.1001/archpsyc.63.5.490. [DOI] [PubMed] [Google Scholar]
- 36.Pulay AJ, Dawson DA, Hasin DS, et al. Violent behavior and DSM-IV psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:12–22. doi: 10.4088/jcp.v69n0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Van Dorn R, Volavka J, Johnson N. Mental disorder and violence: is there a relationship beyond substance use? Social Psychiatry and Psychiatric Epidemiology. doi: 10.1007/s00127-011-0356-x. Epub Feb 26, 2011. [DOI] [PubMed] [Google Scholar]
- 38.Carpenter WT, Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. American Journal of Psychiatry. 1988;145:578–583. doi: 10.1176/ajp.145.5.578. [DOI] [PubMed] [Google Scholar]
- 39.Swanson JW, Swartz MS, Van Dorn RA, et al. Comparison of antipsychotic medication effects on reducing violence in people with schizophrenia. British Journal of Psychiatry. 2008;193:37–43. doi: 10.1192/bjp.bp.107.042630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Swanson JW, Van Dorn RA, Swartz MS, et al. Alternative pathways to violence in persons with schizophrenia: the role of childhood antisocial behavior problems. Law and Human Behavior. 2008;32:228–240. doi: 10.1007/s10979-007-9095-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.