Abstract
Asymptomatic Chlamydia trachomatis infections are common in HIV-infected men who have sex with men (MSM). Although C. trachomatis combined with HIV would be likely to enhance inflammation, the asymptomatic course suggests otherwise. We assessed local inflammation, mucosal damage, and cytokine concentrations in rectal mucosal fluid samples from patients with HIV (with or without the use of combination antiretroviral therapy [cART]) and with or without the presence of rectal C. trachomatis. Rectal swabs from 79 MSM (with and without C. trachomatis, HIV, and cART use) who reported a history of receptive anal sex were analyzed for neutrophil activation (measured by myeloperoxidase [MPO]), mucosal leakage (measured by albumin and alpha-2-macroglobulin), and proinflammatory and anti-inflammatory cytokines. C. trachomatis infection, HIV infection, and cART use in MSM had no differential effects on rectal neutrophilic inflammation and mucosal damage. Interleukin 8 (IL-8) was found to correlate with MPO, and MPO correlated with markers of mucosal damage. In HIV-negative participants, men with C. trachomatis infection had lower concentrations of monocyte chemotactic protein 1 (MCP-1), IL-1α, and IL-1 receptor antagonist (IL-1RA) than men without rectal C. trachomatis infection (P = 0.005, 0.007, and 0.07, respectively). We found no difference in anal cytokine concentrations in HIV-infected participants in relation to the presence of C. trachomatis infection or cART use. In participants with rectal C. trachomatis infection, those who were HIV negative had lower median concentrations of IL-8 and IL-1α than those with HIV (P = 0.05 and 0.06, respectively). The slope of the regression line between MPO and IL-8 was reduced in participants with rectal C. trachomatis infection. C. trachomatis dampens cytokine concentrations but not in HIV-infected patients. The extent of mucosal damage was comparable in all patient groups. The apparent reduced neutrophil response to IL-8 in HIV-infected patients with C. trachomatis infection is in accordance with its asymptomatic course.
INTRODUCTION
Urogenital infection with Chlamydia trachomatis is the most commonly reported sexually transmitted infection (STI) and continues to be a major public health problem worldwide. Untreated C. trachomatis infections can lead to serious complications, such as pelvic inflammatory disease in women and epididymitis in men (1). Asymptomatic C. trachomatis infections are common, including in men who have sex with men (MSM) who are infected with human immunodeficiency virus (HIV) (2–5). This is thus a major clinical problem, since C. trachomatis infection is regarded as an important cofactor in incident HIV infections among MSM (6, 7). C. trachomatis infection is associated with increased HIV shedding (8, 9), and the treatment of C. trachomatis urethritis reduces seminal HIV RNA concentrations in HIV-infected men (10). The exact mechanisms by which C. trachomatis infections increase viral shedding and why C. trachomatis infections are often asymptomatic are not well understood. It has been suggested that sexually transmitted infections (STIs), such as C. trachomatis, enhance HIV transmission through an increased release of proinflammatory cytokines (8), which attenuates the local mucosal immune defense.
Several studies have assessed the concentrations of proinflammatory cytokines in C. trachomatis infections and other STIs. In vitro, C. trachomatis has increased the concentration of cytokines in fibroblasts like synovial and epithelial cells (11, 12). Furthermore, in vivo increases in local proinflammatory and anti-inflammatory cytokines in C. trachomatis infections have been found in cervical lavage specimens in women (13) and on urethral swabs in men (14, 15). Increased concentrations of cytokines were also detected in the urine of men infected with Neisseria gonorrhoeae before the onset of symptoms, and these concentrations peaked at the onset of symptoms (16).
Taken together, it is likely that HIV-infected patients coinfected with C. trachomatis have more pronounced local inflammation than patients with either HIV or C. trachomatis infection. In addition, HIV-infected patients, especially those who are not treated with combination antiretroviral therapy (cART), may have decreased cellular immunity (17), which might impede the adaptive immune response to C. trachomatis and further aggravate inflammation. The enhanced inflammation, however, is not consistent with the commonly asymptomatic course of C. trachomatis infection in HIV-infected patients. To our knowledge, mucosal damage and the inflammatory and immune responses of the rectal mucosa have not been previously studied. The aim of this exploratory study was to assess whether rectal C. trachomatis infection status, HIV infection status, and use of cART affect local markers of mucosal damage (measured by leakage) and inflammation (measured by neutrophil activation), as well as the concentrations of several proinflammatory and anti-inflammatory cytokines and chemokines (interleukin 8 [IL-8], monocyte chemotactic protein 1 [MCP-1], macrophage inflammatory protein 1β [MIP-1β], IL-1α, IL-1β, interleukin 1 receptor antagonist [IL-1RA], IL-6, and IL-10) in the rectums of MSM who have had receptive anal intercourse.
MATERIALS AND METHODS
Study population.
The outpatient STI clinic of the Public Health Service of Amsterdam (GGD Amsterdam) offers free and anonymous STI testing and treatment (18). From November 2010 to February 2011, consecutive MSM attendees of the clinic who reported having receptive anal sex in the preceding 6 months and who were visiting the clinic for an STI screening were invited to participate in the study. Further inclusion criteria were being ≥16 years of age and having a sufficient understanding of the study as presented in Dutch or English. Before routine consultation with the nurse, the study was explained and the patient was invited to participate. After obtaining informed consent for participation, we asked HIV-infected patients for written approval to obtain data on CD4 cell count, HIV RNA load, and cART use from the physician treating their HIV infection. Patients who declined to permit us to obtain data from their treating physicians were still allowed to participate. We aimed to select 90 participants from the total group who gave informed consent for cytokine testing. To study the effects of C. trachomatis status, HIV status, and cART use on markers of inflammation, mucosal damage, and cytokine concentrations, we intended to recruit 15 participants in each of the following 6 groups: group A, C. trachomatis-negative and HIV-negative MSM; group B, C. trachomatis-negative HIV-infected MSM not receiving cART; group C, C. trachomatis-negative HIV-infected MSM receiving cART; group D, C. trachomatis-positive HIV-negative MSM; group E, C. trachomatis-positive HIV-infected MSM not receiving cART; and group F, C. trachomatis-positive HIV-infected MSM receiving cART.
Participants who were diagnosed with lymphogranuloma venereum, rectal gonorrhea, rectal herpes, anal warts, or non-C. trachomatis proctitis were excluded. Also, participants who were diagnosed with syphilis or acute hepatitis B or C infection were excluded. For the analysis, we selected consecutive participants for each of the six groups. However, for groups consisting of HIV-infected MSM, we preferred those who permitted us to obtain data from the physician treating their HIV infection over those who did not. Also, we preferred participants without any other STI except rectal C. trachomatis infection. The medical ethics committee of the Academic Medical Center approved the study. All participants provided written informed consent.
Procedures and laboratory testing.
All patients were screened for STIs according to the clinic protocol (19). A nucleic acid amplification test (NAAT) (Gen-Probe Aptima Combo 2 assay; Gen-Probe Incorporated, San Diego, CA) was used to diagnose C. trachomatis infection. HIV screening was performed via a third-generation commercial microparticle enzyme immunoassay system (AxSYM HIV Ag/Ab Combo assay; Abbott, Abbott Park, IL). HIV-positive test results were confirmed by immunoblot (INNO-LIA HIV I/II score; Innogenetics NV, Ghent, Belgium).
An additional anal swab for cytokine measurements was taken from all participants with a dry cotton tip swab before the standard rectal swabs for the C. trachomatis and N. gonorrhoeae tests were performed. The swab was placed 5 cm into the rectum, twisted for 10 s, and placed in 1 ml phosphate-buffered saline (PBS) (pH 7.4) at 4°C, and debris was cleared by centrifugation at 260 × g for 10 min within 24 h of collection. The supernatant was stored in aliquots at −20°C until analysis.
The amount of mucosal lining fluid on the swabs differed among the participants. Albumin (Alb) is a relatively small molecule in the circulation, which passes the mucosal barrier relatively unrestricted. Thus, the concentration in the mucosal lining fluid is almost in equilibrium with the concentration in the circulation (20) unless there is leakage across the mucosal barrier, such as that caused by inflammatory damage. Consequently, the concentration of albumin (Alb) in the supernatant of the swab reflects the dilution of the mucosal lining fluid. The albumin quotient [Q(Alb)] (calculated as [Alb]supernatant/[Alb]serum) was calculated for each participant. We adjusted for the dilution of the mucosal-lining fluid for each participant by dividing the observed values for the various parameters in the swab by the Q(Alb). The amount of Alb was determined using nephelometry (modular preanalytics EVO [MPA]; Roche).
When there is substantial leakage across the rectal mucosa, Q(Alb) should not be used to adjust for the dilution of the mucosal lining fluid. To check whether there was substantial leakage, we also assessed the concentration of alpha-2-macroglobulin (A2M). A2M is a large molecule in the circulation, and its passage across the mucosal membrane is more restricted than that of albumin, unless there is mucosal leakage (21). This mucosal leakage can be expressed as Q(A2M) (calculated as [A2M]supernatant/[A2M]serum) or by comparison of the leakage of A2M with that of albumin in the relative coefficient of excretion (RCE) [calculated by Q(A2M)/Q(Alb) (22)]. In case of dilution of the mucosal lining fluid, the Q(Alb) and Q(A2M) are attenuated in a similar manner. In case of leakage across the mucosal barrier, the Q(A2M) values will be close to those of Q(Alb), thus raising the RCE. A2M was determined by enzyme-linked immunosorbent assay (ELISA) (21).
The concentration of myeloperoxidase (MPO) released by activated neutrophils in the supernatant was taken as a marker of neutrophilic inflammation and was measured by ELISA (lower detection limit, 1.5 ng/ml) (23). The MPO ELISA had an interassay coefficient of variation (CV) of <15% and an intra-assay CV of <15%. MPO values were adjusted for variable dilution by dividing by the Q(Alb).
The concentrations of IL-8, MCP-1, MIP-1β, IL-1α, IL-1β, IL-1RA, IL-6, and IL-10 were analyzed in the supernatant with a multiplex fluorescent bead assay, according to the standard protocol (Bio-Rad Laboratories, Clinical Diagnostics Group, Hercules, CA). Fluorescence was quantified with a Bio-Plex 200 (Bio-Rad Laboratories, Clinical Diagnostics Group, Hercules, CA). Cytokine concentrations were adjusted for variable dilution by dividing by the Q(Alb).
Although the volume of the rectal swab samples was limited, we performed recoveries with standard material for A2M, MPO, and the cytokines IL-8, MCP-1, MIP-1β, IL-6, and IL-10, which yielded recoveries between 78 and 122% or better. We were not able to perform recoveries for IL-1α, IL-1β, IL-1RA, and albumin and therefore cannot exclude that the amounts of these proteins were underestimated. The values for Alb, A2M, and MPO were based on at least two closely matching values from serial dilutions, confirming the identity of the quantified proteins. Several rectal swab samples were rerun in Luminex, yielding values very similar to those obtained before.
Statistical analyses.
A value of half the lower limit of detection was assigned to samples with cytokine or MPO concentrations below the lower limit of detection of the assay. The effects of C. trachomatis infection status, HIV infection status, and cART use on the markers of mucosal damage and inflammation and on cytokine concentrations were analyzed by the following comparisons: (i) the effect of C. trachomatis infection, by comparing HIV-negative participants without and with C. trachomatis infection (group A versus D) and by comparing HIV-infected participants without and with C. trachomatis infection (groups B plus C versus E plus F); (ii) the effect of HIV, by comparing HIV-negative and HIV-infected participants with C. trachomatis infection (group D versus E plus F); (iii) the effect of cART use, by comparing HIV-infected participants with C. trachomatis infection without and with cART use (E versus F); and (iv) participants with self-reported anal symptoms versus participants without self-reported anal symptoms.
Differences between the Q(A2M), Q(Alb), RCE, MPO, and cytokine concentrations were calculated by the Wilcoxon test. No corrections for multiple testing were done. In scatter plots, fitted regression lines were calculated. We plotted Q(A2M) against Q(Alb) because a marked correlation would suggest no leakage across the rectal mucosa. We also plotted MPO against IL-8 for C. trachomatis-negative participants and C. trachomatis-positive participants to assess whether there were differences in the MPO increases in reaction to IL-8 increases; IL-8 is a major chemokine for neutrophil recruitment and activation, and increases of IL-8 should correspond with increases in MPO.
Data analyses were performed with Stata 11.2 (Intercooled Stata; Stata, College Station, TX). Differences were considered significant at a P value of ≤ 0.05 and near significant at P values of >0.05 and ≤0.1. In the figures, a log10 scale was used. The adjusted values are presented in Fig. 1 and 2 and in Tables S2, S3, and S4 in the supplemental material, unless indicated otherwise.
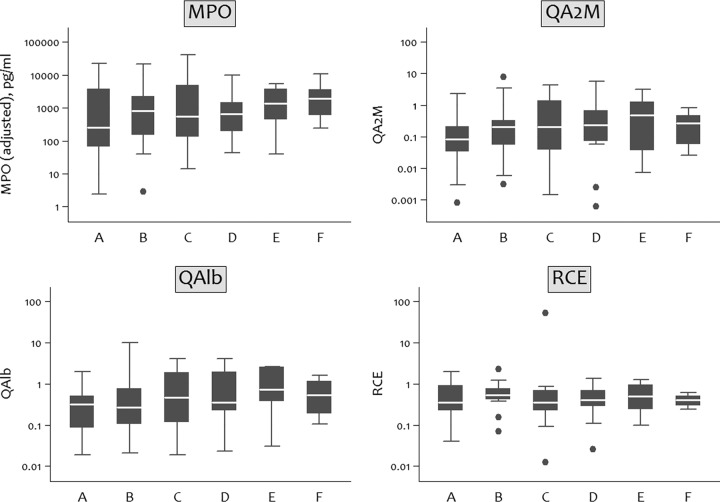
Fig 1.
Adjusted MPO concentrations and Q(A2M), RCE, and Q(Alb) concentrations for each group in study on rectal cytokines and C. trachomatis, Amsterdam, 2010 to 2011. For Q(A2M) and Q(Alb), the values were multiplied by 1,000. MPO, myeloperoxidase; A2M, alpha-2-macroglobulin; Q(A2M), ratio of A2M in supernatant to A2M in serum; Q(Alb), ratio of albumin in supernatant to albumin in serum. RCE was calculated by Q(A2M)/Q(Alb). MPO concentration was adjusted by dividing by the Q(Alb). The boxes represent the values from the 25 to 75 percentiles, the middle lines represent the medians, the vertical lines extend from the minimum to the maximum values, and the filled circles represent outliers.
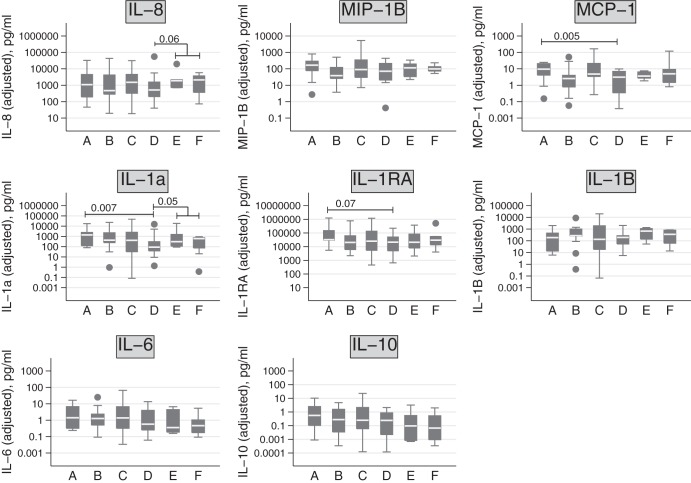
Fig 2.
Adjusted cytokine concentrations by group in study on rectal cytokines and C. trachomatis infection, Amsterdam, 2010 to 2011. Cytokine concentrations were adjusted by dividing by the Q(Alb). IL, interleukin; MIP, macrophage inflammatory protein; Q(Alb), ratio of albumin in supernatant to albumin in serum. The boxes represent the values from the 25 to 75 percentiles, the middle lines represent the medians, the vertical lines extend from the minimum to the maximum values, and the filled circles represent outliers.
RESULTS
Study population.
Of 961 MSM who were screened for eligibility, 288 were excluded because they reported not having had receptive anal sex in the 6 months preceding the study visit (see Fig. S1 in the supplemental material). Of the 673 eligible MSM, 91 (13.5%) refused to participate. Of the remaining MSM, 79 consecutive participants were selected for groups A to F. The numbers in each group do not total exactly 15, as too few men fit the criteria for some groups (e.g., E and F), and some men ultimately had different HIV and cART statuses than were initially reported (groups B and C). The participant characteristics are depicted in Table 1. The MPO, Alb, A2M, or cytokine concentrations could not be analyzed in the samples from three participants. Only five (6.3%) MSM had self-reported rectal symptoms, such as itching or discharge, and four of the five were diagnosed with rectal C. trachomatis infection.
Table 1.
Demographic characteristics of 79 MSM included in the study on rectal cytokines and Chlamydia trachomatis infection, Amsterdam, 2010 to 2011a
| Participant characteristics | Values by infection status, group, HIV status, and cART use |
|||||
|---|---|---|---|---|---|---|
|
C. trachomatis negative |
C. trachomatis positive |
|||||
| Group A, HIV− | Group B, HIV+ cART− | Group C, HIV+ cART+ | Group D, HIV− | Group E, HIV+ cART− | Group F, HIV+ cART+ | |
| No. | 15 | 13 | 19 | 15 | 8 | 9 |
| Demographics | ||||||
| Age (median [IQR]) (yr) | 40 (27–48) | 40 (33–46) | 46 (42–49) | 33 (29–43) | 36 (30–40) | 43 (29–52) |
| Ethnicity (no. [%]) | ||||||
| Dutch | 11 (73) | 11 (85) | 17 (89) | 11 (73) | 4 (50) | 7 (89) |
| Other | 4 (27) | 2 (15) | 2 (10) | 4 (27) | 4 (50) | 2 (11) |
| Anal symptoms (no. [%]) | ||||||
| No | 15 (100) | 13 (100) | 18 (95) | 14 (93) | 7 (88) | 7 (78) |
| Yes | 0 | 0 | 1 (5) | 1 (7) | 1 (13) | 2 (22) |
| HIV clinical data | ||||||
| HIV plasma viral load (median [IQR]) (copies/ml) | 1,930 (310–29,319)b | 20 (20–20) | 14,500 (10,000–254,000)c | 20 (20–20)d | ||
| HIV plasma viral load (no. [%]) | ||||||
| <50 copies/ml | 1 (8) | 19 (100) | 0 | 7 (78) | ||
| ≥50 copies/ml | 5 (39) | 0 | 3 (38) | 0 | ||
| Data missing | 7 (54) | 0 | 5 (63) | 2 (22) | ||
| CD4+ T cells (median [IQR]) (cells/mm3) | 735 (400–880)b | 534 (430–690) | 460 (440–940)c | 670 (430–700)d | ||
| CD4+ T cells (no. [%]) | ||||||
| <200 cells/mm3 | 0 | 1 (5) | 0 | 0 | ||
| ≥200 cells/mm3 | 6 (46) | 18 (95) | 3 (38) | 7 (78) | ||
| Data missing | 7 (54) | 0 | 5 (62) | 2 (22) | ||
MSM, men who have sex with men; cART, combination antiretroviral therapy; IQR, interquartile range.
Based on 6 participants with available test results.
Based on 3 participants with available test results.
Based on 7 participants with available test results.
Data on plasma HIV RNA and CD4 cell count were missing for participants who were newly diagnosed with HIV (n = 7) and for participants who declined to give permission for obtaining information about plasma HIV RNA and CD4 counts from the physician treating their HIV infection (n = 7). One HIV-infected participant had never received cART but nevertheless had an undetectable viral load.
Markers of inflammation and mucosal damage (A2M, albumin, RCE, and MPO).
The values for the Q(A2M), Q(Alb), RCE, and MPO concentrations for each group are shown graphically in Fig. 1 and in Table S2 in the supplemental material.
Markers of mucosal damage.
There were no significant differences in Q(A2M), Q(Alb), and RCE between the groups (Fig. 1). The relationship between Q(A2M) and Q(Alb) in sampled mucosal fluids is shown in Fig. S3 in the supplemental material. The correlation between Q(A2M) and Q(Alb) indicated no mucosal leakage, and thus adjustment by Q(Alb) for dilution of mucosal lining fluid was justified. Only one sample deviated markedly from the fitted line, which suggests that the mucosal barrier was reduced for this participant.
Markers of inflammation.
Figure 1 shows the MPO concentrations for each group. There were no significant differences in MPO concentrations between groups. Q(A2M) and RCE correlated with MPO (not shown) (Spearman's ρ = 0.6 and ρ = 0.5, respectively), which is suggestive of neutrophil activation causing mucosal damage.
Cytokine concentrations.
Concentrations of proinflammatory and anti-inflammatory cytokines are shown by group in Fig. 2, and differences between the groups with a P value of <0.1 are shown in box plots. Numerical data are shown in Table S2 in the supplemental material. Table S4 in the supplemental material shows an overview of the differences between adjusted and unadjusted cytokine concentrations. Although an adjustment of the cytokine concentrations for dilution resulted in lower P values, three out of the five unadjusted values already showed significant or near-significant differences.
Influence of C. trachomatis on cytokine concentrations.
Among the HIV-negative participants, the median concentrations of MCP-1, IL-1α, and IL-1RA were unexpectedly higher (at a P value of <0.1) in those without rectal C. trachomatis infection (group A) than in those with C. trachomatis infection (group D). In HIV-infected participants, there were no differences in the median concentrations of cytokines between those with and without rectal C. trachomatis infection.
Influences of HIV and cART on cytokine concentrations.
In participants with rectal C. trachomatis infection, HIV-negative MSM (group D) appeared to have lower median concentrations of IL-8 and IL-1α than participants with HIV (groups E and F) (unadjusted P = 0.09 and unadjusted P = 0.04, respectively). An adjustment of the concentrations for dilution resulted in similar differences (P = 0.06 and P = 0.05, respectively). There were no differences in median cytokine concentrations between HIV-infected participants with and without cART, irrespective of the presence or absence of C. trachomatis infection.
Asymptomatic versus symptomatic patients.
The median concentrations of IL-6 and IL-10 were higher in asymptomatic patients (n = 74) than in patients with symptoms (n = 5) (P = 0.04 and P = 0.01, respectively) (adjusted IL-6, 0.8 versus 0.2 pg/ml, and adjusted IL-10, 0.3 versus 0.01 pg/ml, respectively).
MPO and IL-8 concentrations.
Since IL-8 is a major chemokine for neutrophil recruitment and activation, we assessed the relationship between MPO and IL-8 concentrations in men without and with C. trachomatis infection (see Fig. S5 in the supplemental material), with different results. We found that increases in IL-8 corresponded with greater increases in MPO in MSM without C. trachomatis (groups A, B, and C) than in those with C. trachomatis infection (groups D, E, and F). In MSM with C. trachomatis infection, however, more neutrophil activation was seen at low IL-8 concentrations.
DISCUSSION
The most important finding in this study is that mucosal damage and neutrophil inflammation were not different between patients with or without C. trachomatis infection, HIV, and cART use. Interestingly, C. trachomatis infection was associated with suppressed cytokine (IL-8, MCP-1, IL-1α, and IL-1RA) expression in HIV-negative patients but not in those infected with HIV (IL-8 and IL-1α). C. trachomatis infection was also associated with an attenuated neutrophil response to IL-8, which may explain why there were no differences in inflammation and mucosal damage between the patient groups. To our knowledge, this is the first report of a study on rectal cytokine concentrations and rectal parameters of inflammation. We found that rectal C. trachomatis infection in MSM is not paralleled by enhanced inflammation, which may explain why rectal C. trachomatis infections are often asymptomatic.
Influences of C. trachomatis, HIV, and cART on mucosal damage and inflammation.
In vitro and in vivo studies have suggested that C. trachomatis infections in the urethra and vagina lead to an increased release of inflammatory mediators (13–15), and thus, we expected an increased local inflammatory response and mucosal damage in participants with rectal C. trachomatis infection. We used the Q(A2M), Q(Alb), and RCE [calculated by Q(A2M)/Q(Alb)] as markers of rectal mucosal damage and MPO concentration as a marker of the neutrophil inflammatory response. There were, however, no significant differences for these parameters, indicating no difference in the extent of mucosal damage between the patient groups. The correlation between Alb and A2M in rectal samples and the correlation between MPO and markers of mucosal damage underscore the genuineness of these findings. Since mechanical stress can lead to inflammation (24), local mechanical stress in the rectum caused by receptive anal sex may have overshadowed differences in the markers of mucosal damage and inflammation between the groups.
Influence of C. trachomatis, HIV, and cART on cytokine concentration.
C. trachomatis infection in HIV-infected MSM neither reduced nor increased cytokine concentrations. In HIV-negative MSM, however, we found reduced cytokine concentrations in those with C. trachomatis infection compared to those without C. trachomatis infection. These results are not due to the adjustment for dilution, since three out of the five unadjusted values already showed significant or near-significant differences. In previous studies, C. trachomatis-infected epithelial cells were found to release more IL-1α (12), and C. trachomatis infections of the urethra and cervix displayed increased IL-6, IL-8, and IL-10 concentrations (12–15, 25). It is probable that the microbial load of the gastrointestinal tract is increased more than those in the cervix and urethra (26), which may underlie observed differences in the inflammatory responses to C. trachomatis infection between the rectum and the cervix or urethra. An alternative explanation for the reduced cytokine concentrations in C. trachomatis-infected HIV-negative patients is that C. trachomatis infection induces indoleamine 2,3-dioxygenase (IDO) activity that inhibits immune responses (27). Since IDO expression is dependent on T-cell activation, a reduced T-cell response, as may occur in HIV-infected individuals, can prevent the induction of the inhibitory effect of IDO. The lack of difference in cytokine concentrations between HIV-infected MSM with or without C. trachomatis infection in our study supports that explanation.
In HIV-infected participants in our study with rectal C. trachomatis infection, the median cytokine concentrations did not differ between MSM who used cART and those who did not. This lack of difference is in contrast to the findings of a study in HIV-infected women without C. trachomatis infection (28) that showed that the concentrations of tumor necrosis factor alpha (TNF-α), IL-6, and IL-1β in cervical lavages decreased after initiation of cART. Our results may also be explained by the absence of a difference in immune status. In our participants with and without cART, all had relatively high concentrations of CD4+ T cells; the median circulating CD4+ T cell concentrations were 670 and 460 cells/mm3, respectively.
Asymptomatic versus symptomatic participants.
Most C. trachomatis-infected participants (88%) in our study were asymptomatic. In another study, increased concentrations of cytokines were detected in the urine of N. gonorrhoeae-infected men before the onset of symptoms, and these concentrations peaked simultaneously with the onset of symptoms (16). In our study, the lack of symptoms in those with C. trachomatis infection might be explained by the fact that cytokine concentrations did not differ in HIV-infected MSM with and without C. trachomatis infection and were reduced in HIV-negative MSM infected with C. trachomatis. Another explanation is that the median concentrations of IL-6 and IL-10 were higher in asymptomatic participants. Since IL-6 and IL-10 can have anti-inflammatory effects, increased concentrations of these cytokines may lead to a decreased inflammatory response and, therefore, fewer symptoms.
A limitation of this study is the small number of participants in each group. Nevertheless, the study still required the screening of nearly 1,000 men attending the STI clinic in order to include the 76 that were eventually included in the analysis. As a result, the power of the study was limited, which means that we might have missed important differences in the data. Since there were no data available on cytokine concentrations in rectal fluid samples, we performed no calculations for sample size. This was a pilot study, and we aimed to include 15 participants per group. In view of the dynamic range of most cytokines, strong effects on cytokine concentrations due to C. trachomatis, HIV, or both would have been detected. No corrections for multiple testing were done. Since patients not receiving cART had relatively high CD4+ T-cell counts, the contrast between HIV-infected participants receiving cART and those not receiving cART was small. This may explain why we did not find a difference in cytokine concentrations between these groups.
The adjustment for dilution of the samples by Q(Alb) might have resulted in overadjustment or underadjustment of the results. However, as there were no significant differences in the measured parameters of mucosal damage and the results were comparable without adjustment for dilution, overestimation or underestimation was not expected. We did not inquire about the most recent occurrence of receptive anal intercourse. Recent receptive anal sex might have caused local trauma, which might have affected local cytokine release, markers of inflammation, and mucosal leakage. It is possible that we did not find differences in the inflammatory markers between the groups because all the men may have had local trauma caused by receptive anal sex. Another limitation is that we were unable to distinguish between truly active C. trachomatis infection and the deposition of genetic material due to recent anal sexual activity. Bacterial load measurements might have helped to distinguish these two conditions, but some studies suggest that bacterial load measurements may be unable to make that distinction (29, 30); we did not have bacterial load measurements. Furthermore, we have no information about the estimated duration of the C. trachomatis infections, which might have influenced our results.
In conclusion, levels of mucosal damage and neutrophil inflammation did not differ between patients with or without C. trachomatis infection, HIV infection, and cART use. C. trachomatis infection was associated with suppressed cytokine (IL-8, MCP-1, IL-1α, and IL-1RA) expression in HIV-negative patients but not in those infected with HIV (IL-8 and IL-1α). C. trachomatis infection was also associated with an attenuated neutrophil response to IL-8. Thus, C. trachomatis infection in MSM is not paralleled by enhanced inflammation, which may explain why C. trachomatis infections are often asymptomatic. Further studies are required to clarify the exact process by which C. trachomatis escapes the mechanisms in the rectum that initiate inflammation and eradication of a pathogen.
Supplementary Material
ACKNOWLEDGMENTS
We thank all participants and colleagues of the STI clinic of the Health Service of Amsterdam, especially Anne Rutte for the inclusion of participants and sample handling and Martijn van Rooijen for data management. We thank our colleagues at the Public Health Laboratory (Health Service Amsterdam) for STI testing, Barbara Dierdorp, Tamara Dekker, and Marianne van de Pol (AMC, Departments of Experimental Immunology and Respiratory Medicine) for the determination of inflammatory parameters and cytokines, Ronald Geskus, Jan Prins, and Ferdinand Wit for critical review of the manuscript, and Sally Ebeling for editorial assistance.
The authors disclose no conflicts of interest.
H.D.V., D.P., S.G., R.L., M.H., T.H., and M.F.S.V.D.L. designed the study. M.H. and M.F.S.V.D.L. were responsible for statistical analysis. M.H., M.F.S.V.D.L., R.L., and S.G. wrote the paper. All authors assisted in revising the manuscript and have seen and approved the final submitted version of the manuscript.
This study was funded by grant no. 7115 0001 from the Netherlands Organisation for Health Research and Development (ZonMw).
The funding agency had no role in the study design, data collection, data analysis, data interpretation, or the writing of the paper.
Footnotes
Published ahead of print 31 July 2013
Supplemental material for this article may be found at http://dx.doi.org/10.1128/CVI.00763-12.
REFERENCES
- 1.Paavonen J, Eggert-Kruse W. 1999. Chlamydia trachomatis: impact on human reproduction. Hum. Reprod. Update 5:433–447 [DOI] [PubMed] [Google Scholar]
- 2.Heiligenberg M, Rijnders B, Schim van der Loeff MF, de Vries HJ, van der Meijden WI, Geerlings SE, Fennema HS, Prins M, Prins JM. 2012. High prevalence of sexually transmitted infections in HIV-infected men during routine outpatient visits in the Netherlands. Sex. Transm. Dis. 39:8–15 [DOI] [PubMed] [Google Scholar]
- 3.Kent CK, Chaw JK, Wong W, Liska S, Gibson S, Hubbard G, Klausner JD. 2005. Prevalence of rectal, urethral, and pharyngeal chlamydia and gonorrhea detected in 2 clinical settings among men who have sex with men: San Francisco, California, 2003. Clin. Infect. Dis. 41:67–74 [DOI] [PubMed] [Google Scholar]
- 4.Rieg G, Lewis RJ, Miller LG, Witt MD, Guerrero M, Daar ES. 2008. Asymptomatic sexually transmitted infections in HIV-infected men who have sex with men: prevalence, incidence, predictors, and screening strategies. AIDS Patient Care STDS 22:947–954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Annan NT, Sullivan AK, Nori A, Naydenova P, Alexander S, McKenna A, Azadian B, Mandalia S, Rossi M, Ward H, Nwokolo N. 2009. Rectal chlamydia–a reservoir of undiagnosed infection in men who have sex with men. Sex. Transm. Infect. 85:176–179 [DOI] [PubMed] [Google Scholar]
- 6.Cohen MS, Hoffman IF, Royce RA, Kazembe P, Dyer JR, Daly CC, Zimba D, Vernazza PL, Maida M, Fiscus SA, Eron JJ., Jr 1997. Reduction of concentration of HIV-1 in semen after treatment of urethritis: implications for prevention of sexual transmission of HIV-1. AIDSCAP Malawi Research Group. Lancet 349:1868–1873 [DOI] [PubMed] [Google Scholar]
- 7.Kaul R, Pettengell C, Sheth PM, Sunderji S, Biringer A, MacDonald K, Walmsley S, Rebbapragada A. 2008. The genital tract immune milieu: an important determinant of HIV susceptibility and secondary transmission. J. Reprod. Immunol. 77:32–40 [DOI] [PubMed] [Google Scholar]
- 8.Johnson LF, Lewis DA. 2008. The effect of genital tract infections on HIV-1 shedding in the genital tract: a systematic review and meta-analysis. Sex. Transm. Dis. 35:946–959 [DOI] [PubMed] [Google Scholar]
- 9.Rotchford K, Strum AW, Wilkinson D. 2000. Effect of coinfection with STDs and of STD treatment on HIV shedding in genital-tract secretions: systematic review and data synthesis. Sex. Transm. Dis. 27:243–248 [DOI] [PubMed] [Google Scholar]
- 10.Sadiq ST, Taylor S, Kaye S, Bennett J, Johnstone R, Byrne P, Copas AJ, Drake SM, Pillay D, Weller I. 2002. The effects of antiretroviral therapy on HIV-1 RNA loads in seminal plasma in HIV-positive patients with and without urethritis. AIDS 16:219–225 [DOI] [PubMed] [Google Scholar]
- 11.Hanada H, Ikeda-Dantsuji Y, Naito M, Nagayama A. 2003. Infection of human fibroblast-like synovial cells with Chlamydia trachomatis results in persistent infection and interleukin-6 production. Microb. Pathog. 34:57–63 [DOI] [PubMed] [Google Scholar]
- 12.Rasmussen SJ, Eckmann L, Quayle AJ, Shen L, Zhang YX, Anderson DJ, Fierer J, Stephens RS, Kagnoff MF. 1997. Secretion of proinflammatory cytokines by epithelial cells in response to Chlamydia infection suggests a central role for epithelial cells in chlamydial pathogenesis. J. Clin. Invest. 99:77–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vats V, Agrawal T, Salhan S, Mittal A. 2007. Primary and secondary immune responses of mucosal and peripheral lymphocytes during Chlamydia trachomatis infection. FEMS Immunol. Med. Microbiol. 49:280–287 [DOI] [PubMed] [Google Scholar]
- 14.Pate MS, Hedges SR, Sibley DA, Russell MW, Hook EW, III, Mestecky J. 2001. Urethral cytokine and immune responses in Chlamydia trachomatis-infected males. Infect. Immun. 69:7178–7181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guha D, Chatterjee R. 2009. Cytokine levels in HIV infected and uninfected Indian women: correlation with other STAs. Exp. Mol. Pathol. 86:65–68 [DOI] [PubMed] [Google Scholar]
- 16.Ramsey KH, Schneider H, Cross AS, Boslego JW, Hoover DL, Staley TL, Kuschner RA, Deal CD. 1995. Inflammatory cytokines produced in response to experimental human gonorrhea. J. Infect. Dis. 172:186–191 [DOI] [PubMed] [Google Scholar]
- 17.Alimonti JB, Koesters SA, Kimani J, Matu L, Wachihi C, Plummer FA, Fowke KR. 2005. CD4+ T cell responses in HIV-exposed seronegative women are qualitatively distinct from those in HIV-infected women. J. Infect. Dis. 191:20–24 [DOI] [PubMed] [Google Scholar]
- 18.Van Rooijen MS, van Leeuwen AP. 2010. Jaarverslag 2010. Soa-polikliniek, Amsterdam, The Netherlands [Google Scholar]
- 19.Heijman TL, Van der Bij AK, De Vries HJ, Van Leent EJ, Thiesbrummel HF, Fennema HS. 2007. Effectiveness of a risk-based visitor-prioritizing system at a sexually transmitted infection outpatient clinic. Sex. Transm. Dis. 34:508–512 [DOI] [PubMed] [Google Scholar]
- 20.Thompson AB, Mueller MB, Heires AJ, Bohling TL, Daughton D, Yancey SW, Sykes RS, Rennard SI. 1992. Aerosolized beclomethasone in chronic bronchitis. Improved pulmonary function and diminished airway inflammation. Am. Rev. Respir. Dis. 146:389–395 [DOI] [PubMed] [Google Scholar]
- 21.Out TA, Jansen HM, van Steenwijk RP, de Nooijer MJ, van de Graaf EA, Zuijderhoudt FM. 1987. ELISA of ceruloplasmin and alpha-2-macroglobulin in paired bronchoalveolar lavage fluid and serum samples. Clin. Chim. Acta 165:277–288 [DOI] [PubMed] [Google Scholar]
- 22.Schoonbrood DF, Lutter R, Habets FJ, Roos CM, Jansen HM, Out TA. 1994. Analysis of plasma-protein leakage and local secretion in sputum from patients with asthma and chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 150:1519–1527 [DOI] [PubMed] [Google Scholar]
- 23.Bresser P, Out TA, van Alphen L, Jansen HM, Lutter R. 2000. Airway inflammation in nonobstructive and obstructive chronic bronchitis with chronic Haemophilus influenzae airway infection. Comparison with noninfected patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 162:947–952 [DOI] [PubMed] [Google Scholar]
- 24.Wolthuis EK, Choi G, Dessing MC, Bresser P, Lutter R, Dzoljic M, van der Poll T, Vroom MB, Hollmann M, Schultz MJ. 2008. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology 108:46–54 [DOI] [PubMed] [Google Scholar]
- 25.Al-Mously N, Eley A. 2007. Interaction of Chlamydia trachomatis serovar E with male genital tract epithelium results in secretion of proinflammatory cytokines. J. Med. Microbiol. 56:1025–1032 [DOI] [PubMed] [Google Scholar]
- 26.Vossenkämper A, Macdonald TT, Marchès O. 2011. Always one step ahead: how pathogenic bacteria use the type III secretion system to manipulate the intestinal mucosal immune system. J. Inflamm. (Lond.) 8:11. 10.1186/1476-9255-8-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ibana JA, Belland RJ, Zea AH, Schust DJ, Nagamatsu T, AbdelRahman YM, Tate DJ, Beatty WL, Aiyar AA, Quayle AJ. 2011. Inhibition of indoleamine 2,3-dioxygenase activity by levo-1-methyl tryptophan blocks gamma interferon-induced Chlamydia trachomatis persistence in human epithelial cells. Infect. Immun. 79:4425–4437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sachdeva RK, Wanchu A, Bagga R, Malla N, Sharma M. 2010. Effect of non-nucleoside reverse transcriptase inhibitors on cytokine, chemokine, and immunoglobulin profiles in serum and genital secretions of HIV-infected women. J. Interferon Cytokine Res. 30:299–310 [DOI] [PubMed] [Google Scholar]
- 29.Wiggins R, Graf S, Low N, Horner PJ, Chlamydia Screening Studies (ClaSS) Study Group 2009. Real-time quantitative PCR to determine chlamydial load in men and women in a community setting. J. Clin. Microbiol. 47:1824–1829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gomes JP, Borrego MJ, Atik B, Santo I, Azevedo J, Brito de Sá A, Nogueira P, Dean D. 2006. Correlating Chlamydia trachomatis infectious load with urogenital ecological success and disease pathogenesis. Microbes Infect. 8:16–26 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.