Abstract
Background
Health risks such as tobacco use, excessive alcohol consumption, and unhealthy body weight can contribute to the development of chronic health problems.
Objectives
Estimate the associations of tobacco use, excessive alcohol consumption, and obesity with health care expenditure and chronic diseases among South Africans on a comprehensive medical scheme.
Methods
Analyze health survey and medical claims data for a cross-sectional sample of 70 000 South Africans in 2010.
Results
Moderately obese individuals with body mass index (BMI) between 30 and 35 averaged R 2 300 or 11% higher medical expenditure than never-smokers with a BMI under 30. This increase is comparable to being a current or past smoker (expenditure increase by R 2 600 or 13%). Severely obese individuals (BMI over 35), however, have increased health care costs by R 4 400 (23% increase). This exceeds the difference between a 40 and a 50 year old (increase of R 3 200). Being overweight or consuming excessive alcohol was not significantly associated with medical expenditures. Absolute and relative excess expenditures associated with these health risks are higher among older individuals. In the 54–69 age group, estimated additional expenses were R 6 200 for smoking (20% increase over never-smokers with BMI under 30), R 6 600 for moderate obesity (21%), and R 15 800 for severe obesity (51% increase). Overweight or heavy drinking were not statistically significant.
Conclusion
Obesity and tobacco use are associated with significantly increased health care expenditure. Severe obesity doubles these excess costs.
Introduction
Health risks such as obesity, smoking, and excessive alcohol intake are common amongst South African and much of the disease burden can be attributed to these risk factors.[1] These risk factors are potentially modifiable, through smoking cessation programs, taxation and regulation of tobacco and alcohol products, or programs that encourage healthy diets or increase physical activity. The prevalence of chronic diseases, including diabetes and certain cancers, has increased in South Africa and will continue to rise unless there are active countermeasures.[2–4] These chronic health conditions, in turn, are thought to be drivers of increasing healthcare expenditures.
Understanding the relative contributions of risk factors to poor health allows better targeting of health promotion programs to make prevention efforts more cost-effective. Health promotion activities traditionally focused on smoking and excessive alcohol intake, whereas overweight and obesity have become prominent in recent policy debates. Obesity rates are increasing rapidly among South African adolescents, setting the stage for an increase in obesity-related chronic conditions over the next decades.[5]
This paper compares the associations between obesity, smoking, excessive alcohol intake and health care utilization and the prevalence of chronic conditions among adult South Africans on a private medical scheme. The privately insured population accounts for about 17% of South African adults, has a higher income, and has greater access to medical care than uninsured South Africans.
While obesity and overweight are sometimes grouped together, the health and healthcare consequences differ dramatically. US studies have shown little or no effect of overweight on health care cost or mortality, yet large effects of higher levels of obesity. [6] [7] Hence, we distinguish overweight, moderate, and severe obesity in this analysis.
Methods
The data are drawn from members of a comprehensive Discovery Health medical plan who were also enrolled in the Vitality health promotion program. We use data from an online health risk assessment (HRA) fielded in 2010 and health care costs data for 2010. The HRA collects data on selected health risks, including smoking, alcohol consumption, and body height and weight, and is fielded as part of the health promotion program (similar data are not available for plan member not enrolled in Vitality). The assessment has a response rate of about 35%. Survey responses completed by adults aged 18 and older in 2010 were merged to their medical claims of the same year. The total population is 74 504, and half of them are female.1 651 women who reported being pregnant were excluded. In addition, 3 473 respondents provided no response for one or more key variables (i.e., smoking status, alcohol consumption, and body height or weight) and were excluded in the multivariate analysis, resulting in a total of analytic sample of 69 380. A separate analysis was conducted for individuals aged 54–69 (8 765 observations or 13% of total sample). The Human Subjects Protection Committee at RAND Corporation reviewed and approved the research plan.
The dependent variables are health care expenditure in 2010 (both total expenditure and expenditure by inpatient and outpatient) and a count of the presence of 17 common chronic conditions derived from diagnoses on claims (including hypertension, hypercholesterolemia, liver disease, pulmonary disease, diabetes).
The main explanatory variables are body-mass index (BMI, calculated as weight in kilograms divided by height in meters squared) and its standard categories: underweight (BMI < 18.5), normal weight (18.5 ≤ BMI < 25), overweight (25 ≤ BMI < 30), moderate obese (30 ≤ BMI < 35), and severe obese (BMI ≥ 35); excessive alcohol intake is defined as having three or more drinks per day; and being current or past regular smoker (grouped together). There is no information on lifetime duration of smoking or weight history. Other explanatory variables include any alcohol consumption, age as a linear spline with knots at age 30, 40, 50, and 60, and gender.
BMI was calculated from self-reported height and weight. Self-report on average understates weight (more so for women) and overstates height (more so for men).[8] The underreporting of weight increases with weight, and prevalence at the same cutoff points are therefore lower than if BMI were calculated from independent measurement. Reporting accuracy in this South African population is unknown, but in the US, using the 2007–2008 National Health and Nutrition Examination Survey, an objective cutoff point of 30 would correspond to a cutoff point of 28.7 for men and 28.4 for women.[9] We only use this adjustment for comparison purposes as its applicability for populations outside the US is unclear. Self-report biases are not limited to height or weight, as smoking or alcohol consumption tends to be underreported as well.
We illustrate the bivariate association between BMI and healthcare expenditure by plotting a semi-parametric local polynomial estimate of expenditure on BMI. These curves are only drawn for BMIs between 18.5 and 35 because there are few observations in the underweight or severe obesity category for local estimates. In the multivariate analyses, we conduct ordinary least squares (OLS) of raw expenditure on explanatory variables using the full dataset (this model estimates adjusted averages for each group instead of local estimates at every BMI point). OLS provides unbiased estimates and avoids statistical complications associated with retransformation (e.g. estimates of log-models).[10] Multi-part models may improve estimation efficiency,[11] but our sample is large enough to provide precise estimates even in absence of multi-part models. All statistical analyses are conducted in Stata SE 12.1 (StataCorp, College Station, TX).
Sensitivity analyses are performed to assess the robustness of the qualitative conclusions across sample classifications and alternative model specifications. We estimate separate models for different age groups, men only, and women only. We also repeat the analyses on members on different (less comprehensive) health plans and use alternative statistical models (e.g. two-part model and log transformation of expenditure).
Results
Table 1 reports descriptive sample statistics from men and women. The average BMI in 2010 based on self-report height and weight was 27.1 for adult men and 25.6 for adult women, corresponding to an obesity prevalence of 24.4% and 18%, respectively. Just over 6% of men and women are severely obese (BMI of 35 or more). Underweight (BMI < 18.5, results not shown) was rare among women and extremely rare among men (only 148 men). About one third of the sample is a current or prior regular smoker and a majority drinks some alcohol. However, having 3 drinks or more daily is uncommon.
Table 1.
Descriptive Statistics of the Study Sample
| Men (N = 35 880) |
Women (N = 35 322) |
|
|---|---|---|
| Age | 41.4 (11.2) | 39.7 (10.8) |
| Body mass index | 27.7 (4.64) | 25.6 (5.6) |
| Overweight (BMI ≥ 25) | ||
| Obesity (BMI ≥ 30) | 24.4 (42.9) | 18.0 (38.4) |
| Severe obesity (BMI ≥ 35) | 6.4 (24.6) | 6.5 (24.8) |
| Current or past regular smoker | 39.3 (48.8) | 31.9 (46.6) |
| Any alcohol consumption | 75.9 (42.7) | 62.0 (48.5) |
| Heavy drinking (3 or more drinks per day) | 1.1 (10.6) | 0.3 (5.4) |
| Total healthcare expenditure (rand) | 18 605 (43 557) | 22 845 (37 288) |
| Outpatient expenditure (rand) | 12 768 (23 051) | 15 994 (22 769) |
| Inpatient expenditure (rand) | 5 837 (31 974) | 6 851 (24 114) |
Notes: The study sample consists of Discovery Health comprehensive plan members who completed a health risk assessment survey in 2010. Standard deviations of arithmetic means are in parentheses. All differences between male and female are statistically significant at p < 0.01 using two-sample t-test.
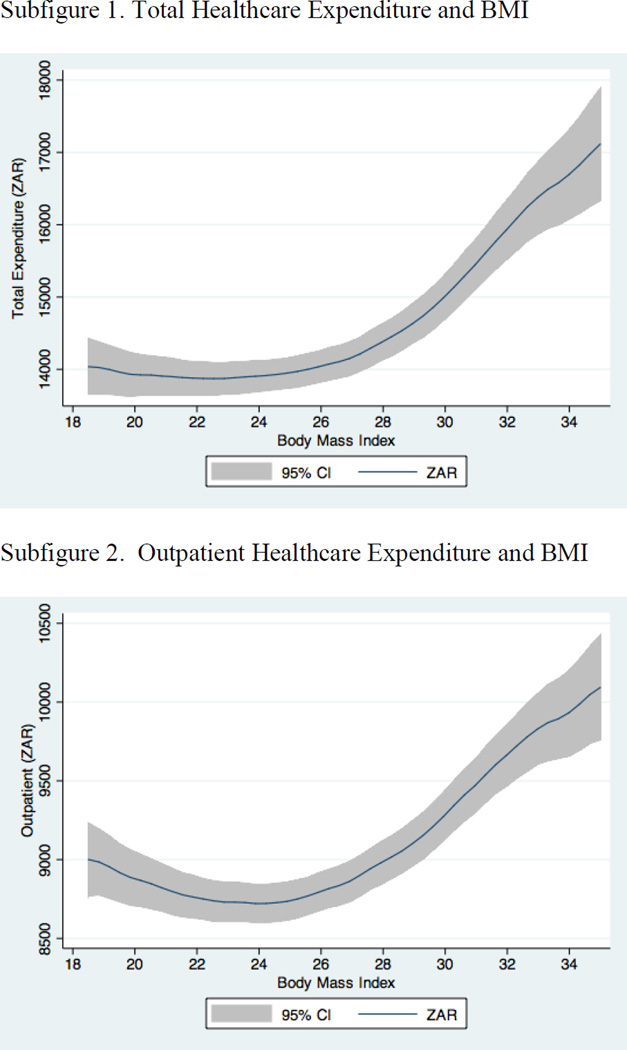
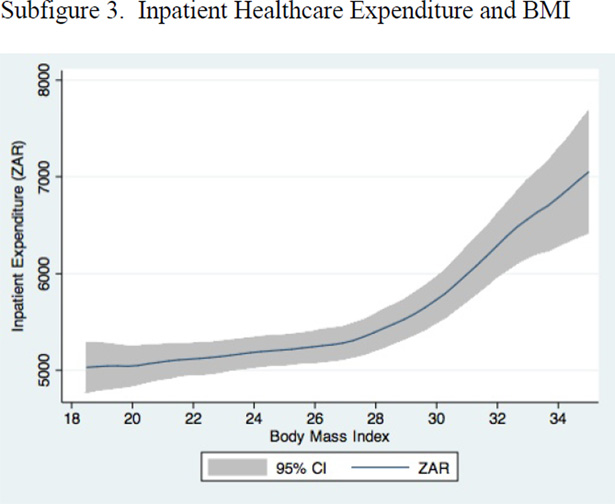
Figure 1 illustrates the association between BMI and healthcare expenditure in three parts: total expenditure, outpatient expenditure only, and inpatient expenditure only. A small reduction in total expenditure is present in the low BMI range and the reduction seems more pronounced for outpatient expenditure, which reaches its minimum in BMIs between 24 and 25. A constant rise in expenditure is observed for BMIs greater than 25, and this increasing trend is accelerated for BMIs 30 or more for inpatient costs. We exclude BMIs in the range of underweight and severe obesity due to insufficient sample size for this graphical display even for the full data set.
Figure 1.
Total, Outpatient, and Inpatient Healthcare Expenditure in 2010 and Body Mass Index (BMI)
Notes: The bivariate associations between BMI and healthcare expenditure are eatimated using semi-parametric local polynomial regressions. We only draw this curve for BMIs between 18.5 and 35 because there are few observations in the underweight or severe obesity category for local estimates.
Table 2 reports results from multivariate analyses for each BMI group and for three other risk factors: aging, current or past smoking, and excessive alcohol intake (3 or more drinks per day). Expenditures in people aged 50 were R 3 204 more than in people aged 40, with almost all the difference due to additional outpatient services with no significant effect on inpatient costs. A 10 year age difference also predicted an additional.27 chronic medical problems (or 27 new conditions among 100 people). Severe obesity has an even larger effect on medical expenditures and health care costs: an increase of R4 425 per person, split between inpatient and outpatient, and an incidence of an additional 70 chronic conditions per 100 severely obese individuals that would not occur among otherwise similar individuals in the normal weight range (row 2). With total expenditure averaging R 20 000 for never-smokers with a BMI under 30, a R4 425 increase corresponds to a 22 percent increase. The effect of moderate obesity (row 3) was only half of that, an increase of R 2 238 or 11 percent. Overweight had no effect on health care expenditures compared to normal weight (row 4). Smoking (both current and previous, row 5) had an effect on costs that was similar to moderate obesity (R 2 596, 13% increase), but it had a smaller effect on chronic conditions. Heavy drinkers use fewer medical services despite having more chronic conditions (row 6).
Table 2.
Estimated Change in Healthcare Expenditure and Chronic Conditions Associated with Specific Behavioral Risk Factors – All Ages
| Total expenditure |
Outpatient expenditure |
Inpatient expenditure |
Count of chronic conditions (maximum 17) |
|
|---|---|---|---|---|
| Aging 10 years from 40 to 50 | 3 204** (594) | 3 269** (335) | −60 (420) | 0.27** (0.0018) |
| Overweight (25 ≤ BMI < 30) | 140 (360) | −220 (203) | 360 (252) | 0.18** (0.01) |
| Obese (30 ≤ BMI < 35) | 2 238** (474) | 537* (267) | 1 700** (335) | 0.41** (0.01) |
| Severe obesity (BMI ≥ 35) | 4 425** (647) | 1 909** (364) | 2 515** (457) | 0.70** (0.02) |
| Current or past regular smoker | 2 596** (322) | 1 301** (182) | 1 294** (227) | 0.17** (0.01) |
| Heavy drinking | −2 022 (1 804) | −1 156 (1 016) | −865 (1 274) | 0.34** (0.05) |
Notes: The study sample (N = 69 380) consists of Discovery Health comprehensive plan members who completed a health risk assessment survey in 2010. Reference group for body weight is 18.5 ≤ BMI < 25.. Other control variables include a spline function to capture nonlinear age effects, and indicator variables for male, any alcohol consumption, and underweight.
p < 0.05;
p < 0.001.
Table 3 repeats the analysis for individuals 54–69 years old to parallel a US study.[6] This age group accounts for 13% of our full data set, resulting in larger standard errors. With total expenditure averaging around R 31 000 for never-smokers with a BMI under 30 in this age group in 2010, the estimated excess costs of moderate obesity (R 6 639) correspond to a 21% increase and for severe obesity (R 15 835) to a 51% increase. Smoking is associated with excess costs of R 6 195, a 20% increase. Overweight has no significant association with health care costs. There were too few individuals with heavy alcohol intake to provide meaningful estimates, so we do not show results for this variable.
Table 3.
Age Group 54–69: Estimated Change in Healthcare Expenditure and Chronic Conditions
| Total expenditure |
Outpatient expenditure |
Inpatient expenditure |
Count of chronic conditions (maximum 17) |
|
|---|---|---|---|---|
| Overweight (25 ≤ BMI < 30) | 1 143 (1 521) | 651 (737) | 491 (1 175) | 0.36** (0.04) |
| Obese (30 ≤ BMI < 35) | 6 639** (1 972) | 1 516 (955) | 5 122** (1 522) | 0.65** (0.05) |
| Severe obesity (BMI ≥ 35) | 15 835** (2 805) | 6 946** (1 360) | 8 889** (2 166) | 0.97** (0.07) |
| Current or past regular smoker | 6 195** (1 340) | 3 107** (650) | 3 087** (1 035) | 0.24** (0.03) |
Notes: The study sample (N =8765) consists of Discovery Health comprehensive plan members who completed a health risk assessment survey in 2010 and were between 54 and 69 years old. Reference group for body weight is 18.5 ≤ BMI < 25. Other control variables include a spline function to capture nonlinear age effects, and indicator variables for male, any alcohol consumption, and underweight.
p < 0.05;
p < 0.001.
The sensitivity analyses find the qualitative results (not shown) to be fairly consistent across different subgroups (by age, gender, and type of health plan) and model specifications (OLS vs. two-part model), except for the underweight individuals and individuals under 30. Moderate obesity is associated with an increase in healthcare expenditure by 10– 24%, severe obesity 22–51%, and smoking 8–20%. The exceptions are individuals under the age of 30: for them, there is no significant association between obesity, smoking, or excessive alcohol consumption and health care expenditures. Dependent upon sample stratification, the healthcare expenditure among the underweight population ranges from small reduction to large increase (the latter always occurs among male under 40 years old). Because average health care costs increase with age as well, the absolute magnitude of the excess costs of poor health habits are higher for older individuals (and correspondingly smaller for younger individuals) than the population effects in Table 2. Moreover, the relative increase is largest among people in their 50s and 60s.
Discussion
This paper is the first to provide data on the relationship between levels of overweight and obesity, smoking, and excessive alcohol intake and medical expenditures among South Africans on a comprehensive medical scheme. Across the adult population, obesity has a substantial effect on health care expenditure and there are large differences in expenditure by degree of obesity. Compared to individuals in the normal or overweight range, severely obese individuals used 23% more medical services and moderately obese individuals used 11% more, which is similar to the group of current or past smokers.
The results are based on cross-sectional observational data and self-report for health risks. So the results do not show the causal flow from risks to costs, only association. Reverse causality, i.e. health causing risk factors, is less of an issue for obesity or smoking than it would be for something like physical activity because injuries and illness are a direct cause of reduced activity levels, but will exist for some individuals (e.g. weight gain caused by certain medications). Underweight can be a consequence of severe illness, and often is a late stage of terminal conditions, which may be a reason of why our estimates for underweight are very sensitive to sample selection.
Physical activity and diet are unmeasured variable correlated with obesity, although they can have independent health effects. Empirically, it is difficult to disentangle these factors because activity and diet are very hard to measure and we have no meaningful measures for our population. Physical activity and diet are the upstream health behaviors that can be targeted, whereas BMI is an outcome of energy balance and not directly a modifiable health behavior. The study uses self-reported height and weight, which generally underestimate BMI. This means that our prevalence of severe obesity is lower than in objectively measured data, whereas estimated effects are larger than if objectively measured BMI were used because “true” BMI is higher.
The health consequences of poor health habits are not instantaneous, are likely to depend on total exposure duration, and may interact with aging. The survey does not capture total exposure, e.g. years of smoking or years of obesity. Thus the estimated cost consequences of health behaviors are population averages and likely to be smaller for individuals who are younger or have been exposed to a health risk for a shorter duration and higher for older individuals and longer exposures. While no measures of exposure (e.g. years of smoking, years of obesity) are available, we can estimate models stratified by age. When we restrict the analysis to individuals between 54 and 69 to parallel the US study by Andreyeva et al.[6], moderate obesity increases expenditures by 21% for this age group (up from 11% for the full population), severe obesity by 51% (up from 23%), and smoking by 20% (up from 13%). This is comparable to the US estimates for this age group, where moderate obesity was associate with an increase of 25% and severe obesity with an increase of 50% or more.[6] In a meta-analysis of mortality studies, overweight was not associated with increased mortality rates, whereas higher levels of obesity were associated with increased mortality.[It is expected that the association between obesity and health care costs increases in middle age because this is the time when chronic conditions caused by poor health behaviors manifest. That also means that the high rates of obesity among younger cohorts will only show their adverse impacts in the future.
The absence of a significant effect of excessive alcohol consumption may seem surprising since many believe that alcohol abuse has a large effect on health care costs, but is also consistent with evidence from other countries.[12–13] There are important outcomes outside the scope of this analysis that could provide a different ranking. Smoking may still account for more premature deaths and alcohol abuse is likely to account for more externalities (e.g. drunk driving accidents).
The results are based on defined sample of health plan members who complete a health assessment and may therefore not be generalizable to all South Africans in medical plans (and obviously do not apply to the majority of South Africans that do not receive private health care). About one third of the sample is a current or past smoker and only 12 percent admit to current smoking, with only a 1 percentage point difference between men and women. In contrast, the 2003 South Africa Demographic and Health Survey[14] reported current daily smoking rates of more than 30 percent for men. For South Africa, the social impact of smoking would be larger than in our sample due to the high prevalence among the general South African population.
The 2003 South Africa Demographic and Health Survey objectively measured height and weight measures and reported an average BMI of 24.0 for men and 27.2 for women, corresponding to obesity rates of 14 and 30 percent. Our data uses self-reported height and weight, which is not directly comparable. Trying to adjust for the difference using alternative cutoff points based on US data, we estimate that 34 percent of men and 24 percent of women in our study would be classified as obese based on objective measurements. This is more than double the rate for men in the 2003 survey, but less for women, indicating substantial differences in obesity prevalence by gender between participants in medical schemes and uninsured South Africans.
We can also compare our data to the United States Behavioral Risk Factor Surveillance System (BRFSS), a national telephone survey that also uses self-reported height and weight to calculate BMI. For American men in 2010, the BRFSS gives a mean BMI of 27.9, corresponding to an obesity rate of 28.0 percent. This is not very different from the average BMI of 27.7 and an obesity rate of 24.4 percent for South African men in our sample. For American women in 2010, the BRFSS gives an average BMI of 27.1 and an obesity rate of 26.5 percent, compared to an average BMI of 25.6 and an obesity rate of 18 percent in our South African sample of women.
For all health risk, whether smoking, problem drinking, or obesity, a time lag intervenes between obesity and development of chronic health problems. In the United States, the largest declines in smoking rates happened between 1960 and 1980, whereas the largest increase in obesity has occurred since 1980. In South Africa, the full long-run consequences of increased obesity rates at the aggregate level are probably not yet visible.
Acknowledgments
Financial support was provided by the National Cancer Institute (Grant No. R21CA161287) and the National Institute of Child Health & Human Development (Grant No. R21HD071568). We thank Derek Yach for comments on an earlier draft.
Contributor Information
Roland Sturm, RAND Corporation.
Ruopeng An, University of Illinois at Urban Champaign.
Josiase Maroba, Discovery Vitality, Johannesburg, South Africa.
Deepak Patel, Discovery Vitality, Johannesburg, South Africa.
REFERENCES
- 1.Mayosi BM, Flisher AJ, Lalloo UG, et al. The burden of non-communicable diseases in South Africa. Lancet. 2009;374(9693):934–947. doi: 10.1016/S0140-6736(09)61087-4. [ http://dx.doi.org/10.1016%2FS0140-6736%2809%2961087-4] [PMID:19709736] [DOI] [PubMed] [Google Scholar]
- 2.Kengne AP, Echouffo-Tcheugui JB, Sobngwi E, et al. New insights on diabetes mellitus and obesity in Africa-Part 1: prevalence, pathogenesis and comorbidities. [accessed on June 5, 2013];Heart. 2013 doi: 10.1136/heartjnl-2012-303316. Available at: http://heart.bmj.com/content/early/2013/05/16/heartjnl-2012-303316.long. [ http://dx.doi.org/10.1136%2Fheartjnl-2012-303316] [DOI] [PubMed] [Google Scholar]
- 3.Peer N, Steyn K, Lombard C, et al. Rising diabetes prevalence among urban-dwelling black South Africans. PLoS One. 2012;7(9):e43336. doi: 10.1371/journal.pone.0043336. [ http://dx.doi.org/10.1371%2Fjournal.pone.0043336] [PMID: 22962583] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peer N, Bradshaw D, Laubscher R, et al. Urban-rural and gender differences in tobacco and alcohol use, diet and physical activity among young black South Africans between 1998 and 2003. Glob Health Action. 2013;6:19216. doi: 10.3402/gha.v6i0.19216. [ http://dx.doi.org/10.3402%2Fgha.v6i0.19216] [PMID: 23364100] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reddy SP, Resnicow K, James S, et al. Rapid increases in overweight and obesity among South African adolescents: comparison of data from the South African National Youth Risk Behaviour Survey in 2002 and 2008. Am J Public Health. 2012;102(2):262–268. doi: 10.2105/AJPH.2011.300222. [ http://dx.doi.org/10.2105%2FAJPH.2011.300222] [PMID: 21940919] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andreyeva T, Sturm R, Ringel JS. Moderate and severe obesity have large differences in health care costs. Obes Res. 2004;12(12):1936–1943. doi: 10.1038/oby.2004.243. [ http://dx.doi.org/10.1038%2Foby.2004.243] [PMID: 15687394] [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Kit BK, Orpana H, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [ http://dx.doi.org/10.1001%2Fjama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hattori A, Sturm R. The obesity epidemic and changes in self-report biases in BMI. Obesity. 2013;21(4):856–860. doi: 10.1002/oby.20313. [ http://dx.doi.org/10.1002%2Foby.20313] [PMID: 23712990] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. [accessed on June 5, 2013];Int J Obes. 2012 doi: 10.1038/ijo.2012.159. Available at: http://www.nature.com/ijo/journal/vaop/ncurrent/full/ijo2012159a.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manning WG, Mullahy J. Estimating log models: to transform or not to transform. J Health Econ. 2001;20(4):461–494. doi: 10.1016/s0167-6296(01)00086-8. [ http://dx.doi.org/10.1016%2FS0167-6296%2801%2900086-8] [PMID: 11469231] [DOI] [PubMed] [Google Scholar]
- 11.Duan N, Manning WG, Morris CN, et al. A comparison of alternative models for the demand for medical care. J Bus Econ Stat. 1983;1(2):115–126. [ http://dx.doi.org/10.2307%2F1391852] [Google Scholar]
- 12.Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff. 2002;21(2):245–253. doi: 10.1377/hlthaff.21.2.245. [ http://dx.doi.org/10.1377%2Fhlthaff.21.2.245] [DOI] [PubMed] [Google Scholar]
- 13.Polen MR, Green CA, Freeborn DK, et al. Drinking patterns, health care utilization, and costs among HMO primary care patients. J Behav Health Serv Res. 2001;28(4):378–399. doi: 10.1007/BF02287770. [ http://dx.doi.org/10.1007%2FBF02287770] [PMID: 11732242] [DOI] [PubMed] [Google Scholar]
- 14.Medical Research Council. [accessed on June 5, 2013];2003 South Africa Demographic and Health Survey. Available at: http://www.info.gov.za/view/DownloadFileAction?id=90143.