Abstract
In aquatic birds, influenza A viruses mainly replicate in the intestinal tract without significantly affecting the health of the host, but in mammals, they replicate in the respiratory tract and often cause disease. Occasionally, influenza viruses have been detected in stool samples of hospitalized patients and in rectal swabs of naturally or experimentally infected mammals. In this study, we compared the biological and molecular differences among four wild-type avian H1N1 influenza viruses and their corresponding fecal and lung isolates in DBA/2J and BALB/cJ mice. All fecal and lung isolates were more pathogenic than the original wild-type viruses, when inoculated into mice of both strains. The increased virulence was associated with the acquisition of genetic mutations. Most of the novel genotypes emerged as PB2E627K, HAF128V, HAF454L, or HAH300P variations, and double mutations frequently occurred in the same isolate. However, influenza virus strain- and host-specific differences were also observed in terms of selected variants. The avian H1N1 virus of shorebird origin appeared to be unique in its ability to rapidly adapt to BALB/cJ mice via the fecal route, compared to the adaptability of the H1N1 virus of mallard origin. Furthermore, a bimodal distribution in fecal shedding was observed in mice infected with the fecal isolates, while a normal distribution was observed after infection with the lung isolates or wild-type virus. Fecal isolates contained HA mutations that increased the activation pH of the HA protein. We conclude that influenza virus variants that emerge in fecal isolates in mammals might influence viral transmission, adaptation to mammals, and viral ecology or evolution.
INTRODUCTION
Influenza A viruses are naturally found in wild aquatic birds, mainly in the orders Anseriformes (e.g., ducks, geese, and swans) and Charadriiformes (e.g., gulls and shorebirds), preferentially replicating in the epithelial lining of the intestines and causing no apparent disease (1–3). Virus is shed via feces, contaminating open water sources (e.g., ponds, lakes) and the surrounding environment, and is transmitted orally to infect naive birds. Influenza viruses that cause seasonal or pandemic influenza in humans and epidemics in pigs and horses are ultimately derived from the aquatic bird reservoir (1) and replicate primarily in the upper and lower respiratory tract. However, the literature contains several reports of fecal shedding of influenza viruses from mammals after natural or experimental infection with influenza viruses of avian, swine, equine, or human origin (4–22).
Although the main route of influenza virus infection is respiratory in mammals, gastrointestinal manifestations can occur, especially during the early stages of the disease. During the 2009 H1N1 pandemic, gastrointestinal symptoms were observed in 25% of the hospitalized patients (23). In a recent case-control study, viral RNA for influenza B virus, 2009 pandemic H1N1 virus, and seasonal H3N2 virus was detected in stool samples from adult patients with diarrhea (16). Furthermore, fecal shedding has been detected by viral RNA analysis of hospitalized adult and pediatric patients (5, 7) and high-risk influenza patients of various ages (4 to 92 years) (4) who were infected with seasonal influenza A viruses (H1N1 or H3N2 subtypes) or influenza B viruses. Infectious virus was isolated from stool samples from two patients with seasonal H1N1 infections; one was an adult patient (5), and the other was an immunocompromised pediatric patient with long-term viral shedding (>2 months) (10). Viral RNA from pandemic H1N1 has been detected in stool samples (11, 12), and the infectious virus was isolated in rare cases (11). In patients with highly pathogenic H5N1 influenza, viral RNA was frequently detected in rectal swab/stool samples (9, 17, 18). Virus recovery by cell culture has also been reported (6, 17, 18). In addition to gastrointestinal symptoms, hematuria and viremia were observed in association with renal pathology as a consequence of infection with seasonal influenza virus or the 2009 pandemic H1N1 virus (24–26).
Viral RNA and infectious viruses have also been detected in intestines, feces, and rectal swabs of mammals (i.e., mice, ferrets, cats, and pigs) experimentally infected with influenza A viruses of various origins. Infection of ferrets with human viruses (H1N1, H3N2, H5N1, H7N7, H7N3, and H7N2) (14, 15, 19, 20) or viruses of swine or equine origin (8) or avian origin (8, 21) results in moderate viral titers in rectal swabs and intestines, regardless of the route of inoculation. In pigs, human influenza A virus (H3N2) was found in the feces (8) and viral RNA for swine H1N1 virus was detected in the intestines (27), though other human (H5N1) and swine (H3N2 and H1N1) viruses were not detected (28). The 2009 pandemic H1N1 virus has been isolated in the rectal swabs and intestines of experimentally infected cats, though no lesions were observed (22). Avian influenza A viruses were found at moderate titers in the feces and intestines of mice (21) but not in those of pigs (27, 28). Although avian influenza A viruses replicate well in the intestines of aquatic bird hosts, human and swine influenza viruses could not be detected in the intestinal tracts of ducks (29). Thus, the presence of influenza A viruses in the fecal material or intestinal tract appears to be not only subtype specific but also host specific.
Despite multiple reports of the detection of viral RNA and infectious influenza viruses in the feces of naturally and experimentally infected mammals, the source of virus in feces is still not clear. We do not know whether some strains of influenza A viruses can replicate in the intestinal tract of mammals, originate from a secondary replication site, or simply transfer from the respiratory tract to the digestive tract by the mucociliary escalator when the virus is swallowed. Regardless of the site of replication, the virus reaches the intestinal tract of mammals and is shed in the feces. To date, the molecular and biological features of influenza viruses in feces and the gastrointestinal tract have not been studied. We do not know the duration of fecal shedding, the amount of infectious particles in feces during influenza virus infection, or the potential that these viruses have to be transmitted via the fecal-oral route and cause infections in mammals. Additionally, we do not know whether fecal shedding serves as a tool for the selection of novel variants in mammals or plays any role in viral evolution. Therefore, it is important to address these questions to understand the biology of influenza viruses thoroughly.
In our previous study (21), we detected infectious viruses in the feces of DBA/2J mice and BALB/cJ mice and in the rectal swabs of ferrets infected with North American avian H1N1 influenza A viruses. In this study, we compared the molecular and biological properties of lung and fecal isolates to those of the original wild-type viruses. We examined the fecal isolates recovered from infected mice to determine whether they can cause respiratory infection in mammals upon intranasal inoculation and whether the viruses shed in feces are novel variants of the original wild-type virus selected during respiratory infection. We also report on how the genetic variants that emerged via different routes (feces versus lung) affect the viral shedding pattern in feces and pathogenesis during the subsequent round of infection.
MATERIALS AND METHODS
Ethics statement.
All animal experiments were conducted in an animal biosafety level 2+ (biosafety level 2 with enhanced biocontainment for pandemic H1N1 influenza A virus) facility at St. Jude Children's Research Hospital (St. Jude). Studies were done in compliance with the policies of the National Institutes of Health and the Animal Welfare Act and with the approval of the St. Jude Institutional Animal Care and Use Committee.
Animals.
Six-week-old female DBA/2J or BALB/cJ mice were purchased from the Jackson Laboratories (Bar Harbor, ME). Upon arrival, all mice were acclimatized in the Animal Resources Center at St. Jude for 1 week before infection. They were given food and water ad libitum.
Pathogenicity of wild-type viruses and passage isolates.
Four avian H1N1 viruses (A/mallard/MN/AI07-3136/2007 [md/MN/07a], A/mallard/MN/AI07-3100/2007 [md/MN/07b], A/shorebird/DE/300/2009 [sb/DE/09], and A/mallard/ALB/88/2004 [md/ALB/04]) were selected from among the most pathogenic avian H1N1 viruses, as determined by their pathogenicity scores in DBA/2J mice in our previous study (21). To determine the pathogenicity of the wild-type viruses, DBA/2J mice and BALB/cJ mice were inoculated intranasally with 106 50% egg infective doses (EID50s)/ml of a wild-type virus (n = 5/group). Fecal and lung samples were collected from all infected mice, and viral isolation was carried out in 10- to 11-day-old embryonated chicken eggs as described previously (21). To test the pathogenicity of the fecal and lung isolates, infection-naive DBA/2J mice and BALB/cJ mice were infected intranasally with a fecal or lung isolate of each wild-type virus as described above. The mice were then monitored for 14 days (n = 5/group). Fecal specimens were collected daily, and daily viral titers in each group's pooled feces were determined in terms of the number of EID50s/ml by inoculating 10- to 11-day-old embryonated chicken eggs with 10-fold serial dilutions of each sample in a solution of sterile phosphate-buffered saline (PBS) and antibiotics. Viral titers were calculated by the method of Reed and Muench (30).
Statistical analyses for survival curves were done by log-rank (Mantel-Cox) and Gehan-Breslow-Wilcoxon tests using GraphPad Prism software for Windows (v5; GraphPad Software, Inc., La Jolla, CA). Statistical significance was determined at a P value of 0.05.
Histopathology.
DBA/2J or BALB/cJ mice were infected with 106 EID50s/ml of the sb/DE/09 fecal isolate. As a negative control, 1× sterile PBS was used to inoculate DBA/2J and BALB/cJ mice. At 3 and 4 days postinoculation (dpi), the mice were euthanized, and tissue for histologic examination was collected from several organs (i.e., lungs, nasal cavity, small intestine, large intestine, pancreas, kidney, liver, spleen, and brain) and fixed in 10% neutral buffered formalin. The fixed tissue was embedded in paraffin, cut into 4-μm sections, stained with hematoxylin-eosin, and examined by light microscopy. Histopathologic assessment of the organ samples was conducted in a blinded manner.
Immunohistochemistry.
Goat anti-influenza virus NP antibody (USBiological, Swampscott, MA) was used for detecting virus-infected cells by immunohistochemistry. Deparaffinized tissue sections were treated in antigen retrieval buffer (target retrieval, pH 9) at 110°C for 15 min and subsequently allowed to reach room temperature in 30 min. Endogenous peroxidase activity was quenched by incubating the slides with 3% H2O2 for 5 min, and nonspecific binding of secondary antibody was blocked using the Background Sniper reagent (BioCare Medical, Concord, CA) for 30 min. Endogenous biotin reactivity was inhibited by incubating the slides in avidin/biotin blocker (Dako, Carpinteria, CA) for 10 min. Polyclonal goat anti-influenza virus NP (1:1,000) was applied to the sections for 60 min at room temperature. Following washing, donkey anti-goat biotin-conjugated antibody (1:200; Santa Cruz, Santa Cruz, CA) was applied for 30 min. Visualization of primary antibody binding was achieved by application of streptavidin-horseradish peroxidase (Thermo-Shandon, Fremont, CA) for 10 min, followed by application of diaminobenzidine (Thermo-Shandon; Freemont, CA) for 5 min. The tissue was then rinsed with tap water and counterstained with hematoxylin. Before use, the primary antibody was adsorbed by diluting it in 5% mouse serum (Jackson ImmunoResearch, West Grove, PA) in antibody diluent for 4 to 18 h. Tissue sections were also reacted with an equivalent amount of PBS as a negative control.
Genomic analyses of the virus isolates.
Whole-genome sequence analyses were performed to identify genetic variants that emerged due to passaging in mice and the route that the virus was shed or replicated. For this study, we sequenced the fecal isolates obtained from DBA/2J mice during our previous study (21) and the corresponding wild-type avian H1N1 viruses; the fecal and lung isolates acquired after intranasal inoculation of DBA/2J mice or BALB/cJ mice with wild-type md/ALB/04, sb/DE/09, md/MN/07a, or md/MN/07b virus; and the fecal and lung isolates obtained after intranasal inoculation of DBA/2J or BALB/cJ mice with the fecal isolate of md/ALB/04, sb/DE/09, md/MN/07a, or md/MN/07b virus obtained during the current study. The fecal and lung isolates obtained upon intranasal inoculation with wild-type viruses are described as passage 1 isolates, and those obtained after intranasal inoculation with the fecal isolates are described as passage 2 isolates.
The viral RNA was extracted from each isolate by using a QIAamp viral RNA kit (Qiagen, Germantown, MD) according to the manufacturer's instructions and subjected to sequencing on high-throughput (Illumina, San Diego, CA) and traditional (Sanger) sequencing platforms. Multiple cDNA libraries were prepared using the standard Illumina protocol. Briefly, gene segments were amplified by universal influenza virus primers MBTuni12 and MBTuni13 (31) using a SuperScript III One-Step reverse transcription-PCR (RT-PCR) Platinum Taq HiFi kit (Invitrogen, Grand Island, NY). Then, Illumina adapters were ligated to DNA fragments to which a sheared, end-repaired, and poly(A) tail was added. The index sequences were inserted into each sample during the last round of amplification.
Whole-genome sequencing was done on an Illumina Genome Analyzer IIx system. Multiplex sequencing runs were performed to allow all wild-type viruses to be sequenced in one lane and all passage isolates to be sequenced in another. Single reads of 125 to 140 bases were collected for the samples. The sequencing reads were uniformly truncated to 75 bases due to low base-calling qualities after that position. Illumina adapter sequences were then removed using the program Cutadapt (32). The wild-type viruses were sequenced by both Sanger and Illumina sequencing, and the Sanger sequences were used as mapping references for the passaged fecal and lung isolates. In the few cases where Sanger data were not available, publicly available sequences matched by host species, region, and year were substituted as references. The Burrows-Wheeler alignment (BWA) tool was used for mapping (33). PCR duplicates were removed using the Picard program (http://picard.sourceforge.net).
Reads from samples sequenced together in multiplex have been reported to contaminate each other in Illumina sequencing instruments (34). Possible contaminant reads from the multiplexed samples in the same lane were removed by iteratively mapping each read to pairs of strains: the strain's known wild-type reference and an alternate competing strain from the same sequencing run. Reads that mapped uniquely to the alternate strain were discarded. The remaining reads were used for mapping for variant detection. In cases where no sequence for the expected contaminating strains was available, a list of public strains representing the known diversity of the virus was used for decontamination.
Genetic variants were detected using the program Bambino (35). Variants were required to meet a minimum minor allele frequency of 20%. Some automatically detected variants were removed after manual inspection in the Bambino graphical viewer, if they showed characteristics of contaminants or low-quality sequencing. Randomly selected groups of genetic variants that were detected by high-throughput sequencing were validated by Sanger sequencing. Each gene segment was amplified separately using the Qiagen one-step RT-PCR kit. Amplified products were cleaned with a QIAquick gel extraction kit (Qiagen) according to the manufacturer's instructions. Each amplicon was sequenced with a BigDye Terminator (v3.1) cycle sequencing kit on Applied Biosystems 3730xl DNA analyzers. For amplification and sequencing, previously published primer sequences were used (36). Sequence reads were assembled using the SeqMan program in the DNASTAR Lasergene 9 Core Suite (DNASTAR, Inc., Madison, WI). The consensus sequences were aligned using MEGA (v5.0) software (37) and checked for the genetic variants.
HA activation pH.
To measure the hemagglutinin (HA) activation pH values of fecal isolates from passages 1 and 2 compared to the activation pH value of the wild-type virus sb/DE/09, we performed fusion-induced hemolysis and acid stability assays. The fecal isolates used in these assays were selected on the basis of the HA mutations that they acquired. The pH of fusion-induced hemolysis was determined using horse red blood cells (hRBCs) as previously described (38). Briefly, virus stock was standardized to 128 hemagglutinating units in 50 μl solution. Standardized virus was then diluted in 1% hRBCs at a ratio of 1:4 and incubated on ice for 1 h to allow the binding of virus to the cells. The cells were then pelleted at 72 × g for 3 min. Pellets were resuspended in 100 μl pH-adjusted buffer consisting of PBS supplemented with Ca2+ and Mg2+ (PBS+) and incubated at 37°C for 1 h to allow activation of the HA protein and promote fusion. Cells were then pelleted at 72 × g for 3 min, and the amount of HA-induced cell lysis was determined as a function of the amount of hemoglobin released into the supernatant, which was measured at an absorbance of 405 nm.
To determine the acid stabilities of the viruses, prestandardized virus stock (107 50% tissue culture infective doses [TCID50s]/ml) was diluted at 1:100 in PBS+ acid buffers adjusted to the desired pH at increments of 0.2 pH unit by using 0.1 M citric acid and incubated at 37°C for 1 h. Following incubation, acid-treated viruses were neutralized in virus infection medium (1× minimal essential medium [MEM], 4% bovine serum albumin, 3% NaHCO3, 1× antibiotic-antimycotic solution, 1× MEM vitamin solution, 200 mM l-glutamine, 40 mg/liter gentamicin sulfate). The remaining infectious virus titer was then determined by measuring the number of TCID50s.
Nucleotide sequence accession numbers.
Sequences for the wild-type viruses (n = 23) were deposited in the GenBank nucleotide database at the National Center for Biotechnology Information (NCBI) (GenBank accession numbers KF424015 to KF424198).
RESULTS
Patterns of fecal shedding in mice.
To determine the pattern of viral shedding in the feces of mice infected with wild-type, fecal, or lung isolates of avian H1N1 viruses (md/MN/07a, md/MN/07b, sb/DE/09, or md/ALB/04), we collected fresh fecal samples daily from each group of BALB/cJ mice. Due to the rapid progression of the disease in DBA/2J mice after inoculation with fecal or lung isolates, fecal samples could not be collected from those animals. Therefore, we could not compare the differences in fecal virus shedding between DBA/2J mice and BALB/cJ mice.
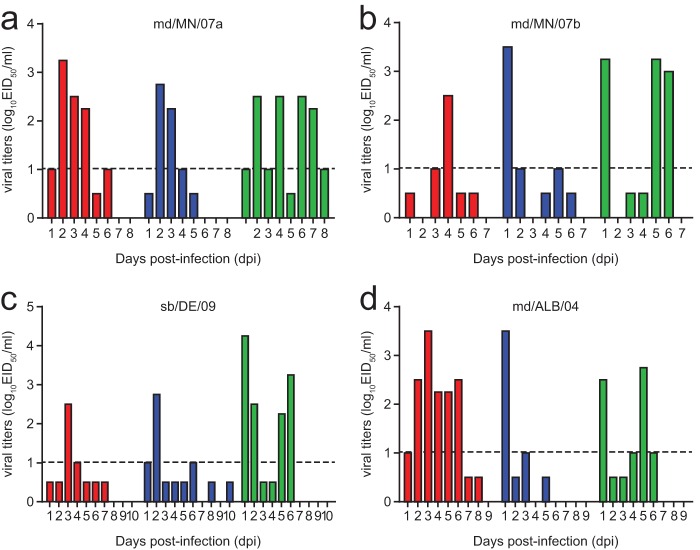
The viral shedding patterns in the feces of the BALB/cJ mice were distinctly different between animals infected with fecal isolates of avian H1N1 viruses and those infected with lung isolates or wild-type viruses. Upon infection with wild-type viruses, fecal shedding was detected in modest titers (2.25 to 3.5 log10 EID50s/ml). We observed the peak viral titer only at one time point in two groups of mice infected with sb/DE/09 (3 dpi) or md/MN/07b (4 dpi). For the other two groups of mice, the peak viral titers were detected on several consecutive days that followed a normal distribution (Fig. 1). Mice infected with the lung isolates shed virus at modest viral titers (2.25 to 3.5 log10 EID50s/ml) at 1 to 3 dpi. Thereafter, the titers fell to undetectable levels (<1 log10 EID50/ml) (Fig. 1). In contrast, mice infected with the fecal isolates shed various amounts of virus for a longer period: moderate viral titers (2.5 to 4.25 log10 EID50s/ml) were detected at 1 to 2 dpi, followed by a drop to almost undetectable levels and then a return to approximately the initial titers (2.25 to 3.25 log10 EID50s/ml) at 5 to 6 dpi. This result was consistent for each group of BALB/cJ mice infected with the fecal isolates from mice inoculated with avian H1N1 viruses. Thus, BALB/cJ mice infected with fecal isolates follow a bimodal distribution in their viral shedding pattern in feces (Fig. 1). The pattern of viral shedding in mice infected with wild-type viruses was almost indistinguishable from that of animals infected with the lung isolate in terms of the normal distribution of shedding, although the peak viral titers were obtained at different time points upon infection with the wild-type or lung isolate.
Fig 1.
Pattern of fecal shedding in BALB/cJ mice intranasally infected with the wild type (red), a lung isolate (blue), or a fecal isolate (green) of the following viruses: A/mallard/MN/AI07-3136/2007 (md/MN/07a), A/mallard/MN/AI07-3100/2007 (md/MN/07b), A/shorebird/DE/300/2009 (sb/DE/09), or A/mallard/ALB/88/2004 (md/ALB/04). Viral titers are given as the log10 number of EID50s/ml, and the minimal detection level is indicated by a dashed line at 1 log10 EID50/ml. Fecal samples with titers below the detection level were positive by hemagglutination assay when they were tested undiluted.
Pathogenicity of fecal and lung isolates in mice.
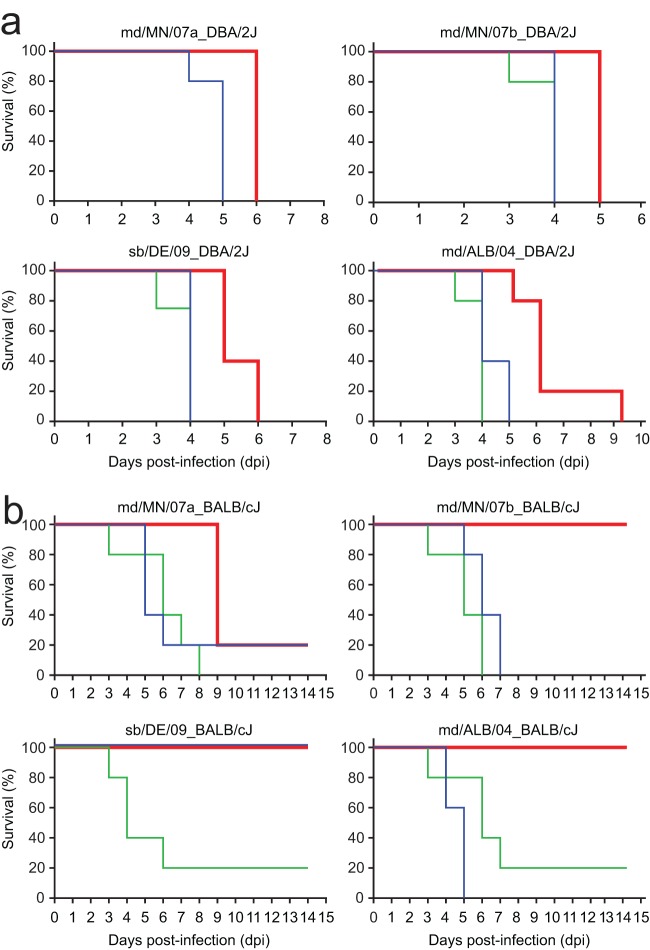
To compare the pathogenicity of passage 1 fecal isolates and lung isolates with that of the corresponding wild-type viruses, we inoculated DBA/2J and BALB/cJ mice intranasally. The fecal and lung isolates were significantly more lethal than their wild-type counterparts (P < 0.05) in both strains of mice (Fig. 2). However, the pathogenicity of most fecal isolates did not differ from that of the corresponding lung isolates (P > 0.05).
Fig 2.
Survival curves for DBA/2J (a) and BALB/cJ (b) mice infected with the wild type (red), passage 1 fecal isolates (green), or passage 1 lung isolates (blue) of the following viruses: A/mallard/MN/AI07-3136/2007 (md/MN/07a), A/mallard/MN/AI07-3100/2007 (md/MN/07b), A/shorebird/DE/300/2009 (sb/DE/09), or A/mallard/ALB/88/2004 (md/ALB/04). Mortality was determined on the basis of death or euthanasia at 25% weight loss. Each group included five mice, except for the group of DBA/2J mice infected with sb/DE/09, which included four mice.
Overall mortality was slightly delayed in animals inoculated with lung isolates compared to that in mice inoculated with fecal isolates (Fig. 2). The pattern of early mortality (i.e., 20% by 3 dpi) was consistent between mouse strains infected with the fecal isolates. However, early mortalities were delayed by 1 to 2 days in the mice infected with the lung isolates (Fig. 2). We could not compare the fecal isolate of md/MN/07a to its corresponding wild-type virus or lung isolate, because virus could not be recovered from the feces of DBA/2J mice infected with wild-type md/MN/07a. In general, we could not assess the differences in pathogenicity of fecal and lung isolates in DBA/2J mice because the animals were so highly sensitive to influenza A virus infections (21, 39–41).
Three of the four wild-type H1N1 viruses (md/MN/07b, sb/DE/09, and md/ALB/04) did not cause mortality in BALB/cJ mice, but md/MN/07a caused 80% mortality by 9 dpi (Fig. 2b). In the groups of BALB/cJ mice infected with the fecal or lung isolates of md/MN/07b or md/ALB/04, the pathogenicity of fecal and lung isolates was significantly higher than that of wild-type viruses (P < 0.05), but no statistically significant difference in pathogenicity was observed between the fecal isolates and lung isolates (P > 0.05) (Fig. 2b). The fecal isolates of md/MN/07a or sb/DE/09 were significantly more pathogenic than the corresponding wild-type viruses (P < 0.05), but the lung isolates were not (P > 0.05). The pathogenicity of the fecal isolate of sb/DE/09 was significantly different from that of the corresponding lung isolate (P < 0.05). However, there was no difference between the pathogenicities of fecal and lung isolates of md/MN/07a (P > 0.05) (Fig. 2b).
Overall, the pathogenicities of fecal and lung isolates were virus strain specific. The passage isolates obtained from BALB/cJ mice infected with avian H1N1 viruses of mallard origin showed no difference in pathogenicity, while the pathogenicities of isolates obtained from the same strain of mice infected with an avian H1N1 virus of shorebird origin differed significantly.
Histopathologic features of infected organs.
The lungs of the DBA/2J mice and BALB/c mice infected with the fecal isolate of sb/DE/09 had similar pathological features, but the lesions observed in DBA/2J mice were more extensive and severe than those observed in BALB/cJ mice. The lungs had necrotizing bronchitis and bronchiolitis with acute patchy alveolitis in the adjacent alveoli. Pathological changes were not observed in any of the other organs examined.
Immunohistochemical assay showed that viral antigens were mainly in the upper and lower respiratory tissues, such as the nasal cavity, trachea, bronchioles, and alveoli. In comparison, no viral antigens were observed in the pancreas, small or large intestine, kidney, gallbladder, liver, or brain.
Genetic variations in fecal isolates of DBA/2J mice infected with wild-type viruses.
To analyze whether the fecal isolates obtained from DBA/2J mice (n = 22) in our previous study (21) were genetically different from the corresponding wild-type viruses used for inoculation, we examined the whole-genome sequences of each fecal and wild-type isolate after deep sequencing. Genetic variations were present in 19 of 22 fecal isolates from DBA/2J mice. Of those, 15 isolates carried HA mutations (Table 1).
Table 1.
Nonsynonymous genetic variants detected in fecal samples from DBA/2J mice at 3 or 4 dpi after intranasal inoculation with avian H1N1 viruses
| Influenza A virus fecal isolate | PIb | Variation(s) in the following influenza virus genesa: |
|||||
|---|---|---|---|---|---|---|---|
| PB2 | PA | HA | NP | NA | NS1 | ||
| A/mallard/ALB/119/1998 | 4 | N498S | |||||
| A/mallard/MN/AI07-3100/2007c | 4 | ||||||
| A/shorebird/DE/300/2009 | 4 | E627K | H300P | ||||
| A/mallard/ALB/201/1998 | 4 | L8I, V324I | |||||
| A/pintail/ALB/210/2002 | 4 | I96L | |||||
| A/mallard/OH/4809-9/2008 | 4 | N483K | |||||
| A/shorebird/DE/324/2009 | 4 | E627K | H300P, F454L | ||||
| A/mallard/ALB/88/2004 | 4 | A84D, E627K | D52N, F128V, F454L | ||||
| A/redheaded duck/MN/Sg-00123/2007 | 3 | F128V, D434N | N483K | ||||
| A/pintail/ALB/69/2005 | 3 | G316S | |||||
| A/northern shoveler/MN/Sg-00651/2008 | 3 | L86F | |||||
| A/gull/DE/428/2009 | 3 | E627K | H300P | ||||
| A/mallard/ALB/267/96 | 3 | V324I | K111N | ||||
| A/shorebird/DE/170/2009 | 3 | E627K | H300P | ||||
| A/mallard/MO/466554-14/2007 | 3 | F128V | S42N | ||||
| A/blue-winged teal/LA/B228/86 | 3 | L122 M | N483K | ||||
| A/mallard/TN/11464/85 | 3 | F454L | N483K | ||||
| A/canvasback/ALB/276/2005c | 3 | ||||||
| A/mallard/MN/Sg-00628/2008 | 3 | L86F | |||||
| A/mallard/MN/Sg-00627/2008c | 2 | ||||||
| A/shorebird/DE/274/2009 | 2 | A232V | |||||
| A/green-winged teal/LA/Sg-00090/2007 | 1 | V410A | P215S | ||||
No genetic variations were detected in the PB1 or M genes of any fecal isolate.
PI, pathogenicity index. Pathogenicity index values were previously determined in DBA/2J mice (21). PI values are as follows: 4, most pathogenic; 3, moderately pathogenic; 2, low pathogenic; 1, least pathogenic.
No genetic variations were detected in this isolate.
In five fecal isolates, PB2E627K mutations were detected, and four of these were in mice infected with viruses of shorebird and gull origin. This suggests that avian H1N1 viruses isolated from Charadriiformes species have the unique ability to rapidly adapt to mammals. The other amino acid substitutions were observed in the NP gene (N483K and N498S) of the five isolates, the NA gene (S42N, K111N, and A232V) of three isolates with no consistent pattern, the PA gene (G316S) of one isolate, and the NS1 gene (P215S) of another isolate. The mutations detected in the PB2 and NP genes were observed in the fecal isolates from mice inoculated with either the most pathogenic (pathogenicity index [PI], 4) or moderately pathogenic (PI, 3) avian H1N1 viruses. The mutations in other genes did not show any correlation to the pathogenicity of the initial viruses described in DBA/2J mice (21). Half of the fecal isolates examined were found to be double mutants (i.e., viruses with simultaneous mutations in two genes).
Because we frequently detected HA mutations in the fecal isolates, we sought to determine the location of these mutations on the structure of the HA molecule to understand whether they may have functional significance (Fig. 3). One mutation (L8I) was detected in the signal peptide (Table 1). Four other mutations (L86F, I96L, L122M, and F128V) were detected in the vestigial esterase domain. Six mutations (D52N, H300P, V324I, V410A, D434N, and F454L) were located in the stalk region (Fig. 3).
Fig 3.
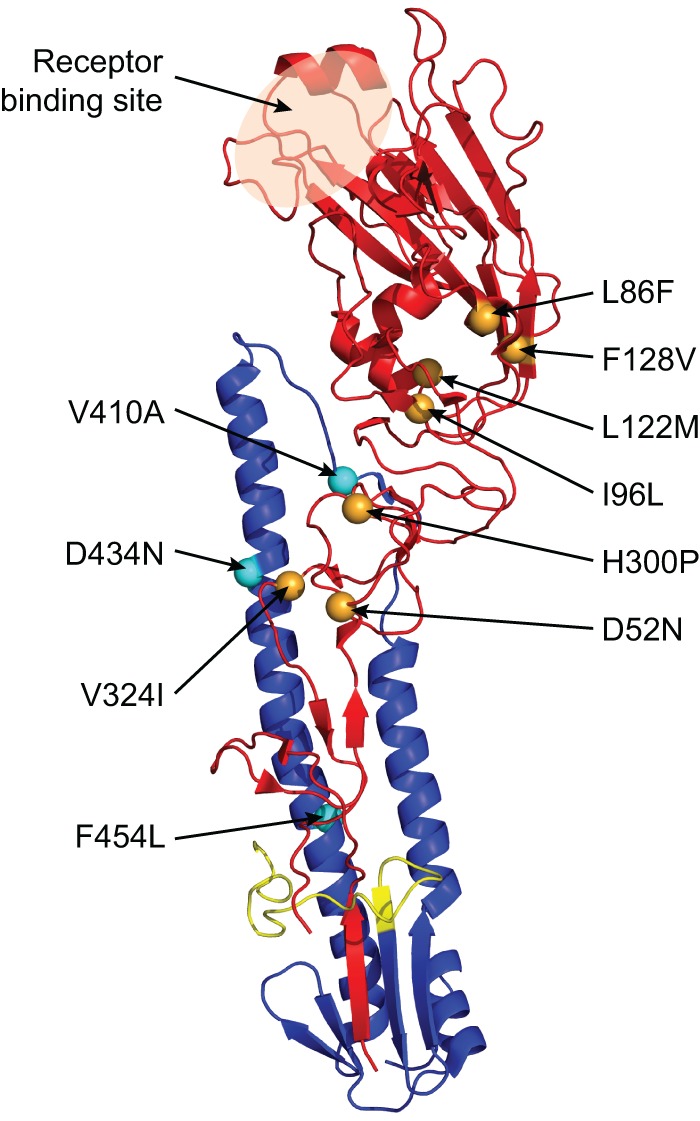
Structural illustration of the genetic variations detected in the HA molecule of the passage 1 fecal isolates after intranasal inoculation of DBA/2J mice with avian H1N1 influenza A viruses. The HA1 subunit is shown in red, and the HA2 subunit is shown in blue. The fusion peptide of the HA2 subunit is shown in yellow. Orange spheres indicate the mutations detected in HA1, and the light blue spheres indicate the mutations detected in HA2. The amino acid substitutions observed in fecal isolates are indicated (H1 numbering). The PyMOL molecular graphics system (62) was used to generate the structure using avian H1 protein structure (Protein Data Bank accession number 3HTO) (63).
Selection of variants from passaged viruses.
To further investigate whether fecal isolates are genetically different from their corresponding wild-type viruses and lung isolates, we analyzed the passage 1 fecal and lung isolates from DBA/2J and BALB/cJ mice after inoculation with a wild-type virus (md/ALB/04, sb/DE/09, md/MN/07a, or md/MN/07b). Then, we analyzed the passage 2 fecal isolates obtained at two time points and passage 2 lung isolates obtained at one time point (as shown in Table 2) from both strains of mice inoculated with a passage 1 fecal isolate to examine the selection of variants via the fecal route versus lung replication during the second infection.
Table 2.
Selection of variants in fecal and lung isolates from mice infected with avian H1N1 influenza viruses
| Virus | Mouse strain | Passage | Source of virus (dpi) | Variation(s) in the following influenza virus genesa: |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PB2 | PB1 | PA | HA | NP | NA | NS1 | ||||
| A/mallard/ALB/88/2004 | DBA/2J | 1 | Fecal (4) | A84D, E627K | D52N, F128V, F454L | |||||
| DBA/2J | 1 | Lung (6) | E627K | H300P, F128V, F454L | ||||||
| DBA/2J | 2 | Fecal (1) | E627K | F128V, F454L | ||||||
| DBA/2J | 2 | Fecal (2) | E627K | K578E, P607S | F128V, F454L | L95I | ||||
| DBA/2J | 2 | Lung (4) | E627K | P607S | F128V | L95I | ||||
| BALB/cJ | 1 | Fecal (3) | D161N | D52N, F128V, F454L | L95I | |||||
| BALB/cJ | 1 | Lungb | ||||||||
| BALB/cJ | 2 | Fecal (1) | E627K, A684S | K578E, P607S | F128V, F454L | L95I | ||||
| BALB/cJ | 2 | Fecal (5) | E65D, D161N, | K578E, P607S | K19R | F128V, F454L | L95I | |||
| E627K, A684S | ||||||||||
| BALB/cJ | 2 | Lung (3) | F128V, F454L | L95I | ||||||
| A/shorebird/DE/300/2009 | DBA/2J | 1 | Fecal (4) | E627K | H300P | |||||
| DBA/2J | 1 | Lung (5) | E627K | |||||||
| DBA/2J | 2 | Fecal (1) | E627K | H300P, F454L | N207D | |||||
| DBA/2J | 2 | Fecal (2) | E627K | H300P | ||||||
| DBA/2J | 2 | Lung (4) | E627K | H300P, Q406K, F454L | ||||||
| BALB/cJ | 1 | Fecal (4) | E627K | H300P | ||||||
| BALB/cJ | 1 | Lung (3) | T105A | |||||||
| BALB/cJ | 2 | Fecal (1) | E627K | H300P | ||||||
| BALB/cJ | 2 | Fecal (6) | E627K | H300P | P120L, A232V | |||||
| BALB/cJ | 2 | Lung (6) | E627K | H300P | ||||||
| A/mallard/MN/AI07-3136/2007 | DBA/2Jc | 1 | Lung (6) | L61 M | R430K | S94N | ||||
| BALB/cJ | 1 | Fecal (3) | L61 M | R430K | S94N | |||||
| BALB/cJ | 1 | Lung (6) | V125I | R430K | S94N | |||||
| BALB/cJ | 2 | Fecal (1) | D52E, H300Q | R430K | S94N | |||||
| BALB/cJ | 2 | Fecal (6) | L61M, V324I | S94N | ||||||
| BALB/cJ | 2 | Lung (3) | R430K | S94N | ||||||
| A/mallard/MN/AI07-3100/2007 | DBA/2J | 1 | Fecal (4) | |||||||
| DBA/2J | 1 | Lung (5) | ||||||||
| DBA/2J | 2 | Fecal (1) | ||||||||
| DBA/2J | 2 | Fecal (4) | ||||||||
| DBA/2J | 2 | Lung (4) | ||||||||
| BALB/cJ | 1 | Fecal (4) | E627K | E349G | ||||||
| BALB/cJ | 1 | Lungb | ||||||||
| BALB/cJ | 2 | Fecal (1) | E627K | |||||||
| BALB/cJ | 2 | Fecal (5) | E627K | |||||||
| BALB/cJ | 2 | Lung (3) | N498S | |||||||
Predominant mutations are formatted in bold. No genetic mutations were detected in the M gene of any isolate.
This isolate was not sequenced.
No fecal isolate was obtained.
We found that nearly all passage 1 fecal and lung isolates obtained from both strains of mice differed from the wild-type viruses, with the exception of the isolates obtained from DBA/2J mice infected with md/MN/07b (Table 2). Moreover, the mutations acquired by the fecal isolates differed from those acquired by the lung isolates (Table 2). The PB2E627K mutation and HA mutations (HAD52N, HAF128V, and HAF454L in md/ALB/04 and HAH300P in sb/DE/09) were frequently detected simultaneously in the fecal isolates of both mouse strains (Table 2). The double mutations were also associated with the pathogenicity of the fecal isolates obtained from passage 1 when inoculated in mouse models (Fig. 2). In the fecal isolate from BALB/cJ mice infected with md/ALB/04, instead of PB2E627K, the PB2D161N mutation was observed in association with the HAD52N, HAF128V, and HAF454L mutations. In fact, this isolate was less pathogenic than the corresponding lung isolate (Fig. 2b). On the other hand, the PB2E627K and HAH300P mutations in the fecal isolate from BALB/cJ mice infected with the sb/DE/09 virus were strongly associated with the increased pathogenicity of the fecal isolate, whereas the lung isolate, which did not acquire either the PB2E627K or the HAH300P mutation during the first infection, was nonpathogenic.
None of the isolates from the most pathogenic avian H1N1 virus in BALB/cJ mice (md/MN/07a) acquired the PB2E627K mutation, though both passage 1 isolates were more pathogenic than the original wild-type virus. The cumulative effects of mutations in HA (L61M in the fecal isolate and V125I in the lung isolate) and NAR430K might increase the pathogenicity of these isolates due to the HA-NA balance. The accumulation of NS1S94N might also be important in pathogenicity. Overall, increased pathogenicity in mice was associated with the emergence of the PB2E627K mutation in three viruses, and HA mutations accompanied the PB2E627K mutation in two (Table 2).
Upon infection with the passage 1 fecal isolates, genetic differences were detected between passage 2 fecal and lung isolates. Moreover, novel variations emerged in the fecal isolates obtained at two different time points. The simultaneous occurrence of PB2E627K and HAF128V and F454L in md/ALB/04 was maintained in passage 2 fecal isolates from DBA/2J and BALB/cJ mice, while lung isolates carried only two of these mutations (PB2E627K and HAF128V in DBA/2J mice and HAF128V and HAF454L in BALB/cJ mice). Additional mutations were acquired by the fecal isolates obtained on a later day (PB1K578E, PB1P607S, and NS1L95I at 2 dpi in DBA/2J mice and PB2E65D, PB2D161N, and PAK19R at 5 dpi in BALB/cJ mice). On the other hand, the fecal isolates obtained from the DBA/2J and BALB/cJ mice infected with wild-type sb/DE/09 acquired the double mutation PB2E627K and HAH300P in passage 1; therefore, these mutations were inherited by passage 2 fecal and lung isolates of both mouse strains infected with the passage 1 fecal isolate of sb/DE/09. However, additional mutations were acquired by different isolates (e.g., NS1N207D in the fecal isolates of DBA/2J mice at 1 dpi, HAQ406K in the lung isolates of DBA/2J mice at 4 dpi, and NAP120L and NAA232V in the fecal isolates of BALB/cJ mice at 6 dpi) (Table 2).
Although some mutations were inherited from the passage 1 fecal isolates and were maintained in passage 2 fecal and lung isolates, novel mutations were acquired in the fecal isolates obtained later (5 to 6 dpi) (Table 2). Furthermore, we observed genetic differences between passage 2 fecal isolates and lung isolates. In each passage, we detected virus- and host-specific differences in the accumulated or maintained mutations that contributed to the increased pathogenicity of the passage isolates.
HA activation pH and acid stability.
Mutations that alter the acid stability of the HA protein are associated with adaptation and the increased virulence of influenza viruses in mice (42–45). Therefore, we tested whether HA mutations in the fecal isolates altered the acid stability of the wild-type virus so that it could better adapt to replication in mice. Fecal isolates from passages 1 and 2 in DBA/2J mice inoculated with sb/DE/09 were triggered for fusion and caused hemolysis of hRBCs at pH 5.4 or lower. In comparison, fecal isolates from BALB/cJ mice caused an equivalent amount of fusion-induced hemolysis at pH 5.2 or lower (Fig. 4a). The wild-type sb/DE/09 virus was the most stable of the five, causing fusion-induced hemolysis occurring at pH 5.0 or lower (Fig. 4a). We then compared the stability of these viruses upon treatment with acidic pH buffers to measure the retention of infectivity after acid exposure of wild-type and mutant viruses (Fig. 4b). The infectivity of the fecal isolates from both DBA/2J and BALB/cJ mice was completely destroyed at pH 5.4, whereas that of the wild-type virus was maintained until exposure to pH 5.2. Overall, these results suggest that HA mutations in the fecal isolates destabilized the HA protein, resulting in activation of this protein for fusion at higher pHs, thus increasing the virulence of the fecal isolates.
Fig 4.
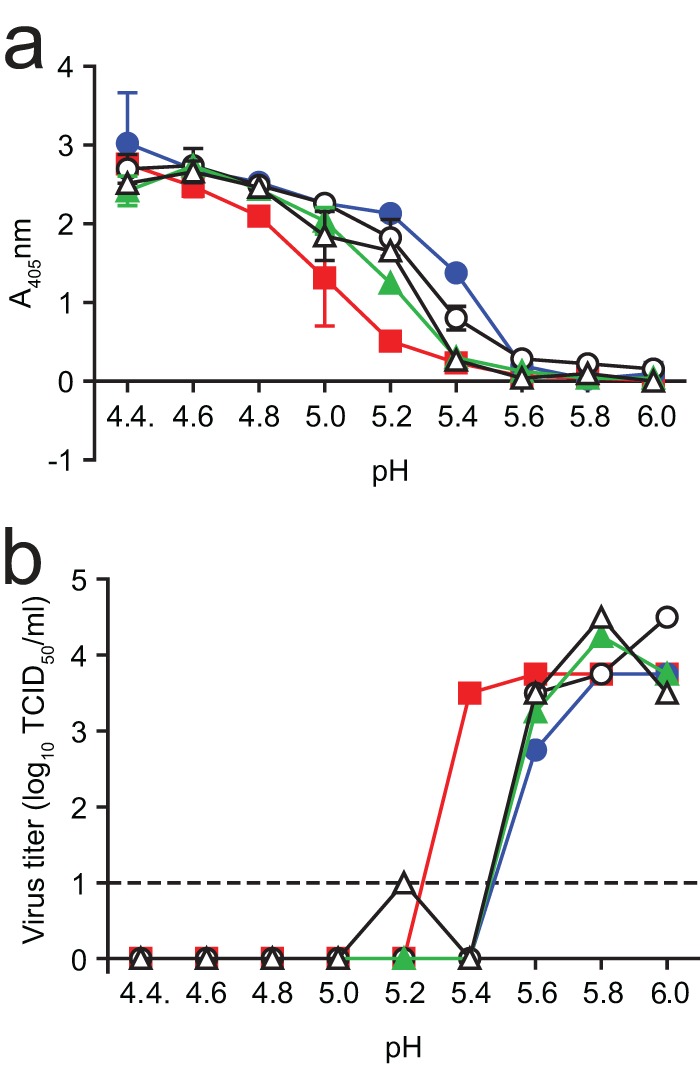
pH of activation of the HA protein. (a) Fusion-induced hemolysis of hRBCs upon incubation under the indicated pH conditions with wild-type sb/DE/09 virus (red squares), passage 1 or 2 fecal isolates recovered from DBA/2J mice (blue circles, passage 1; white circles, passage 2, day 1), or those recovered from BALB/cJ mice (green triangles, passage 1; white triangles, passage 2, day 6). (b) Under acidic conditions, the infectivity of the fecal isolates obtained from both strains of mice was reduced in comparison to that of the wild-type virus.
DISCUSSION
Although the source of influenza virus in feces and how it passes through the mammalian digestive tract are poorly understood, we hypothesize that there is a strong selection for genetic variants that are shed in feces during an influenza virus infection. Here we demonstrated that the fecal isolates obtained from mice infected with avian H1N1 viruses caused a severe respiratory infection and a longer period of viral shedding in feces upon intranasal inoculation. Furthermore, the fecal isolates were at least as pathogenic as the corresponding lung isolates. In BALB/cJ mice infected with the fecal isolate of sb/DE/09, however, a drastic increase in the pathogenicity of the fecal isolate compared to that of the lung isolate, which was nonpathogenic, was shown. The fecal isolate of sb/DE/09 acquired two mutations (PB2E627K and HAH300P), but the lung isolate acquired only one (PB2T105A). Therefore, pathogenicity was associated with the mutations acquired by the fecal isolate. The mutations in HA were located at regions that might affect the acid stability of the isolate. We showed that mice infected with fecal isolates have a bimodal distribution of viral shedding in the feces, whereas mice infected with a wild-type virus or lung isolates have a normal distribution of viral shedding in the feces.
Molecular analyses demonstrated that both fecal and lung isolates were genetically different from the wild-type viruses. Furthermore, genetic differences were detected between fecal and lung isolates. Molecular dissimilarities between the passage isolates and the parental strain used for inoculation suggested that the viruses shed via the feces did not originate by swallowing of parental viruses during intranasal inoculation on day 0. Detailed examination of human colonic samples indicated that sialic acid α-2,6 receptors are abundant on the epithelial cells of the gastrointestinal tract, and sialic acid α-2,3 receptors can be found from the ileum to the rectum, with abundant expression of avian sialic acid α-2,3 receptors in goblet cells being found in the large intestine (46). However, we did not detect viral antigens or lesions in the pancreas, liver, or intestines. Thus, we can only speculate that a portion of infectious influenza viruses in a quasispecies population is selected during replication in the upper or lower respiratory tracts and displaced to the gastrointestinal tract due to mucociliary movements. However, this phenomenon merits further investigation.
The emergence of novel variants among fecal and lung isolates was also related to the pathogenicity phenotype in the corresponding mouse models. The PB2E627K mutation determines the host range for influenza viruses (47) and increases the virulence in a mouse model (48). The increased virulence of the fecal isolates might well be due to the selection of the PB2E627K mutation, which was associated with the increased pathogenicity of fecal isolates in three of the four viruses examined. However, it is noteworthy that neither passage isolate of the most pathogenic avian H1N1 virus in BALB/cJ mice acquired the PB2E627K mutation, suggesting that multiple molecular strategies were implemented by each virus to adapt to the mammalian host.
Although the PB2E627K mutation is important for efficient viral replication in mice, it was not the sole factor associated with the increased virulence of the fecal isolates. The adaptive genetic variations were mainly detected in the PB2 and HA genes of the fecal and lung isolates, which is consistent with the findings of other laboratories, in terms of influenza virus adaptation and virulence in mice (49). Moreover, these mutations were generally maintained in the fecal isolates after the second passage, and additional mutations in different gene segments were acquired, especially on later days postinfection.
The day-to-day variation in the accumulation of mutations in passage 2 fecal isolates was associated with the bimodal fecal shedding pattern in BALB/cJ mice infected with the passage 1 fecal isolates. The emergence of novel variants and the increased viral titers in the feces by 5 to 6 dpi, regardless of the decreasing number of mice in each group due to infection, suggest that the appearance of novel variants later during the infection is replication dependent. However, some of those mutations were eliminated from the virus population during respiratory infection and were replaced with other mutations in lung isolates. For instance, during infections with the fecal isolates after passage 1 of md/ALB/04, PB1K578E and HAF454L mutations were not selected in the passage 2 lung isolate of DBA/2J mice and PB2E65D, PB2D161N, PB2E627K, PB2A684S, PB1K578E, PB1P607S, and PAK19R mutations were not selected in the passage 2 lung isolate of BALB/cJ mice. Thus, our findings demonstrate the selection of novel variants through fecal shedding, regardless of the parental strain used for intranasal inoculation.
In terms of the distribution of the genetic variants across the genomes, pathogenesis was observed to be a polygenic trait that is not only virus specific but also host specific. This result is consistent with the findings of others (49, 50). Fecal isolates were obtained from pooled samples from each group of mice, and lung isolates were obtained from individual mice. Due to the small amount of fecal samples collected from each mouse as a result of appetite loss during influenza virus infection, we had to pool fecal samples from each group for successful virus isolation. Although the use of pooled fecal samples might introduce discrepancies into the sequence analyses, the genetic differences between the fecal and lung isolates were clear. For instance, in BALB/cJ mice infected with passage 1 fecal isolates from mice infected with md/ALB/04 or md/MN/07b, lung isolates were recovered from mice that died of infection at 3 dpi. None of the mice carried the PB2E627K mutation in their lung isolates, but the fecal isolates had PB2E627K at 1 and 5 dpi. Thus, we would expect to find PB2E627K in the lungs at 3 dpi, especially because that mutation is strongly associated with mammalian adaptation and increased pathogenicity in mice.
The HA mutations that we identified were mainly in the stalk and vestigial esterase domain of the HA molecule and not in the receptor-binding domain. This is most likely due to the expression of α-2,3 sialic acid receptors in mouse models (51, 52). Increased fusion pH is associated with increased virulence in mice (42). Due to the positions of the amino acid substitutions and the nature of the wild-type avian influenza viruses, we studied the stability of fecal and lung isolates in different pH environments. The fusion pH of the fecal isolates was higher than that of the wild-type virus. Therefore, mutations detected on HA might contribute to the increased pathogenesis of the fecal isolates by altering the acid stability. The pH of the mouse's stomach is 3.0 in animals that have been recently fed and 4.0 in animals that are in a fasted state; the intestinal pH is less than 5.2 (53).
In a hypothetical scenario of viruses passing through the gastrointestinal tract, one would expect that they would be completely inactivated in the feces after being exposed to acidic conditions. The fact that infectious viruses with an HA activation pH of ≥5.4 were isolated from the feces suggests either that the novel variants were mixed with food and well protected during passage through the acidic environment of the digestive tract or that the novel variants were the products of viral replication at another, as yet unidentified site. They may perhaps pass through the acid environment with uncleaved HA proteins—thereby being protected from acid inactivation—and then be primed for infectivity by subsequent proteolytic cleavage. Computational analyses performed on the basis of 2009 pandemic H1N1 sequences available from the National Center for Biotechnology Information Influenza Virus Resource showed that the HAQ310H mutation is associated with mild cases and fatal cases (54). Therefore, the immediate acquisition of HAH300P in the fecal isolates of sb/DE/09 might have significance, on the basis of the close proximity of these two mutations in the stalk of the HA molecule. The functional importance of these mutations needs to be further investigated.
As shown previously, the adaptation of the 2009 pandemic H1N1 virus (A/CA/04/2009) to BALB/cJ mice requires at least nine passages in the lung (55). Similarly, the adaptation of human H3N2 virus (A/Hong Kong/1/68) requires 20 serial passages in the lung to observe adaptive mutations in the CD-1 mouse model (49). Increased pathogenicity has been observed with mouse-adapted avian H9N2 following eight lung-to-lung passages (56). However, we observed increased pathogenicity in fecal isolates after only one passage. Although this rapid adaptation could be the result of the unique nature of avian H1N1 viruses, this finding suggests that fecal shedding is a novel strategy for the rapid adaptation of some influenza viruses to mammalian hosts.
The differences between fecal isolates and lung isolates, in terms of pathogenesis and molecular changes, indicated strain-specific variations on the basis of the host of origin. The avian H1N1 viruses isolated from Charadriiformes may have the unique ability to rapidly adapt to mammals via the fecal route, and those isolated from Anseriformes may use both fecal and respiratory dissemination for this purpose. However, this phenomenon needs further investigation. The emergence of novel variants via different routes during influenza virus infection might influence the emergence of epidemics and perhaps pandemics. The lack of hygienic conditions in underdeveloped regions and parts of developing countries might also contribute to the accumulation of novel variants in the population. Influenza virus transmission can occur via fomites, and the maintenance of virus infectivity on such objects varies, depending on whether their surfaces are porous or nonporous (57–59). Therefore, the transmission of novel variants selected through the fecal route may be increased, especially in public areas, due to a lack of proper hand washing.
Coprophagy, or feeding on excrement, is common in lagomorphs (rabbits), rodents (mice, rats, guinea pigs), foals, swine, and nonhuman primates (60). Some of these animals are natural hosts for influenza A viruses, but others are prone to influenza virus infections only in experimental settings. To our knowledge, rectal swabs are not examined for viral detection during equine influenza outbreaks (Thomas Chambers, Gluck Equine Research Center, University of Kentucky, personal communication). Therefore, coprophagy might result in the contact transmission of novel influenza virus variants shed by feces in nature, especially among mammals that commonly consume feces. In such incidents, fecal isolates with novel genetic variations might cause more severe respiratory disease, leading to the emergence of influenza outbreaks in nature. A few consequences of such an event would be contact transmission of fecal isolates in mammals and selection of different variants that contribute to viral evolution and viral ecology. This could lead to the emergence of new mammalian reservoirs for influenza, and the potential for transmission of these fecal variants to humans would be higher, especially in locales where the human-animal interface is high.
In conclusion, this study addresses the potential importance of fecal shedding during influenza virus infection in mammals. Whether viral shedding via feces provides an additional source of transmission for mammals in nature is unknown. Nonetheless, during the 2009 H1N1 pandemic, the Centers for Disease Control and Prevention suggested that all bodily fluids be handled with precaution due to the unknown transmissibility of the virus (61). With increased awareness of risk assessment efforts for influenza A virus epidemics and pandemics, this study raises concern for the lack of proper hygienic conditions, especially in underdeveloped and developing countries where humans commonly interact with animals.
ACKNOWLEDGMENTS
This work was supported by contract no. HHSN266200700005C from the National Institute of Allergy and Infectious Diseases, National Institutes of Health, U.S. Department of Health and Human Services, and by ALSAC.
We thank Dave Stallknecht of the Southeastern Cooperative Wildlife Disease Study (University of Georgia) and Scott Krauss for providing the viruses, Patrick Seiler and Heather Forrest for their help preparing samples for histologic examinations, the staff of the St. Jude Animal Resource Center for providing excellent care to the animals throughout the course of the experiment, Angela McArthur for editorial assistance, Julie Groff for assistance with the graphical arts, and James Knowles for excellent administrative assistance.
Footnotes
Published ahead of print 21 August 2013
REFERENCES
- 1.Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. 1992. Evolution and ecology of influenza A viruses. Microbiol. Rev. 56:152–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kida H, Yanagawa R, Matsuoka Y. 1980. Duck influenza lacking evidence of disease signs and immune response. Infect. Immun. 30:547–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hinshaw VS, Webster RG, Turner B. 1979. Water-borne transmission of influenza A viruses? Intervirology 11:66–68 [DOI] [PubMed] [Google Scholar]
- 4.Chan MC, Lee N, Chan PK, Leung TF, Sung JJ. 2009. Fecal detection of influenza A virus in patients with concurrent respiratory and gastrointestinal symptoms. J. Clin. Virol. 45:208–211 [DOI] [PubMed] [Google Scholar]
- 5.Chan MC, Lee N, Chan PK, To KF, Wong RY, Ho WS, Ngai KL, Sung JJ. 2011. Seasonal influenza A virus in feces of hospitalized adults. Emerg. Infect. Dis. 17:2038–2042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Jong MD, Bach VC, Phan TQ, Vo MH, Tran TT, Nguyen BH, Beld M, Le TP, Truong HK, Nguyen VV, Tran TH, Do QH, Farrar J. 2005. Fatal avian influenza A (H5N1) in a child presenting with diarrhea followed by coma. N. Engl. J. Med. 352:686–691 [DOI] [PubMed] [Google Scholar]
- 7.Dilantika C, Sedyaningsih ER, Kasper MR, Agtini M, Listiyaningsih E, Uyeki TM, Burgess TH, Blair PJ, Putnam SD. 2010. Influenza virus infection among pediatric patients reporting diarrhea and influenza-like illness. BMC Infect. Dis. 10:3. 10.1186/1471-2334-10-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kawaoka Y, Bordwell E, Webster RG. 1987. Intestinal replication of influenza A viruses in two mammalian species. Brief report. Arch. Virol. 93:303–308 [DOI] [PubMed] [Google Scholar]
- 9.Liu Y, Gao R, Hu W, Ma M, Wang W, He J, Wang J, Li D, Shu Y. 2011. Detection of highly pathogenic avian influenza virus H5N1 in peripheral blood mononuclear cells and stool of a patient. Lab. Med. 42:310–313 [Google Scholar]
- 10.Pinsky BA, Mix S, Rowe J, Ikemoto S, Baron EJ. 2010. Long-term shedding of influenza A virus in stool of immunocompromised child. Emerg. Infect. Dis. 16:1165–1167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.To KK, Chan KH, Li IW, Tsang TY, Tse H, Chan JF, Hung IF, Lai ST, Leung CW, Kwan YW, Lau YL, Ng TK, Cheng VC, Peiris JS, Yuen KY. 2010. Viral load in patients infected with pandemic H1N1 2009 influenza A virus. J. Med. Virol. 82:1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoo SJ, Moon SJ, Kuak EY, Yoo HM, Kim CK, Chey MJ, Shin BM. 2010. Frequent detection of pandemic (H1N1) 2009 virus in stools of hospitalized patients. J. Clin. Microbiol. 48:2314–2315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tong S, Li Y, Rivailler P, Conrardy C, Castillo DA, Chen LM, Recuenco S, Ellison JA, Davis CT, York IA, Turmelle AS, Moran D, Rogers S, Shi M, Tao Y, Weil MR, Tang K, Rowe LA, Sammons S, Xu X, Frace M, Lindblade KA, Cox NJ, Anderson LJ, Rupprecht CE, Donis RO. 2012. A distinct lineage of influenza A virus from bats. Proc. Natl. Acad. Sci. U. S. A. 109:4269–4274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glathe H, Hilgenfeld M, Lebhardt A, Strittmatter HU, Schulze P, Brandt B. 1984. The intestine of ferret—a possible site of influenza virus replication. Acta Virol. 28:287–293 [PubMed] [Google Scholar]
- 15.Maines TR, Jayaraman A, Belser JA, Wadford DA, Pappas C, Zeng H, Gustin KM, Pearce MB, Viswanathan K, Shriver ZH, Raman R, Cox NJ, Sasisekharan R, Katz JM, Tumpey TM. 2009. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science 325:484–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arena C, Amoros JP, Vaillant V, Balay K, Chikhi-Brachet R, Varesi L, Arrighi J, Blanchon T, Carrat F, Hanslik T, Falchi A. 2012. Simultaneous investigation of influenza and enteric viruses in the stools of adult patients consulting in general practice for acute diarrhea. Virol. J. 9:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buchy P, Mardy S, Vong S, Toyoda T, Aubin JT, Miller M, Touch S, Sovann L, Dufourcq JB, Richner B, Tu PV, Tien NT, Lim W, Peiris JS, Van der Werf S. 2007. Influenza A/H5N1 virus infection in humans in Cambodia. J. Clin. Virol. 39:164–168 [DOI] [PubMed] [Google Scholar]
- 18.de Jong MD, Simmons CP, Thanh TT, Hien VM, Smith GJ, Chau TN, Hoang DM, Chau NV, Khanh TH, Dong VC, Qui PT, Cam BV, Ha do Q, Guan Y, Peiris JS, Chinh NT, Hien TT, Farrar J. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belser JA, Gustin KM, Maines TR, Pantin-Jackwood MJ, Katz JM, Tumpey TM. 2012. Influenza virus respiratory infection and transmission following ocular inoculation in ferrets. PLoS Pathog. 8:e1002569. 10.1371/journal.ppat.1002569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yen HL, Lipatov AS, Ilyushina NA, Govorkova EA, Franks J, Yilmaz N, Douglas A, Hay A, Krauss S, Rehg JE, Hoffmann E, Webster RG. 2007. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J. Virol. 81:6890–6898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kocer ZA, Krauss S, Stallknecht DE, Rehg JE, Webster RG. 2012. The potential of avian H1N1 influenza A viruses to replicate and cause disease in mammalian models. PLoS One 7:e41609. 10.1371/journal.pone.0041609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van den Brand JM, Stittelaar KJ, van Amerongen G, van de Bildt MW, Leijten LM, Kuiken T, Osterhaus AD. 2010. Experimental pandemic (H1N1) 2009 virus infection of cats. Emerg. Infect. Dis. 16:1745–1747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dawood FS, Jain S, Finelli L, Shaw MW, Lindstrom S, Garten RJ, Gubareva LV, Xu X, Bridges CB, Uyeki TM. 2009. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N. Engl. J. Med. 360:2605–2615 [DOI] [PubMed] [Google Scholar]
- 24.Khakpour M, Nik-Akhtar B. 1977. Epidemics of haemorrhagic cystitis due to influenza A virus. Postgrad. Med. J. 53:251–253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tse H, To KK, Wen X, Chen H, Chan KH, Tsoi HW, Li IW, Yuen KY. 2011. Clinical and virological factors associated with viremia in pandemic influenza A/H1N1/2009 virus infection. PLoS One 6:e22534. 10.1371/journal.pone.0022534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kupferman JC, Trachtman H, Spitzer ED. 2011. Acute glomerulonephritis and acute kidney injury associated with 2009 influenza A:H1N1 in an infant. Pediatr. Nephrol. 26:153–154 [DOI] [PubMed] [Google Scholar]
- 27.De Vleeschauwer A, Atanasova K, Van Borm S, van den Berg T, Rasmussen TB, Uttenthal A, Van Reeth K. 2009. Comparative pathogenesis of an avian H5N2 and a swine H1N1 influenza virus in pigs. PLoS One 4:e6662. 10.1371/journal.pone.0006662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lipatov AS, Kwon YK, Sarmento LV, Lager KM, Spackman E, Suarez DL, Swayne DE. 2008. Domestic pigs have low susceptibility to H5N1 highly pathogenic avian influenza viruses. PLoS Pathog. 4:e1000102. 10.1371/journal.ppat.1000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Webster RG, Yakhno M, Hinshaw VS, Bean WJ, Murti KG. 1978. Intestinal influenza: replication and characterization of influenza viruses in ducks. Virology 84:268–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493–497 [Google Scholar]
- 31.Zhou B, Donnelly ME, Scholes DT, St George K, Hatta M, Kawaoka Y, Wentworth DE. 2009. Single-reaction genomic amplification accelerates sequencing and vaccine production for classical and swine origin human influenza A viruses. J. Virol. 83:10309–10313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martin M. 2011. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet.journal 17:10–12 [Google Scholar]
- 33.Li H, Durbin R. 2009. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25:1754–1760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kircher M, Sawyer S, Meyer M. 2012. Double indexing overcomes inaccuracies in multiplex sequencing on the Illumina platform. Nucleic Acids Res. 40:e3. 10.1093/nar/gkr771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edmonson MN, Zhang J, Yan C, Finney RP, Meerzaman DM, Buetow KH. 2011. Bambino: a variant detector and alignment viewer for next-generation sequencing data in the SAM/BAM format. Bioinformatics 27:865–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Obenauer JC, Denson J, Mehta PK, Su X, Mukatira S, Finkelstein DB, Xu X, Wang J, Ma J, Fan Y, Rakestraw KM, Webster RG, Hoffmann E, Krauss S, Zheng J, Zhang Z, Naeve CW. 2006. Large-scale sequence analysis of avian influenza isolates. Science 311:1576–1580 [DOI] [PubMed] [Google Scholar]
- 37.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. 2011. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol. Biol. Evol. 28:2731–2739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krenn BM, Egorov A, Romanovskaya-Romanko E, Wolschek M, Nakowitsch S, Ruthsatz T, Kiefmann B, Morokutti A, Humer J, Geiler J, Cinatl J, Michaelis M, Wressnigg N, Sturlan S, Ferko B, Batishchev OV, Indenbom AV, Zhu R, Kastner M, Hinterdorfer P, Kiselev O, Muster T, Romanova J. 2011. Single HA2 mutation increases the infectivity and immunogenicity of a live attenuated H5N1 intranasal influenza vaccine candidate lacking NS1. PLoS One 6:e18577. 10.1371/journal.pone.0018577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Srivastava B, Blazejewska P, Hessmann M, Bruder D, Geffers R, Mauel S, Gruber AD, Schughart K. 2009. Host genetic background strongly influences the response to influenza A virus infections. PLoS One 4:e4857. 10.1371/journal.pone.0004857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boon AC, deBeauchamp J, Krauss S, Rubrum A, Webb AD, Webster RG, McElhaney J, Webby RJ. 2010. Cross-reactive neutralizing antibodies directed against pandemic H1N1 2009 virus are protective in a highly sensitive DBA/2 mouse influenza model. J. Virol. 84:7662–7667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pica N, Iyer A, Ramos I, Bouvier NM, Fernandez-Sesma A, Garcia-Sastre A, Lowen AC, Palese P, Steel J. 2011. The DBA.2 mouse is susceptible to disease following infection with a broad, but limited, range of influenza A and B viruses. J. Virol. 85:12825–12829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hartley CA, Reading PC, Ward AC, Anders EM. 1997. Changes in the hemagglutinin molecule of influenza type A (H3N2) virus associated with increased virulence for mice. Arch. Virol. 142:75–88 [DOI] [PubMed] [Google Scholar]
- 43.Ward AC, de Koning-Ward TF. 1995. Changes in the hemagglutinin gene of the neurovirulent influenza virus strain A/NWS/33. Virus Genes 10:179–183 [DOI] [PubMed] [Google Scholar]
- 44.Smeenk CA, Brown EG. 1994. The influenza virus variant A/FM/1/47-MA possesses single amino acid replacements in the hemagglutinin, controlling virulence, and in the matrix protein, controlling virulence as well as growth. J. Virol. 68:530–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zaraket H, Bridges OA, Russell CJ. 2013. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus replication and pathogenesis in mice. J. Virol. 87:4826–4834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shu Y, Li CK, Li Z, Gao R, Liang Q, Zhang Y, Dong L, Zhou J, Dong J, Wang D, Wen L, Wang M, Bai T, Li D, Dong X, Yu H, Yang W, Wang Y, Feng Z, McMichael AJ, Xu XN. 2010. Avian influenza A(H5N1) viruses can directly infect and replicate in human gut tissues. J. Infect. Dis. 201:1173–1177 [DOI] [PubMed] [Google Scholar]
- 47.Subbarao EK, London W, Murphy BR. 1993. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J. Virol. 67:1761–1764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shinya K, Hamm S, Hatta M, Ito H, Ito T, Kawaoka Y. 2004. PB2 amino acid at position 627 affects replicative efficiency, but not cell tropism, of Hong Kong H5N1 influenza A viruses in mice. Virology 320:258–266 [DOI] [PubMed] [Google Scholar]
- 49.Ping J, Dankar SK, Forbes NE, Keleta L, Zhou Y, Tyler S, Brown EG. 2010. PB2 and hemagglutinin mutations are major determinants of host range and virulence in mouse-adapted influenza A virus. J. Virol. 84:10606–10618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen H, Bright RA, Subbarao K, Smith C, Cox NJ, Katz JM, Matsuoka Y. 2007. Polygenic virulence factors involved in pathogenesis of 1997 Hong Kong H5N1 influenza viruses in mice. Virus Res. 128:159–163 [DOI] [PubMed] [Google Scholar]
- 51.Ning ZY, Luo MY, Qi WB, Yu B, Jiao PR, Liao M. 2009. Detection of expression of influenza virus receptors in tissues of BALB/c mice by histochemistry. Vet. Res. Commun. 33:895–903 [DOI] [PubMed] [Google Scholar]
- 52.Ibricevic A, Pekosz A, Walter MJ, Newby C, Battaile JT, Brown EG, Holtzman MJ, Brody SL. 2006. Influenza virus receptor specificity and cell tropism in mouse and human airway epithelial cells. J. Virol. 80:7469–7480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McConnell EL, Basit AW, Murdan S. 2008. Measurements of rat and mouse gastrointestinal pH, fluid and lymphoid tissue, and implications for in-vivo experiments. J. Pharm. Pharmacol. 60:63–70 [DOI] [PubMed] [Google Scholar]
- 54.Lee RT, Santos CL, de Paiva TM, Cui L, Sirota FL, Eisenhaber F, Maurer-Stroh S. 2010. All that glitters is not gold—founder effects complicate associations of flu mutations to disease severity. Virol. J. 7:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ilyushina NA, Khalenkov AM, Seiler JP, Forrest HL, Bovin NV, Marjuki H, Barman S, Webster RG, Webby RJ. 2010. Adaptation of pandemic H1N1 influenza viruses in mice. J. Virol. 84:8607–8616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang J, Sun Y, Xu Q, Tan Y, Pu J, Yang H, Brown EG, Liu J. 2012. Mouse-adapted H9N2 influenza A virus PB2 protein M147L and E627K mutations are critical for high virulence. PLoS One 7:e40752. 10.1371/journal.pone.0040752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Greatorex JS, Digard P, Curran MD, Moynihan R, Wensley H, Wreghitt T, Varsani H, Garcia F, Enstone J, Nguyen-Van-Tam JS. 2011. Survival of influenza A(H1N1) on materials found in households: implications for infection control. PLoS One 6:e27932. 10.1371/journal.pone.0027932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Boone SA, Gerba CP. 2005. The occurrence of influenza A virus on household and day care center fomites. J. Infect. 51:103–109 [DOI] [PubMed] [Google Scholar]
- 59.Bean B, Moore BM, Sterner B, Peterson LR, Gerding DN, Balfour HH., Jr 1982. Survival of influenza viruses on environmental surfaces. J. Infect. Dis. 146:47–51 [DOI] [PubMed] [Google Scholar]
- 60.Soave O, Brand CD. 1991. Coprophagy in animals: a review. Cornell Vet. 81:357–364 [PubMed] [Google Scholar]
- 61.Centers for Disease Control and Prevention 2010. Interim guidance on infection control measures for 2009 H1N1 influenza in healthcare settings, including protection of healthcare personnel. Centers for Disease Control and Prevention, Atlanta, GA [Google Scholar]
- 62.DeLano WL. 2002. The PyMOL molecular graphics system, version 1.5.0.4. Schrödinger, LLC, New York, NY [Google Scholar]
- 63.Lin T, Wang G, Li A, Zhang Q, Wu C, Zhang R, Cai Q, Song W, Yuen KY. 2009. The hemagglutinin structure of an avian H1N1 influenza A virus. Virology 392:73–81 [DOI] [PubMed] [Google Scholar]