Abstract
H5N1 influenza viruses pose a pandemic threat but have not acquired the ability to support sustained transmission between mammals in nature. The restrictions to transmissibility of avian influenza viruses in mammals are multigenic, and overcoming them requires adaptations in hemagglutinin (HA) and PB2 genes. Here we propose that a further restriction to mammalian transmission of the majority of highly pathogenic avian influenza (HPAI) H5N1 viruses may be the short stalk length of the neuraminidase (NA) protein. This genetic feature is selected for when influenza viruses adapt to chickens. In our study, a recombinant virus with seven gene segments from a human isolate of the 2009 H1N1 pandemic combined with the NA gene from a typical chicken-adapted H5N1 virus with a short stalk did not support transmission by respiratory droplet between ferrets. This virus was also compromised in multicycle replication in cultures of human airway epithelial cells at 32°C. These defects correlated with a reduction in the ability of virus with a short-stalk NA to penetrate mucus and deaggregate virions. The deficiency in transmission and in cleavage of tethered substrates was overcome by increasing the stalk length of the NA protein. These observations suggest that H5N1 viruses that acquire a long-stalk NA through reassortment might be more likely to support transmission between humans. Phylogenetic analysis showed that reassortment with long-stalk NA occurred sporadically and as recently as 2011. However, all identified H5N1 viruses with a long-stalk NA lacked other mammalian adapting features and were thus several genetic steps away from becoming transmissible between humans.
INTRODUCTION
Since the first documented lethal outbreak in humans of highly pathogenic avian influenza (HPAI) H5N1 virus in 1997, more than half of the people with confirmed infection have died (1). Although the case fatality rate may be much lower in a pandemic scenario, there is reason to worry that a pandemic caused by an H5N1 influenza virus could be severe. Currently, H5N1 viruses that have evolved in nature demonstrate limited or no transmission from person to person (2), indicating that host range barriers have so far prevented an H5N1 pandemic. Understanding the exact nature of the host range barriers may aid in the prediction of and preparation for future influenza pandemics.
Influenza A virus is a lipid-enveloped virus with an eight-segment negative-sense RNA genome. A balance between the activities of the two surface glycoproteins hemagglutinin (HA) and neuraminidase (NA) is deemed crucial for virus replication and transmission (3, 4). The paradigm is that infection is initiated when HA binds the cell surface receptor sialic acid (SA) and completed when NA cleaves SA from the surface of the same cell, thus allowing progeny particles to be released and disperse (5).
Most efforts to understand why H5N1 does not transmit between people have focused on the receptor binding specificity and stability of the H5 HA protein (6–18). Avian influenza virus HAs bind α2,3-linked sialic acid (α2,3 SA) receptors that are abundant in the avian enteric tract but sparse in the upper respiratory tract of humans (10, 17, 19–24). Previous pandemic viruses have HA proteins that originated from an avian source but acquired several amino acid changes, which switched the receptor binding preference from α2,3-linked SA to α2,6-linked SA (25, 26). Although unnatural mutations that increase H5 HA binding to α2,6-linked receptors have been identified (7, 8, 18) and some currently circulating H5 HAs in birds appear to have evolved an increased capacity for α2,6 SA binding (17), all naturally occurring H5 HAs still maintain a higher affinity for α2,3-linked receptors, and this phenotype likely limits their transmissibility between humans (23, 24). Mutations in PB2 have also been shown to be important for transmission of avian influenza viruses in mammals (11, 27, 28). In addition to these high barriers for HA and PB2 adaptation, it is likely that other genes of the avian virus limit its ability to transform into a circulating human pathogen.
Recent panzootic H5N1 influenza viruses emerged from wild birds in Southeast Asia. Influenza A/Goose/Guangdong/1/96 (GsGd96) virus is the lineage-defining strain for both the HA and NA of currently circulating H5N1 viruses, and this strain had six basic amino acids at the HA cleavage site, a genetic feature associated with HPAI virus. Sequencing of viruses from the 1997 outbreak of HPAI H5N1 in humans and poultry revealed that compared with the GsGd96 NA, the NA of the 1997 outbreak viruses had a 19-amino-acid (aa) deletion in its stalk region (20, 29, 30). NA stalk truncation occurs following transmission of influenza viruses in poultry farms (20, 31) and also during experimental passage of virus from wild aquatic birds to gallinaceous poultry (chickens or turkeys) (32–34). The 1997 H5N1 virus lineage was effectively “stamped out,” but H5N1 viruses reemerged in 2003 with a new genetic constellation named “genotype Z.” The 2003 H5N1 viruses derived their HA and NA gene segments from the GsGd96 lineage, while the internal genes, which originated from other avian influenza viruses, were gained through reassortment (35). Early isolates of genotype Z retained the multibasic cleavage site (MBCS) in HA and possessed a long-stalk-length NA, including the human H5N1 isolate A/HongKong/213/03. However, HPAI H5N1 viruses with a 20-aa stalk truncation in NA rapidly emerged and subsequently spread across Asia, Europe, and Africa (36, 37). According to Li et al., 99% of HPAI H5N1 viruses isolated between 2003 and 2011 had NA with a short stalk (38).
Several groups have used reverse genetics to demonstrate that NA stalk length affects the biological properties of influenza viruses. NAs with different stalk lengths have similar enzyme kinetics when cleaving single-valent substrates (39–41). In contrast, when the substrate is multivalent, such as when it is presented on red blood cells (RBCs), a short stalk length reduces the rate of viral elution (39–43). NA stalk truncation enhances replication and virulence of influenza virus in eggs and chickens (32, 34, 40, 43), explaining why it has emerged during poultry passage. A short NA stalk had various effects on replication in cell culture; in A549 cells, viruses with short-stalk NAs grew to higher titers, while the opposite was observed in Madin-Darby canine kidney (MDCK) cells (9, 43). Both Zhou et al. and Matsuoka et al. found that virulence in mice was enhanced for viruses with a truncated NA stalk compared to their equivalents with a long stalk (39, 43).
The selective force for NA truncation in gallinaceous hosts is not yet clearly elucidated, but NA stalk deletion is often coupled with increased HA glycosylation, which has been shown to reduce receptor binding affinity (20, 29, 31, 44). Mutations in HA or NA often drive compensatory change in the other gene in order to conserve the critical balance in activities relative to SA expression in the target tissue.
Evidence that NA plays an important role in viral entry is building. For example, in highly differentiated cultures of human airway cells, the NA inhibiting the drug oseltamivir reduced the efficiency with which virus could initiate infection (45), and we previously showed that deficiencies in the capacity of an avian influenza virus to spread through culture at low temperatures mapped to the NA gene (46). Whether these functions underlie the role of NA in supporting transmission is not presently clear (4, 47).
The primary site of replication of human influenza viruses is the upper respiratory tract (22, 48, 49). The nasal mucosa, which is cooled by inhaled air, has a mean temperature between 30°C and 34°C (50). Avian influenza viruses replicate optimally at higher temperatures than human viruses (51). We previously showed that an NA from an avian virus restricted the ability of a human-avian reassortant influenza virus to spread in cultures of human airway epithelial (HAE) cells at 32°C (46). This NA, derived from an H7N1 HPAI virus, had a short stalk. Mucus-secreting goblet cells are abundant in the human upper respiratory tract, and secreted mucus forms a glycan-rich layer that covers the apical surface of airway epithelial cells. The main components of mucus are mucins, which are large complex glycoproteins with multiple sialic acid moieties that can act as decoy receptors (52, 53). For influenza virus to penetrate to the apical surface of target epithelium, it may be necessary for the viral NA to desialate the mucus barrier. Our previous finding that virus with avian NA did not spread efficiently through HAE cell cultures (46) might be explained if avian virus NAs with short stalks were less competent for this function, especially at cool temperatures.
In this study, we used viruses generated by reverse genetics to explore the effect of stalk length on viral replication and transmission. Here we show that in the context of an otherwise transmission-competent prototypic pandemic H1N1 virus, the NA from an HPAI H5N1 virus reduced transmission via respiratory droplets (RD) between ferrets, and this was due to its short stalk length. Furthermore, we show that low transmissibility of virus with a short-stalk NA might be partially accounted for by a reduction in the ability to cleave tethered substrates and penetrate through the mucus barrier.
MATERIALS AND METHODS
Ethics statement.
All work performed was approved by the local genetic manipulation (GM) safety committee of Imperial College London, St. Mary's Campus (center number GM77), and the Health and Safety Executive of the United Kingdom. All animal research described in this study was carried out under a United Kingdom Home Office License, PPL/70/6643. Human nasal airway epithelial (HNE) cells were obtained from patients undergoing surgical nasal polypectomy and used to create cell cultures by Epithelix Sarl following the guidelines set out in the Declaration of Helsinki on biomedical research (Hong Kong amendment, 1989). Epithelix also follows ethical guidelines in accordance with French Biobanks, which are governed by a “nonproperty” principle and require approval by a local ethics committee at each collection center, plus written informed consent from each donor, and maintenance of data confidentiality.
Bioinformatics and phylogenetic trees.
The NA stalk domain was considered to begin at aa 39, which is the first variable amino acid after the transmembrane domain ends, and end at aa 91 (N1 numbering), just before a conserved cysteine that forms a disulfide bond with another cysteine in the head domain to make a large loop (54) (Fig. 1). Therefore, the most frequent stalk length of a human influenza virus NA is 53 aa, and the length of the H5N1 NAs with a 20-aa deletion is 33 aa. Nucleotide and amino acid alignments for Fig. 1 were performed using Geneious with default options and manual adjustment (Geneious Pro, version 5.6.3).
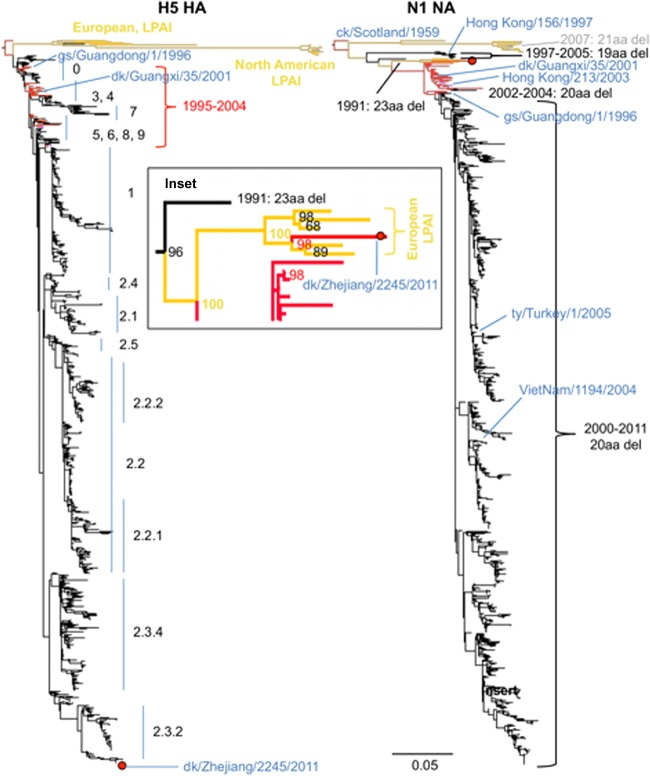
Fig 1.
Sequence alignment of human, avian, and engineered NAs. Sequences of N1 NA are shown by full-length amino acid sequence (A), nucleotide sequence of region covering stalk deletion (B), and amino acid sequence of stalk region (C). The first sequence, A/England/195/2009 (E195 NA), is the natural full-length sequence of a prototypic pandemic NA, followed by the natural sequence from A/turkey/Turkey/1/05 NA (SStyNA), from which nucleotides 145 to 204 are deleted. The third sequence (ck/JilinNA) is from the N1 NA of A/chicken/Jilin/hl/04 virus and was the sequence, without a stalk deletion, found in GenBank to have the highest nucleotide identity with SStyNA. The final sequence (LStyNA) was engineered by inserting nucleotides 145 to 204 from ck/JilinNA into SStyNA. Amino acids are colored as bars in panel A and block outlined in panel C where they differ among the NA sequences in this set (blue, positively charged; red, negatively charged; green, polar; yellow, nonpolar). Nucleotides in panel B are block outlined in gray where E195 NA differs from ck/JilinNA. The green bar at the bottom shows the length of the stalk domain.
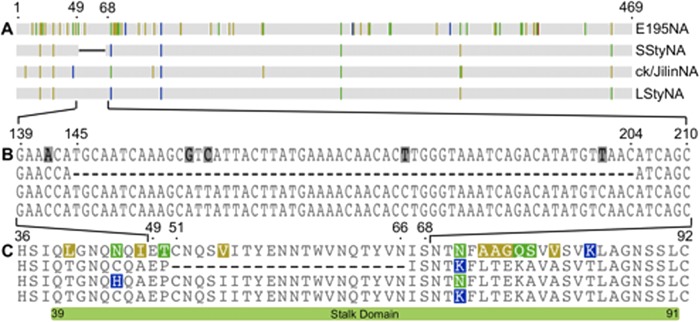
For Table 4, Fig. 7, and Fig. S1 in the supplemental material, full-length coding of HA and NA H5N1 nucleotide sequences from any host, location, and year were downloaded from the NCBI influenza virus resource database (55). Duplicate isolates, isolates from environmental samples, unknown avian (and blowfly) samples, and poor-quality isolates (multiple ambiguities) were removed, leaving a total of 1,150 matched HA and NA sequences. Alignments were performed in MUSCLE in MEGA 5.05 (56), with manual adjustments. After alignment, the sequence data were processed in R utilizing packages ape and seqinr. Phylogenetic trees were estimated using RAxML (57) with the GTR+Γ substitution model (general time reversible plus discretized gamma distribution of rates over sites) and 100 bootstraps. Trees were displayed and colored according to pathogenicity and stalk length annotations using FigTree (58).
Table 4.
HPAI H5N1 influenza viruses isolated after 1995 for which paired HA and NA sequences were available from different hosts with short- or long-stalk NA genesa
| Host | No. (%) of viruses |
||||||
|---|---|---|---|---|---|---|---|
| Avian—Anseriformes | Avian—Galliformes | Avian—other | Human | Swine | Other mammals | Total | |
| H5N1 with MBCS | 425 | 404 | 105 | 159 | 20 | 14 | 1,127 |
| SSNA | 395 (93) | 396 (98) | 101 (96) | 157 (99) | 16 (80) | 14 (100) | 1,079 (96) |
| LSNA | 30 (7) | 8 (2) | 4 (4) | 2 (1) | 4 (20) | 0 (0) | 48 (4%) |
Short-stalk NA genes predominate (96%) within this data set of HPAI H5N1 influenza viruses. Four percent of HPAI H5N1 viruses have long-stalk NA genes that were acquired through reassortment. HPAI H5N1 viruses with long-stalk NA are more common in Anseriformes than in Galliformes. “Avian—other” for long-stalk NA include 2 Ciconiiformes, 1 Passeriform, and 1 Falconiform. MBCS, multibasic cleavage site (2 or more, usually 5 or 6, basic amino acids).
Fig 7.
NA and HA maximum likelihood phylogenetic trees. Maximum likelihood phylogenetic trees were constructed from 1,150 paired H5N1 full-length sequences. The HA tree (left) shows that HPAI H5N1 viruses with long-stalk NAs are mostly isolates that belong to early clades (0, 3, 4, 5, 6, 7, 8, and 9) and one isolate from clade 2.3.2. The NA tree (right) shows that stalk truncation has occurred five times in this data set (annotated in gray and black, with the year of the earliest virus isolate and number of amino acids that were deleted), while stalk elongation was not observed. Taxon names have been removed for clarity (see Fig. S1A and B in the supplemental material for full virus names). Branch colors are as follows: red, avian HPAI LSNA; pink, mammalian HPAI LSNA; gold, avian LPAI LSNA; black, avian and mammal HPAI SSNA; gray, avian LPAI SSNA. Years indicate the date of virus isolation. The inset shows that the LSNA of dk/Zhejiang/2245/2011 was most closely related to NAs within the European LPAI clade. Inset nodes are labeled with bootstrap values. Virus names of interest and HA clades are noted. Dk/Zhejiang/2245/2011 is indicated with a red dot. del, deletion.
Cells.
Madin-Darby canine kidney (MDCK) cells (ATCC) were maintained in Dulbecco modified Eagle medium (DMEM; Gibco-Invitrogen, Inc.) supplemented with 10% fetal bovine serum (Biosera, Inc.), 1% penicillin-streptomycin (Sigma-Aldrich, Inc.), and 1% nonessential amino acids (Sigma-Aldrich, Inc.). HNE cells were obtained from Epithelix Sarl and cultured by following the manufacturer's protocol.
Plasmids and recombinant viruses.
The influenza virus A/England/195/09 (E195) is typical of H1N1 2009 pandemic strains (59). The virus was isolated from the nose swab of a sick individual who returned to England from Mexico in April 2009. E195 was sequenced by the Health Protection Agency, UK (HPA), GenBank (GQ166654 to GQ166661). Gene sequences were designed in silico using Geneious, version 5.5, according to methods published previously (60), so that each segment of influenza viral genome was flanked by a human RNA polymerase promoter I and a ribozyme. Sequences were synthesized by GeneArt (now LifeTechnologies) and inserted into plasmid pMA or pMK.
Influenza A/turkey/Turkey/1/2005 virus (ty05), a clade 2.2.1 HPAI H5N1 virus, is representative of the clade of viruses that caused a panzootic H5N1 outbreak in Europe in 2005. The rescue plasmid for ty05 NA (GenBank EF619973) was a kind gift from Ron Fouchier (Erasmus University). This NA had naturally become truncated by 20 aa and thus is a short-stalk NA (SStyNA). To elongate the stalk, a protein sequence search of ty05 NA was performed in Geneious. Of the 100 sequences returned, only 34 had full-length stalks. To find the genetic sequence with closest identity to ty05 NA, nucleotide sequences of the seven top matches with a full-length stalk were aligned with ty05 NA. The sequence for A/chicken/Jilin/hl/2004 (ck/Jilin/04) proved to be most similar, with 97.2% identity. To make LStyNA, site-directed mutagenesis was performed on the ty05 NA plasmid to insert the equivalent nucleotides from ck/Jilin/04. Primer sequences are available upon request.
Viruses were generated using the reverse-genetics coculture rescue technique described previously (61), and titers of viral stocks were determined by plaque assay. Briefly, virus was serially diluted 10-fold in duplicate and allowed to bind MDCK cells in a 12-well plate for 1 h at 37°C. The inoculum was removed, and Avicel (RMC BioPolymer Corp.) (62) in overlay medium with final concentrations of 1× MEM, 0.21% bovine serum albumin (BSA) V, 1 mM l-glutamate, 0.15% sodium bicarbonate, 10 mM HEPES, 1× penicillin-streptomycin (all from Gibco), and 0.01% dextran DEAE (Sigma) plus 1.4 μg/ml tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-treated trypsin (Lorne Laboratories) was added on top of the cells. Cells were then incubated for 3 days at 37°C to allow plaque formation, which was detected after fixing with 50:50 methanol-acetone (VWR) and staining with primary antibody raised against influenza nucleoprotein (NP) (clone H7 MAB 2F6-C9, provided by the Health Protection Agency London) and secondary antibody, goat anti-murine polyclonal IgG–β-galactosidase (IgG–β-Gal; (AbD Serotec), and developing blue cells with cyanide buffer and 5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside (X-Gal) substrate (Sigma).
Viral growth curves.
Multicycle growth curves were performed with cells incubated at 32°C. MDCK cells at 70% confluence were inoculated in triplicate with each virus at a multiplicity of infection (MOI) of 0.01 and incubated for 1 h, after which the inoculum was removed, cells were washed with phosphate-buffered saline (PBS) three times, and 1 ml of serum free medium with 1.2 μg/ml of TPCK-treated trypsin (Lorne Biolabs) was added before returning the cells to incubate for specified periods. At each sampling time point, 1 ml of medium was removed and replaced afresh.
For growth curves in HAE cells, accumulated mucus was first washed from the apical surface, by twice adding 200 μl of DMEM and incubating the cells for 30 min before removal. Next, triplicate wells of cells were inoculated with each virus at an MOI of 0.01 and incubated for 1 h. Cells were washed twice before reincubation at 32°C. Samples were collected at predetermined time points in 300 μl of DMEM, after incubation for 30 min. All samples were stored at −80°C with 0.35% BSA V (Invitrogen) until a plaque assay was performed with MDCK cells as described above to determine viral titer.
Data were analyzed using Prism GraphPad, version 5.0, and statistical significance was determined by one-way analysis of variance, followed by Bonferroni's multiple-comparison test to determine significance between pairs.
Transmission model.
Animal studies were performed as described previously (48, 63). Female ferrets (20 to 24 weeks old) weighing 650 to 1,100 g were obtained from a designated supplier. After acclimatization, sera were obtained and tested by microneutralization (MN) assay against the 7 plus 1 viruses used in the study, all of which had the HA of A/Eng/195/2009, the predominant circulating human influenza virus at the time of experimentation. All ferrets were negative for pH1N1 2009 influenza antibodies at the start of the experiments (MN titer < 10).
In each experiment, four donor ferrets were inoculated intranasally, under light anesthesia using ketamine (22 mg/kg) and xylazine (0.9 mg/kg), with 1 × 106 PFU of virus in 200 μl, on day zero. Twenty-four hours after inoculation, one direct-contact (DC) ferret was cohoused with each donor and one respiratory droplet (RD)-exposed ferret was housed in a cage adjacent to each donor cage, separated by two dividers, 10 cm apart with holes 3 mm in diameter. All animals were weighed and subjected to nasal washing daily either until four consecutive days of no virus shedding or for 15 days in total after the first exposure day, by which time no virus was detected. The nasal wash (NW) was plaqued on the day of collection in MDCK cells as described above. The limit of viral detection was 10 PFU/ml of nasal wash. Strict protocols were followed to prevent cross-contamination between animals during all procedures, as previously described (48). Terminal blood samples, collected 21 days postexposure, were tested for seroconversion by MN assay using the respective challenge virus for each experiment.
Sera were heat inactivated for 30 min at 56°C. MN assay was performed on MDCK cells that were plated in 96-well tissue culture plates (Greiner) and challenged in triplicate, by incubation overnight (37°C and 5% CO2) with 5 × 104 PFU/well of virus in the presence of 2-fold dilutions of sera from 1/10 to 1/1,280 in viral diluent (DMEM [Gibco] plus 10 mM penicillin-streptomycin [Invitrogen] plus 0.35% BSA V [Invitrogen]). Cells were fixed and stained as described above. Ferrets were considered seronegative if all three wells with serum diluted 1/10 were positive for infected cells. A ferret was considered seropositive when no infected cells were found in the any of the three wells with serum diluted 1/20 or further, indicating that seroreactivity had increased from an MN titer of <10 to ≥20.
Neuraminidase enzyme activity assays.
NA enzyme activity was measured using the small soluble substrate 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA; Sigma) as previously described (64). Viruses were first diluted in the presence of a standard amount of substrate in order to determine a viral dilution that would yield approximately equal amounts of product per reaction over 1 h. To assay the reaction rate, the substrate was serially diluted in triplicate 2-fold in 2-[N-morpholino]ethanesulphonic acid (MES; Sigma) assay buffer over seven wells, so that the most concentrated well had 50 μl of 150 μM MUNANA and the eighth well had only buffer, used as a baseline. Equivalent volumes of diluted virus were added to each well. The assay was performed in black, flat-bottom, 96-well Matrix microplates (Thermo) at 32°C. A test was deemed successful if the R2 value was >0.9. A Fluostar Omega (BMG Labtech) was used to measure UV fluorescence emission every 4 min, for 60 min, with a 355-nm excitation filter and 460-nm emission filter. Omega MARS software (BMG Labtech) was used to calculate the Km and Vmax of each virus using the Michaelis-Menten equation. Three different preparations of each virus were tested in three different experimental runs to determine the mean values and standard deviations. Statistical significance was determined using t test followed by Bonferroni correction for multiple measurements.
Erythrocyte elution assays were performed either by using concentrated virus stocks or by diluting each virus to equal hemagglutination titers (16 hemagglutination units [HAU]) and then diluting them in 2-fold steps across a 96-well, V-bottomed microtiter plate (Greiner) and mixing them with PBS containing chicken or human red blood cells so that they were at a final concentration of 0.5%. After incubation for 1 h at 4°C, the plate was moved to 32°C and elution was observed every 20 min. Virus was deemed to have eluted from RBCs when a pellet became visible. Elution tests were performed in duplicate or triplicate, and the data shown are representative of three experiments. The percentage of HA titer remaining at each time point compared to the start was plotted.
To visualize virion aggregation, HNE cells were infected, in triplicate, at an MOI of 20 of either SStyNA or LStyNA virus, while three negative-control wells were left uninfected. Twenty-four hours postinfection, released virions were harvested from the apical surface of the cells by incubation with 50 μl of DMEM (Gibco) for 15 min. Electron microscopy (EM) was performed using standard methods as described previously (65). In brief, virions from a 5-μl drop of apically exposed DMEM were adhered to a freshly glow-discharged 400-mesh hexagonal grid coated with a Formvar film, washed in water, and then negatively stained with uranyl acetate. Virions were identified by the presence of an array of spike proteins on spherical or filamentous objects. Virus particles were counted either as aggregated (when clearly touching another virus particle) or in singlet form (when a particle was not touching any other virus particles). Virus particles in over 10 fields of view at a ×11,500 magnification were counted per well, viewed using an FEI Tecnai G2 electron microscope (FEI) with a Soft Imaging System Megaview III charge-coupled device camera. Images were collected at a ×120,000 magnification, using ANALYSIS version DOCU software and Olympus SI Viewer (both from Olympus Soft Imaging Solutions), and prepared for publication using Graphic Converter X (Lemkesoft, version 6.7.7).
To measure the effect of mucus on viral infectivity, mucus was collected from the surface of HNE cells and stored at 4°C. Virus was incubated at 4°C for 1 h either with mucus diluted 70-fold in virus diluent (PBS plus 0.35% BSA V; Gibco) or with virus diluent without mucus. The cool incubation temperature was used to allow viral HA to bind terminally sialated glycans while preventing viral NA from cleaving them. The virus with or without mucus was then added to MDCK cells and incubated for 120 min at 32°C. At the end of the incubation, cells were thoroughly washed with PBS and plaques were developed as described above. Mucus inhibition of viral infectivity was performed in triplicate and normalized to virus infectivity in the absence of mucus. The triplicate experiment was repeated on a separate date, and the data (n = 6) were aggregated.
Statistical analysis.
All statistical analyses were performed using Prism 6 software (GraphPad). Viral titers from growth curves were normalized by taking the log10 of each measurement, and then comparisons were made using a repeated-measure two-way analysis of variance (ANOVA) with Tukey's multiple-comparison test. The data were considered as one family, and titers of each virus were compared at each time point for a total of 12 comparisons. Samples collected from the same well were considered matched. Area-under-the-curve (AUC) comparisons from NW titers were also made on log10-normalized values using a repeated-measure two-way ANOVA, recognizing that virus shed from ferrets of the same group were matched. All AUC values were considered as one family, and three comparisons were made between SStyNA and LStyNA, one for each exposure route: inoculation, DC, and RD. Bonferroni's multiple-comparison test was used to determine P values for each comparison. Comparisons for first day and total days of virus shed were also made using the same method as used for AUC comparisons, except for the first day of shedding for RD ferrets, for which a comparison could not be made. Comparisons between Km, Vmax, and viral input into MUNANA assay as well as mucus inhibition of infectivity were made by one-way ANOVA with Tukey's multiple-comparison test. Statistical comparison of virion aggregation was made using an unpaired t test assuming equal standard deviation.
RESULTS
In primary airway epithelial cell culture, replication of a virus with a short-stalk NA is attenuated compared to that of viruses with a long-stalk NA.
The stalk region of human influenza viruses' NA is about 50 aa long (66) and is hereafter termed a long stalk (Fig. 1). Li et al. showed that the vast majority of NAs from avian influenza H5N1 viruses have a stalk deletion of 20 aa, which is hereafter termed a short stalk (38).
To investigate the effect of stalk length of an avian N1 NA on viral phenotype, we used reverse genetics to generate viruses that had seven gene segments from a prototypic strain of pandemic H1N1 influenza virus A/England/195/09 (E195) (63), plus segment six from the clade 2.2.1 HPAI H5N1 virus A/turkey/Turkey/1/05 (ty05). Like for the overwhelming majority of the contemporary H5N1 H5 viruses, the NA of ty05 has a short stalk with the 20-aa deletion that predominates throughout genotype Z viruses. This wild-type form of ty05 NA was termed SStyNA. To create a long-stalk NA (LStyNA), nucleotides encoding the stalk region of the NA from a close genetic relative with a full-length stalk, A/chicken/Jilin/hl/04, were engineered into the ty05 NA plasmid (Fig. 1). Wild-type E195 virus (wtE195), with its cognate NA (E195 NA) that has a long stalk, was also generated. The sequences of E195 NA and LStyNA differed by 56 aa: 8 in the transmembrane domain, 14 in the stalk domain, and 34 in the head domain.
NA stalk length has been shown to have various effects on viral growth in cell culture. Under multicycle conditions in MDCK cells at 32°C, we found that LStyNA showed increased replication over SStyNA virus, with log mean differences of 0.66 (95% confidence interval [CI], 0.11 to 1.21; P < 0.01) and 0.89 (95% CI, 0.34 to 1.44; P < 0.001) at 24 and 48 h postinfection (hpi), respectively (Fig. 2A). Primary human airway epithelial cell cultures offer a more physiologically relevant cell culture system for comparison of influenza virus growth because they are multilayered, differentiated, and polarized, have ciliated and nonciliated cells, and secrete mucus onto their apical surface, which is exposed to air. In primary cultures of human nasal airway epithelial cells (HNE cells) at 32°C, both wtE195 and LStyNA viruses grew to higher titers than SStyNA virus, with the greatest log mean difference between LStyNA and SStyNA being 2.03 (95% CI, 1.20 to 2.86, P < 0.0001) at 48 h hpi (Fig. 2B).
Fig 2.
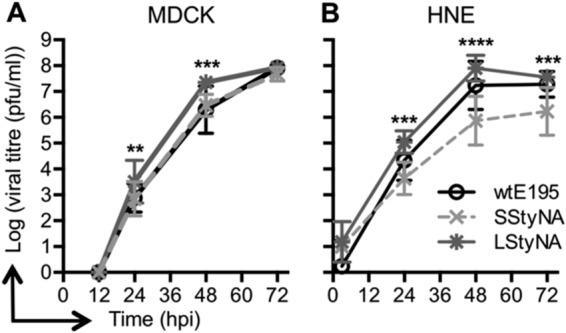
Multicycle virus replication of SStyNA is attenuated in cell culture. Multicycle virus replication was assessed in MDCK cells (A) and HNE cells (B) both at 32°C following infection at an MOI of 0.01. The mean viral titer of each virus (n = 3) is indicated with a symbol, and error bars represent 95% confidence intervals. Note that the 95% confidence intervals for LStyNA at 48 and 72 hpi in MDCK cells and at 72 hpi in HNE cells do not show because they were very small. Asterisks indicate the P values for the differences between SStyNA and LStyNA: **, P < 0.01; ***, P < 0.001; ****, P < 0.0001.
Respiratory droplet transmission in ferrets is limited by a short-stalk NA.
Previously, we showed that recombinant E195 virus generated by reverse genetics transmitted to 3/3 ferrets via respiratory droplets (63). Others have reported a rate of 66% to 100% for respiratory droplet transmission using similar prototypic pandemic viruses in ferrets (47, 67–70). To determine whether introduction of the avian N1 NA would affect transmission and if stalk length would influence this, four ferrets were inoculated intranasally with 1 × 106 PFU of either SStyNA or LStyNA virus in 200 μl of PBS, and 24 h later, a direct-contact (DC) ferret was cohoused with each donor, while a RD-exposed ferret was housed in an adjacent cage, separated by perforated panels. Ferrets were subjected to nasal washing daily, and plaque assays were performed to determine the viral titer shed in the nasal wash (Fig. 3).
Fig 3.
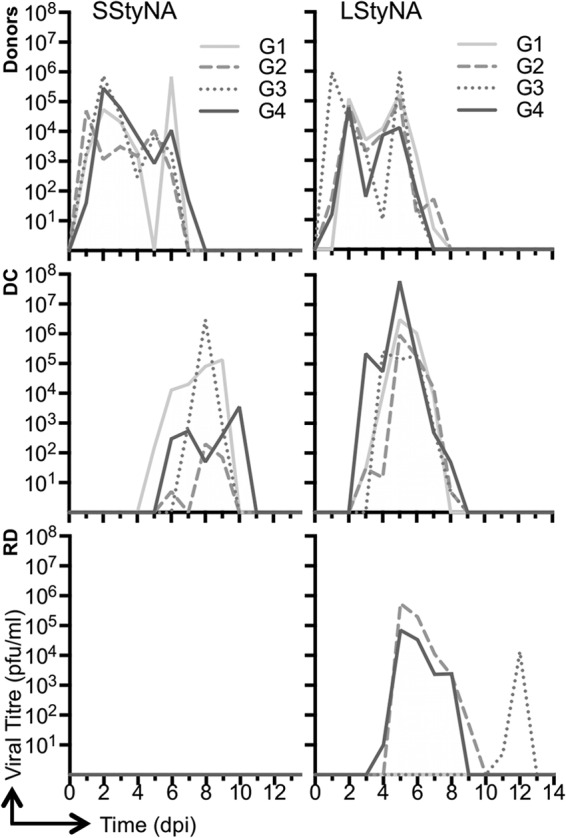
Short-stalk NA limits influenza virus transmission in ferrets. Donor ferrets were inoculated with 106 PFU of either SStyNA (Red) or LStyNA (Blue) on day zero and housed in separate cages. The day after inoculation, one DC ferret was cohoused with each donor and one RD ferret was housed in an adjacent cage separated by two perforated panels. Viral titer from nasal wash was determined daily by plaque assay. dpi, days postinfection. “G” refers to one donor, one DC, and one RD-exposed ferret in shared or adjoining cages, respectively.
Both SStyNA and LStyNA viruses were shed by all inoculated donors and all DC-exposed animals. Ferrets inoculated with SStyNA or LStyNA virus shed similar amounts of infectious virus, as determined by calculating the mean area under the curve (AUC), 5.0 × 105 (PFU × days)/ml (PFU multiplied by days per ml averaged per group) for SStyNA or 6.3 × 105 (PFU × days)/ml for LStyNA, over 6 or 6.3 days, respectively. Figure 3 shows the amount of virus detected daily in the NWs from individual ferrets, and Table 1 shows the mean differences with 95% CIs and P values. However, DC ferrets infected with the SStyNA virus shed less virus, over a shorter period, than LStyNA virus-infected DC animals. SStyNA virus-infected DC animals shed, on average, 8.1 × 105 (PFU × days)/ml for a mean of 4 days, while DC ferrets infected with the LStyNA virus shed, on average, 1.7 × 107 (PFU × days)/ml for a mean of 5.3 days. Although these differences were not statistically significant, they showed a trend that related a shorter NA stalk length to reduced viral shedding by ferrets infected through DC transmission. Additionally, the first day of shedding by DC ferrets exposed to the SStyNA virus was delayed by an average of 2.75 days compared to that for the DC ferrets exposed to the LStyNA virus, and this difference was statistically significant. Furthermore, although three of the four ferrets exposed by RD to the LStyNA virus acquired infection, no virus was detected in the nasal wash of any of the ferrets similarly exposed to the SStyNA virus (Fig. 3, bottom graphs).
Table 1.
Mean difference between amounts of virus shed, day virus was first shed, and number of days that virus was shed from ferrets after exposure to LStyNA in comparison to SStyNAa
| Exposure route | Log AUC, PFU × days/ml (95% CI) | 1st day (95% CI) | Total days (95% CI) |
|---|---|---|---|
| Inoculation | −0.06 (−2.63 to 2.52) | −0.25 (−1.23 to 0.73) | 0.25 (−2.06 to 2.56) |
| DC | 2.06 (−0.50 to 4.64) | 2.75 (1.77 to 3.73)**** | 1.25 (−1.06 to 3.56) |
| RD | 3.76 (1.19 to 6.33)** | N/A | 3.00 (0.69 to 5.31)** |
PFU × days/ml, PFU multiplied by days per ml averaged per group (n = 4); 1st day, first day virus was shed postinoculation or postexposure, averaged by group; total days, total number of days that virus was detected in the nasal wash, averaged by group; N/A, not applicable. **, P < 0.01; ****, P < 0.0001.
Microneutralization (MN) assays performed on serum collected preexposure showed that all ferrets were seronegative (MN titer < 10) for the challenge virus before the experiment. A second serum sample was collected 21 days after the first day of exposure. All ferrets that were virally positive by nasal wash were found to seroconvert (MN titer ≥ 320). Although none of the ferrets that were exposed via RD to the SStyNA virus were virologically positive, one seroconverted, but with a low MN titer (MN titer = 20). The three ferrets that shed virus following exposure via RD to the LStyNA virus were seropositive (MN titer > 1,280), and the one ferret that did not shed virus remained seronegative (MN titer < 10) (Table 2).
Table 2.
Seroconversion of ferrets upon exposure to virus with short- or long-stalk NAa
| Virus | No. of ferrets which showed seroconversion/total |
||
|---|---|---|---|
| Inoculated ferrets | DC ferrets | RD ferrets | |
| SStyNA | ND | 2/2 (1 had an MN titer of 320; 1 had an MN titer of 640) | 1/4 (3 had an MN titer of <10; 1 had an MN titer of 20) |
| LStyNA | 4/4 (all had an MN titer of >1,280) | 4/4 (all had an MN titer of >1,280) | 3/4 (3 had an MN titer of >1,280; 1 had an MN titer of <10) |
Sera were collected both before and 21 days after inoculation or exposure. All ferrets were serologically negative (MN titer < 10) by MN assay before the experiment. One ferret exposed via respiratory droplet to the SStyNA virus did not shed virus and yet seroconverted. ND, not done.
Ferrets were weighed daily, and none lost a significant amount of weight throughout the experiment. There was no significant difference in weight change between ferrets that were inoculated with or exposed to SStyNA or LStyNA virus.
Enzyme activity of NA to cleave complex substrates is limited by a short stalk.
To test whether the stalk length difference between SStyNA and LStyNA affected sialidase activity, an enzyme assay was performed using the small soluble substrate MUNANA. The amount of virus input for the assay was standardized so that equal amounts of NA enzymatic activity were assayed. Using this method of standardization required almost 10-fold more PFU per well of wtE195 virus than of either virus with tyNA (P < 0.05) (Table 3). wtE195 virus displayed a slightly higher Km and Vmax than those of either virus with tyNA, but only the Km difference was statistically significant between wtE195 and SStyNA (P < 0.05). Importantly, there was no significant difference between the Km or Vmax of the SStyNA and LStyNA enzymes, indicating that stalk length did not directly affect enzyme activity (Table 3).
Table 3.
Cleavage of a small soluble substrate (MUNANA) by viral NAa
| Virus | Km (μM) | Vmax (FU/s) | Virus (PFU/well) |
|---|---|---|---|
| SStyNA | 60 ± 14* | 96 ± 17 | 2.7 × 105 ± 1.7 × 10** |
| LStyNA | 86 ± 23 | 108 ± 38 | 3.0 × 105 ± 2.0 × 105* |
| wtE195 | 139 ± 31 | 133 ± 25 | 2.5 × 106 ± 4.0 × 105 |
Input of virus to achieve equivalent conversion of substrate was standardized by viral dilution after preliminary determination of NA activity. Results are given as the means ± standard deviations from three independent determinations on triplicate samples where the R2 was >0.98. The differences between SStyNA and LStyNA were not statistically significant in any comparison. When the difference between a wtE195 value and a value for SStyNA or LStyNA reached statistical significance, it is indicated by asterisks next to the SStyNA or LStyNA value: *, P < 0.05; **, P < 0.01. FU, fluorescent units.
To test the ability of NA to cleave SA from a more complex substrate than the untethered MUNANA, we performed an erythrocyte elution assay. This involved incubating viruses with red blood cells (RBCs) for 1 h on ice, which allowed the HA to bind sialated glycans, followed by incubation at 32°C, which allowed the NA to cleave SA and promote virion elution from the RBCs, resulting in a loss of hemagglutination. The heamagglutination reactions were programmed with 16 HAU of each virus. This equated to 2.57 × 106 PFU of SSTyNA virus, 2.93 × 106 PFU of LSTyNA virus, and 2.25 × 106 PFU of E195 virus. wtE195 and LStyNA viruses, which have long NA stalks, were fully eluted from the chicken RBCs after 1 and 24 h, respectively, while virus with SStyNA was not fully eluted from chicken RBCs even after 24 h (Fig. 4A). The elution assay was repeated using human RBCs. All three viruses were able to fully reverse the hemagglutination reaction; however, full RBC elution of virus with SStyNA took longer than that of its long-stalk equivalent (Fig. 4B). Thus, 16HAU of LStyNA virus was completely eluted in 20 min, at which time 8 HAU of SStyNA remained. Not until after 60 min of incubation at 32°C was SStyNA virus fully eluted.
Fig 4.
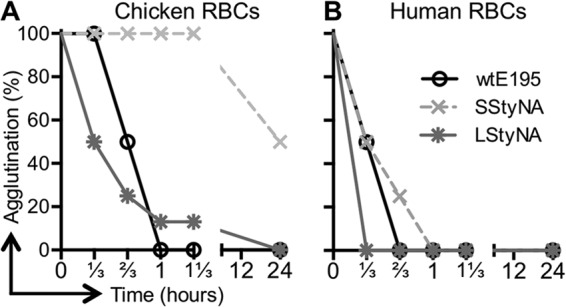
Viruses with short-stalk NA are eluted slowly from red blood cells. Concentrated viruses were diluted to equal HAU and then mixed with RBCs at 4°C to promote hemagglutination. After HA was established, the plate was moved to 32°C to promote NA enzyme activity. The loss of HA was assessed every 20 min and determined by the appearance of an RBC pellet. Experiments were performed three times with different batches of virus, and graphs are representative of the pattern seen with chicken (A) and human (B) RBCs.
NA plays a role in the release and dispersal of virus particles by disaggregating virions through cleaving SA from the glycoproteins on the virion surface, which HA would otherwise bind. To compare the efficiency by which virus with SStyNA and LStyNA achieved this, we visualized virus particles released following infection of HNE cell cultures by electron microscopy (Fig. 5A). Both viruses gave rise to spherical virions following HNE cell infection. The mean of three wells showed that SStyNA virions tended to aggregate in clumps. Only 25% (95% CI, 37 to 14%) of the particles with SStyNA were singlets, while the majority, 61% (95% CI, 73 to 50%) of the particles with LStyNA were observed as discrete virions. Observations of more than 450 particles per virus from three separately infected cell cultures over 10 fields of view indicated that the difference in the percent aggregation of released particles was statistically significant (P < 0.001) (Fig. 5B).
Fig 5.
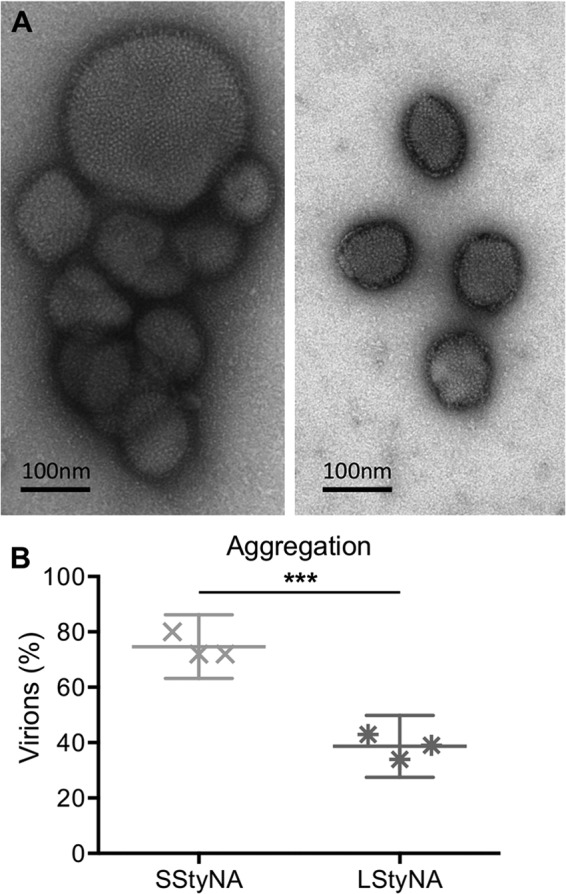
Virions with short-stalk NA aggregate more than virions with long-stalk NA. HNE cells were infected with either SStyNA or LStyNA virus (MOI of 20) and incubated at 32°C. Twenty-four hours later, released virions were collected in a small volume, negatively stained with uranyl acetate, and then visualized using an electron microscope. Virions were considered aggregated if two or more were clearly touching. (A) Representative EM images show that SStyNA virions tended to aggregate (left), and LStyNA virions did not (right). Supernatant from uninfected wells lacked virions (not shown). (B) The average percentage of virions aggregated determined by counting over 150 virions per well from three separate wells for each virus. Symbols represent individual wells; the middle line is the mean, and error bars denote 95% confidence intervals. ***, P < 0.001.
Inhibition of viral infectivity by mucus is more pronounced when virus has a truncated NA stalk.
Mucus contains many complex sialated glycans and has been proposed to act as an innate barrier to influenza virus infection by impeding viral access to the target epithelial cell layer. Previously we showed that incubating influenza viruses with mucus harvested from uninfected ferret nasal wash or from uninfected HNE cell cultures inhibited virus infectivity of MDCK cells (48). Those experiments were performed with virus and mucus at 4°C to prevent the NA enzyme digesting away the inhibitory sialic acid moieties. In the present study, we wished to assess the ability of different viral NA enzymes to overcome the inhibition of infectivity by mucus and to determine whether the stalk length of NA affected this phenotype. Mucus was collected from the apical surface of HNE cell cultures. Each virus was incubated at 32°C in the presence or absence of mucus and assayed for viral infectivity on MDCK cells, which do not secrete mucus. If NA was able to cleave receptor decoys within the mucus, then after incubation, a proportion of infectivity should be recovered. Infectivity remaining was normalized to that in the absence of mucus. Even after 2 h of incubation, only a very small amount, 11%, of SStyNA viruses were able to initiate infection in the presence of mucus (Fig. 6). In contrast, viruses with long NA stalks more readily overcame mucus inhibition: wtE195 virus recovered 54% and LStyNA virus recovered 40% infectivity. The difference in infectivity recovered by both viruses with full-length stalks compared to SStyNA virus was statistically significant (P < 0.0001). This experiment was also performed with shorter incubation times, and the same pattern was observed (data not shown).
Fig 6.
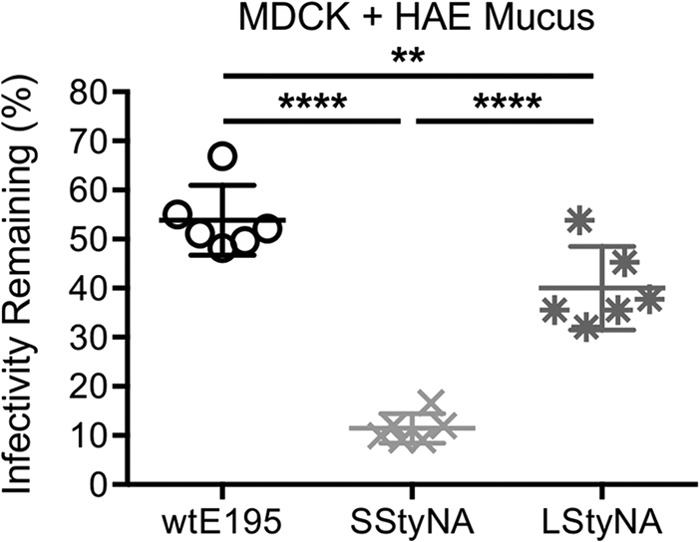
Mucus inhibits infectivity of virions with short-stalk NA more than long-stalk NA. Infectivity remaining was determined as the percentage of virions that infected MDCK cells (MOI, 0.00001) in the presence of mucus, compared to the absence of mucus, after 2 h of incubation at 32°C followed by plaque assay. Error bars denote 95% confidence intervals. **, P < 0.01; ****, P < 0.0001; n = 6.
Long-stalk HPAI H5N1 NAs are rare but detected.
Our data implied that a virus with a short-stalk N1 NA gene faced an additional barrier that would have to be overcome if such a virus were to cause a human pandemic. It was already clear that the overwhelming majority of H5N1 viruses were paired with SS NAs (38) (Table 4), but it was unclear which H5N1 clades contained the LS NAs. Maximum likelihood phylogenetic trees of paired H5N1 HA and NA sequences were generated, and HA clades were labeled (Fig. 7). Coloration of the trees according to the presence or absence of MBCS (red and black versus gold) and SS NA (black and gray) or LS NA (red) clearly shows that many LS N1 NAs were from the European and North American LPAI H5N1 clades (gold). Interestingly, most of the HPAI H5N1 viruses with an LS NA have HAs that belong to the early clades (0, 3, 4, 5, 6, 7, 8, and 9). H5N1 viruses of clade 2 are those that have increased host range and wide geographical spread. The only clade 2 HPAI H5N1 virus with an LS NA was isolated from a domestic duck in 2011 in Zhejiang Province, China. In summary, the HA tree showed that acquisition of an LS NA by a contemporary HPAI H5N1 virus through reassortment was incredibly rare but had occurred.
The NA tree reinforced the idea that stalk truncation events are infrequent but can lead to persistent lineages and showed that stalk truncation occurred five times within this data set: once within the North American LPAI H5N1 clade (labeled with gray text) and once each within four HPAI H5N1 clades (labeled with black text). Notably, the ty05 N1 NA used in this study had the 20-aa deletion that dominates contemporary HPAI H5N1 viruses. The NA tree also showed that the origin of the LS NA found in dk/Zhejiang/2245/2011 was from the otherwise LPAI European clade (see Fig. 7 inset).
Some HPAI H5N1 viruses with long-stalk NA had HA genes with mammalian adaptations, but all retained PB2 627E.
It is clear that genes other than the NA gene also play an important role in controlling influenza virus transmission, such as the HA and PB2 genes. Therefore, sequences of HA and PB2 from H5N1 viruses with LS NAs were searched for genetic traits that had previously been shown to associate with mammalian adaptation (9, 10, 67, 71). Lack of the glycosylation site at residue 158 (H3 numbering) in HA due to an N158D or T160A mutation has been shown to increase replication and transmission of H5N1 viruses in guinea pigs (11) and ferrets (67, 72) when H5 mutations that alter the receptor binding preference toward α2,6-linked SA are also present. Accordingly, an H5N1 virus with a long-stalk NA and lacking this glycosylation site might be one step closer to a mammal-transmissible phenotype. Interestingly, and perhaps of some concern, we found that most (94%; 45/48) of the H5N1 viruses that had long-stalk NA also lacked the HA glycosylation site from residues 158 to 160.
The only virus with long-stalk NA and an HA mutation associated with increased α2,6 SA receptor binding was A/Hong Kong/213/03, which had the mutation S227N (10, 73), but this virus was isolated from a human without further transmission and was shown not to transmit to RD-exposed ferrets (74). Examination of the 44 PB2 gene sequences available for viruses with long-stalk NA, including A/Hong Kong/213/03 and A/duck/Zhejiang/bj/2002, found that all had PB2 627E, rather than K, and therefore might show compromised virus replication and transmission in mammals (28, 75).
DISCUSSION
This study was designed to determine whether the truncated NA from an HPAI H5N1 virus limits RD transmission of an otherwise human H1N1 influenza virus in a ferret model and to explore the importance of stalk length to NA functions that counter human innate barriers to infection. We found that a recombinant virus, SStyNA, with an avian virus NA that has a short stalk combined with seven other gene segments from a transmissible prototypic 2009 pandemic virus had reduced growth in cell culture at 32°C. This was particularly pronounced in primary differentiated human nasal epithelial cell cultures that expressed mucus and recapitulated our previous observations that surface glycoproteins of avian influenza viruses limit virus spread in these cultures at temperatures of the upper airways (46). We found that differences in viral phenotypes conferred by short-stalk NA such as attenuated replication, inability to overcome mucus inhibition, and slower elution from red blood cells also occurred at 37°C (data not shown), but they were more readily detected at cooler temperatures, likely due to the slowing of enzyme kinetics. We also found that SStyNA virus was compromised in its transmission to exposed ferrets. SStyNA virus was transmitted to only one out of four RD-exposed ferrets. We attribute the defect in transmission largely to the shortened stalk length of NA because a second recombinant virus, LStyNA, that differed only by a 20-aa insertion into the stalk of its NA transmitted to three of four similarly exposed ferrets. Moreover, the one RD-exposed ferret that seroconverted following exposure to SStyNA-infected animals did not shed detectable virus in nasal wash, suggesting that a chain of RD transmission would not be supported for the SStyNA virus. Although SStyNA virus did transmit to cohoused animals, the amount of virus shed by recipient DC ferrets was lower than that of ferrets exposed in the same way to LStyNA virus. Also, time of shedding was both delayed and shortened. All of these observations indicate that a short NA stalk length is a significant factor that can limit viral growth and transmission.
Binding by HA to α2,6-linked SA receptors, HA stability, and internal genes competent for efficient replication in mammalian cells in vivo are deemed crucial for RD transmission of influenza virus in mammals (3, 28, 76). Since RD transmission of an H5N1 virus was not achieved despite numerous attempts (8, 9, 74, 77, 78) until recently (67, 71), we studied the effect of NA stalk length in the context of seven genes, all but the NA gene, from a prototypic pandemic H1N1 virus. We considered the pandemic H1 to be a reasonable HA partner for the avian N1 NA because it had recently crossed the species barrier into humans. Indeed, initial reports showed that the 2009 pandemic H1 HA bound α2,6 SA strongly while retaining some residual binding to α2,3 SA (79–82). The six internal genes from the pandemic virus were also well suited for transmission studies, as they had been proven to support RD transmission in the ferret model (63, 68–70).
Two papers recently described ferret RD-transmissible H5N1 viruses (67, 71). The NA gene in the transmissible H5 virus generated by Imai et al. was derived from pH1N1 2009 virus and therefore had a full-length stalk. Herfst et al. generated their transmissible H5 virus with a short-stalk NA. This virus had numerous additional mutations both engineered into HA and PB2 and acquired during ferret passage. However, this virus was less efficiently transmitted than were human seasonal and pandemic influenza strains (71). It would be interesting to see if NA stalk elongation would improve the transmission efficiency of this virus.
A role for NA in viral infectivity and transmissibility in mammals has been noted previously. Data from Matsuoka et al. showed that NA stalk length had various effects on viral infectivity in mice (39). Other studies have shown a link between NA enzymatic activity and RD transmission in guinea pigs and ferrets. In the context of a 2009 H1N1 pandemic precursor virus, Yen et al. showed that replacing a swine N2 NA with the pandemic N1 NA, which had much higher sialidase activity, improved transmission efficiency from 1/3 to 3/3 RD-exposed ferrets (4). This improved transmission efficiency correlated with reduced aggregation at the surface of MDCK cells (4). Lakdawala et al. showed that compared to a virus with classical swine N1 NA, virus with pandemic N1 NA had higher NA enzyme activity and increased numbers of viral genome copies in small respirated particles, which also were associated with increased transmission efficiency (47). Conversely, viruses with reduced NA enzyme kinetics, as a result of mutations that confer NA drug resistance, often show reduced transmission (83). In cases where drug resistance does not compromise transmission, equal or improved RD transmission was dependent on compensatory amino acid mutations in NA that restore good expression of NA enzyme activity at the infected cell surface and on the virion (84).
In our studies, we observed similar nasal wash viral titers shed from the two groups of inoculated donor animals, but SStyNA virions aggregated more than LStyNA virions. It is possible that aggregated virions are less able to be incorporated into the appropriately sized respiratory droplets for transmission through the air (85) or that they are compromised in their ability to initiate infection in the recipient animal. Indeed, we showed that virus with a short-stalk NA had a reduced ability to initiate infection in the presence of mucus, perhaps because it was compromised in its ability to cleave tethered multivalent sialic acid substrates present in the glycocalyx. Neutralization of virus by mucus was significantly reduced through extending the NA stalk length. Together, these observations suggest that cleavage of SA from viral glycoproteins and mucins was compromised by NA's short stalk length. We did not test the virus' ability to overcome inhibition of infectivity by ferret mucus, and so we cannot categorically say that the in vitro measurement accounted for the difference in transmissibility between eth two viruses. However, it is an observable correlation that will be interesting to pursue in future studies.
Our findings have implications with regard to the characteristics of HA and NA if an H5 pandemic were to arise. The barriers to transmission observed in our experiments could be overcome in three ways: (i) a short-stalk HPAI H5N1 NA could enhance its activity through compensatory mutations that counteract its steric hindrance, (ii) an H5 HA with low avidity for its receptor could balance the low activity of a short-stalk NA, or (iii) reassortment in birds, swine, or humans could lead to the pairing of an H5 HA with a long-stalk NA.
Although a virus with a short-stalk NA has not supported transmission of a human influenza virus in the past, enzyme activity of a short-stalk NA could be enhanced in several ways that might overcome this genetic barrier. Mutations that improve NA protein expression density on the virion surface (86) or substrate affinity and/or reaction velocity (87–89) have been associated with improved influenza virus replication or transmission. Moreover, it is likely that different short-stalk NAs naturally vary in enzyme activity and therefore start out from a different baseline in this adaptive pathway. In an experiment whose data are not shown here, we performed the mucus infectivity assay with a virus pair similar to SStyNA and LStyNA, but the NA was from the H7N1 virus A/ck/Italy/13474/1999 (ckIt99) and naturally had a 21-aa stalk truncation. We found that stalk elongation again increased infectivity in the presence of mucus. Notably, for this NA the initial extent of mucus inhibition of infectivity was less drastic than for the SStyNA virus, suggesting that ckIt99 virus had an inherently more active NA than that of ty05. Therefore, it is possible that transmission between mammals might be tolerated by some viruses with short-stalk NA but not others.
Viruses with a short-stalk NA might gain fitness through HA mutations that reduce affinity or alter specificity of SA binding and make the receptor decoys in mucus less able to inhibit virus infectivity. For example, the HA of seasonal H1N1 strains acquired mutations near the receptor binding site that were associated with improved replication when paired with a 2008 drug-resistant NA (90). Similarly, a change in HA receptor binding of influenza B viruses was observed in virus isolates that carried NA mutations conferring resistance to neuraminidase inhibitors following treatment (91). We previously showed that the inhibitory effect of mucus on virus infectivity was reduced by mutations in the HA that altered its receptor binding specificity (48). Thus, a virus with a short-stalk NA might reduce the SA avidity of its HA, for example, by accumulation of HA glycosylation sites as seen in gallinaceous hosts (20, 31, 34). According to Xu et al., the HA from the 2009 pandemic has the lowest avidity of the four most recent human pandemic virus HAs (92). Therefore, the pandemic H1 HA used in this study might have been the most likely to balance an NA with a substantially reduced activity due to stalk truncation, and yet we still found that this HA-NA combination showed compromised transmission.
The possibility of reassortment to restore NA stalk length prompted us to look at the frequency of long-stalk NAs in H5N1 influenza viruses generated by reassortment in nature. In line with the findings of Li et al. (38), we found that the majority of avian HPAI H5N1 viruses have short stalks (Fig. 7 and Table 4). However, some HPAI H5N1 viruses isolated from birds, swine, and humans did have a long-stalk NA (Table 4). Therefore, we suggest that NA stalk length should be determined for all new H5N1 viral isolates since, according to our findings, viruses with a long-stalk NA have a lower barrier to overcome in order to become mammal transmissible. A virus with H5 HA could gain an NA with a longer stalk from any of the nine NA subtypes. Influenza viruses with long-stalk NA genes are more common in Anseriformes (38), so domestic ducks and geese may act as mixing vessels for generating HPAI H5 HA with long-stalk NA. However, all of the HPAI H5 HA genes with long-stalk NA genes from these avian hosts so far retained amino acids 224N, 226Q, and 228G, which confer an avian-like receptor binding preference on α2,3 SA. Therefore, these hosts are unlikely to transmit virus with pandemic potential directly to humans. Using reverse genetics, introduction of a long-stalk NA from a human influenza virus has been shown to increase H5 virus transmission. Chen et al. showed that a virus with an H5 HA, which was mutated so that it bound α2,6-linked SA, did not support RD transmission between ferrets with its cognate NA, but when it was paired with the long-stalk N2 NA of a human seasonal H3N2 virus, RD transmission was achieved (8). Imai et al. also reported that RD transmission was achieved in ferrets with a modified H5 HA paired with seven other influenza virus genes from a pandemic H1N1 strain, including the long-stalk NA (67). Taken together, these findings support our hypothesis that RD transmission of virus with a short-stalk NA in mammals might be increased by acquisition of a long stalk.
In summary, this report showed that the short stalk length of an avian virus NA led to reduced transmission of a virus which was otherwise efficiently transmitted. These findings suggest that a fully poultry-adapted H5N1 virus may be less likely to initiate the next human pandemic than previously thought without substantial mutation or reassortment of the NA gene. Furthermore, our data reinforce the idea that multigenic adaptation (93) may be needed for an animal influenza virus to jump the host species barrier and become a pandemic strain.
Supplementary Material
ACKNOWLEDGMENTS
We thank Ron Fouchier for A/turkey/Turkey/5/05 NA plasmid, Lorian Hartgroves for A/England/195/09 plasmid design, Peter Stilwell for technical assistance, the staff of CBS, Imperial College London, for their expert help, and Michael Hollinshead for materials and assistance in collecting EM images.
Footnotes
Published ahead of print 17 July 2013
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JVI.00967-13.
REFERENCES
- 1.WHO 2013. Cumulative number of confirmed human cases of avian influenza A(H5N1) reported to WHO. WHO, Geneva, Switzerland: http://www.who.int/influenza/human_animal_interface/H5N1_cumulative_table_archives/en/ [Google Scholar]
- 2.Aditama TY, Samaan G, Kusriastuti R, Sampurno OD, Purba W, Misriyah Santoso H, Bratasena A, Maruf A, Sariwati E, Setiawaty V, Glass K, Lokuge K, Kelly PM, Kandun IN. 2012. Avian influenza H5N1 transmission in households, Indonesia. PLoS One 7:e29971. 10.1371/journal.pone.0029971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mitnaul LJ, Matrosovich MN, Castrucci MR, Tuzikov AB, Bovin NV, Kobasa D, Kawaoka Y. 2000. Balanced hemagglutinin and neuraminidase activities are critical for efficient replication of influenza A virus. J. Virol. 74:6015–6020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yen H-L, Liang C, Wu C-Y, Forrest HL, Ferguson A, Choy K-T, Jones J, Wong DD-Y, Cheung PP-H, Hsu C, Li OT, Yuen KM, Chan RWY, Poon LLM, Chan MCW, Nicholls JM, Krauss S, Wong C-H, Guan Y, Webster RG, Webby RJ, Peiris M. 2011. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc. Natl. Acad. Sci. U. S. A. 108:14264–14269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palese P, Tobita K, Ueda M, Compans RW. 1974. Characterization of temperature sensitive influenza virus mutants defective in neuraminidase. Virology 61:397–410 [DOI] [PubMed] [Google Scholar]
- 6.Auewarakul P, Suptawiwat O, Kongchanagul A, Sangma C, Suzuki Y, Ungchusak K, Louisirirotchanakul S, Lerdsamran H, Pooruk P, Thitithanyanont A, Pittayawonganon C, Guo C-T, Hiramatsu H, Jampangern W, Chunsutthiwat S, Puthavathana P. 2007. An avian influenza H5N1 virus that binds to a human-type receptor. J. Virol. 81:9950–9955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayora-Talavera G, Shelton H, Scull MA, Ren J, Jones IM, Pickles RJ, Barclay WS. 2009. Mutations in H5N1 influenza virus hemagglutinin that confer binding to human tracheal airway epithelium. PLoS One 4:e7836. 10.1371/journal.pone.0007836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen L-M, Blixt O, Stevens J, Lipatov AS, Davis CT, Collins BE, Cox NJ, Paulson JC, Donis RO. 2011. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology 422:105–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chutinimitkul S, van Riel D, Munster VJ, van den Brand JMA, Rimmelzwaan GF, Kuiken T, Osterhaus ADME, Fouchier RAM, de Wit E. 2010. In vitro assessment of attachment pattern and replication efficiency of H5N1 influenza A viruses with altered receptor specificity. J. Virol. 84:6825–6833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gambaryan A, Tuzikov A, Pazynina G, Bovin N, Balish A, Klimov A. 2006. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology 344:432–438 [DOI] [PubMed] [Google Scholar]
- 11.Gao Y, Zhang Y, Shinya K, Deng G, Jiang Y, Li Z, Guan Y, Tian G, Li Y, Shi J, Liu L, Zeng X, Bu Z, Xia X, Kawaoka Y, Chen H. 2009. Identification of amino acids in HA and PB2 critical for the transmission of H5N1 avian influenza viruses in a mammalian host. PLoS Pathog. 5:e1000709. 10.1371/journal.ppat.1000709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maines TR, Chen L-M, Van Hoeven N, Tumpey TM, Blixt O, Belser JA, Gustin KM, Pearce MB, Pappas C, Stevens J, Cox NJ, Paulson JC, Raman R, Sasisekharan R, Katz JM, Donis RO. 2011. Effect of receptor binding domain mutations on receptor binding and transmissibility of avian influenza H5N1 viruses. Virology 413:139–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russell RJ, Stevens DJ, Haire LF, Gamblin SJ, Skehel JJ. 2006. Avian and human receptor binding by hemagglutinins of influenza A viruses. Glycoconj. J. 23:85–92 [DOI] [PubMed] [Google Scholar]
- 14.Shelton H, Ayora-Talavera G, Ren J, Loureiro S, Pickles RJ, Barclay WS, Jones IM. 2011. Receptor binding profiles of avian influenza virus hemagglutinin subtypes on human cells as a predictor of pandemic potential. J. Virol. 85:1875–1880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Su Y, Yang H-Y, Zhang B-J, Jia H-L, Tien P. 2008. Analysis of a point mutation in H5N1 avian influenza virus hemagglutinin in relation to virus entry into live mammalian cells. Arch. Virol. 153:2253–2261 [DOI] [PubMed] [Google Scholar]
- 16.Veljkovic V, Veljkovic N, Muller CP, Müller S, Glisic S, Perovic V, Köhler H. 2009. Characterization of conserved properties of hemagglutinin of H5N1 and human influenza viruses: possible consequences for therapy and infection control. BMC Struct. Biol. 9:21. 10.1186/1472-6807-9-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watanabe Y, Ibrahim MS, Ellakany HF, Kawashita N, Mizuike R, Hiramatsu H, Sriwilaijaroen N, Takagi T, Suzuki Y, Ikuta K. 2011. Acquisition of human-type receptor binding specificity by new H5N1 influenza virus sublineages during their emergence in birds in Egypt. PLoS Pathog. 7:e1002068. 10.1371/journal.ppat.1002068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamada S, Suzuki Y, Suzuki T, Le MQ, Nidom CA, Sakai-Tagawa Y, Muramoto Y, Ito M, Kiso M, Horimoto T, Shinya K, Sawada T, Kiso M, Usui T, Murata T, Lin Y, Hay A, Haire LF, Stevens DJ, Russell RJ, Gamblin SJ, Skehel JJ, Kawaoka Y. 2006. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 444:378–382 [DOI] [PubMed] [Google Scholar]
- 19.Ito T, Suzuki Y, Suzuki T, Takada A, Horimoto T, Wells K, Kida H, Otsuki K, Kiso M, Ishida H, Kawaoka Y. 2000. Recognition of N-glycolylneuraminic acid linked to galactose by the alpha2,3 linkage is associated with intestinal replication of influenza A virus in ducks. J. Virol. 74:9300–9305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matrosovich M, Zhou N, Kawaoka Y, Webster R. 1999. The surface glycoproteins of H5 influenza viruses isolated from humans, chickens, and wild aquatic birds have distinguishable properties. J. Virol. 73:1146–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nicholls JM, Chan MCW, Chan WY, Wong HK, Cheung CY, Kwong DLW, Wong MP, Chui WH, Poon LLM, Tsao SW, Guan Y, Peiris JSM. 2007. Tropism of avian influenza A (H5N1) in the upper and lower respiratory tract. Nat. Med. 13:147–149 [DOI] [PubMed] [Google Scholar]
- 22.Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440:435–436 [DOI] [PubMed] [Google Scholar]
- 23.Stevens J, Blixt O, Chen L-M, Donis RO, Paulson JC, Wilson IA. 2008. Recent avian H5N1 viruses exhibit increased propensity for acquiring human receptor specificity. J. Mol. Biol. 381:1382–1394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312:404–410 [DOI] [PubMed] [Google Scholar]
- 25.Matrosovich M, Tuzikov A, Bovin N, Gambaryan A, Klimov A, Castrucci MR, Donatelli I, Kawaoka Y. 2000. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J. Virol. 74:8502–8512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solórzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, García-Sastre A. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315:655–659 [DOI] [PubMed] [Google Scholar]
- 27.Steel J, Lowen AC, Mubareka S, Palese P. 2009. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 5:e1000252. 10.1371/journal.ppat.1000252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Hoeven N, Pappas C, Ja Belser Maines TR, Zeng H, García-Sastre A, Sasisekharan R, Katz JM, Tumpey TM. 2009. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc. Natl. Acad. Sci. U. S. A. 106:3366–3371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bender C, Hall H, Huang J, Klimov A, Cox N, Hay A, Gregory V, Cameron K, Lim W, Subbarao K. 1999. Characterization of the surface proteins of influenza A (H5N1) viruses isolated from humans in 1997–1998. Virology 254:115–123 [DOI] [PubMed] [Google Scholar]
- 30.Xu X, Subbarao Cox NJ, Guo Y. 1999. Genetic characterization of the pathogenic influenza A/Goose/Guangdong/1/96 (H5N1) virus: similarity of its hemagglutinin gene to those of H5N1 viruses from the 1997 outbreaks in Hong Kong. Virology 261:15–19 [DOI] [PubMed] [Google Scholar]
- 31.Banks J, Speidel ES, Moore E, Plowright L, Piccirillo A, Capua I, Cordioli P, Fioretti A, Alexander DJ. 2001. Changes in the haemagglutinin and the neuraminidase genes prior to the emergence of highly pathogenic H7N1 avian influenza viruses in Italy. Arch. Virol. 146:963–973 [DOI] [PubMed] [Google Scholar]
- 32.Hossain MJ, Hickman D, Perez DR. 2008. Evidence of expanded host range and mammalian-associated genetic changes in a duck H9N2 influenza virus following adaptation in quail and chickens. PLoS One 3:e3170. 10.1371/journal.pone.0003170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Obenauer JC, Denson J, Mehta PK, Su X, Mukatira S, Finkelstein DB, Xu X, Wang J, Ma J, Fan Y, Rakestraw KM, Webster RG, Hoffmann E, Krauss S, Zheng J, Zhang Z, Naeve CW. 2006. Large-scale sequence analysis of avian influenza isolates. Science 311:1576–1580 [DOI] [PubMed] [Google Scholar]
- 34.Sorrell EM, Song H, Pena L, Perez DR. 2010. A 27-amino-acid deletion in the neuraminidase stalk supports replication of an avian H2N2 influenza A virus in the respiratory tract of chickens. J. Virol. 84:11831–11840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guan Y, Poon LLM, Cheung CY, Ellis TM, Lim W, Lipatov AS, Chan KH, Sturm-Ramirez KM, Cheung CL, Leung YHC, Yuen KY, Webster RG, Peiris JSM. 2004. H5N1 influenza: a protean pandemic threat. Proc. Natl. Acad. Sci. U. S. A. 101:8156–8161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown IH. 2010. Summary of avian influenza activity in Europe, Asia, and Africa, 2006–2009. Avian Dis. 54:187–193 [DOI] [PubMed] [Google Scholar]
- 37.Guan Y, Peiris JSM, Lipatov AS, Ellis TM, Dyrting KC, Krauss S, Zhang LJ, Webster RG, Shortridge KF. 2002. Emergence of multiple genotypes of H5N1 avian influenza viruses in Hong Kong SAR. Proc. Natl. Acad. Sci. U. S. A. 99:8950–8955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li J, Zu Dohna H, Cardona CJ, Miller J, Carpenter TE. 2011. Emergence and genetic variation of neuraminidase stalk deletions in avian influenza viruses. PLoS One 6:e14722. 10.1371/journal.pone.0014722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matsuoka Y, Swayne DE, Thomas C, Rameix-Welti M-A, Naffakh N, Warnes C, Altholtz M, Donis R, Subbarao K. 2009. Neuraminidase stalk length and additional glycosylation of the hemagglutinin influence the virulence of influenza H5N1 viruses for mice. J. Virol. 83:4704–4708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Munier S, Larcher T, Cormier-Aline F, Soubieux D, Su B, Guigand L, Labrosse B, Cherel Y, Quéré P, Marc D, Naffakh N. 2010. A genetically engineered waterfowl influenza virus with a deletion in the stalk of the neuraminidase has increased virulence for chickens. J. Virol. 84:940–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang W, Xue T, Wu X, Zhang P, Zhao G, Peng D, Hu S, Wang X, Liu X, Liu W, Liu X. 2011. Increase in viral yield in eggs and MDCK cells of reassortant H5N1 vaccine candidate viruses caused by insertion of 38 amino acids into the NA stalk. Vaccine 29:8032–8041 [DOI] [PubMed] [Google Scholar]
- 42.Castrucci MR, Kawaoka Y. 1993. Biologic importance of neuraminidase stalk length in influenza A virus. J. Virol. 67:759–764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou H, Yu Z, Hu Y, Tu J, Zou W, Peng Y, Zhu J, Li Y, Zhang A, Yu Z, Ye Z, Chen H, Jin M. 2009. The special neuraminidase stalk-motif responsible for increased virulence and pathogenesis of H5N1 influenza A virus. PLoS One 4:e6277. 10.1371/journal.pone.0006277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baigent SJ, McCauley JW. 2001. Glycosylation of haemagglutinin and stalk-length of neuraminidase combine to regulate the growth of avian influenza viruses in tissue culture. Virus Res. 79:177–185 [DOI] [PubMed] [Google Scholar]
- 45.Matrosovich MN, Matrosovich TY, Gray T, Roberts NA, Klenk H. 2004. Neuraminidase is important for the initiation of influenza virus infection in human airway epithelium. J. Virol. 78:12665–12667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scull MA, Gillim-Ross L, Santos C, Roberts KL, Bordonali E, Subbarao K, Barclay WS, Pickles RJ. 2009. Avian influenza virus glycoproteins restrict virus replication and spread through human airway epithelium at temperatures of the proximal airways. PLoS Pathog. 5:e1000424. 10.1371/journal.ppat.1000424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lakdawala SS, Lamirande EW, Suguitan AL, Wang W, Santos CP, Vogel L, Matsuoka Y, Lindsley WG, Jin H, Subbarao K. 2011. Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog. 7:e1002443. 10.1371/journal.ppat.1002443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roberts KL, Shelton H, Scull M, Pickles R, Barclay WS. 2011. Lack of transmission of a human influenza virus with avian receptor specificity between ferrets is not due to decreased virus shedding but rather a lower infectivity in vivo. J. Gen. Virol. 92:1822–1831 [DOI] [PubMed] [Google Scholar]
- 49.van Riel D, den Bakker MA, Leijten LME, Chutinimitkul S, Munster VJ, de Wit E, Rimmelzwaan GF, Fouchier RAM, Osterhaus ADME, Kuiken T. 2010. Seasonal and pandemic human influenza viruses attach better to human upper respiratory tract epithelium than avian influenza viruses. Am. J. Pathol. 176:1614–1618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lindemann J, Leiacker R, Rettinger G, Keck T. 2002. Nasal mucosal temperature during respiration. Clin. Otolaryngol. Allied Sci. 27:135–139 [DOI] [PubMed] [Google Scholar]
- 51.Massin P, van der Werf S, Naffakh N. 2001. Residue 627 of PB2 is a determinant of cold sensitivity in RNA replication of avian influenza viruses. J. Virol. 75:5398–5404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matrosovich M, Klenk H-D. 2003. Natural and synthetic sialic acid-containing inhibitors of influenza virus receptor binding. Rev. Med. Virol. 13:85–97 [DOI] [PubMed] [Google Scholar]
- 53.Thornton DJ, Rousseau K, McGuckin MA. 2008. Structure and function of the polymeric mucins in airways mucus. Annu. Rev. Physiol. 70:459–486 [DOI] [PubMed] [Google Scholar]
- 54.Basler CF, García-Sastre A, Palese P. 1999. Mutation of neuraminidase cysteine residues yields temperature-sensitive influenza viruses. J. Virol. 73:8095–8103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bao Y, Bolotov P, Dernovoy D, Kiryutin B, Zaslavsky L, Tatusova T, Ostell J, Lipman D. 2008. The influenza virus resource at the National Center for Biotechnology Information. J. Virol. 82:596–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. 2011. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol. Biol. Evol. 28:2731–2739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stamatakis A. 2006. RAxML-VI-HPC: maximum likelihood-based phylogenetic analyses with thousands of taxa and mixed models. Bioinformatics 22:2688–2690 [DOI] [PubMed] [Google Scholar]
- 58.Rambaut A. FigTree. http://tree.bio.ed.ac.uk/software/figtree/ Institute of Evolutionary Biology, University of Edinburgh, Edinburgh, United Kingdom [Google Scholar]
- 59.Ellis J, Iturriza M, Allen R, Bermingham A, Brown K, Gray J, Brown D. 2009. Evaluation of four real-time PCR assays for detection of influenza A(H1N1)v viruses. Euro Surveill. 14:20–22 [DOI] [PubMed] [Google Scholar]
- 60.Fodor E, Devenish L, Engelhardt OG, Palese P, Brownlee GG, García-Sastre A. 1999. Rescue of influenza A virus from recombinant DNA. J. Virol. 73:9679–9682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Elleman CJ, Barclay WS. 2004. The M1 matrix protein controls the filamentous phenotype of influenza A virus. Virology 321:144–153 [DOI] [PubMed] [Google Scholar]
- 62.Matrosovich M, Matrosovich T, Garten W, Klenk H-D. 2006. New low-viscosity overlay medium for viral plaque assays. Virol. J. 3:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.van Doremalen N, Shelton H, Roberts KL, Jones IM, Pickles RJ, Thompson CI, Barclay WS. 2011. A single amino acid in the HA of pH1N1 2009 influenza virus affects cell tropism in human airway epithelium, but not transmission in ferrets. PLoS One 6:e25755. 10.1371/journal.pone.0025755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.WHO Global Influenza Surveillance Network 2011. Manual for the laboratory diagnosis and virological surveillance of influenza. World Health Organization, Geneva, Switzerland [Google Scholar]
- 65.Hollinshead M, Vanderplasschen A, Smith GL, Vaux DJ. 1999. Vaccinia virus intracellular mature virions contain only one lipid membrane. J. Virol. 73:1503–1517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Reid AH H, Fanning TG, Janczewski TA, Taubenberger JK. 2000. Characterization of the 1918 “Spanish” influenza virus neuraminidase gene. Proc. Natl. Acad. Sci. U. S. A. 97:6785–6790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Itoh Y, Shinya K, Kiso M, Watanabe T, Sakoda Y, Hatta M, Muramoto Y, Tamura D, Sakai-Tagawa Y, Noda T, Sakabe S, Imai M, Hatta Y, Watanabe S, Li C, Yamada S, Fujii K, Murakami S, Imai H, Kakugawa S, Ito M, Takano R, Iwatsuki-Horimoto K, Shimojima M, Horimoto T, Goto H, Takahashi K, Makino A, Ishigaki H, Nakayama M, Okamatsu M, Takahashi K, Warshauer D, Shult PA, Saito R, Suzuki H, Furuta Y, Yamashita M, Mitamura K, Nakano K, Nakamura M, Brockman-Schneider R, Mitamura H, Yamazaki M, Sugaya N, Suresh M, Ozawa M, Neumann G, Gern J, Kida H, Ogasawara K, Kawaoka Y. 2009. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature 460:1021–1025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Maines TR, Jayaraman A, Belser JA, Wadford DA, Pappas C, Zeng H, Gustin KM, Pearce MB, Viswanathan K, Shriver ZH, Raman R, Cox NJ, Sasisekharan R, Katz JM, Tumpey TM. 2009. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science 325:484–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Munster VJ, de Wit E, van den Brand JMA, Herfst S, Schrauwen EJA, Bestebroer TM, van de Vijver D, Boucher CA, Koopmans M, Rimmelzwaan GF, Kuiken T, Osterhaus ADME, Fouchier RAM. 2009. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science 325:481–483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Herfst S, Schrauwen EJA, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus ADME, Fouchier RAM. 2012. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336:1534–1541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang W, Lu B, Zhou H, Suguitan AL, Cheng X, Subbarao K, Kemble G, Jin H. 2010. Glycosylation at 158N of the hemagglutinin protein and receptor binding specificity synergistically affect the antigenicity and immunogenicity of a live attenuated H5N1 A/Vietnam/1203/2004 vaccine virus in ferrets. J. Virol. 84:6570–6577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shinya K, Hatta M, Yamada S, Takada A, Watanabe S, Halfmann P, Horimoto T, Neumann G, Kim JH, Lim W, Guan Y, Peiris M, Kiso M, Suzuki T, Suzuki Y, Kawaoka Y. 2005. Characterization of a human H5N1 influenza A virus isolated in 2003. J. Virol. 79:9926–9932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Maines TR, Chen L-M, Matsuoka Y, Chen H, Rowe T, Ortin J, Falcón A, Nguyen TH, Mai LQ, Sedyaningsih ER, Harun S, Tumpey TM, Donis RO, Cox NJ, Subbarao K, Katz JM. 2006. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc. Natl. Acad. Sci. U. S. A. 103:12121–12126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Subbarao EK, London W, Murphy BR. 1993. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J. Virol. 67:1761–1764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wagner R, Matrosovich M, Klenk H-D. 2002. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev. Med. Virol. 12:159–166 [DOI] [PubMed] [Google Scholar]
- 77.Jackson S, Van Hoeven N, Chen L-M, Maines TR, Cox NJ, Katz JM, Donis RO. 2009. Reassortment between avian H5N1 and human H3N2 influenza viruses in ferrets: a public health risk assessment. J. Virol. 83:8131–8140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yen H-L, Lipatov AS, Ilyushina NA, Govorkova EA, Franks J, Yilmaz N, Douglas A, Hay A, Krauss S, Rehg JE, Hoffmann E, Webster RG. 2007. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J. Virol. 81:6890–6898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Belser JA, Jayaraman A, Raman R, Pappas C, Zeng H, Cox NJ, Katz JM, Sasisekharan R, Tumpey TM. 2011. Effect of D222G mutation in the hemagglutinin protein on receptor binding, pathogenesis and transmissibility of the 2009 pandemic H1N1 influenza virus. PLoS One 6:e25091. 10.1371/journal.pone.0025091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bradley KC, Jones CA, Tompkins SM, Tripp RA, Russell RJ, Gramer MR, Heimburg-Molinaro J, Smith DF, Cummings RD, Steinhauer DA. 2011. Comparison of the receptor binding properties of contemporary swine isolates and early human pandemic H1N1 isolates (Novel 2009 H1N1). Virology 413:169–182 [DOI] [PubMed] [Google Scholar]
- 81.Childs RA, Palma AS, Wharton S, Matrosovich T, Liu Y, Chai W, Campanero-Rhodes MA, Zhang Y, Eickmann M, Kiso M, Hay A, Matrosovich M, Feizi T. 2009. Receptor-binding specificity of pandemic influenza A (H1N1) 2009 virus determined by carbohydrate microarray. Nat. Biotechnol. 27:797–799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liu Y, Childs RA, Matrosovich T, Wharton S, Palma AS, Chai W, Daniels R, Gregory V, Uhlendorff J, Kiso M, Klenk H-D, Hay A, Feizi T, Matrosovich M. 2010. Altered receptor specificity and cell tropism of D222G hemagglutinin mutants isolated from fatal cases of pandemic A(H1N1) 2009 influenza virus. J. Virol. 84:12069–12074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bouvier NM, Lowen AC, Palese P. 2008. Oseltamivir-resistant influenza A viruses are transmitted efficiently among guinea pigs by direct contact but not by aerosol. J. Virol. 82:10052–10058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bouvier NM, Rahmat S, Pica N. 2012. Enhanced mammalian transmissibility of seasonal influenza A/H1N1 viruses encoding an oseltamivir-resistant neuraminidase. J. Virol. 86:7268–7279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ. 2013. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 9:e1003205. 10.1371/journal.ppat.1003205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bloom JD, Gong LI, Baltimore D. 2010. Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science 328:1272–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Abed Y, Pizzorno A, Bouhy X, Boivin G. 2011. Role of permissive neuraminidase mutations in influenza A/Brisbane/59/2007-like (H1N1) viruses. PLoS Pathog. 7:e1002431. 10.1371/journal.ppat.1002431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mountford CE, Grossman G, Holmes KT, O'Sullivan WJ, Hampson AW, Raison RL, Webster R. 1982. Effect of monoclonal anti-neuraminidase antibodies on the kinetic behavior of influenza virus neuraminidase. Mol. Immunol. 19:811–816 [DOI] [PubMed] [Google Scholar]
- 89.Rameix-Welti M-A, Enouf V, Cuvelier F, Jeannin P, van der Werf S. 2008. Enzymatic properties of the neuraminidase of seasonal H1N1 influenza viruses provide insights for the emergence of natural resistance to oseltamivir. PLoS Pathog. 4:e1000103. 10.1371/journal.ppat.1000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ginting TE, Shinya K, Kyan Y, Makino A, Matsumoto N, Kaneda S, Kawaoka Y. 2012. Amino acid changes in hemagglutinin contribute to the replication of oseltamivir-resistant H1N1 influenza viruses. J. Virol. 86:121–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mochalova L, Bright R, Xu X, Korchagina E, Chinarev A, Bovin N, Klimov A. 2010. Shift in oligosaccharide specificities of hemagglutinin and neuraminidase of influenza B viruses resistant to neuraminidase inhibitors. Glycoconj. J. 27:321–327 [DOI] [PubMed] [Google Scholar]
- 92.Xu R, Zhu X, McBride R, Nycholat CM, Yu W, Paulson JC, Wilson IA. 2012. Functional balance of the hemagglutinin and neuraminidase activities accompanies the emergence of the 2009 H1N1 influenza pandemic. J. Virol. 86:9221–9232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Russell CA, Fonville JM, Brown AEX, Burke DF, Smith DL, James SL, Herfst S, van Boheemen S, Linster M, Schrauwen EJ, Katzelnick L, Mosterín A, Kuiken T, Maher E, Neumann G, Osterhaus ADME, Kawaoka Y, Fouchier RAM, Smith DJ. 2012. The potential for respiratory droplet-transmissible A/H5N1 influenza virus to evolve in a mammalian host. Science 336:1541–1547 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.