Abstract
Background
The extent to which low medication adherence in hypertensive individuals contributes to disparities in stroke and transient ischemic attack (TIA) risk is poorly understood.
Methods
Investigators examined the relationship between self-reported medication adherence and blood pressure (BP) control (<140/90 mm Hg), Framingham Stroke Risk Score, and physician-adjudicated stroke/TIA incidence in treated hypertensive subjects (n = 15,071; 51% black; 57% in Stroke Belt) over 4.9 years in the national population-based REGARDS cohort study.
Results
Mean systolic BP varied from 130.8 ± 16.2 mm Hg in those reporting high adherence to 137.8 ± 19.5 mm Hg in those reporting low adherence (P for trend < .0001). In logistic regression models, each level of worsening medication adherence was associated with significant and increasing odds of inadequately controlled BP (≥140/90 mm Hg; score = 1, odds ratio [95% confidence interval], 1.20 [1.09–1.30]; score = 2, 1.27 [1.08–1.49]; score = 3 or 4, 2.21 [1.75–2.78]). In hazard models using systolic BP as a mediator, those reporting low medication adherence had 1.08 (1.04–1.14) times greater risk of stroke and 1.08 (1.03–1.12) times greater risk of stroke or TIA.
Conclusion
Low medication adherence was associated with inadequate BP control and an increased risk of incident stroke or TIA.
Keywords: Medication adherence, blood pressure control, stroke, transient ischemic attack
Introduction
Despite a plethora of effective antihypertensive agents, nearly half of patients with hypertension do not achieve guideline recommended treatment targets.1 Data from multiple investigators suggest an important relationship between lower medication adherence and risk of stroke symptoms, stroke, and adverse cardiovascular (CV) outcomes.2–5 In patients with established coronary artery disease, inadequate medication adherence was associated with a 2.3-fold increase in the hazard ratio for adverse CV events.6 Lower medication adherence has also been identified as a contributing factor to persistent blood pressure (BP) elevation following medication intensification.7 Barriers to medication adherence are multifactorial and include complex medication regimens, dosing frequency, behavioral factors, trust, communication, side effects, and other complications of treatment. However, it is unclear which hypertensive persons with lower medication adherence are at greatest risk of developing adverse CV outcomes, and if this increased risk is mediated through higher BP levels. Further, the relationship between socioeconomic and other barriers to proper medication-taking behavior and both lower medication adherence and subsequent CV risk is not well described. To address these important gaps in our understanding, we examined the relationship between medication adherence, BP control, Framingham Stroke Risk Score (FSRS), and adjudicated stroke and transient ischemic attack (TIA) outcomes in a national population-based sample of black and white treated hypertensive individuals.
Methods
Study Sample and Baseline Data Collection
The REasons for Geographic And Racial Disparities in Stroke (REGARDS) study is designed to examine factors associated with the geographic and racial disparities in stroke incidence as well as causes of excess stroke mortality in the southeastern U.S. (ie, Stroke Belt) relative to the rest of the nation and among blacks relative to whites. The methods of this study have been described in detail elsewhere.8 In short, REGARDS is a population-based, prospective, longitudinal cohort study of 30,239 subjects aged ≥45 years, 45% male, 55% female, 41% black, 59% white, 55% from the stroke belt region, and 45% from the rest of the continental U.S. REGARDS provides a unique opportunity to examine medication adherence, BP control, and stroke/TIA incidence among a national sample of black and white hypertensive adults who are receiving medication therapy for hypertension.
The REGARDS cohort was recruited between January 2003 and October 2007 and evaluated every 6 months over a mean follow-up period of 4.9 years. REGARDS included a computer-assisted telephone interview with each subject to collect demographic characteristics, including address, age, gender, and race (each subject self-reported race, and by design, the study compared only non-Hispanic black and white subjects, excluding other race/ethnic groups). Analysis in this paper is limited to treated hypertensive participants, defined as all subjects from the cohort who reported in their telephone interview that a physician had told them they had hypertension/high blood pressure and who also had a home visit evaluation that included documentation of antihypertensive medications. All prescription medication names were recorded verbatim from the pharmacy label during a home visit, and antihypertensive medications were identified by the investigators and categorized by drug class.
The primary exposure of interest was medication adherence. Self-reported general medication adherence was assessed using the previously validated 4-item scale developed by Morisky.9 Each yes response is counted leading to a total adherence score that ranges from 0 = highest adherence to 4 = lowest adherence. This 0 to 4 scoring was then used to categorize subjects into four groups by level of adherence as follows: 0 = high adherence; 1 = good adherence; 2 = moderate adherence; 3 to 4 = low adherence. The Morisky scale is a well-validated measure that has been extensively used for more than 20 years to assess medication adherence in a variety of individuals/settings.9 Other intermediate predictors included baseline BP levels and FSRS as described below.
The primary outcomes of interest were adjudicated stroke and/or TIA events. Each subject was followed at 6-month intervals. A trained interviewer administered a standardized questionnaire that specifically asked, since the last follow-up, “Have you been told by a physician that you had a stroke?” and “Have you been told by a physician that you had a mini-stroke or TIA, also known as a transient ischemic attack?” For each positive response, the date and time of each event was recorded. Each self-reported stroke or TIA event was then carefully adjudicated via medical records review by a physician-led medical review team. Stroke events were defined following the World Health Organization definition10 but also included events with symptoms lasting <24 hours with neuroimaging consistent with acute ischemia or hemorrhage, and cases where adjudicators agreed that the event was likely a stroke or death related to stroke but information was incomplete for World Health Organization or clinical classification. A TIA was defined as a similar disturbance with symptoms lasting less than 24 hours and with neuroimaging results negative for stroke.
Data on traditional CV risk factors and socioeconomic factors were also collected in order to adjust for potential confounding in our analyses of the relationship between adherence and stroke/TIA outcomes. Each subject, at baseline, also completed an in-home visit conducted by a trained health professional, which included measurement of height and weight via standard procedures. BP was assessed as the average of two measurements obtained with an aneroid sphygmomanometer after being in the seated position for at least 3 minutes with both feet on the floor. A 12-lead electrocardiogram (ECG) was obtained, and all ECGs were read by a trained cardiologist in a centralized ECG reading laboratory at Wake Forest University/Baptist Medical Center in Winston-Salem, NC, using a pre-defined interpretation protocol.11 Atrial fibrillation was determined to be present if there was a self-reported history (asked as “Has a doctor or other health professional ever told you that you had atrial fibrillation?”) or if characteristic findings were present on the ECG as defined in the protocol. Left ventricular hypertrophy was defined to be present or absent based on ECG findings using the Sokolow-Lyon limb lead criteria12 as specified in the protocol. Blood specimens were obtained, and total and high density lipoprotein cholesterol were measured in accordance with the National Cholesterol Education Program guidelines.13 The FSRS14 was also calculated as a composite measure of stroke risk factors and included the following variables: age, gender, systolic BP, use of antihypertensive medications, current smoking status, history of heart disease, diabetes, left ventricular hypertrophy, and atrial fibrillation.
Additional data collected included the following: annual household income (<$20,000/year, $20,000 to $35,000/year, $35,000 to $75,000/year, and >$75,000/year), education level (less than high school education, high school graduate, some college, and college graduate or higher), and health insurance (yes or no). Also collected was a health history including a history of heart disease (self-reported myocardial infarction, coronary artery bypass grafting, bypass, angioplasty, stenting, or evidence of myocardial infarction on the study ECG) and/or diabetes (self-reported diabetes or if fasting glucose ≥126 mg/dL, or if non-fasting glucose ≥200 mg/dL, or the presence of diabetes oral tablets or insulin during the home visit). The presence of depressive symptoms was assessed using the previously validated four-item Center for Epidemiologic Studies Depression (CES-D) questionnaire.15 Subjects with a CES-D score ≥ 4 were determined to have a high level of psychological distress/depressive symptoms. Health behavior data collected included smoking (categorized as nonsmoker, past smoker, or current smoker), exercise (how often per week the subject exercised enough to work up a sweat; categorized as never, one to three times per week, or four or more times per week), alcohol consumption (categorized as none, moderate [1 to 7 drinks per week for women and 1 to 14 drinks per week for men], and heavy [anything more than moderate alcohol consumption] as recommended by the National Institute on Drug Abuse). The study was approved by the Institutional Review Board at the University of Alabama-Birmingham, and each subject provided informed consent.
Analysis
The present study examined the relationship between self-reported medication adherence and BP control (<140/90 mm Hg based on JNC 7 report),16 FSRS,14 and adjudicated stroke/TIA incidence during follow-up in treated hypertensive subjects. The initial analysis characterized the proportion of subjects with low self-reported medication adherence (operationalized as 3 or 4 on the Morisky scale) and the relationship between low medication adherence and socio-demographic variables and individual cardiovascular risk factors. The relationship between medication adherence and the FSRS was also assessed by analysis of variance.
We then assessed the relationship between medication adherence and the proportion of subjects meeting guideline-recommended BP goals (<140/90 mm Hg),16 examined first in an unadjusted (crude) logistic regression model and then in additional models that incrementally added the following groups of variables: 1) demographic characteristics (race, age, gender, and region [Stroke Belt vs. non-Stroke Belt]) 2) socioeconomic factors (income, education, insurance), and finally 3) cardiovascular risk factors (smoking, diabetes, history of heart disease, left ventricular hypertrophy, depressive symptoms, atrial fibrillation).
The longitudinal relationship between baseline self-reported medication adherence and subsequent adjudicated stroke or TIA events during the follow-up period was examined in a series of Cox proportional hazards models. These models used an analogous approach as the cross-sectional analysis, adding groups of variables incrementally, first adjusting for demographic characteristics, then socioeconomic factors, and then CV risk factors. Each Cox proportional hazards model employed systolic BP as a mediating variable. Mediation was performed using the “a times b” approach as described by MacKinnon.17 The model used to determine the “a” coefficient was analysis of variance/analysis of covariance with Morisky score as the predictor variable and systolic BP as the outcome variable of interest. The model used to determine the “b” coefficient was a Cox proportional hazards model with systolic BP as the predictor variable and adjudicated stroke/TIA as the outcome variable of interest. Both a and b coefficients were significantly greater than zero, which was the requirement for mediation. Ninety-five percent Wald confidence intervals for the mediation coefficient, ab, were calculated and exponentiated for interpretation as hazard ratios. All analyses were performed using SAS version 9.2 (SAS, Cary, NC).
Results
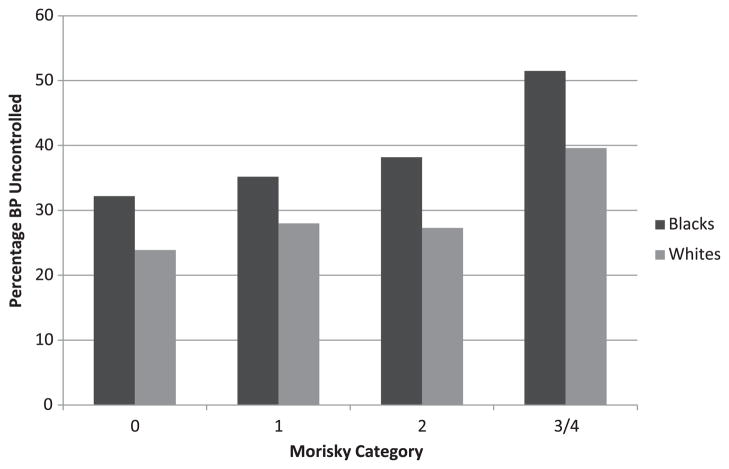
The present study included a total of n = 15,071 treated hypertensive subjects, 51% black, 57% living in the southeastern U.S. Stroke Belt followed for an average of 4.9 years. Sixty-nine percent (n = 10,399) of subjects reported high medication adherence (Morisky score = 0), 23% (n = 3466) a score of 1, 5% (n = 753) a score of 2, and 3% (n = 453) a score of 3 or 4. Detailed demographic characteristics for the study group are given in Table 1, separated into two medication adherence categories (Morisky scale of 0 to 2 vs. 3 or 4). Low medication adherence (Morisky scale of 3 or 4) was significantly more common among subjects who were black, female, and among those reporting limited income. However, medication adherence patterns were not significantly different by geographic location (Stroke Belt vs. non-Stroke Belt). Mean systolic BP varied from 130.8 ± 16.2 mm Hg in those reporting high adherence (Morisky score of 0) to 137.8 ± 19.5 mm Hg in those reporting the lowest medication adherence (score of 3 or 4) (P for trend < .0001). The Figure shows the percentage of subjects by race with an inadequately controlled BP (≥140/90 mm Hg) at each level of adherence.
Table 1.
Baseline characteristics of treated hypertensive subjects from the REGARDS cohort study by medication adherence category (0 to 2 vs. 3 or 4 affirmative responses on Morisky scale)
| Parameter | Morisky 0 to 2 Affirmative Responses | Morisky 3 or 4 Affirmative Responses | P Value |
|---|---|---|---|
| Mean age, years | 66.2 | 65.0 | .0157 |
| Black, % | 50.3 | 67.2 | <.0001 |
| Female, % | 56.9 | 66.9 | .0003 |
| <High school education, % | 15.5 | 19.2 | .0192 |
| High school graduate, % | 27.6 | 30.8 | |
| Some college education, % | 26.6 | 26.9 | |
| College graduate, % | 30.3 | 23.1 | |
| Income <$20k, % | 21.5 | 31.1 | <.0001 |
| Income $20k-$34k, % | 26.0 | 26.6 | |
| Income $35k-$74k, % | 28.1 | 19.5 | |
| Income $75k and above, % | 12.0 | 7.7 | |
| Income – refused, % | 12.3 | 15.1 | |
| % CES-D score ≥ 4 | 12.4 | 24.0 | <.0001 |
| Mean Systolic BP | 131.2 | 137.8 | <0.0001 |
BP, blood pressure; CES-D, Center for Epidemiologic Studies Depression.
Figure.
Proportion of subjects with uncontrolled BP (>140/90 mm Hg) by category of self-reported medication adherence and race.* BP, blood pressure.*P < .01.
Compared with a Morisky score of 0, each level of worsening medication adherence was associated with significant and increasing odds of inadequately controlled BP (≥140/90 mm Hg) in fully adjusted logistic regression models: score = 1, odds ratio (95% confidence interval [CI]), 1.19 (1.09–1.30); score = 2, 1.27 (1.08–1.49); score = 3 or 4, 2.21 (1.75–2.78); see Table 2. The lowest category of medication adherence (Morisky scale of 3 or 4) was associated with significantly higher 10-year FSRS (Morisky score of 0 = mean FSRS of 13.4 [95% CI, 13.1–13.6]; Morisky score of 1 = mean FSRS of 13.3 [95% CI, 12.9–13.8]; Morisky score of 2 = mean FSRS of 12.9 [95% CI, 11.9–13.8]; Morisky score of 3 or 4 = mean FSRS of 15.8 [95% CI, 14.3–17.3]; P < .001).
Table 2.
Logistic regression model - odds ratio (95% confidence interval) for uncontrolled blood pressure (≥140/90 mm Hg)
| Reference: Morisky - 0 Affirmative | Unadjusted (n = 15,071) | Demographics + CV Risk Factors (n = 13,945) | Demographic and Socioeconomic Factors + CV Risk Factors (n = 13,924) |
|---|---|---|---|
| Morisky - 1 affirmative | 1.18 (1.08, 1.28) | 1.20 (1.10, 1.31) | 1.20 (1.10, 1.31) |
| Morisky - 2 affirmative | 1.32 (1.14, 1.54) | 1.30 (1.10, 1.52) | 1.27 (1.08, 1.49) |
| Morisky - 3 or 4 affirmative | 2.34 (1.88, 2.90) | 2.27 (1.80, 2.86) | 2.21 (1.75, 2.78) |
CV, Cardiovascular.
In Cox analyses with systolic BP as the mediating variable, those reporting low medication adherence (Morisky score of 3 or 4) had 1.08 (1.04–1.14) times greater rate of stroke and 1.08 (1.03–1.12) times greater rate of stroke or TIA in fully adjusted models (see Table 3). Neither race nor geographic location (Stroke Belt vs. non-Stroke Belt) was a significant independent predictor of stroke/TIA risk in fully adjusted models. Similarly, there was no evidence of effect modification by race or income when an interaction term for race × income was introduced into the model. However, for those participants who experienced a stroke/TIA during follow-up, the age at event onset was significantly younger for blacks than whites (68.5 ± 8.8 years vs. 71.6 ± 8.7 years; P < .01).
Table 3.
Relationship of medication adherence to risk of incident stroke/TIA - Cox hazards model using mediation analysis - indirect effects hazard ratio (95% confidence interval)*
| Reference: Morisky - 0 Affirmative | Unadjusted | Fully Adjusted |
|---|---|---|
| Morisky - 1 affirmative | 1.02 (1.00, 1.03) | 1.01 (1.00, 1.02) |
| Morisky - 2 affirmative | 1.03 (1.01, 1.06) | 1.02 (1.00, 1.04) |
| Morisky - 3 or 4 affirmative | 1.12 (1.06, 1.17) | 1.08 (1.03, 1.12) |
Systolic blood pressure used as mediating variable.
Discussion
The present paper adds to a growing literature3–7 on the importance of medication adherence by demonstrating, in a national, population-based sample, a significant relationship between lower medication adherence and inadequately controlled BP, increased FSRS, and the incidence of adjudicated stroke and TIA in the subsequent 5 years. The study demonstrates a significant inverse relationship between lower levels of medication adherence and both mean systolic BP and the percentage of subjects with inadequate BP control. While the efficacy of diet and lifestyle changes in the treatment of hypertension is known,16,18 antihypertensive medications remain the mainstay of treatment for essential hypertension. Further, adequate medication adherence is associated with improved BP control and with reductions in stroke in at risk subjects.4–6 As medication adherence declined from a Morisky score of 0 to a score of 3 or 4, the proportion of subjects with inadequately controlled BP increased by approximately 16% in whites and approximately 20% in blacks, and was associated with both increased FSRS and an increased risk for incident stroke/TIA. It is important to note that the age of onset for incident stroke/TIA events was significantly earlier (approximately 3 years on average) in blacks than in whites, suggesting that lower medication adherence may contribute to an increased risk for earlier onset of stroke/TIA events in treated black hypertensives.
These findings have important clinical implications. Because medication adherence information is often not available outside of advanced health systems, low medication adherence is frequently undetected. Recent data suggests that providers are unlikely to recognize low medication adherence,19 and, if elevated BP occurs, may intensify treatment, even in the setting of low medication adherence. The extent to which individuals take prescribed medications following treatment intensification in the setting of lower medication adherence is unknown. The extent to which subjects change adherence patterns after an office visit that includes treatment intensification is also unknown.
Substantial controversy exists about how to manage hypertensive patients in situations where office BP values are elevated yet medication adherence is low or unknown. The extent to which elevated BP values are attributable to low medication adherence versus other causes such as increased sodium intake or possible treatment resistance are not clear. Our data demonstrate that, among treated hypertensives, low medication adherence is clearly associated with risk, including uncontrolled BP, increased FSRS, and increased risk for incident stroke/TIA, suggesting the need for more effective diagnostic and intervention strategies. Preliminary data from Rose et al suggest that treatment intensification is ultimately the most effective strategy to achieve controlled BP regardless of the status of medication adherence.20 However, few randomized trials are available that define the most effective strategies to employ in this common clinical scenario of elevated BP and unknown or low medication adherence.
Our study also illustrates a small but clinically important increase in the odds of incident stroke or TIA associated with low general medication adherence, even when controlling for other relevant risk factors. This particular approach, involving a mediation analysis, suggests that this occurs via a mechanism that we would hypothesize – through inadequately controlled BP – perhaps the most important known risk factor for stroke and TIA. While the magnitude of increase in risk appears to be small, even a small increase in risk for the very large population of individuals in the U.S. with treated hypertension has important public health implications. The small increase in risk may also relate to the fact that lower medication adherence is often not an “all or none” medication-taking phenomenon. Rather, low medication adherence may involve missing a varying percentage of medication doses during limited time periods, and this may not be sufficient to result in uncontrolled BP in some individuals. Finally, the increase in risk in this general hypertensive population is lower than that reported by Gehi et al; however, these authors were studying a much higher risk population with established coronary artery disease.
This study has important limitations. Medication adherence was assessed using a self-report instrument that measures non-specific medication adherence and does not focus exclusively on cardiovascular or antihypertensive medications. Reduced medication adherence in this study was lower than that reported in some studies; self-reported medication adherence may be subject to social desirability bias and may lead to misclassification regarding the true prevalence of low medication adherence.21 Self-reported medication adherence in this large national study could not be verified by pharmacy fill/refill data or electronically monitored prescription vial caps. However, the Morisky scale is a well validated instrument that has been used for more than 25 years, and recent evidence demonstrates its correlation with pharmacy fill/refill data.10,22 BP was measured at baseline, and the time course of the relationship between self-reported medication adherence and BP control cannot be elucidated. Stroke and TIA events were self-reported or proxy reported and physician adjudicated. However, there was no systematic attempt to review medical records or insurance claims data in subjects who did not report an event.
In conclusion, these findings from a national sample of treated hypertensive individuals demonstrate that low levels of self-reported general medication adherence is strongly associated with poor BP control, increased FSRS, and subsequently with an increased risk of incident stroke or TIA. While lower medication adherence was more common among blacks and blacks had earlier onset of events, neither race nor residence in the southeastern Stroke Belt was independently associated with stroke/TIA risk in adjusted multivariate models.
Acknowledgments
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Footnotes
This paper was presented at the American Heart Association -Epidemiology and Prevention/Nutrition, 2012 Scientific Sessions. March 15, 2012, San Diego, CA.
The authors have no financial conflicts of interest to disclose.
References
- 1.Centers for Disease Control. Vital signs: prevalence, treatment, and control of hypertension—United States, 1999–2002 and 2005–2008. MMWR. 2011;60:103–8. [PubMed] [Google Scholar]
- 2.Durant RW, McClure LA, Halanych JH, Lewis CE, Prineas RJ, Glasser SP, et al. Trust in physicians and BP control in blacks and whites being treated for hypertension in the REGARDS Study. Ethnicity and Disease. 2010;20:282–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Muntner P, Halanych JH, Reynolds K, Durant R, Vupputuri S, Sung V, et al. Low medication adherence and the incidence of stroke symptoms among individuals with hypertension: data from the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. J Clin Hypertens. 2011;13:479–86. doi: 10.1111/j.1751-7176.2011.00464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey JE, Wan JY, Tang J, Ghani MA, Cushman WC. Antihypertensive medication adherence, ambulatory visits, and risk of stroke and death. J Gen Int Med. 2010;25:495–503. doi: 10.1007/s11606-009-1240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ovbiagele B, Campbell S, Faiz A, Chambless LE VISP Study Investigators. Relationship between non-specific prescription pill adherence and ischemic stroke outcomes. Cerebrovasc Dis. 2010;29:146–53. doi: 10.1159/000262311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence with cardiovascular events in patients with stable coronary heart disease. Arch Int Med. 2007;167:1798–803. doi: 10.1001/archinte.167.16.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heisler M, Hogan MM, Hofer TP, Schmittdiel JA, Pladevall M, Kerr EA. When more is not better: treatment intensification among hypertensive patients with poor medication adherence. Circulation. 2008;117:2884–92. doi: 10.1161/CIRCULATIONAHA.107.724104. [DOI] [PubMed] [Google Scholar]
- 8.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The REasons for Geographic And Racial Differences in Stroke study: objectives and design. Neuroepidemiology. 2005;25:135–43. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 9.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 10.WHO Task Force on Stroke and other Cerebrovascular Disorders: Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke. 1989;20:1407–31. doi: 10.1161/01.str.20.10.1407. [DOI] [PubMed] [Google Scholar]
- 11.ECG Reading Laboratory, Wake Forest University/-Baptist Medical Center. [Accessed December 14, 2012]; Available at: http://epicare.phs.wfubmc.edu/public/Epicare_Home.cfm.
- 12.Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar and limb leads. Am Heart J. 1949;37:161–6. doi: 10.1016/0002-8703(49)90562-1. [DOI] [PubMed] [Google Scholar]
- 13.National Cholesterol Education Program Expert Panel. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel: Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), Final Report. Bethesda, MD: National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health; Sep, 2002. (NIH publ. no. 02–5215) [Google Scholar]
- 14.D’Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke. 1994;25:40–3. doi: 10.1161/01.str.25.1.40. [DOI] [PubMed] [Google Scholar]
- 15.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 16.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. the National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection Evaluation, and Treatment of High Blood Pressure. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 17.MacKinnon DP. Introduction to Statistical Mediation Analysis. New York: Taylor & Francis; 2008. [Google Scholar]
- 18.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 19.Meddings J, Kerr EA, Heisler M, Hofer TP. Physician assessments of medication adherence and decisions to intensify medications for patients with uncontrolled blood pressure: still no better than a coin toss. BMC Health Services Research. 2012;12:270–85. doi: 10.1186/1472-6963-12-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rose AJ, Berlowitz DR, Manze M, Orner MB, Kressin NR. Intensifying therapy for hypertension despite suboptimal adherence. Hypertension. 2009;54:524–9. doi: 10.1161/HYPERTENSIONAHA.109.133389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choo PW, Rand CS, Inui TS, Lee MLT, Cain E, Cordeiro-Breault M, et al. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Medical Care. 1999;37:846–57. doi: 10.1097/00005650-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Krousel-Wood MA, Islam T, Webber LS. New medication adherence scale versus pharmacy fill rates in hypertensive seniors. Am J Man Care. 2009;15:59–66. [PMC free article] [PubMed] [Google Scholar]