Abstract
Introduction:
The optimal surgical treatment of end-stage primary glenohumeral osteoarthritis remains controversial. The objective of this article is to systematically review the current available literature to formulate evidence-based guidelines for treatment of this pathology with an arthroplasty.
Materials and Methods:
A systematic literature search was performed to identify all articles from 1990 onward that presented data concerning treatment of glenohumeral arthritis with total shoulder arthroplasty (TSA) or head arthroplasty (HA) with a minimal follow-up of 7 years. The most relevant electronic databases were searched.
Results:
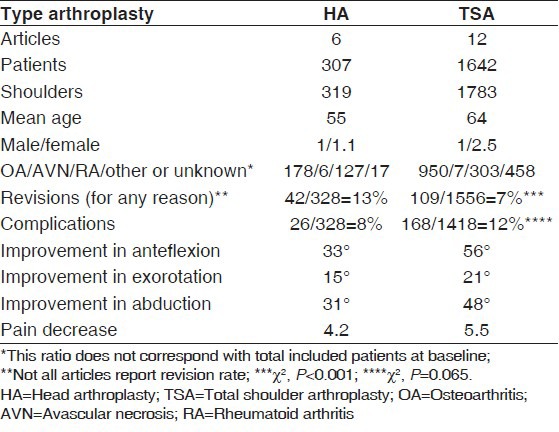
After applying the inclusion and exclusion criteria, we identified 18 studies (of the initial 832 hits). The search included a total of 1,958 patients (HA: 316 and TSA: 1,642) with 2,111 shoulders (HA: 328 + TSA: 1,783). The revision rate for any reason in the HA group (13%) was higher than in the TSA group (7%) (P < 0.001). There was a trend of a higher complication rate (of any kind) in the TSA group (12%) when compared with the HA group (8%) (P = 0.065). The weighted mean improvement in anteflexion, exorotation and abduction were respectively 33°, 15° and 31° in the HA group and were respectively 56°, 21° and 48° in the TSA group. Mean decrease in pain scores was 4.2 in the HA and 5.5 in the TSA group.
Conclusion:
Finally, we conclude that TSA results in less need for revision surgery, but has a trend to result in more complications. The conclusions of this review should be interpreted with caution as only Level IV studies could be included.
Level of Evidence:
IV.
Keywords: Arthroplasty, complication, glenoid, humerus, osteoarthritis, revision rate, shoulder, systematic review
INTRODUCTION
The total shoulder replacement is possibly the first documented replacement of a large joint in the human body. In 1893, Jules Emile Péan inserted a platinum cylinder with a rubber head in a 37-years-old patient with tuberculosis of the shoulder. The survival of the prosthesis was 2 years.[1] Since then both design and survival rates have improved significantly. Modern shoulder replacement was introduced by Neer in the 1950s for the treatment of proximal humeral fractures.[2,3] Subsequent modifications and the introduction of glenoid resurfacing broadened the indications to other disease processes, including end-stage glenohumeral osteoarthritis. If non-operative treatment for osteoarthritis fails, the surgical options commonly considered are humeral head arthroplasty (HA) (with or without the stem) and total shoulder arthroplasty (TSA). The optimal surgical treatment of end-stage primary glenohumeral osteoarthritis remains controversial. HA has the benefits of decreased operative time, decreased blood loss and less technical difficulty, yet there is concern regarding the progression of glenoid arthritic changes even with bone loss and the need for future revision surgery or conversion to TSA.[4] TSA is associated with increased operative time and blood loss, is technically more challenging and incurs risks of potential glenoid loosening and polyethylene wear.
Radnay et al.[5] performed a systematic review and meta-analysis regarding the treatment of primary glenohumeral osteoarthritis and concluded that in comparison with HA, TSA significantly improves pain relief, range of motion and patient satisfaction and has a significantly lower rate of revision surgery. However, this conclusion is not based on the long-term outcome studies.
When deciding to perform a HA or a TSA two factors are very relevant, the possibility of glenoid loosening in TSA versus the possibility of glenoid erosion when performing a HA. The most common databases were assessed to compare the revision rates of both types of arthroplasty with long-term follow-up. The objective of this article is to systematically review the current available literature to formulate evidence-based guidelines to treat glenohumeral arthritis with arthroplasty. Secondarily, we will formulate guidelines and recommendations for future research.
MATERIALS AND METHODS
Inclusion and exclusion criteria
We reviewed the titles and abstracts of all relevant articles from 1990 onward. A predefined set of criteria was followed to determine whether or not to include the material. Relevant data was selected from articles written in the English, German and Dutch languages in which arthroplasty were used as the form of treatment for glenohumeral osteoarthritis. All treatments comprised of a minimal follow-up of 7 years and all types of glenohumeral osteoarthritis were included (idiopathic, rheumatic, post-traumatic, osteonecrosis, rotator cuff arthropathy). Gleno-humeral osteoarthritis was defined as a joint disease and further characterized by several factors—loss of cartilage, subchondral sclerosis, cyst formation, deterioration of the joint and the formation of new bone (osteophytes) around the joint. History, physical examination and radiographs were all used to determine a diagnosis.
Articles concerned with arthroplasties performed after a proximal humeral or glenoid fracture or with additional bone grafting and biologic resurfacing of the glenoid were not considered. Excluded from the review were articles reporting on the results of revision operations or articles dealing with biochemical studies as well as any article concentrating on the survival of the glenoid component or stem. Articles that did not report on new patient series, such as review articles and expert opinions were not used. In addition, abstracts of scientific meetings that were not published as full text articles were not considered and any case reports on 5 or less patients were excluded. Any data presented in more than one article was only included once.
Identification of studies
A wide-ranging and comprehensive search was performed with the assistance of a clinical librarian. This search was limited to adult patients and included the following Mesh terms: Shoulder, arthroplasty, revision, survival, complication, function, pain, outcome, humerus and glenoid [Figure 1]. The PubMed/MedLine, Cochrane Clinical Trial Register and Embase databases were searched for studies performed from 1990 to October 2011. All resulting publications were additionally manually checked to verify that they met the inclusion criteria. A review of the title and abstract was performed in order to identify the relevant articles. The above mentioned criteria were then applied to the full text to determine articles for inclusion in this review. The reviews were done independently by MB and PG with disagreements handled through a group discussion. Disagreements that remained unresolved were handled through arbitration by a third author, MS. Studies were not blinded for author, affiliation and source.
Figure 1.
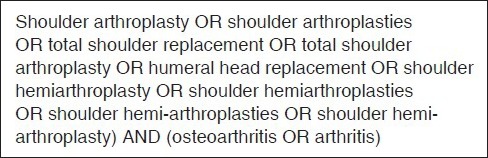
PubMed/MedLine search strategy
Data extraction
Once the initial review of the articles was complete, several data points were collected from the articles meeting the inclusion criteria: Number of patients, gender, age and type of arthroplasty, follow-up, function, pain, revision rate and general complications. A further review was done to reassess the data and determine if any of the articles met the inclusion criteria. Most studies had differing inclusion criteria, resulting in a different outcome measures. This prohibited a proper meta-analysis and comparison. The following outcome measures were compared: Pain scores, functional outcome, revision rate, complication rate and range of motion.
Quantitative analysis
The results of the included studies were pooled for dichotomous and continuous outcome measures. Dichotomous outcome measures were compared with the Chi-square test.
For continuous outcome measures, a weighted mean was calculated based on the means (and the standard deviation [SD's]) of the included studies. Lack of adequate reporting of the SD's prohibited a statistical evaluation and comparison of two types of arthroplasties for continuous outcome measures. A P value of less than 0.05 was considered significant.
Methodological quality
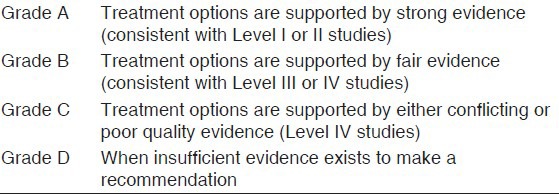
In order to determine methodological quality, the studies were accessed and assigned a level of evidence defined by the Centre for Evidence Based Medicine (http://www.cebm.net). In general, the following levels are defined in studies on therapy or prognosis: Level I is attributed to well-designed and performed randomized controlled trials; Level II is attributed to cohort studies; Level III is attributed to case control studies; Level IV is attributed to case series; and Level V is attributed to expert opinion articles [Table 1]. These evidence levels were assigned by the two authors, XX and XX, with disagreement resolved through discussion. Recommendations for clinical practices were formulated based on the level assigned and a grade was added. Grade A meant treatment options were supported by strong evidence (consistent with Level I or II studies); Grade B meant treatment options were supported by fair evidence (consistent with Level III or IV studies); Grade C meant treatment options were supported by either conflicting or poor quality evidence (Level IV studies); and Grade D was used when insufficient evidence existed to make a recommendation [Table 2].
Table 1.
Levels of evidence in intervention studies
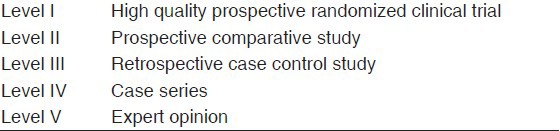
Table 2.
Grades of recommendation (given to various treatment options based on the level of evidence supporting that treatment
RESULTS
The initial search resulted in 832 hits. After applying the in-and exclusion criteria, we identified 18 series that report on the results of TSA,[6,7,8,9,10,11,12,13,14,15,16,17] or HA[5,12,18,19,20,21] [Figure 2]. The included studies are summarized in Table 3. All studies were case series (level of evidence: IV). The first study was published in 1995[5] and the most recent in 2011.[14,18] 11 series were from the US and seven were from Europe. The smallest study was from Betts et al.[6] and the largest from Walch et al.[14] The search included a total of 1958 patients (HA: 307 and TSA: 1642) with 2111 shoulders (HA: 319 + TSA: 1783) in both groups. The mean age in the HA group was 55 years and 64 years in the TSA group. The male/female ration in the HA group was 1/1.1 and 1/2.5 in the TSA group. The shoulder pathologies for which the arthroplasty was performed are summarized in Table 4.
Figure 2.
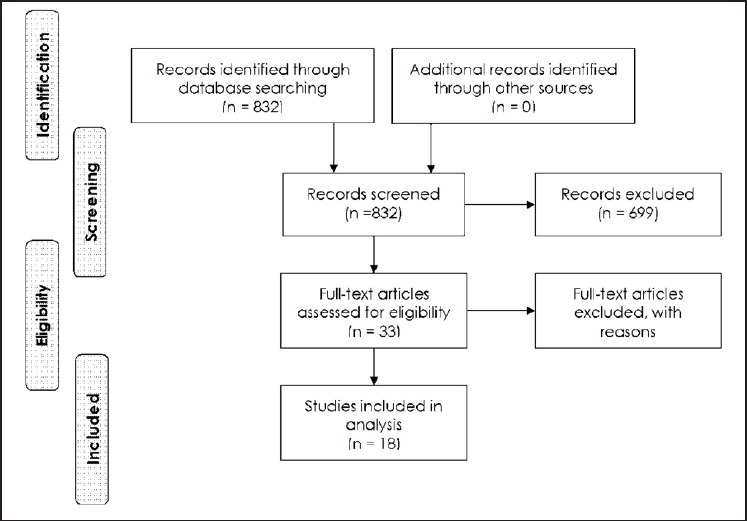
Flowchart summarizing the selection procedure for the articles eligible for systematic reviewing
Table 3.
Characteristics of included studies
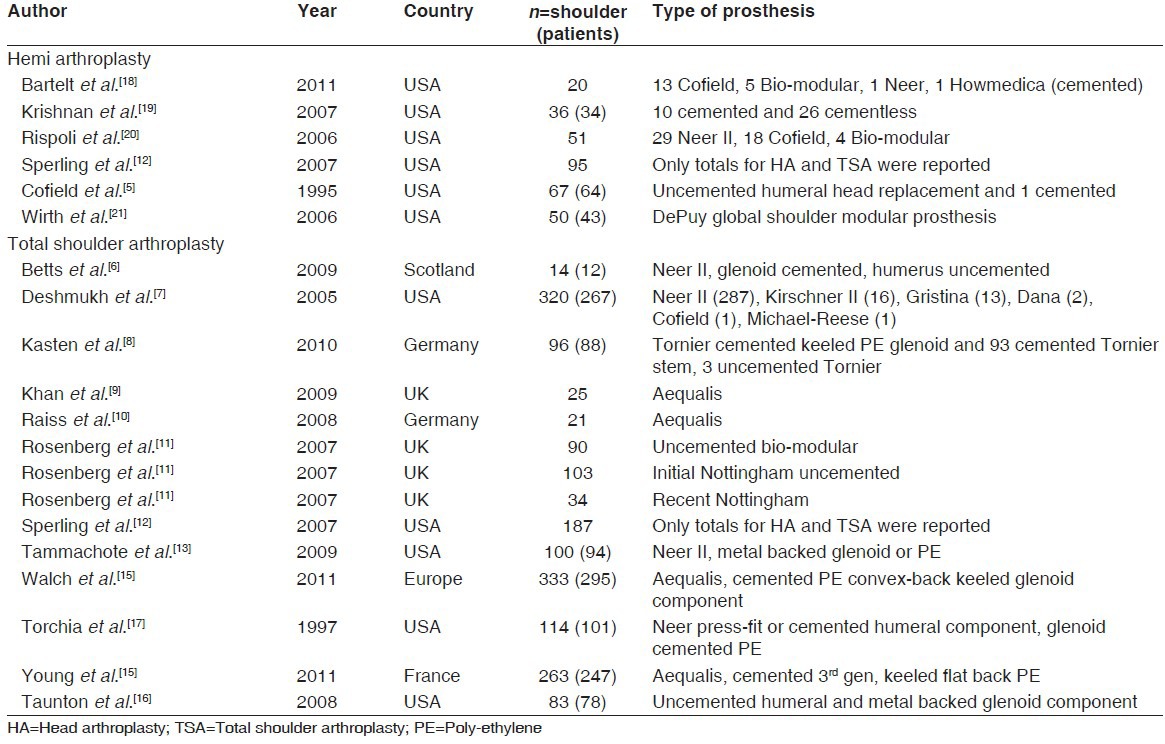
Table 4.
Results
As many studies did report a mean for continuous outcome measures, but without a SD, we calculated a weighted mean as a result no statistical comparison was possible due to the lack of reporting SD's. Pooling of functional outcome data and pain scores was not possible subsequent to a lack of data.
Revisions
Revision rate was reported by all but one study.[11] The revision rate for any reason in the HA group (13%) was higher than in the TSA group (7%) (P < 0.001). No difference was made between revisions of the humeral or glenoid component. The revision rate was calculated of all 1884 (328 HA + 1556 TSA) shoulders. In the HA group five revisions were performed for other reasons than painful glenoid or glenoid arthritis. Almost all patients with glenoid erosion were revised to a TSA.
Complications
Complication rate was reported by al studies; although, the exact type of complication was not mentioned in all articles. There was a trend of a higher complication rate (of any kind) in the TSA group (12%) when compared with the HA group (8%) (P = 0.065). This rate could be calculated over 1746 (328 HA + 1418 TSA) shoulders.
Range of movement
Improvement in the range of movement was reported by all series in the HA group[5,12,18,19,20,21] and by ten series in the TSA group.[8,9,10,11,12,13,14,15,16,17] The weighted mean improvement in anteflexion, exorotation and abduction were respectively 33°, 15° and 31° in the HA group. The weighted mean improvement in anteflexion, exorotation and abduction were respectively 56°, 21° and 48° in the TSA group. A statistical comparison was not possible due to the missing SD's reported in the included articles.
Pain decrease
Four studies concerning TSA[6,9,12,16] and 4[12,18,20,21] reporting a decrease in pain after HA were included in this analysis. Mean decrease in pain scores was 4.2 in the HA group and 5.5 in the TSA group. Scores reported on a 5 point scale were calculated to a 10 point scale and pain scores from constant scores were not included in this analysis.
DISCUSSION
The objective of this systematic review was to collect evidence concerning the long-term outcome of HA and TSA and to compare these two treatments. After including 18 articles, we concluded that TSA results in less revision surgery, but results in more complications. This is the first review with a strict methodology based on a large sample size, which compares the long-term (mean FU of included studies was at least 7 years) outcome of HA and TSA for osteoarthritis of the shoulder.
The conclusions of this review should be interpreted with caution due some limitations. Firstly, only Level IV studies could be included; there are no randomized or controlled trials with a long-term (>7 years) follow-up. There are differences in some baseline characteristics and duration of follow-up between the 2 groups. A relation between underlying diagnosis and risk of revision of both arthroplasties was described.[22] There is also a relation between gender and revision rates, with male gender having twice the risk of revision of shoulder arthroplasties.[23,24,25] Based on a series of patients with a TSA, Henn et al. concluded that younger patients have greater expectations of a TSA, which may have implications for the outcome and implant longevity.[26] Farng et al.[27] concluded that implant survival is largely driven by factors associated with increased activity and age. We did not evaluate body mass index and comorbidities as these were not associated with an increased risk of revision.[22]
There are only 18 publications, which report on the long-term results of total or hemi shoulder arthroplasty. This low number is astonishing when considering the increasing number of shoulder arthroplasties performed annually in the western world.[28] And that the first arthroplasty was performed in 1893, with the shoulder arthroplasty being popularized in the fifties by Neer.[2,3]
Comparison of the continuous outcome measures (pain, range of movement) was not possible due to lack of reporting of SD's in the original articles. The differences between anteflexion, exorotation and abduction were in favor of the TSA, respectively 23°, 6° and 17°.
Many studies are performed by high volume and designer groups so the results will probably be better than in lower volume centers. Hammond et al. conclude that patients of surgeons with higher average annual caseloads of TSA and HA have decreased complication rates and hospital lengths of stay compared with patients of surgeons who perform fewer of these procedures.[29]
We included articles from 1990 (with minimal follow-up of 7 years) so all arthroplasties performed from 1983 and later will be included in our analysis. The design of the arthroplasties and especially of the glenoid components has improved in these years. Strauss et al.[28] reviewed the literature and concluded that no definitive conclusions can be made with respect to an optimal design. Biomechanical and early clinical data indicate that pegged, curved-back, cemented prostheses with a radial mismatch of 4-7 mm provides an improved opportunity for stable long-term fixation, provided that it is implanted with the most advanced cement preparation techniques, in the proper version and is fully seated.[28]
Current review and other recent other systematic reviews[25,30,31] conclude that TSA has some advantages over HA. Despite this, many HAs are still used for primary glenohumeral arthritis.[32] We propose careful consideration of both options, but analysis of existing evidence shows a preference toward TSA. Some surgeons state that a HA can always be converted to a TSA in cases of symptomatic glenoid erosion. Carroll et al. however, concluded that the results of a revision of a HA to a TSA are inferior to those of primary TSA and this operation should be considered as a salvage procedure.[4]
For future research projects, it would be interesting to report the long-term results of previously reported RCT's or to initiate a large multicenter trial. Ideally, these long-term follow-up multicenter trials would have a sample size calculation, use computer randomization, would focus on patient related outcome measures and would have blinding of the patients and outcome assessors.[33]
CONCLUSIONS
TSA results in less need for revision surgery when compared to hemiarthroplasty (Grade C).
TSA has a trend to result in more complications when compared to hemiarthroplasty (Grade C).
ACKNOWLEDGMENT
This study was presented on the Annual Amphia Shoulder Meeting. The authors are grateful to Hanny Vriends for her help with the systematic search and collecting the required articles. The authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice or other charitable or non-profit organization with which the authors or a member of their immediate families, are affiliated or associated.
Footnotes
Source of Support: Nil
Conflict of Interest: There are no conflicts of interest.
REFERENCES
- 1.The classic: On prosthetic methods intended to repair bone fragments. Clin Orthop Relat Res. 1973;94:4–7. doi: 10.1097/00003086-197307000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Neer CS., 2nd Articular replacement for the humeral head. J Bone Joint Surg Am. 1955;37-A:215–28. [PubMed] [Google Scholar]
- 3.Neer CS., 2nd Indications for replacement of the proximal humeral articulation. Am J Surg. 1955;89:901–7. doi: 10.1016/0002-9610(55)90160-4. [DOI] [PubMed] [Google Scholar]
- 4.Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: Long-term results. J Shoulder Elbow Surg. 2004;13:599–603. doi: 10.1016/j.jse.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 5.Cofield RH, Frankle MA, Zuckerman JD. Humeral head replacement for glenohumeral arthritis. Semin Arthroplasty. 1995;6:214–21. [PubMed] [Google Scholar]
- 6.Betts HM, Abu-Rajab R, Nunn T, Brooksbank AJ. Total shoulder replacement in rheumatoid disease: A 16- to 23-year follow-up. J Bone Joint Surg Br. 2009;91:1197–200. doi: 10.1302/0301-620X.91B9.22035. [DOI] [PubMed] [Google Scholar]
- 7.Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: Long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14:471–9. doi: 10.1016/j.jse.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 8.Kasten P, Pape G, Raiss P, Bruckner T, Rickert M, Zeifang F, et al. Mid-term survivorship analysis of a shoulder replacement with a keeled glenoid and a modern cementing technique. J Bone Joint Surg Br. 2010;92:387–92. doi: 10.1302/0301-620X.92B3.23073. [DOI] [PubMed] [Google Scholar]
- 9.Khan A, Bunker TD, Kitson JB. Clinical and radiological follow-up of the aequalis third-generation cemented total shoulder replacement: A minimum ten-year study. J Bone Joint Surg Br. 2009;91:1594–600. doi: 10.1302/0301-620X.91B12.22139. [DOI] [PubMed] [Google Scholar]
- 10.Raiss P, Aldinger PR, Kasten P, Rickert M, Loew M. Total shoulder replacement in young and middle-aged patients with glenohumeral osteoarthritis. J Bone Joint Surg Br. 2008;90:764–9. doi: 10.1302/0301-620X.90B6.20387. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg N, Neumann L, Modi A, Mersich IJ, Wallace AW. Improvements in survival of the uncemented Nottingham total shoulder prosthesis: A prospective comparative study. BMC Musculoskelet Disord. 2007;8:76. doi: 10.1186/1471-2474-8-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sperling JW, Cofield RH, Schleck CD, Harmsen WS. Total shoulder arthroplasty versus hemiarthroplasty for rheumatoid arthritis of the shoulder: Results of 303 consecutive cases. J Shoulder Elbow Surg. 2007;16:683–90. doi: 10.1016/j.jse.2007.02.135. [DOI] [PubMed] [Google Scholar]
- 13.Tammachote N, Sperling JW, Vathana T, Cofield RH, Harmsen WS, Schleck CD. Long-term results of cemented metal-backed glenoid components for osteoarthritis of the shoulder. J Bone Joint Surg Am. 2009;91:160–6. doi: 10.2106/JBJS.F.01613. [DOI] [PubMed] [Google Scholar]
- 14.Walch G, Young AA, Melis B, Gazielly D, Loew M, Boileau P. Results of a convex-back cemented keeled glenoid component in primary osteoarthritis: Multicenter study with a follow-up greater than 5 years. J Shoulder Elbow Surg. 2011;20:385–94. doi: 10.1016/j.jse.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Young A, Walch G, Boileau P, Favard L, Gohlke F, Loew M, et al. A multicentre study of the long-term results of using a flat-back polyethylene glenoid component in shoulder replacement for primary osteoarthritis. J Bone Joint Surg Br. 2011;93:210–6. doi: 10.1302/0301-620X.93B2.25086. [DOI] [PubMed] [Google Scholar]
- 16.Taunton MJ, McIntosh AL, Sperling JW, Cofield RH. Total shoulder arthroplasty with a metal-backed, bone-ingrowth glenoid component. Medium to long-term results. J Bone Joint Surg Am. 2008;90:2180–8. doi: 10.2106/JBJS.G.00966. [DOI] [PubMed] [Google Scholar]
- 17.Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the neer prosthesis: Long-term results. J Shoulder Elbow Surg. 1997;6:495–505. doi: 10.1016/s1058-2746(97)90081-1. [DOI] [PubMed] [Google Scholar]
- 18.Bartelt R, Sperling JW, Schleck CD, Cofield RH. Shoulder arthroplasty in patients aged fifty-five years or younger with osteoarthritis. J Shoulder Elbow Surg. 2011;20:123–30. doi: 10.1016/j.jse.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 19.Krishnan SG, Nowinski RJ, Harrison D, Burkhead WZ. Humeral hemiarthroplasty with biologic resurfacing of the glenoid for glenohumeral arthritis. Two to fifteen-year outcomes. J Bone Joint Surg Am. 2007;89:727–34. doi: 10.2106/JBJS.E.01291. [DOI] [PubMed] [Google Scholar]
- 20.Rispoli DM, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am. 2006;88:2637–44. doi: 10.2106/JBJS.E.01383. [DOI] [PubMed] [Google Scholar]
- 21.Wirth MA, Tapscott RS, Southworth C, Rockwood CA., Jr Treatment of glenohumeral arthritis with a hemiarthroplasty: A minimum five-year follow-up outcome study. J Bone Joint Surg Am. 2006;88:964–73. doi: 10.2106/JBJS.D.03030. [DOI] [PubMed] [Google Scholar]
- 22.Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: Analysis of 2588 shoulders over three decades (1976 to 2008) J Bone Joint Surg Br. 2011;93:1513–7. doi: 10.1302/0301-620X.93B11.26938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox TJ, Cil A, Sperling JW, Sanchez-Sotelo J, Schleck CD, Cofield RH. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:859–63. doi: 10.1016/j.jse.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 24.Martin SD, Zurakowski D, Thornhill TS. Uncemented glenoid component in total shoulder arthroplasty. Survivorship and outcomes. J Bone Joint Surg Am. 2005;87:1284–92. doi: 10.2106/JBJS.C.00947. [DOI] [PubMed] [Google Scholar]
- 25.Singh JA, Sperling J, Buchbinder R, McMaken K. Surgery for shoulder osteoarthritis. Cochrane Database Syst Rev. 2010;10 doi: 10.1002/14651858.CD008089.pub2. >CD008089. [DOI] [PubMed] [Google Scholar]
- 26.Henn RF, 3rd, Ghomrawi H, Rutledge JR, Mazumdar M, Mancuso CA, Marx RG. Preoperative patient expectations of total shoulder arthroplasty. J Bone Joint Surg Am. 2011;93:2110–5. doi: 10.2106/JBJS.J.01114. [DOI] [PubMed] [Google Scholar]
- 27.Farng E, Zingmond D, Krenek L, Soohoo NF. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20:557–63. doi: 10.1016/j.jse.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 28.Strauss EJ, Roche C, Flurin PH, Wright T, Zuckerman JD. The glenoid in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:819–33. doi: 10.1016/j.jse.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 29.Hammond JW, Queale WS, Kim TK, McFarland EG. Surgeon experience and clinical and economic outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2003;85-A:2318–24. doi: 10.2106/00004623-200312000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Bryant D, Litchfield R, Sandow M, Gartsman GM, Guyatt G, Kirkley A. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am. 2005;87:1947–56. doi: 10.2106/JBJS.D.02854. [DOI] [PubMed] [Google Scholar]
- 31.Radnay CS, Setter KJ, Chambers L, Levine WN, Bigliani LU, Ahmad CS. Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: A systematic review. J Shoulder Elbow Surg. 2007;16:396–402. doi: 10.1016/j.jse.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 32.Rasmussen JV, Jakobsen J, Brorson S, Olsen BS. The Danish shoulder arthroplasty registry: Clinical outcome and short-term survival of 2,137 primary shoulder replacements. Acta Orthop. 2012;83:171–3. doi: 10.3109/17453674.2012.665327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: A multicenter study. J Shoulder Elbow Surg. 2002;11:130–5. doi: 10.1067/mse.2002.121146. [DOI] [PubMed] [Google Scholar]


