Abstract
Traumatic injuries are the most studied yet most challenging for a dentist. Extrusive luxation injuries are usually managed by repositioning tooth in the original position and pulp sensibility is evaluated at regular periodic intervals. However, when injuries are chronic, tooth is necrotic with compromised periodontal support, treatment is a challenge. Intentional replantation utilizing growth factors in fibrin rich network of platelet rich fibrin can be a treatment modality in such patients where other restorative modalities to establish function-esthetics rehabilitation is not possible.
Keywords: Extrusive luxation, permanent tooth, platelet rich fibrin, reimplantation, wound healing
INTRODUCTION
Traumatic injuries are one of the most studied and yet most difficult to manage in dentistry. Most traumatic injuries occur in childhood and adolescence.[1] Management of traumatic injuries requires multidisciplinary approach. Treatment is complex and the prognosis is often uncertain.[2] Andersen et al.,[3] identified five different types of luxation injuries, i.e., concussion, subluxation, extrusive luxation, lateral luxation and intrusive luxation. Luxation injuries comprise 15-61% of dental trauma to permanent teeth; while frequency of 62-72% has been reported in the primary dentition.[3] Predominant etiologic factors of luxation injuries in the permanent dentition are bicycle injuries, falls, fights and sport injuries, whereas fall dominate in the primary dentition.
Prognosis of these injuries is dependent on various factors such as degree and type of displacement, treatment delays, root maturation, associated crown fractures and type of displacement.[4,5,6] Extruded teeth should be immediately repositioned and splinted with a flexible splint for 2-3 weeks.[7] If complete repositioning is not possible due to treatment delay, arrangement is required to position apically using orthodontic forces.
However, when extrusive luxation is severe and the tooth is greatly mobile, extraction is the preferred treatment and replacement can be carried out using removable partial denture (RPD), fixed partial denture (FPD) or implant placement. In patients who cannot afford implant due to financial constrains or FPD is contraindicated due to growing age, then intentional replantation can be considered as an alternative treatment modality.[8]
Intentional replantation is defined as intentional removal of tooth and reinsertion into extraction socket before or after endodontic treatment.[9] It can be considered as the last resort in maintaining tooth with hopeless prognosis as treatment usually aims at most conservative option that satisfy individual esthetic and functional requirements.
Here, we present a case of a 16-year-old boy, where management of extrusive luxation of the left central incisor (21) was done by intentional replantation using benefits of platelet rich fibrin (PRF) in attempt to regenerate lost periodontal structure.
CASE REPORT
A 16-year-old boy reported, with a chief complaint of mobile upper front teeth. His dental history revealed history of trauma 8 months back. Trauma led to avulsed maxillary right central incisor (11), extrusively luxated displaced out of the arch with Grade III mobility maxillary left central incisor (21), fractured (Ellis Class III) left lateral incisor (22) [Figure 1].
Figure 1.

Initial presentation: Shows extrusive luxated central incisor and fractured lateral incisor
Pulp sensibility was performed and both left central and lateral incisor (21, 22) were found to be nonresponsive. Intraoral radiographs revealed severe bone loss with respect to maxillary left elicited with right lateral incisor (12). Fremitus test was found to be negative. Case was diagnosed as primary endo and secondary perio lesion. The prognosis of tooth (21) appeared to be hopeless. Hence, extraction was advised for the left central incisor (21), which was extruded, non-responsive and had severe bone loss. Various replacement options such as RPD and implant were suggested to patient, but patient was keen on retaining his natural tooth and had financial constraints.
Hence, intentional replantation was considered as a treatment option. The probable outcome of treatment and complication were explained to patient and written consent was obtained.
The main goal of treatment was to achieve a conservative approach and thereby fulfill the individual's requirement. Treatment plan consisted of Phase I therapy followed by endodontic treatment, which was to be followed by intentional replantation.
Phase I therapy was performed and patient was posted for endodontic treatment. Calcium hydroxide dressing was given for 2 weeks followed by obturation with Gutta percha.[10] Surgery was planned 1 week after completion of endodontic treatment.
Local anesthesia (2% lignocaine HCl with 1:80000 adrenalines) was administered. Full thickness mucoperiosteal flap was reflected. On flap reflection, severe bone loss extending more than 2/3rd root length on palatal aspect was seen [Figure 2]. Tooth was atraumatically extracted and was immediately placed in a solution of tetracycline (500 mg of tetracycline dissolved in 20 ml saline) for a period of 5 min[11,12] and was then transferred to a solution of sodium fluoride (0.05% w/v) for a period of 5 min [Figures 3 and 4]. After degranulation and curettage, PRF was prepared.
Figure 2.
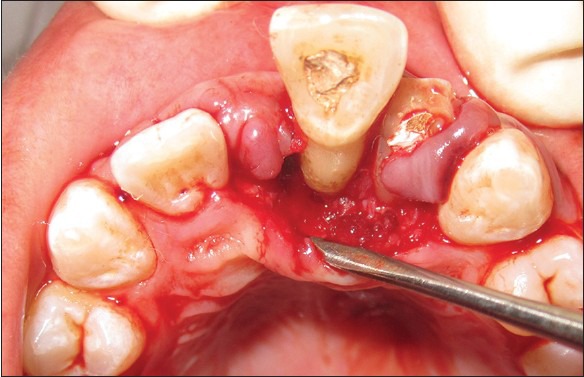
Palatal flap reflection shows severe bone loss
Figure 3.

Tooth extracted atraumatically and subjected to solution of tetracycline
Figure 4.

Tooth transferred to solution of sodium fluoride
A total volume 10 ml of blood was withdrawn, which was immediately centrifuged at 3000 rpm for preparation of PRF.[13,14] PRF obtained was mixed with nano hydroxyapatite (HA) crystals and was placed in the tooth socket and bony defect. The tooth was replanted and aligned [Figure 5]. Flap was repositioned immediately and sutured using 3-0 silk sutures. Fiber reinforced composite resin splinting was done, periodontal pack was applied. Patient was put on amoxicillin 500 mg tid for 5 days and a combination of aceclofenac and paracetamol bid was given for 3 days. Mouthwash containing 0.2% chlorhexidine was advised from the day following surgery. Patient was recalled after 1 week for suture removal, revealed satisfactory healing was seen.
Figure 5.

Tooth reimplanted in socket
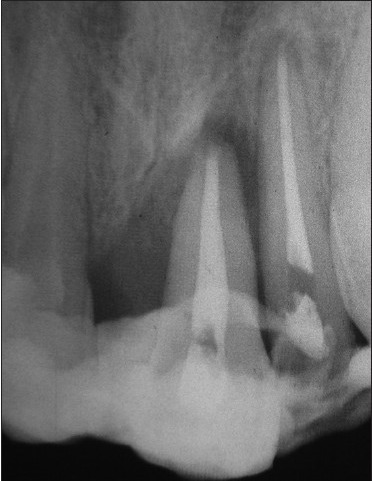
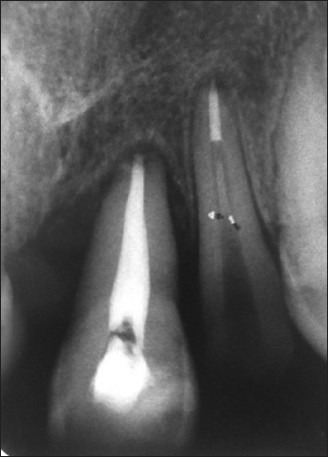
Intraoral periapical radiograph (IOPAR) using long cone technique was taken to ascertain alignment of the tooth [Figures 6 and 7]. Oral hygiene instruction was reinforced and strict instruction not to bite on anterior teeth was given. Patient was put on regular recall visits.
Figure 6.

Pre-operative intraoral periapical radiograph showing extensive bone loss
Figure 7.

Post-operative intraoral periapical radiograph taken after 7 days, to ascertain alignment of tooth and apical positioning
Patient was recalled after 2 months and it was observed that there was a significant reduction in in probing pocket depth. Radiograph taken revealed radiopacity in periapical area suggestive of periodontal repair or regeneration [Figure 8].
Figure 8.
Intraoral periapical radiograph taken 2 months post-operative: Shows radiopacity in periapical area, suggestive of periodontal repair or regenerate
In 3rd month, IOPAR has taken revealed significant radiopacity in periapical area [Figure 9]. Splint was removed. Mobility was found to be remarkably reduced to Grade I with a significant reduction in probing pocket depth. As mobility was reduced and patient was comfortable, esthetic correction was planned. Right central incisor (11) had avulsed and the left central incisor (21) had migrated toward midline so, a composite buildup of right lateral incisor (12) was performed. This was followed by restoration of Ellis Class III fractured 22, using post-placement followed by composite buildup [Figure 10]. Furthermore, lingual splint was placed in the region of 22 and 21 [Figure 11].
Figure 9.

Intraoral periapical radiograph 3 months post-operative: Shows definitive radiopacity in periapical area
Figure 10.

Esthetic outcome after splint removal, core placement and composite buildup
Figure 11.

Lingual splint placed
Patient was satisfied with the esthetic outcome. Patient has been followed-up for 6 months and so far the treatment outcome has been found to be esthetically and functionally satisfactory.
DISCUSSION
In the present case, patient was young and had financial constraints for implant therapy. He was willing to save the tooth in spite of the informed risks and chances of treatment failure.
One of the factors affecting prognosis is treatment delay. Prognosis of immediately reimplanted tooth is good compared with delayed reimplanted tooth. This could be due to the presence of viable periodontal ligament (PDL) cell in immediately transplanted tooth. In this case tooth was extrusively luxated since 8 months, hence it can be assumed, that portion of root exposed would be devoid of vital PDL cells, which can act as a nidus of infection and thereby lead to external root resorption. Hence, the tooth was treated with a solution of tetracycline, which is known to have antibacterial, anti-inflammatory and also has anti-collagenase property. Tooth was transferred to Sodium fluoride solution (0.05%) to promote mineralization and to prevent root resorption. Studies of intentional replantation in periodontally involved hopeless teeth with Class III mobility, more than 50% bone loss and deep pockets after tetracycline – HCl treatment had shown good results in bone gain and a reduction in pocket depth at the end of 6 months.[8]
Intentional replantation is generally contraindicated in periodontally compromised teeth, however, there are reports suggesting that it can be a successful treatment alternative for periodontally involved hopeless teeth.[15,16,17] which is similar to our case, where the tooth showed a significant reduction in bone gain, reduction in probing depth and mobility after replantation.
Recently, there has been a paradigm shift of regenerative procedure with interest being toward Growth factors, which are a group of natural biologic mediators that regulate key cellular events in tissue regeneration including cell proliferation, chemotaxis, differentiation and matrix synthesis.[18]
PRF, developed by Choukroun et al. in 2001[13,14] is considered as 2nd generation platelet growth factor. It is prepared by centrifugation of blood at 3000 rpm for a period of 10 min. Unlike platelet rich plasma (PRP), PRF does not require the addition of anticoagulant and bovine thrombin and hence there is no chance of antigenicity. PRF looks like a fibrin network and leads to more efficient cell migration and proliferation and thus cicatrization.[19] This unique structure may act as a vehicle for carrying cells that are essential for tissue regeneration. Many growth factors, such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-β), are released from PRF.[20,21,22] PRF consists of a fibrin matrix polymerized in a tetramolecular structure, with the incorporation of platelets, leukocyte and cytokines and circulating stem cells.[20] Organized dense fibrin scaffold of PRF with a high number of leukocytes is concentrated in one part of the clot[23] in vitro studies shows slow and specific release of growth factors (such as TGF-β, PDGF-AB and vascular endothelial growth factor) and glycoproteins (such as thrombospondin-1) for a period ≥7 days.[22] To best of our knowledge none of studies have reported the release pattern of growth factors in vivo. However, based on results of in vitro studies it can be assumed that growth factors are released through out early healing period.
To the best of our knowledge, no studies have reported the clinical use of autologous PRF for treatment of replantation or for managing tooth with hopeless prognosis. Hence taking advantages of PRF into consideration, PRF was used in this case as an adjunctive treatment modality. As the concentration of leukocytes and platelets are more toward the end of the clot, the portion of clot nearest to the red blood cell (RBC) layer was placed PRF clot obtained is inhomogeneous because leukocytes and platelets are concentrated toward the end of clot, portion of the clot toward RBC end was placed in the defect.
Earlier studies with PRF have demonstrated faster healing and bone fill when used in the treatment of cystic cavity,[20] sinus lift procedures,[24] socket preservation,[20] palatal bandage[25] and mandibular Grade II furcation defects.[26]
PRF has been used alone or in combination with bone grafts like HA particles. Porous hydroxyapatite (HAp) bone grafting material has been used to fill periodontal intrabony defects, which has resulted in clinically acceptable responses.[27] It has been shown that HAp bone grafts have excellent bone conductive properties, which permit outgrowth of osteogenic cells from existing bone surfaces into the adjacent bone material.[28]
In the present case, the bone fill and improvement in clinical attachment level could be due to the dual effect of HA and PRF, whereby the HA acts as a space maintainer for tissue regeneration as well as the osteoconductive nature of HA with benefits of sustained release of growth factors could have played a role in the success of the treatment. Results of the present case is similar to the case report of Demir et al. who reported significant bone gain in a case of intentional replanted periodontally involved hopeless teeth with Class III mobility when it was intentionally replanted with PRP, bioactive glass graft material and non-resorbable polytetrafluoroethylene membrane, 12 month follow-up showed significant bone formation and reduction in mobility.[8]
PDGF-BB have been applied to the root surface of extracted teeth in animal studies, which were replanted, it was found to reduce the occurrence of ankylosis and root resorption.[29] In 6 months follow-up in this case, no resorption was seen [Figure 12].
Figure 12.
Intra oral periapical radiograph 6 months post-operative: Shows definitive bone formation in periapical area
Immediate post-operative radiograph revealed good apical positioning of the tooth and alignment with adjacent tooth. Tooth was placed in the arch and immediately splinted with rigid splint. Use of non-rigid splint has been reported, but there is no studies documenting the type of splint to be used in management of traumatized tooth with severe bone loss. In this case, we initially used a rigid splint, which was later replaced by a non-rigid fiber mesh, so as to prevent any complication of ankylosis.
In this case, we did not opt for prosthetic replacement such as FPD as the boy was 16-year-old and was still in the growing phase and had financial constraints. We tried to achieve the maximum esthetic result using composite restorations, which was essential for a young boy.
This case highlights the importance of interdisciplinary approach to successfully manage a traumatized extrusive luxated tooth using a new treatment approach to bring about esthetic and functional rehabilitation.
CONCLUSION
Intentional replantation with PRF can be an alternate and effective treatment modality for management of tooth with a hopeless prognosis. Procedure itself is conservative and relatively inexpensive. The result of the case shows a promising future. Hence, further studies and long-term follow-up is needed to establish this modality of treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM. Replantation of 400 avulsed permanent incisors. 2. Factors related to pulpal healing. Endod Dent Traumatol. 1995;11:59–68. doi: 10.1111/j.1600-9657.1995.tb00462.x. [DOI] [PubMed] [Google Scholar]
- 2.Drummond S, Pessica LS, Monnerat AB, Monnerat AF, de Oliveira Almeida MA. Multidisciplinary solution for an avulsed upper central incisor: Case report. Dent Traumatol. 2011;27:241–6. doi: 10.1111/j.1600-9657.2011.00975.x. [DOI] [PubMed] [Google Scholar]
- 3.Andersen JO, Andersen FM, Anderson L. 4th ed. Oxford: Blackwell Munksgaard; 2007. Textbook and Color Atlas of Traumatic Injuries to the Teeth. [Google Scholar]
- 4.Lee R, Barrett EJ, Kenny DJ. Clinical outcomes for permanent incisor luxations in a pediatric population. II. Extrusions. Dent Traumatol. 2003;19:274–9. doi: 10.1034/j.1600-9657.2003.00208.x. [DOI] [PubMed] [Google Scholar]
- 5.Humphrey JM, Kenny DJ, Barrett EJ. Clinical outcomes for permanent incisor luxations in a pediatric population. I. Intrusions. Dent Traumatol. 2003;19:266–73. doi: 10.1034/j.1600-9657.2003.00207.x. [DOI] [PubMed] [Google Scholar]
- 6.Moule AJ, Moule CA. Minor traumatic injuries to the permanent dentition. Dent Clin North Am. 2009;53:639–59. doi: 10.1016/j.cden.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Kahler B, Heithersay GS. An evidence-based appraisal of splinting luxated, avulsed and root-fractured teeth. Dent Traumatol. 2008;24:2–10. doi: 10.1111/j.1600-9657.2006.00480.x. [DOI] [PubMed] [Google Scholar]
- 8.Demir B, Demiralp B, Güncü GN, Uyanik MO, Cağlayan F. Intentional replantation of a hopeless tooth with the combination of platelet rich plasma, bioactive glass graft material and non-resorbable membrane: A case report. Dent Traumatol. 2007;23:190–4. doi: 10.1111/j.1600-9657.2005.00414.x. [DOI] [PubMed] [Google Scholar]
- 9.Weine FS. The case against intentional replantation. J Am Dent Assoc. 1980;100:664–8. doi: 10.14219/jada.archive.1980.0227. [DOI] [PubMed] [Google Scholar]
- 10.Moule AJ, Moule CA. The endodontic management of traumatized permanent anterior teeth: A review. Aust Dent J. 2007;52:S122–37. doi: 10.1111/j.1834-7819.2007.tb00520.x. [DOI] [PubMed] [Google Scholar]
- 11.Ritter AL, Ritter AV, Murrah V, Sigurdsson A, Trope M. Pulp revascularization of replanted immature dog teeth after treatment with minocycline and doxycycline assessed by laser Doppler flowmetry, radiography, and histology. Dent Traumatol. 2004;20:75–84. doi: 10.1111/j.1600-4469.2004.00225.x. [DOI] [PubMed] [Google Scholar]
- 12.Cvek M, Cleaton-Jones P, Austin J, Lownie J, Kling M, Fatti P. Effect of topical application of doxycycline on pulp revascularization and periodontal healing in reimplanted monkey incisors. Endod Dent Traumatol. 1990;6:170–6. doi: 10.1111/j.1600-9657.1990.tb00413.x. [DOI] [PubMed] [Google Scholar]
- 13.Choukroun J, Adda F, Schoeffler C, Vervelle A. Une opportunité en paro-implantologie: le PRF. Implantodontie. 2001;42:55–62. [Google Scholar]
- 14.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45–50. doi: 10.1016/j.tripleo.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Lu DP. Intentional replantation of periodontally involved and endodontically mistreated tooth. Oral Surg Oral Med Oral Pathol. 1986;61:508–13. doi: 10.1016/0030-4220(86)90396-8. [DOI] [PubMed] [Google Scholar]
- 16.Baykara M, Eratalay K. Replantation in cases with advanced periodontal destruction. J Hacettepe Fac Dent. 1995;19:124–8. [Google Scholar]
- 17.Demiralp B, Nohutçu RM, Tepe DI, Eratalay K. Intentional replantation for periodontally involved hopeless teeth. Dent Traumatol. 2003;19:45–51. doi: 10.1034/j.1600-9657.2003.00084.x. [DOI] [PubMed] [Google Scholar]
- 18.Giannobile WV. The potential role of growth and differentiation factors in periodontal regeneration. J Periodontol. 1996;67:545–53. [PubMed] [Google Scholar]
- 19.Dohan Ehrenfest DM, Del Corso M, Diss A, Mouhyi J, Charrier JB. Three-dimensional architecture and cell composition of a Choukroun's platelet-rich fibrin clot and membrane. J Periodontol. 2010;81:546–55. doi: 10.1902/jop.2009.090531. [DOI] [PubMed] [Google Scholar]
- 20.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 21.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part V: Histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:299–303. doi: 10.1016/j.tripleo.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 22.Dohan Ehrenfest DM, de Peppo GM, Doglioli P, Sammartino G. Slow release of growth factors and thrombospondin-1 in Choukroun's platelet-rich fibrin (PRF): A gold standard to achieve for all surgical platelet concentrates technologies. Growth Factors. 2009;27:63–9. doi: 10.1080/08977190802636713. [DOI] [PubMed] [Google Scholar]
- 23.Dohan Ehrenfest DM, Diss A, Odin G, Doglioli P, Hippolyte MP, Charrier JB. In vitro effects of Choukroun's PRF (platelet-rich fibrin) on human gingival fibroblasts, dermal prekeratinocytes, preadipocytes, and maxillofacial osteoblasts in primary cultures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:341–52. doi: 10.1016/j.tripleo.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 24.Toffler M, Toscano N, Holtzclaw D. Osteotome-mediated sinus floor elevation using only platelet-rich fibrin: An early report on 110 patients. Implant Dent. 2010;19:447–56. doi: 10.1097/ID.0b013e3181f57288. [DOI] [PubMed] [Google Scholar]
- 25.Aravindaksha SP. Batra PUse of platelet rich fibrin (PRF) membrane as palatal bandage. Clin Adv Periodontics. Available from: http://www.joponline.org/doi/pdf/10.1902/cap.2013.130011 . In press.
- 26.Sharma A, Pradeep AR. Autologous platelet-rich fibrin in the treatment of mandibular degree II furcation defects: A randomized clinical trial. J Periodontol. 2011;82:1396–403. doi: 10.1902/jop.2011.100731. [DOI] [PubMed] [Google Scholar]
- 27.Kenney EB, Lekovic V, Han T, Carranza FA, Jr, Dimitrijevic B. The use of a porous hydroxylapatite implant in periodontal defects. I. Clinical results after six months. J Periodontol. 1985;56:82–8. doi: 10.1902/jop.1985.56.2.82. [DOI] [PubMed] [Google Scholar]
- 28.Bowen JA, Mellonig JT, Gray JL, Towle HT. Comparison of decalcified freeze-dried bone allograft and porous particulate hydroxyapatite in human periodontal osseous defects. J Periodontol. 1989;60:647–54. doi: 10.1902/jop.1989.60.12.647. [DOI] [PubMed] [Google Scholar]
- 29.Noda K, Seshima F, Okubo N, Ishii Y, Ota M, Yamada S, et al. Effect of platelet-derived growth factor-BB on root resorption after reimplantation of partially denuded tooth in dog. Dent Traumatol. 2012;28:217–25. doi: 10.1111/j.1600-9657.2011.01070.x. [DOI] [PubMed] [Google Scholar]


