Abstract
Background:
The relationship between anxiety and obesity is still debatable and seems to vary between cultures. The subject has been scarcely investigated in Nigeria, hence this study.
Materials and Methods:
A total of 1584 young-adult Nigerians (56.4% males) of mean age 21.8 ± 2.2 years were studied. Anxiety was assessed using the Beck's Anxiety Index (BAI), while obesity was determined using the bioelectrical impedance analysis (BIA) and body mass index (BMI) methods. Standard protocols were followed for all assessments and measurements. Appropriate descriptive statistics were carried out, while regression and correlation analyses (for continuous variables) and the Chi square tests (for categorical variables) were used to assess the relationship between anxiety and obesity.
Results:
The degree of adiposity of the subjects (males and females alike) classified by %BF standards did not significantly (P > 0.05) affect the proportion of the population with any degree of anxiety. The proportion of population with high anxiety (for both sexes) was similar (P > 0.05) irrespective of their BMI status. All the obese (BMI-wise only) males had low anxiety, while the proportion of thin females (in the low anxiety group) was significantly (P < 0.05) higher than that of their normal weight counterparts. There was neither a significant correlation nor a significant association (P > 0.05) between the BAI scores and the studied measures of adiposity in both male and female subjects.
Conclusion:
The low prevalence of both anxiety and obesity in the studied population may explain the observed lack of association between the studied variables. These findings do not support the “jolly fat” hypothesis.
Keywords: Adiposity, anxiety, association, obesity, young-adult Nigerians
Introduction
Anxiety and obesity are both public health challenges, affecting millions of people of all ages and cultures, though to varying degrees. Whereas anxiety is reported more in developed countries, where it is the most prevalent mental disorder, obesity is one of the most prevalent global public health disorders.[1] The rising trend in the prevalence of obesity globally has been attributed to genetics and lifestyle changes (often arising from urbanization) that encourage the accumulation of excess calories.[2] Impaired mental health has also been reportedly linked to obesity.[3] Some studies have supported the jolly fat hypothesis, where there is a positive association between anxiety and obesity.[4,5,6] However, others have reported no clear association between mental disorders and obesity.[7,8]
Reports on the relationship between mental health and obesity are rarely available in Africa. The bulk of what is known about the relationship between the two are from North America, Asia, and Europe.[9] Even in these populations, literature on the impact of race on the relationship between obesity and mental health is sparse. The few that are available are conflicting.[3] In Nigeria, anxiety affects as much as 21.8% of the population,[10] while 8.8-21.0% of the adult population is obese.[11,12] Apparently, the prevalence of obesity in Nigeria has been increasing steadily owing to changes in lifestyle mentioned above. It has been suggested that the health implications of excess weight is more due to the excess fat and not necessarily excess weight.[13] This may be responsible for the different obesity phenotypes reported in different populations, including Nigeria.[14] Implicit in this is a need for a more rigorous assessment of body fat, rather than relying solely on body mass index (BMI) in studies assessing the relationship between obesity and other health outcomes.
Given the high prevalence of anxiety in Nigeria, and the rising prevalence of obesity in the population, coupled with the dearth of information on the association between anxiety and obesity in Nigeria, it has become important to study the said relationship as the findings could inform prevention and treatment for both disorders. In view of the shortcomings of BMI as an index of adiposity, it is important to also use other measures of adiposity in the study of the said relationship. This study assesses that relationship, and examines the jolly fat hypothesis in young adult Nigerians. It is hypothesized that due to cultural and economic differences between Nigeria and the global West, the relationship between anxiety and obesity in Nigeria would be different from that reported in the Western literature.
Subjects and Methods
Subjects
Undergraduate students of the Michael Okpara University of Agriculture, Umudike (mean age 21.8 ± 2.2 years) who were randomly recruited, participated in this cross-sectional study. Only subjects who: (1) gave an informed verbal consent, (2) had no overt sign of ill-health nor reported present use of therapeutic medication, (3) reported no present use of any ‘drugs’ or ‘substance’, were allowed to participate in the study. Pregnant women were also excluded. A total of 1584 subjects (56.4% males) were effectively recruited and studied. No honoraria were paid to participants.
Methods
Each subject's self-reported age at last birthday was recorded. Heights of the subjects were measured with the subject standing on bare feet, using an inelastic tape fastened to a vertical rod. Height measurements were taken to the nearest 0.1 cm. For weight measurements, an electronic scale was used, and measurements made to the nearest 0.1 kg. The subjects were required to be on bare feet and wearing light clothing before being weighed. BMI was calculated as Weight (Kg)/[Height (m)2].
Body fat % was measured with a BIA device (Omron BF-400, Omron Healthcare Europe BV, Hoofddorp, The Netherlands) following the manufacturer's instructions. The BAI device sends a very weak electrical current of 50 kHz and less than 500 μA through the subject's body (from the sole of the feet up to the entire body) and combines the electrical resistance with the distance of electricity conducted and the pre-entered particulars of the subjects (age, sex, weight, and height) to give the body fat percentage. The in-built formula used by the device was not disclosed by the manufacturer.
To assess the anxiety status of the participants, the beck anxiety inventory (BAI) was administered to them and they were required to conscientiously complete the questionnaire. The BAI is a short list describing 21 anxiety symptoms and requiring respondents to rate how each symptom bothered them in the past week. Its scale (for each symptom) ranges from 0 (not at all) to 3 (severely, I could barely stand it). The total minimum and maximum scores are 0 and 63, respectively. The BAI has a high internal consistency (Cronbachs α = 0.92) and a test-retest reliability over one week of 0.75.[15]
The study was designed in accordance with the Helsinki declaration as modified in Edinburgh, and was approved by Board of the Department of Biochemistry, Michael Okpara University of Agriculture, Umudike on July 14, 2011.
Definitions
BMI classifications of weight status were: (1) thin (BMI < 18.5); (2) normal (BMI ≥ 18.5 but ≤ 24.9); (3) overweight (BMI ≥ 25 but <30), and (4) obese (BMI ≥ 30).[16] For females, %body fat (BF) classifications of adiposity were: (1) low (%BF < 25.4); (2) normal (%BF ≥ 25.4 but ≤31.9); (3) overweight (%BF ≥ 32.0 but ≤37.0); and (4) obese (≥37.1). For males, %BF classifications were: (1) low (%BF <12.7); (2) normal (%BF ≥ 12.7 but ≤ 21.6); (3) overweight (%BF ≥ 21.7 but ≤28.2); and (4) obese (≥28.3). Values for black subjects were used.[17] Subjects with a BAI score of 0-21, 22-35, and ≥ 36 were described as having low, moderate, and high anxiety levels, respectively.[15]
Statistical analyses
Descriptive statistics were carried out on the data generated. Continuous data are reported as means ± standard deviations, while categorical data are presented as percentages. Differences between means were separated by one-way ANOVA for continuous variables and by Chi Square test for categorical variables. The correlation between BAI scores and measures of adiposity (BMI and %body fat values) were assessed using the Pearson's Product moment correlation coefficients, while the linear regression analysis was done to determine the association between both variables. The significant threshold for all analyses was fixed at P < 0.05. Data analyses was done using SPSS version 18.0 (SPSS Inc. Chicago, IL). The results are presented in Tables.
Results
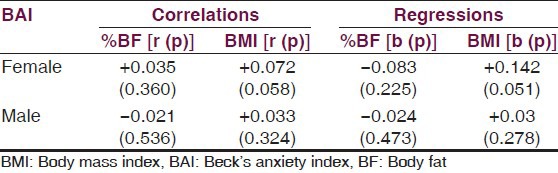
The mean %BF values of the subjects (males and females alike) were within the normal ranges for blacks. Mean %BF values for males were highest in the low anxiety group (20.2 ± 7.9%) and lowest in the high anxiety group (18.9 ± 7.4%). For the females, the values were highest in the high anxiety group (28.7 ± 4.8%), while the lowest was recorded in the low anxiety group (28.1 ± 6.3%). There were no statistically significant differences (P > 0.05) between the mean %BF values of subjects in the low anxiety category and those in the moderate or high anxiety categories, for both males and females. The mean BMI values of the subjects were also largely within the normal range. Males in the moderate anxiety group had the highest mean BMI for males (25.3 ± 8.5 kgm−2), while females in the high anxiety group had the highest mean BMI for the females (23.7 ± 2.6 kgm−2). Again, like the %BF data, there were no significant differences (P > 0.05) between the mean BMI values of the subjects with low anxiety (male and female) and their counterparts with moderate or high anxiety [Table 1]. From Table 2, it is seen that there was neither a significant correlation nor a significant association (P > 0.05) between the BAI scores and the studied measures of adiposity in both male and female subjects.
Table 1.
Distribution of body fat and BMI in the subjects based on their anxiety status
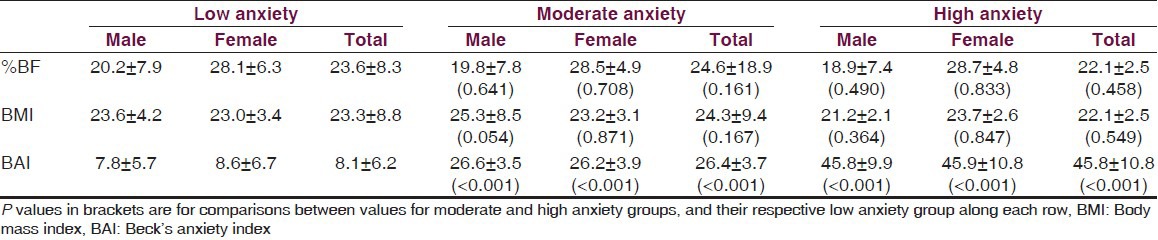
Table 2.
Correlations and regressions between BAI scores and measures of body composition in the studied population
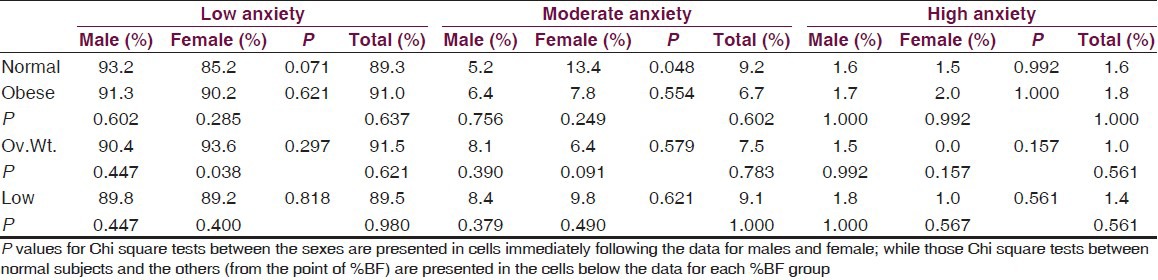
Approximately 90% of the subjects had low degree of anxiety (1.5% had high anxiety, while 8.7% had moderate anxiety). The degree of adiposity of the subjects (males and females alike) classified by %BF standards did not significantly (P > 0.05) affect the proportion of the population with low anxiety. The proportion of the population with moderate anxiety and high anxiety, each, did not vary significantly (P > 0.05) between the different adiposity groups. Females who had a normal %BF had a significantly (P < 0.05) higher proportion with moderate anxiety compared to their male counterparts [Table 3].
Table 3.
Proportions of the population with the different anxiety statuses, stratified by % body fatgroupings
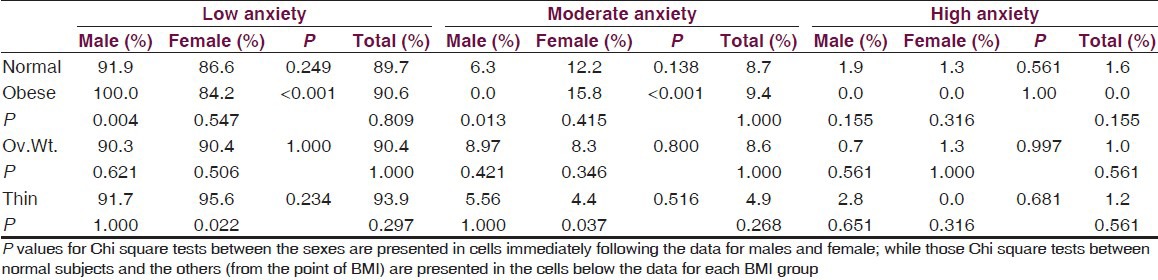
From the point of BMI classifications, the proportion of obese males who had low anxiety was significantly (P < 0.05) higher than that of their normal male counterparts. The proportion of population with low anxiety for the females was similar (P > 0.05) irrespective of their BMI status. The same trend was observed for moderate anxiety. Among subjects with high anxiety, there was no significant variation (P > 0.05) between the proportions of the population in the different BMI groups. None of the obese subjects had high anxiety while all of the obese male subjects had low anxiety [Table 4].
Table 4.
Proportions of the population with the different anxiety statuses, stratified by BMI groupings
Discussions
This study reports no correlations and/or associations between adiposity measured by BMI and %BF, and anxiety in this young-adult population in Nigeria. This is in contrast to some earlier reports,[4,5,6] but agrees with some other reports[7,8] in the literature. The studies that have reported an association between obesity and anxiety (or other mental health conditions) explain it by several mechanisms. Some studies have suggested that obese individuals (in cultures where obesity is stigmatized) may experience weight-related stigma and discrimination,[18] and that they often suffer from obstructive sleep apnea.[19] Obese individuals have also been reported to have disturbed neuroendocrine function and increased levels of circulating inflammatory cytokines.[20,21] Again, obese subjects lead sedentary lives,[22] which worsens the obesity. These factors, individually or collectively, could affect psychological well-being negatively. The finding that increasing physical activity alleviates anxiety[23] possibly by blocking negative thoughts, distracting people from undue worries, increasing social contact, and changing the brain chemistry in a manner that ultimately improves mood[24] seems to support the relationship between anxiety and a sedentary lifestyle-induced obesity. It is also possible that the direction of causality might actually be the reverse; that is, common mental diseases cause weight gain.[5] For instance, it has been shown that increased food intake is seen in subjects with anxiety,[9] thereby leading to obesity in such individuals.
In Nigeria, however, cultural belief systems that make obesity admirable are still prevalent, but are preponderant mostly in rural areas. In educated environments, due to an awareness of the negative health consequences of obesity, people “watch their weights”. Yet even in such environments, to be plump is often associated with wealth and sound mental health. It is usually such that the individual strives not to be slim or obese, but would prefer mild obesity to thinness.
Given that we studied an undergraduate population, it is unlikely that the lack of association or correlation between anxiety and obesity found in this study is due to cultural practices that accept or stigmatize obesity. The prevalence of anxiety reported here is a lot lower than that reported earlier in Nigeria.[10] We had very recently reported the prevalence of obesity in this population to be (by BMI standards and by %BF standards) 1.3% and 8.9%, respectively, while the prevalence of overweight (by the same standards) was 19.4% and 19.5%, respectively.[25] The prevalence of obesity in this population is clearly one of the smallest in the literature for Nigeria. It is therefore more plausible that the low prevalence of both obesity and anxiety in this population is responsible for the observed lack of significant correlation and association between obesity and anxiety. These low prevalence values may be explained by the active lifestyle that undergraduate work in Nigeria requires. Furthermore, due to wide-spread poverty, many undergraduates cannot afford to consume more than their daily energy requirement, despite their gregariousness. Again, the association between common mental disorders and obesity is reported to be stronger at older ages.[26] Since we studied a young-adult population, it is also plausible that their youthfulness may have masked the association. Youths generally post better health indices than older adults.
The finding that none of the obese subjects (by BMI standards) had high anxiety is nonetheless, noteworthy. It apparently (albeit deceptively) supports the jolly fat hypothesis. However, the absence of any significant correlation or association between anxiety and any of the two measures of obesity dispels such an insinuation. Furthermore, the small sample size of the obese subjects may be responsible for observation that none of the obese subjects had high anxiety. This position is further strengthened by the fact that some of the obese subjects (by %BF standards) had moderate to high degrees of anxiety; and the prevalence of anxiety (moderate or high) was statistically similar between the obese subjects, irrespective of sex, and their normal %BF counterparts.
This study showed that the prevalence of anxiety was similar between the sexes, contrary to findings of a male-dominated prevalence of anxiety reported recently in Nigeria[10] or the reports that obese women are more vulnerable than obese men to the development of psychiatric and psychological disorders.[6] Generally, women are more likely to worry about their physique than men in enlightened communities. However, men in Nigeria bear more of the burden of providing for the family and career progression. This could affect their psychological health negatively. Given the age-range of the subjects in this study, especially given cultural practices in Nigeria that ensure that parents pay the bills of their children often beyond graduation from universities, and the active social life lived by young-adults, the similarity in the prevalence of anxiety between the sexes, in this study is understandable.
Limitations of the current study include the reliance on questionnaires, rather than clinical interviews, for assessment of anxiety. The induction period for the development of obesity is quite long, therefore, chronic or recurrent anxiety is a more probable cause than transient anxiety which we measured. Conversely, severe obesity may be required for anxiety to manifest, so the absence of morbidly obese individuals in the cohort may be a limitation. This cohort of undergraduate students may not represent that age bracket in the general population, and necessarily limits the generalisability of these findings. The cross-sectional nature of this study also limits any attempt at inferring causality. Furthermore, the degree to which the results from the BAI that we used (and the deductions thereof) is transferable to individuals who meet the ICD – 10[27] classification is debatable. Moreover, apart from the absence of validation studies for the BAI in our clime, cross-cultural challenges in measuring mental health are known.[28] It is therefore possible that the participants had cultural encumbrances, leading to possible random and systematic misclassifications of mental health. The recruitment of undergraduates who are unarguably literate, coupled with the brevity, simplicity and ability of BAI to measure general anxiety, and its extensive use in that regard,[29] however, attenuate this problem.
The strength of this study lies in (among others) its novelty. This is the first report, to my knowledge, of an investigation into the relationship between anxiety and obesity in young-adult Nigerians. The direct measurements of the heights and weights of the participants and the measurement of their %BF (to avoid reliance on BMI alone) are also strengths. It is hoped that other workers would investigate this relationship further as the findings would guide the understanding of these debilitating illnesses and aid clinical practice.
Conclusion
The relationship between anxiety determined by the BAI, and obesity determined by BMI and BIA was studied in a population of undergraduates in Nigeria. Contrary to reports of a positive or negative association between both factors in some earlier studies, this study found no significant association or correlation between the studied variables. The low prevalence of both anxiety and obesity in the studied population may explain the findings. It appears the jolly fat hypothesis is not applicable to the studied population. The deliberate attempt to grow fat (obese), thinking that it could lead to an improvement in mental health should be discouraged at both the individual and population levels, especially as the adverse health implications of obesity and its sequelae are known to be enormous.
Acknowledgments
I appreciate and acknowledge the field contributions of Ijewereme-Pius Aireku and Attah Peace C.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Lykouras L, Michopoulos J. Anxiety disorders and obesity. Psychiatrike. 2011;22:307–13. [PubMed] [Google Scholar]
- 2.Zhang ZY, Wang MW. Obesity, a health burden of global nature. Acta Pharmacol Sin. 2012;33:145–7. doi: 10.1038/aps.2011.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hillman JB, Dorn LD, Huang B. Association of anxiety and depressive symptoms and adiposity among adolescent females using dual energy X-ray absorptiometry. Clin Pediatr (Phila) 2010;49:671–7. doi: 10.1177/0009922810363155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crisp AH, McGuiness B. Jolly fat: Relation between obesity and psychoneurosis in general population. BMJ. 1976;1:7–9. doi: 10.1136/bmj.1.6000.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kivimaki M, Lawlor DA, Singh-Manoux A, Batty GD, Ferrie JE, Shipley MJ, et al. Common mental disorder and obesity: Insight from four repeat measures over 19 years: Prospective Whitehall II cohort study. BMJ. 2009;339:b3765. doi: 10.1136/bmj.b3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barry D, Pietrzak RH, Petry NM. Gender differences in associations between body mass index and DSM-IV mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Ann Epidemiol. 2008;18:458–66. doi: 10.1016/j.annepidem.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamertz CM, Jacobi C, Yassouridis A, Arnold K, Henkel AW. Are obese adolescents and young adults at higher risk for mental disorders? A community survey. Obes Res. 2002;10:1152–60. doi: 10.1038/oby.2002.156. [DOI] [PubMed] [Google Scholar]
- 8.Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, et al. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117:1203–9. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sunwoo YK, Bae JN, Hahm BJ, Lee DW, Park JI, Cho SJ, et al. Relationships of mental disorders and weight status in the Korean adult population. J Korean Med Sci. 2011;26:108–15. doi: 10.3346/jkms.2011.26.1.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amoran O, Ogunsemi O, Lasebikan V. Assessment of mental disorders using the patient health questionnaire as a general screening tool in western Nigeria: A community-based study. J Neurosci Rural Pract. 2012;3:6–11. doi: 10.4103/0976-3147.91922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olatunbosun ST, Kaufman JS, Bella AF. Prevalence of overweight and obesity in urban adult Nigerians. Obes Rev. 2011;12:233–41. doi: 10.1111/j.1467-789X.2010.00801.x. [DOI] [PubMed] [Google Scholar]
- 12.Wahab KW, Sani MU, Yusuf BO, Gbadamosi M, Gbadamosi A, Yandutse I. Prevalence and determinants of obesity: A cross-sectional study of an adult Northern Nigerian population. Int Arch Med. 2011;4:10. doi: 10.1186/1755-7682-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ejike CE. Lipid accumulation product and waist-to-height ratio are predictors of the metabolic syndrome in a Nigerian male geriatric population. J Rural Trop Public Health. 2011;10:101–5. [Google Scholar]
- 14.Ijeh II, Okorie U, Ejike CE. Obesity, metabolic syndrome and BMI-metabolic-risk sub-phenotypes: A study of an adult Nigerian population. J Med Med Sci. 2010;1:254–60. [Google Scholar]
- 15.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol. 1988;56:893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO) Report of a WHO consultation Technical Report Series No 894. Geneva: WHO; 2000. Obesity: Preventing and managing the global epidemic. [PubMed] [Google Scholar]
- 17.Zhu S, Wang Z, Shen W, Heymsfield SB, Heshka S. Percentage body fat ranges associated with metabolic syndrome risk: Results based on the third National Health and Nutrition Examination Survey (1988-1994) Am J Clin Nutr. 2003;78:228–35. doi: 10.1093/ajcn/78.2.228. [DOI] [PubMed] [Google Scholar]
- 18.Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995-1996 through 2004-2006. Obesity (Silver Spring) 2008;16:1129–34. doi: 10.1038/oby.2008.35. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz DJ, Karatinos G. For individuals with obstructive sleep apnea, institution of CPAP therapy is associated with an amelioration of symptoms of depression which is sustained long term. J Clin Sleep Med. 2007;3:631–5. [PMC free article] [PubMed] [Google Scholar]
- 20.Kumari M, Chandola T, Brunner E, Kivimaki M. A nonlinear relationship of generalized and central obesity with diurnal cortisol secretion in the Whitehall II study. J Clin Endocrinol Metab. 2010;95:4415–23. doi: 10.1210/jc.2009-2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosom Med. 2009;71:171–86. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- 22.Rimer J, Dwan K, Lawlor DA, Greig CA, McMurdo M, Morley W, Mead GE. Exercise for depression. Cochrane Database Syst Rev. 2012;(Issue 7) doi: 10.1002/14651858.CD004366.pub5. Art. No.: CD004366. [DOI] [PubMed] [Google Scholar]
- 23.Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: Efficacy and dose response. Am J Prev Med. 2005;28:1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Jorm AF, Christensen H, Griffiths KM, Rodgers B. Effectiveness of complementary and self-help treatments for depression. Med J Aust. 2002;176:S84–96. doi: 10.5694/j.1326-5377.2002.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 25.Ejike CE, Ijeh II. Obesity in young-adult Nigerians: Variations in prevalence determined by anthropometry and by bioelectrical impedance analysis, and the development of %body fat prediction equations. Int Arch Med. 2012;5:22. doi: 10.1186/1755-7682-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kivimäki M, Batty DG, Singh-Manoux A, Nabi H, Sabia S, Tabak AG, et al. Association between common mental disorder and obesity over the adult life course. Br J Psychiatry. 2009;195:149–55. doi: 10.1192/bjp.bp.108.057299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Geneva: WHO; 1992. World Health Organization. The ICD–10 Classification of Mental and Behavioural Disorders: Clinical descriptions and diagnostic guidelines. [Google Scholar]
- 28.Smit J, van den Berg CE, Bekker LG, Seedat S, Stein D. Translation and cross-cultural adaptation of a mental health battery in an African setting. Afr Health Sci. 2006;6:215–22. doi: 10.5555/afhs.2006.6.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muntingh AD, van der Feltz-Cornelis CM, van Marwijk HW, Spinhoven P, Penninx BW, van Balkom AJ. Is the Beck Anxiety Inventory a good tool to assess the severity of anxiety? A primary care study in the Netherlands Study of Depression and Anxiety (NESDA) BMC Fam Pract. 2011;12:66. doi: 10.1186/1471-2296-12-66. [DOI] [PMC free article] [PubMed] [Google Scholar]


