Sir,
Acinetobacter baumannii (AB) is being increasingly recognized as an important cause of multi-drug-resistant nosocomial infections.[1] In neurosurgical literature it has been associated with secondary intracranial infections (post-traumatic/post-surgical meningitis and abscess formation).[2,3,4,5] Recently, AB has been implicated in necrotizing soft-tissue infections.[6,7,8] A similar type of fulminant wound infection after craniotomy has not been described. We report an unusual case where we had a combination of such wound infection with meningitis and pneumocephalus.
A 45-year-old male presented with a one-month history of progressively increasing left-sided focal motor seizures and features of raised intracranial pressure. He had undergone surgery and radiotherapy for a right frontotemporal astrocytoma (Grade 2) three years back. The magnetic resonance imaging (MRI) brain revealed a right frontal enhancing mass [Figure 1]. He reported high-grade intermittent fever with chills since a week and at the time of admission had anemia, thrombocytopenia and pre-renal azotemia. The peripheral smear was positive for schizonts and merozoites of Plasmodium vivax. After appropriate antimalarial and supportive medical management he was operated eight days after his admission. On the sixth postoperative day he developed craniotomy flap swelling which in an hour's time had markedly progressed to involve the entire scalp. He also became confused and incoherent. A computed tomography (CT) scan revealed significant scalp edema with air pockets in the subcutaneous and subgaleal regions [Figures 2 and 3]. There were postoperative changes in the operated site and diffuse pneumocephalus which had not been present in the immediate postoperative scan obtained a few days earlier [Figure 2]. Suspecting a fulminant necrotizing wound infection with associated meningitis, broad-spectrum antibiotics were started empirically and emergency re-exploration of the wound was performed. At surgery there was soft-tissue edema with crepitus. No tissue necrosis or pus was encountered. The dura appeared intact. A thorough wound wash was given after collecting a swab. The swab grew Acinetobacter baumannii sensitive to colistin, netilmicin, tigecycline and ceftazidime, as well as methicillin-resistant Staphylococcus aureus and Escherichia coli. With appropriate antibiotics (colistin, vancomycin and imepenem) he improved neurologically over a period of two weeks and was discharged for further adjuvant therapy.
Figure 1.
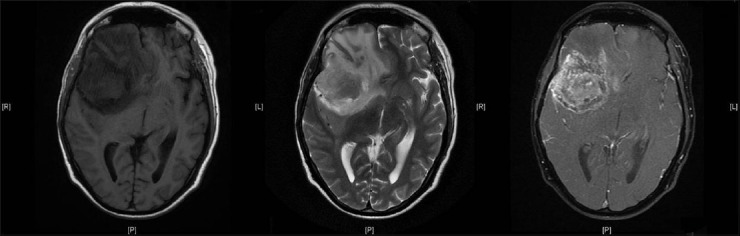
Preoperative magnetic resonance imaging (T1, T2 and post-contrast T1 images) showing a right frontal recurrent tumor
Figure 2.
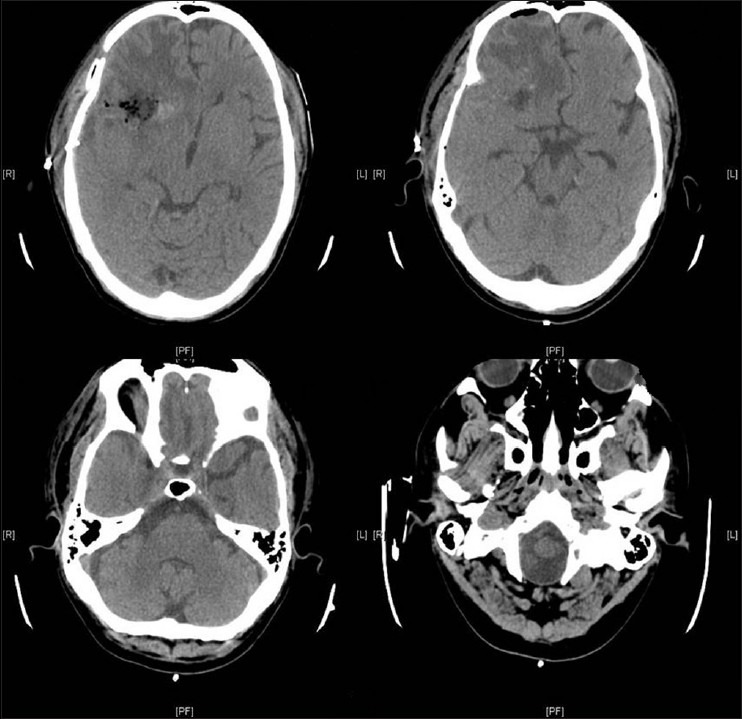
Immediate postoperative computed tomography scan showing only minimal air in the resection cavity
Figure 3.
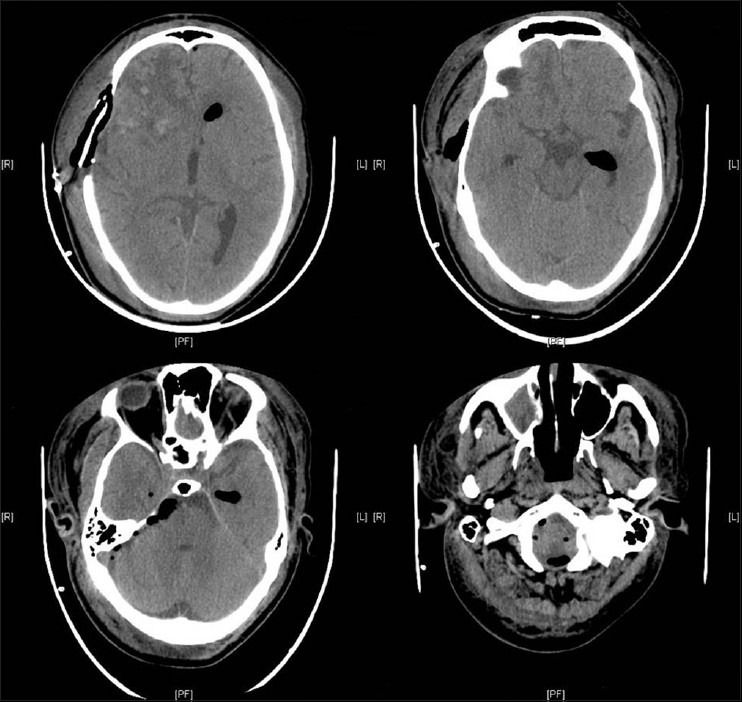
Subsequent computed tomography scan showing significant soft tissue and intracranial pneumocephalus
AB has been reported to cause necrotizing soft-tissue infections,[7] especially with war-related injuries.[8] The wound infection in our case mimicked a necrotizing soft-tissue infection which has not been earlier described in a postoperative setting. Pneumocephalus was also a very unusual occurrence. Though pneumocephalus can occur in the postoperative setting, an earlier scan (immediate postoperative scan a few days earlier) in the same patient did not show any pneumocephalus. Besides, there was no dural leak noted at resurgery (which could also have accounted for the pneumocephalus). Moreover, presence of air in the soft tissue as well as intracranial compartments supports our contention that it was a case of necrotizing wound infection with meningitis producing pneumocephalus caused by AB. Spontaneous pneumocephalus due to meningitis has been reported with gas-forming as well as non gas-forming organisms.[9,10] Though AB is not gas-forming, it still causes necrotizing soft-tissue infections, and hence can even cause pneumocephalus by similar pathogenic mechanisms. Following successful treatment of the infection and improvement in clinical features, this pneumocephalus also resolved, reinforcing the association of the infection by AB and the spectrum of clinico-radiological findings.
References
- 1.Peleg AY, Seifert H, Paterson DL. Acinetobacterbaumannii: Emergence of a successful pathogen. Clin Microbiol Rev. 2008;21:538–82. doi: 10.1128/CMR.00058-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim BN, Peleg AY, Lodise TP, Lipman J, Li J, Nation R, et al. Management of meningitis due to antibiotic-resistant Acinetobacter species. Lancet Infect Dis. 2009;9:245–55. doi: 10.1016/S1473-3099(09)70055-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krol V, Hamid NS, Cunha BA. Neurosurgically related nosocomial Acinetobacterbaumannii meningitis: Report of two cases and literature review. J Hosp Infect. 2009;71:176–80. doi: 10.1016/j.jhin.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 4.Erdem I, Hakan T, Ceran N, Metin F, Akcay SS, Kucukercan M, et al. Clinical features, laboratory data, management and the risk factors that affect the mortality in patients with postoperative meningitis. Neurol India. 2008;56:433–7. doi: 10.4103/0028-3886.44629. [DOI] [PubMed] [Google Scholar]
- 5.Moiyadi A, Shetty P. Abscess in a metastasis. J Neurosurg. 2010;112:474–5. doi: 10.3171/2009.6.JNS09829. [DOI] [PubMed] [Google Scholar]
- 6.Sebeny PJ, Riddle MS, Petersen K. Acinetobacterbaumannii skin and soft-tissue infection associated with war trauma. Clin Infect Dis. 2008;47:444–9. doi: 10.1086/590568. [DOI] [PubMed] [Google Scholar]
- 7.Urschel JD. Classic diseases revisited: Necrotizing soft tissue infections. Postgrad Med J. 1999;75:645–9. doi: 10.1136/pgmj.75.889.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guerrero DM, Perez F, Conger NG, Solomkin JS, Adams MD, Rather PN, et al. Acinetobacterbaumannii-associated skin and soft tissue infections: Recognizing a broadening spectrum of disease. Surg Infect (Larchmt) 2010;11:49–57. doi: 10.1089/sur.2009.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goyal M, Sharma R, Berry M. Diffuse pneumocephalus due to meningitis: CT findings. PediatrRadiol. 1996;26:278–9. doi: 10.1007/BF01372112. [DOI] [PubMed] [Google Scholar]
- 10.Jayaram S, Jadhav S, Rathod D, Tarvade S, Sornan A. Meningitis: An unusual cause of pneumocephalus. J Assoc Physicians India. 2004;52:67–8. [PubMed] [Google Scholar]


