Abstract
Background:
Psychological stress following natural disaster is common. Despite several earthquakes in India, data on evaluation of acute stress among the child victims in the early postdisaster period is scarce. Immediately following a devastating earthquake (6.9 Richter) at Sikkim on September, 18 2011, many children attended North Bengal Medical College, the nearest government tertiary care institution, with unusual stress symptoms.
Objective:
Evaluation of acute stress symptoms in children in the immediate postearthquake period.
Materials and Methods:
This was a cross-sectional study done over 4 weeks and includes all the children from 1 to 12 years presenting with unusual physical or behavioral symptoms. Those with major injuries requiring admission were excluded. They were divided into two age groups. For older children (8-12 years) the 8-item Children Impact of Event Scale (CIES) was used for screening of stress. Unusual symptoms were recorded in younger children (1-8 years) as CIES is not validated < 8 years.
Result:
A total of 84 children (2.66%) out of 3154 had stress symptoms. Maximum attendance was noted in first 3 days (65.47%) and declined gradually. In children ≥ 8 years, 48.78% had psychological stress, which was statistically significant on CIES scores without any gender predilection. Static posturing (41.86%), sleeplessness (32.55%), anorexia (9.30%), recurrent vomiting (13.95%), excessive crying (13.95%), or night-awakenings (4.65%) were found in younger children (n = 43) and three required admission.
Conclusion:
This study represent the first Indian data showing statistically significant psychological impact in older children (8-12 years) and various forms of physical stress symptoms in young children (1-8 years) following earthquake.
Keywords: Acute stress symptoms, disaster, earthquake, physical symptom, psychological impact
Introduction
On September, 18 2011, at 6.10 pm, a devastating earthquake struck Sikkim and the adjacent area in the West Bengal. The epicenter was in Mangan in North Sikkim. The quake had a magnitude of 6.9 on Richter scale and lasted for 40 seconds with several aftershocks. Immediately following the quake, children were brought to our Institute, North Bengal Medical College, which is the nearest tertiary care government institution. Several of those children were physically injured requiring urgent admission and in-patient care. Others who had no or minor injuries visited our department of pediatric medicine for some unusual physical and psychological symptoms.
Psychological impact is not uncommon following a devastating natural disaster. Loss of family members, structural demolition, or terrified response of the victims might produce emotional setbacks in the minds of children and adolescents. Several types of stress response either acute[1] or chronic,[2] in the form of posttraumatic stress disorders, depression, and anxiety symptoms are well reported in world literature.[3] However, data on psychological impact on children following earthquake from India are scarce.
Parents of the affected victims reported that stress symptoms appeared in their children soon after the quake. Some unnatural reactions were observed among the children already admitted in the hospital. This unusual phenomenon drew attention and prompted the researchers for detailed evaluation of these subtle symptoms out of psychological stress in the immediate postearthquake period.
Objective
Evaluation of acute stress symptoms in children in the immediate postearthquake period following the devastating Sikkim earthquake 2011.
Materials and Methods
This was a cross-sectional study over a period of 4 weeks from September, 19 to October, 18 2011 in our Institute North Bengal Medical college, Darjeeling, West Bengal. The Institution is the nearest tertiary care government institution, which is located in the catchment area of the earth quake, approximately 112 km away from the epicenter. Permission from the Institution Ethics Committee was obtained and the consent of the parents or accompanying person was taken after proper explanation.
The children were at first examined and screened by the personnel in the general emergency where ‘TRIAGE’ was done by the on duty doctors. The residents from department of pediatrics were there in the emergency TRIAGE team. Those with major injuries requiring life support or in-patient care were attended and admitted under care of department of Orthopedics and Neurosurgery. Those with no or minor injuries with a few symptoms were referred to the outpatient department (OPD) or emergency room (ER) of the pediatric medicine department. In addition, a considerable number of children with minor injuries and symptoms were directly brought by their parents to the OPD. All these children in the age group of 1-12 years who presented with new onset unusual and acute symptoms or behavioral changes, which might be related to the stressful effect of the earth quake, had been selected as study population. Those with major injuries were not included in our study because the psychological assessment is difficult in sick children and their stress symptoms might be over expressed by the pain and agony of physical trauma.
Clinical assessment and data collection was done collectively by the residents and medical officers in the predesigned proforma under strict supervision of the principal investigator. Analysis of the data was done by the principal investigator with the help of co-investigators. The children having stress symptoms were divided into two age groups: 1-8 years and 8-12 years [Figure 1]. The reason behind this age division is that we planned to apply the 8-item Children Impact of Event Scale (CIES), the effective shorter version of the 13-item scale was used for screening of the psychological stress,[4] which is validated and applicable only to the children 8 years and above. A Bengali version of the tool is used for better understanding of the questions by the children whose mother tongue was Bengali.[4] The CIES-8 consists of a total of eight questions in relation to intrusion (four items) and avoidance symptoms (four items). Children were to mention the frequency of symptoms that they had experienced during the past week (not at all = 0, rarely = 1, sometimes = 2, and often = 3).[5] A total score including the sub scores in the intrusion and avoidance-related questions for each of the child in this age group were analyzed. For meticulous screening and evaluation, consultation with personnel from department of psychiatry was sought. For rest of the children aged between 1 and 8 years, the physical symptoms and signs were recorded as there is no such validated scale for evaluation of stress symptoms [Figure 1].
Figure 1.
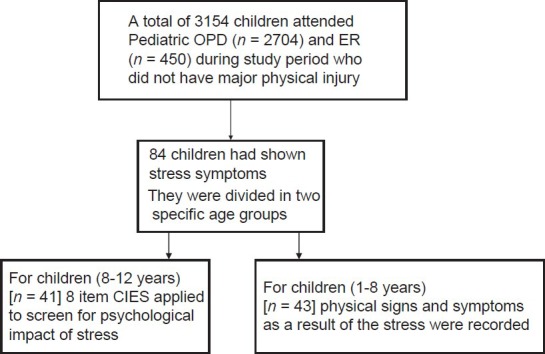
Schematic representation of the study design
Statistical method
Key proportions have been expressed with their 95% confidence interval (CI) assuming a binomial distribution. Fisher's exact test was employed to compare categorical variables between groups (<8 years). Medcalc version 11.6.0 (Mariakerke, Belgium; 2011) and Statistica version 6 (Tulsa, Oklahoma: StatSoft Inc., 2001) software was employed for statistical analysis.
The flow diagram of the study is schematized [Figure 1].
Result
After exclusion of the children with major injuries, a total of 3154 children had attended our department (OPD: 2704, ER: 450) over 4 weeks. Out of those, 84 children (2.66%) had stress symptoms [Figure 1]. The attendance of the children was higher in the initial few days and declined gradually over the next 3 weeks [Figure 2]. The attendance of such children was 23.80% (n = 20), 28.57% (n = 24), and 13.09% (n = 11), respectively in first 3 days. Altogether 65.47% (n = 55) of patients presented with their symptom in first 3 days.
Figure 2.
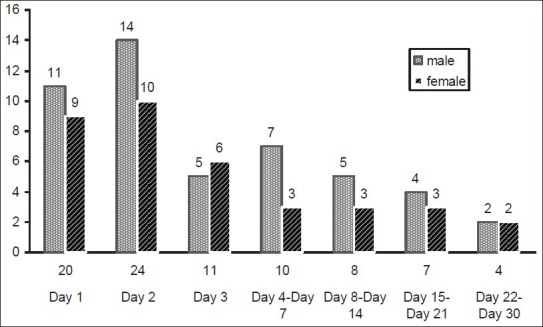
Day and week wise declining trend of attendance of children with respect to number of children in different genders (total n=84 in 30 days period)
Forty-one children aged above 8 years, (19 boys, 22 girls) had symptoms like palpitations (1 boy, 2 girls), dryness of mouth, and excessive water drinking (3 boys, 2 girls). On application of 8-item CIES, 20 out of 41 children (48.78%; 95% CI 26.38-56.54%) scored at least 17, which is considered to be the cut off value for the diagnosis of stress-induced psychological disorder. Rest of them (21) scored between 8 and 17 and none scored below 8 in the scale. No gender differences were observed in the frequency of physical symptoms, that is, static posturing (P = 0.329), sleeplessness (P = 1.000), anorexia (P = 1.000). The total CIES score in terms of avoidance and intrusion sub scores were normally distributed. They were compared between groups by Student's independent samples t-test where, P < 0.05 was considered statistically significant. Similarly no gender differences were observed in CIES scores.
Forty-three children, aged below 8 years (29 boys, 14 girls), collectively had symptoms like static posturing and clinging to caregiver (n = 18, 41.86%), sleeplessness (n = 14, 32.55%), anorexia (n = 4, 9.30%), recurrent vomiting (n = 6, 13.95%), excessive crying (n = 6, 13.95%) or nightmares (n = 2, 4.65%) [Figure 3]. Three children in the younger age group (6.97%, 95% CI 0.61-13.66%) needed hospital admission, for pseudo seizure (n = 2, 4.65%) and secondary enuresis (n = 1, 2.32%). They were admitted for detailed investigation and appropriate management. The study revealed that stress-related physical symptoms were clustered around a specific age group [Figure 3]. Static posturing and excessive cry were more common in toddlers (1-3 year), whereas anorexia, nightmares, pseudo seizures, and secondary enuresis were noted relatively older children (3-8 years).
Figure 3.
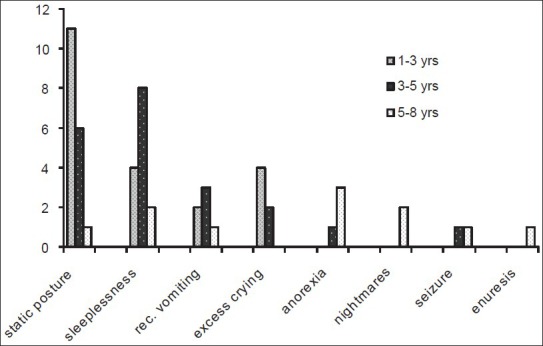
Distribution of physical symptoms in different age groups (1-8) years
Discussion
Children who experience a traumatic event are at risk of developing stress disorder.[6,7] Such events may be natural disasters like earthquake, flood, tsunami, cyclone, or manmade-trauma like terrorist attack, road traffic accidents, etc., Parents often fail to perceive the psychological impact of the disaster on their children. Therefore direct questioning is required to assess the degree of psychological trauma.[8] The traumatic after-experiences may manifest in different ways depending on the age of the child. While the older children can verbalize and answer to the questions expressing their feelings, the younger children may not be able to do so. They might response in their own way with some subtle and unusual physical symptoms. The responses are difficult to interpret and standardize. Variation in response in relation to different developmental stages in the younger children is reported earlier.[9]
Several investigational tools like trauma screening questionnaire,[10] depression self-rating scale, and child posttraumatic stress disorder reaction index[11] are being developed to assess the extent of psychological stress. Most research to date has focused on the effectiveness of the Impact of Events Scale (IES).[12] The modified version of IES is Children's Revised Impact of Event Scale, which has got 8- and 13-item versions. This has been well validated in posttraumatic cases with a high predictive value.[13] The 8-item CIES, the commonly used shorter version, is useful in children aged 8 years and older.[5] Stallard et al., found that a cutoff score of 17 on the 8-item IES correctly identified 69.2% of children with stress disorder.[14] It has a sensitivity of 100% and specificity of 71%.[13] Applying 8-item CIES scale on the children aged 8 years and above in our study, 20 children (9 male, 11 female) (41.46%; 95% CI 26.38-56.54%) scored at least 17. Our study demonstrated a significant psychological impact (P < 0.05) on this age group. Although two earlier studies reported female gender predilection for stress-related psychological impact,[2] we did not find statistically significant gender difference.
Acute stress-induced physical symptoms were notable in children aged below 8 years, for whom CIES is not applicable. Static posture and clinging to care giver was seen most commonly (41.86%). Other symptoms in the form of sleeplessness, anorexia, recurrent vomiting, excessive crying, or nightmares were recorded. Three children in the younger age group needed hospital admission, which emphasizes the seriousness of the impact. Some of the stress-related symptoms were age specific, like static posturing and excessive crying were more common in 1- to 3-year age group, whereas anorexia, nightmares, pseudo seizures, and secondary enuresis were seen in 5- to 8-years age group [Figure 3]. Similar age variation in stress symptoms was reported after the Marmara earth quake in Turkey in 1999, where younger children developed adjustment disorder while older ones had posttraumatic acute stress disorder.[15]
Most disaster-related studies done previously evaluated the long-term psychological impact on the victims rather than their early symptoms.[16,17] Older children and adolescents, like most adults, can remember and communicate the incidences long after the disaster. The recovery might delay and take several months in elderly victims.[16,17] On the contrary, stress-related symptoms are transient in younger children.[18] These signs and symptoms could be picked up only if the assessments are done immediately after the disaster. Such stress symptoms might wane off and less discernible later as evidenced by the gradual decline in the number of attendees in the later weeks [Figure 2]. Similar high incidence of acute stress reaction (ASR) in the early postdisaster period was reported by Soltados et al.[19]
Studies that evaluated the impact of a natural disaster on Indian children are scarce. Two studies, one after Kashmir earthquake and another after Bhuj earthquake, reported physical injuries and surgical emergencies in children.[20,21] Two other studies attempted to assess the psychological impact following earth quake but the age group was above 14 years.[22,23] Another study on children and adolescents (aged ≤ 18 years) done after natural disaster, Tsunami in Andaman and Nicobar islands, during the first 3 months revealed considerable psychiatric morbidity.[24]
The children with stress symptoms were referred for further evaluation for psychiatric illness for better outcome. Community-based cognitive-behavioral and group interventions, group discussions, or play therapy may be effective measures.[24] Better management of a natural disaster can minimize the impact among them. ‘Save the children’ has extended a remarkable contribution in the disaster management through child-centered and community-based approaches in the emergency situations.[25]
The strength of this study is the child population who are comparatively younger to earlier researches. Moreover, detection of the stress symptoms in the early postdisaster period in children is yet unexplored.
There are a few limitation of the study. Those children who attended the hospital had been evaluated and a considerable number of patients still remain there in the community, we assume. Hence, study population is not representative of the total magnitude of the affected children. The children who sustained major physical injuries were also victim of severe psychological trauma, which is operationally difficult to assess in the early weeks.
The present study, first of its kind, on Indian children after an earth quake envisages a future direction for the fellow investigators. Further community-based large studies on acute stress in younger children, needs to be carried out in different parts of the country.
Conclusion
Present study, first of its kind from India, carried out exclusively on child victims of earthquake had shown various forms of stress-related physical symptoms in young children (1-8 years), which varied according to their age. Older children (8-12 years) had demonstrated a statistically significant psychological impact out of stress following natural disaster.
Acknowledgement
The authors thankfully acknowledge the help rendered by all the physicians and staff of the department of Pediatrics, Principal, and Medical Superintendent of North Bengal Medical College, Darjeeling, West Bengal.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Roussos A, Goenjian AK, Steinberg AM, Sotiropoulou C, Kakaki M, Kabakos C, et al. Posttraumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia, Greece. Am J Psychiatry. 2005;162:530–7. doi: 10.1176/appi.ajp.162.3.530. [DOI] [PubMed] [Google Scholar]
- 2.Pynoos RS, Goenjian A, Tashjian M, Karakashian M, Manjikian R, Manoukian G, et al. Post-traumatic stress reactions in children after the 1988 Armenian earthquake. Br J Psychiatry. 1993;163:239–47. doi: 10.1192/bjp.163.2.239. [DOI] [PubMed] [Google Scholar]
- 3.Groome D, Soureti A. Post-traumatic stress disorder and anxiety symptoms in children exposed to the 1999 Greek earthquake. Br J Psychol. 2004;95:387–397. doi: 10.1348/0007126041528149. [DOI] [PubMed] [Google Scholar]
- 4. [Last accessed on 2011 Sep 19]. http://www.childrenandwar.org/measures/children-revised-impact-of-event-scale-8 .
- 5.Dyregrov A, Kuterovac G, Barath A. Factor analysis of the impact of event scale with children in war. Scand J Psychol. 1996;37:339–50. doi: 10.1111/j.1467-9450.1996.tb00667.x. [DOI] [PubMed] [Google Scholar]
- 6.Kenardy JA, Spence SH, Macleod AC. Screening for posttraumatic stress disorder in children after accidental injury. Pediatrics. 2006;118:1002–9. doi: 10.1542/peds.2006-0406. [DOI] [PubMed] [Google Scholar]
- 7.Asarnow J, Glynn S, Pynoos RS, Nahum J, Guthrie D, Cantwell DP, et al. When the earth stops shaking: Earthquake sequelae among children diagnosed for pre-earthquake psychopathology. J Am Acad Child Adolesc Psychiatry. 1999;38:1016–23. doi: 10.1097/00004583-199908000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Shioyama A, Uemoto M, Shinfuku N, Ide H, Seki W, Mori S, et al. The mental health of school children after the Great Hanshin-Awaji Earthquake: II. Longitudinal analysis. Seishin Shinkeigaku Zasshi. 2000;102:481–97. [PubMed] [Google Scholar]
- 9.McDermott BM, Palmer LJ. Postdisaster emotional distress, depression and event related variables: Findings across child and adolescent developmental stages. Australian N Z Psychiatry. 2002;36:754–76. doi: 10.1046/j.1440-1614.2002.01090.x. [DOI] [PubMed] [Google Scholar]
- 10.Brewin CR, Rose S, Andrews B, Green J, Tata P, McEvedy C, et al. Brief screening instrument for post-traumatic stress disorder. Br J Psychiatry. 2002;181:158–62. doi: 10.1017/s0007125000161896. [DOI] [PubMed] [Google Scholar]
- 11.Goenjian AK, Walling D, Steinberg AM, Roussos A, Goenjian HA, Pynoos RS. Depression and PTSD symptoms among bereaved adolescents 6 (1/2) years after the 1988 Spitak earthquake. J Affect Disord. 2009;112:81–4. doi: 10.1016/j.jad.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 12.Horowitz MJ, Wilner N, Alvarez W. Impact of event scale: A measure of subjective stress. Psychosom Med. 1979;41:209–18. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Perrin S, Meiser-Stedman R, Smith P. The children's revised impact of event scale (CRIES): Validity as a screening instrument for PTSD. Behav Cognit Psychother. 2005;33:487–498. [Google Scholar]
- 14.Stallard P, Velleman R, Baldwin S. Psychological screening of children for post-traumatic stress disorder. J Child Psychol Psychiatr. 1999;40:1075–82. [PubMed] [Google Scholar]
- 15.Demir T, Demir DE, Alkas L, Copur M, Dogangun B, Kayaalp L. Some clinical characteristics of children who survived the Marmara earthquakes. Eur Child Adolesc Psychiatry. 2010;19:125–33. doi: 10.1007/s00787-009-0048-1. [DOI] [PubMed] [Google Scholar]
- 16.Bulut S, Bulut S, Tayli A. The dose of exposure and prevalence rates of post traumatic stress disorder in a sample of Turkish children eleven months after the 1999 Marmara earthquakes. Sch Psychol Int. 2005;26:55–70. [Google Scholar]
- 17.Toyabe S, Shioiri T, Kuwabara H, Endoh T, Tanabe N, Someya T, et al. Impaired psychological recovery in the elderly after the Niigata-Chuetsu Earthquake in Japan: A population-based study. BMC Public Health. 2006;14(6):230. doi: 10.1186/1471-2458-6-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoare P. Essential Child Psychiatry. Edinburgh: Churchill Livingstone; 1993. Emotional disorders; pp. 111–31. [Google Scholar]
- 19.Soldatos CR, Paparrigopoulos TJ, Pappa DA, Christodoulou GN. Early post-traumatic stress disorder in relation to acute stress reaction: An ICD-10 study among help seekers following an earthquake. Psychiatry Res. 2006;143:245–53. doi: 10.1016/j.psychres.2005.05.018. [DOI] [PubMed] [Google Scholar]
- 20.Yatoto G, Syed A, Rangrez R, Singh D. Profile of patients admitted in a large teaching hospital as a result of earthquake in kashmir during october 2005. Int J Health Sci (Qassim) 2009;3:209–12. [PMC free article] [PubMed] [Google Scholar]
- 21.Jain V, Noponen R, Smith BM. Pediatric surgical emergencies in the setting of a natural disaster: Experiences from the 2001 earthquake in Gujarat, India. J Pediatr Surg. 2003;38:663–7. doi: 10.1016/jpsu.2003.50178. [DOI] [PubMed] [Google Scholar]
- 22.Sharan P, Chaudhary G, Kavathekar SA, Saxena S. Preliminary report of psychiatric disorders in survivors of a severe earthquake. Am J Psychiatry. 1996;153:556–8. doi: 10.1176/ajp.153.4.556. [DOI] [PubMed] [Google Scholar]
- 23.Chadda RK, Malhotra A, Kaw N, Singh J, Sethi H. Mental health problems following the 2005 earthquake in Kashmir: Findings of community-run clinics. Prehosp Disaster Med. 2007;22:541–5. doi: 10.1017/s1049023x00005409. [DOI] [PubMed] [Google Scholar]
- 24.Math SB, Tandon S, Girimaji SC, Benegal V, Kumar U, Hamza A, et al. Psychological impact of the tsunami on children and adolescents from the andaman and nicobar islands. Prim Care Companion J Clin Psychiatry. 2008;10:31–7. doi: 10.4088/pcc.v10n0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. [Last accessed on 2012 Nov 11]. http://www.savethechildren.in/what-we-do/disaster-risk-reduction-a-emergencies.html .


