Abstract
Background:
In resource-poor setting, identification of predictors of death is of paramount importance for clinicians, so that specific therapies and management strategies can be applied to patients at high risk of dying. This study aims to determine the factors associated with death and predictors of in-patient mortality for stroke among a cohort of stroke patients in two tertiary centers in Northwestern Nigeria.
Materials and Methods:
This was a prospective study of consecutive patients with acute stroke who were admitted to tertiary hospitals in northwestern Nigeria. A single observer, using pre-defined diagnostic criteria, recorded the information of interest including length of stay, outcome (dead or alive all through 30 days), time of death.
Result:
A total of 273 patients comprising 179 male and 94 female stroke patients were recruited. One hundred and seventy-four (63.7%) had infarctive stroke while 99 (36.3%) had hemorrhagic stroke (91 intracerebral and 8 sub-arachnoid hemorrhage). One-month mortality was 37%, and the majority was patients with hemorrhagic stroke (69.6%). About two-third (74.5%) of the mortalities occurred during the first week of the event. Logistic regression showed that severe systolic blood pressure, severe diastolic pressure, second or more episode of stroke, severe GCS, seizures, abnormal pupillary size, hemorrhagic stroke type, presence of aspiration pneumonitis, RBS > 200 mg/dl were independent predictors of mortality in stroke.
Conclusion:
The present study provides information on factors associated with death in stroke. GCS < 8, seizures, abnormal pupillary size, hemorrhagic stroke, aspiration pneumonitis were independent predictors of mortality.
Keywords: Mortality, Northwestern Nigeria, predictors, stroke
Introduction
Stroke is one of the leading causes of death not only in developed countries, but also worldwide.[1] The frequency of stroke in hospital populations in Nigeria varied from 0.9% to 4.0%.[2,3] Reports from various studies in Nigeria showed that stroke was the commonest cause of neurological admissions.[4,5,6] Studies predominantly from southern Nigeria showed that stroke was responsible for 5-17% of medical deaths.[5,6,7] In Kano, Northwestern Nigeria, stroke accounted for 77.6% of neurological admissions.[8] The clinical pattern of stroke in Kano had been shown to be similar to what obtains in other regions of the country and in other developing countries.[9,10,11] Owing to the amount of effort that has to be invested in the planning and provision of health care, stroke is an important public health problem, a burden to health care providers and to the society at large.
Consequently, in resource poor-setting, identification of predictors of death is of paramount importance for clinicians, so that specific therapies and management strategies can be applied to patients at high risk of dying. Nonetheless, these clinical predictors of outcome must be easy to use if they are to gain wide acceptance. Besides, little or no data is available on predictors of mortality following acute stroke in the region.
This study aims to determine the factors associated with death and predictors of in-patient mortality for stroke among a cohort of stroke patients in two tertiary centers in northwestern Nigeria.
Materials and Methods
In this prospective study, consecutive patients that were seen in emergency unit and admitted to the medical wards of the two tertiary hospitals; Aminu Kano Teaching Hospital (AKTH), Kano and Murtala Muhammad Specialist Hospital, (MMSH) Kano, from June 2007 to June 2010 were recruited for the study. Eligibility for the study was in accordance with the World Health Organization (WHO) definition of stroke as ‘a rapidly developing clinical signs of focal (or global) disturbance of cerebral function, with symptoms lasting 24 hours or longer or leading to death, with no apparent cause other than vascular origin.[12] All the patients enrolled were assessed by clinicians experienced in the subtlety of stroke diagnosis, typing, and management. Classification of stroke into hemorrhagic and infarctive stroke was based on computerized tomography of the brain (CT Brain) or magnetic resonance imaging (MRI). The World Health Organization stroke scale was also used in some patients who by reason of cost or otherwise could not do the test. The WHO criterion has a sensitivity of 73% for hemorrhage and 69% for infarction and an overall accuracy of 71% in Nigeria.[13,14]
Patients with ambiguous clinical and/or radiological diagnosis of stroke were excluded from the study. Each diagnosed patient was followed up for 30 days until either death at the hospital or discharge.
At presentation, patients and/or relatives were interviewed to obtain information pertaining to the onset of stroke and pre-existing risk factors, including hypertension, diabetes mellitus, hyperlipidemia, smoking, ischemic heart disease, atria fibrillation, and previous transient ischemic attacks.
A standardized data sheet was used to record the demographic variables including sex, age (If the exact age of the patient was not known, it was calculated by estimating their age at the time of significant events in Nigeria), previous stroke, seizure, blood pressure in recumbent position, pulse, temperature, respiratory rate and pattern, Glasgow Coma Scale (GCS), pupillary size, pupillary reaction, presence of aspiration pneumonitis, co-morbidities, length of stay, outcome (dead or alive all through 30 days), time of death, random blood sugar, lipid profile and were recorded.
During their hospital stay, patients received standard care. They were managed in the general medical wards due to lack of stroke unit in the facilities. The patients were treated in accordance with Aminu Kano Teaching Hospital guideline on stroke management, which is a modification of American Heart Association/American Stroke Association (AHA/ASA) guidelines.[15]
Analysis of data was carried out using the “Statistical Package for Social Sciences” (SPSS) program for Windows version 16.0 (SPSS Inc., Chicago, IL). Univariate analysis was carried out using Pearson Chi-square for categorical variables, scores on severity scale were compared using Chi-square for trend and Student's t test for continuous variables. P < 0.05 was used as a significant level. Then, a logistic multiple regression model was used, and the co-variates were adjusted for each independent (regression) variable to find independent predictors of in-hospital mortality. Variables included in the regression model were those that had a significant P value (P < 0.05) in the univariate analysis. Survival rate was calculated using the Kaplan-Meier method.
Results
During the three-year study period, a total of 273 patients comprising 179 male and 94 female (m:f = 2:1) stroke patients were recruited. Their age ranged from 18 to 90 with a mean age of 55 yrs (sd-16.5). The peak age was in the seventh decade. Ninety-nine (36.3%) patients had computerized tomography of the brain (CT Brain) while six (2.2%) had magnetic resonance imaging (MRI). One hundred and seventy-four (63.7%) had infarctive stroke while 99 (36.3%) had hemorrhagic stroke (91 intracerebral and 8 sub-arachnoid hemorrhage). Table 1 showed distribution of stroke type across sex and age group. Table 2 summarized the traditional risk factor for stroke.
Table 1.
Distribution stroke type and sex by age group
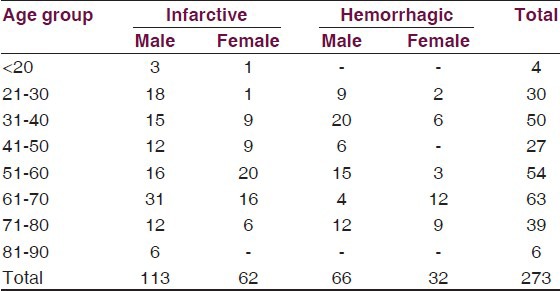
Table 2.
Traditional risk factorsa

One-month mortality was 37%, and the majority was patients with hemorrhagic stroke (69.6%). Figure 1 showed Kaplan-Meier survival curve for ischemic and hemorrhagic stroke. About two-third (74.5%) of the mortalities occurred during the first week of the event.
Figure 1.
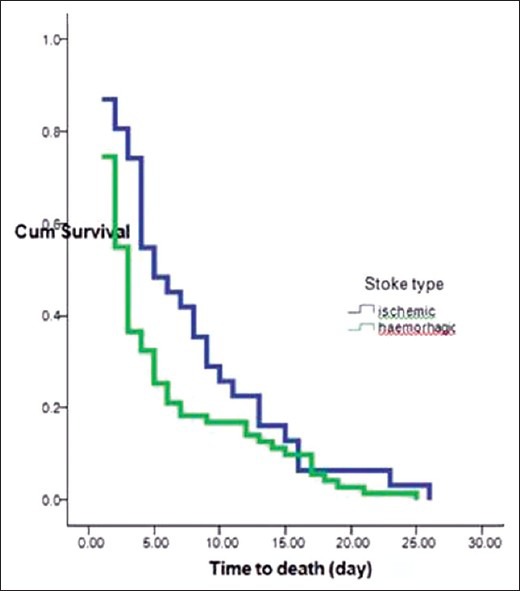
Survival curve for stroke patients with ischemic and hemorrhagic stroke
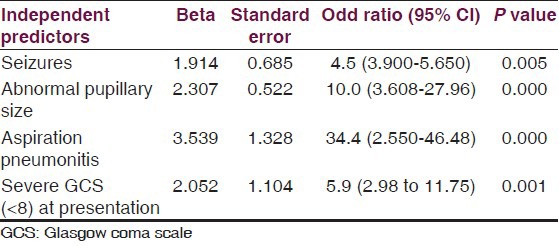
Result of univariate analysis was as displayed in Table 3. Subsequent multivariate analysis and logistic regression showed that GCS < 8, seizures, abnormal pupillary size, hemorrhagic stroke, and aspiration pneumonitis were independent predictors of mortality in stroke [Table 4].
Table 3.
Factors associated with in.hospital mortality at 1 month
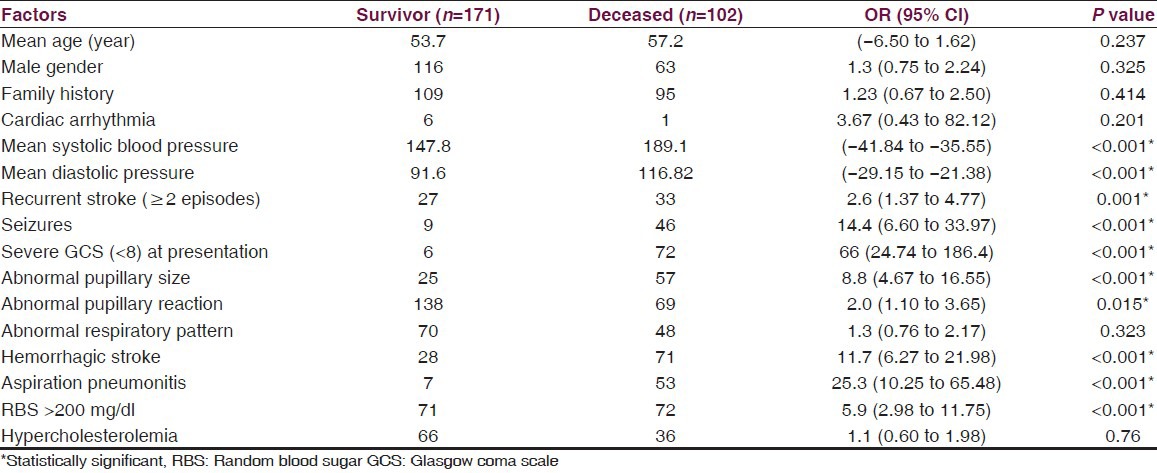
Table 4.
Result of multivariate logistic regression analysis for independent predictors of one month mortality
Discussion
Acknowledging the limitations of hospital-based study, we give account of our findings from the study of predictors of mortality in a two-center prospective study of 273 consecutive stroke patients seen in Kano, Northwestern Nigeria over a three-year period.
The male preponderance in this study is similar to the findings in other studies amongst Africans and non-African populations.[16,17,18,19,20,21] However, some Iranian studies had reported female preponderance.[22,23] The male preponderance in this study may be due to differences in certain risk factors such as smoking, which are more prevalent among men in Nigeria compared with women. The mean age of the patients in this study is similar to that reported by Bwala in northeastern Nigeria but lower than that reported in southwestern Nigeria.[2,17,24]
In the present study, hypertension appeared to be the single most important modifiable risk factor for both ischemic and hemorrhagic stroke followed by smoking, TIA, diabetes, hypercholesterolemia, and cardiac diseases. Studies conducted elsewhere in developing and developed countries showed similar results.[2,17,24,25,26,27] However, smoking was found to be the major stroke risk factor, followed by hypertension and hyperlipidemia in a study conducted by Bak et al. in Denmark.[28] Diabetes mellitus and ischemic heart disease were less important risk factors in their study.
Overall, one-month stroke mortality in this study was 37%. The one-month mortality rate was higher in patients with hemorrhagic stroke than ischemic stroke. This figure is comparable to what was reported in the other geopolitical zones of Nigeria.[4,17,24,29,30] However, the figure is higher than one mortality (20.3%) reported by Ong and Raymond.[31] The Ege Stroke Registry reported an overall 30-day mortality rate of 19.7%, also with a higher mortality rate in hemorrhagic (29%) compared to ischemic stroke (17%).[32] The 28-day case fatality rate for all strokes in the Perth Community Stroke Study was 24%[33] while the Oxfordshire Community Stroke Project[34] reported an overall 30-day case fatality rate of 19%. The care of patients with stroke within the limited health budgets of most African countries offers a major and increasing challenge, thus, the higher figure recorded in this study can be partly attributed to poverty, delayed presentation, lack of facilities, non-existent of stroke unit, and lack of intensive monitoring to mention but few. Nevertheless, this cohort is not likely to be entirely representative of all strokes occurring in the community as those with severe stroke such as primary intracranial hemorrhage causing early death are less likely to have reached the hospital.
In the current study, KM curve gave the impression that death occurs more frequently early than late in the first 30 days for both stroke types. Most of the deaths recorded in this study occurred in the first week of stroke. This finding is in agreement with studies conducted in developed countries. Stegmayr et al.[35] in their study found that patients in Eastern Europe compared to those from Western Europe had a higher 28-day fatality rate in both men and women. They reported 35.7% and 75.3% of the total mortality occurred during the first week of stroke onset in Eastern Europe and Western Europe, respectively. In a similar study in Singapore by Ong and Raymond, half of the total stroke deaths at one month occurred during the first week.[31] Bamford et al. attributed early death within the first seven days to direct effects of neurological damage, whereas deaths during 7-30 days were mainly from immobility.[34]
Hemorrhagic strokes were identified as one of the independent predictors of mortality in this study. This finding is consistent with the report of Ong and Raymond, Jover-Saenz et al.,[36] and Mbala et al.[37] reported similar findings. Early death within the first seven days could be attributed to direct effects of neurological damage. In other words, lower level of consciousness occasioned by raised intracranial pressure associated with hemorrhagic stroke compared to ischemic stroke may partly explain this finding.
High or increasing mean systolic pressure on admission was also associated with stroke mortality; however, the same degree of association was not apparent with diastolic blood pressure. This finding further gave credence to an earlier report by Simon et al. in the Manitoba study cohort of 3983 men; in the study, increasing magnitude of systolic blood pressure and its five-year changes were associated with worsening prognosis. In their study, the same association was less apparent for diastolic blood pressure and was not found for five-year change in diastolic pressure.[38] Pulse pressure has been reported to be a good predictor of stroke mortality in the elderly females, even superior to the label of hypertension. However, no such relationship was found between pulse pressure and mortality in males in a study conducted by Mazza et al.[39]
This study showed that hyperglycemia (RBS > 200 mg/dl) at presentation was associated with poor outcome in stroke; this result is similar to the report of Ong et al.[31] and Yang Wang et al., in which hyperglycemia without a history of diabetes was found to be associated with in-hospital mortality[40] but not a significant predictor of early stroke mortality; however, the study was conducted on ischemic stroke patients only.[31]
GCS < 8 that was found to independently predict mortality in stroke patients in this study has been previously reported by the other workers.[31,41] Some other studies reported GCS < 10 as an independent predictor of death from stroke.[42,43] In reality, unconsciousness was reported the most recognized prognostic determinant of death in acute stroke and is directly related to the severity of the neurological damage.[43,44,45,46,47]
Consistent with other hospital-based studies, aspiration pneumonia was identified as an independent predictor in this study. Dysphagia is an important complication of acute stroke. In an acute stage of the illness, dysphagia is found in up to 50% of stroke patients.[48,49,50] However, dysphagia resolves in most patients within a week to a month and persists in only a small number of subjects beyond six months.[48,49,50] Aspiration with the possible consequence of aspiration pneumonia is the most important acute complication of dysphagia, affecting up to one third of dysphagic patients.[48,51] Report from study elsewhere showed that stroke-associated pneumonia (SAP) accounted for 10% of stroke-related deaths,[52] and has been reported to increase mortality rate by three-fold[52,53] and prolong the hospital stay by two-fold.[53] Thus, adequate measures to forestall aspiration pneumonitis in stroke patients are worthwhile.
In our study, age, gender, presence of cardiac arrhythmia, and hypercholesterolemia, like in some other studies,[36,37,38,39,40,41,42,43,44,45,46] did not predict stroke mortality.
In resource-poor regions, accurate prediction of survival is important for the appropriate management of patients with stroke with major consequences for the organization of meager medical resources.
This study, however, has some limitations; it is hospital-based, not all the patients had neuro-imaging, thereby necessitating the use of WHO stroke score in those who did not have the investigations, potentially giving room for misclassification of stroke. However, the study, being the first of its kind in the region, provides a preliminary database to work with in reducing stroke mortality, which has decreased in recent decades in developed world,[20] but is still one of the most common causes of deaths in sub-Saharan Africa.[2,3,4,5,6,7,8,9,10]
Conclusion
Factors associated with one-month in-hospital mortality of stroke in two tertiary hospitals in Kano were similar to the reports from other studies in developing countries. Abnormal pupillary size, hemorrhagic stroke, aspiration pneumonitis, and GCS < 8 were independent predictors of mortality in stroke.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global burden of disease study. Lancet. 1997;349:1269–76. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 2.Ogun SA, Ojini FI, Ogungbo B, Kolapo KO, Danesi MA. Stroke in south west Nigeria: A 10-year review. Stroke. 2005;36:1120–2. doi: 10.1161/01.STR.0000166182.50840.31. [DOI] [PubMed] [Google Scholar]
- 3.Osuntokun BO, Bademosi O, Akinkugbe OO, Oyediran AB, Carlisle R. Incidence of stroke in an African City: Results from the Stroke Registry Ibadan, Nigeria, 1973-1975. Stroke. 1979;10:205–7. doi: 10.1161/01.str.10.2.205. [DOI] [PubMed] [Google Scholar]
- 4.Ogun SA. Acute stroke Mortality at Lagos University Teaching Hospital: A five year review. Nig Q J Hosp Med. 2000;10:8–10. [Google Scholar]
- 5.Ojini FI, Danesi MA. Pattern of neurological admissions at the Lagos University Teaching Hospital. Nig J Clin Pract. 2003;5:38–41. [Google Scholar]
- 6.Talabi OA. A 3-year review of neurologic admissions in University College Hospital Ibadan, Nigeria. West Afr J Med. 2003;22:150–1. doi: 10.4314/wajm.v22i2.27937. [DOI] [PubMed] [Google Scholar]
- 7.Ogun SA, Adelowo OO, Familoni OB, Jaiyesimi AE, Fakoya EA. Pattern of medical admission at Ogun State University Teaching Hospital: A three year review. West Afr J Med. 2000;19:304–7. [PubMed] [Google Scholar]
- 8.Owolabi LF, Sheu MN, Sheu MY, Fadare J. Pattern of Neurological admissions in the tropics: Experience at Kano, Northwestern Nigeria. Ann Indian Acad Neurol. 2010;13:167–70. doi: 10.4103/0972-2327.70875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Owolabi LF, Nagoda M. Stroke in developing countries: Experience at Kano, Northwestern Nigeria. Sudan JMS. 2012;7:9–14. [Google Scholar]
- 10.Owolabi LF, Ibrahim A. Stroke in Young Adults: A prospective study from Northwestern Nigeria. ISRN Neurology. 2012;10:1–5. doi: 10.5402/2012/468706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Owolabi LF, Yakasai MM. Stroke-related Wernicke's Aphasia Mistaken for Psychosis: A Case Report. J Med Trop. 2011;14(1):83–5. [Google Scholar]
- 12.World Health Organization. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke. 1989;20:1407–31. doi: 10.1161/01.str.20.10.1407. [DOI] [PubMed] [Google Scholar]
- 13.Ogun SA, Odusote KA. Effectiveness of high dose dexamethazone in the treatment in the treatment of acute stroke. West Afr J Med. 2001;9:1–6. [PubMed] [Google Scholar]
- 14.Ogungbo BI, Gregsson B, Mendelow AD, Walker R. Cerebrovascular diseases in Nigeria: What do we know and what do we need to know? Trop Doc. 2003;33:25–30. doi: 10.1177/004947550303300112. [DOI] [PubMed] [Google Scholar]
- 15.Adams HP, Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke. Stroke. 2007;38:1655–711. doi: 10.1161/STROKEAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 16.Viriyavejakul A. Stroke in Asia: An epidemiological consideration. Clin Neuropharmacol. 1990;13:S26–33. doi: 10.1097/00002826-199013003-00003. [DOI] [PubMed] [Google Scholar]
- 17.Bwala SA. “Stroke in a sub-Saharan Nigerian hospital: A retrospective study. Trop Doct. 1989;19:11–4. doi: 10.1177/004947558901900104. [DOI] [PubMed] [Google Scholar]
- 18.Massaro AR. “Stroke in Brazil: A South America perspective,”. Int J Stroke. 2006;1:113–5. doi: 10.1111/j.1747-4949.2006.00029.x. [DOI] [PubMed] [Google Scholar]
- 19.Nicoletti A, Sofia V, Giuffrida S, Bartoloni A, Bartalesi F, Bartolo ML, et al. Prevalence of stroke: A door-to-door survey in rural Bolivia. Stroke. 2000;31:882–5. doi: 10.1161/01.str.31.4.882. [DOI] [PubMed] [Google Scholar]
- 20.Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: The Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147:259–68. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 21.Warlow CP. Epidemiology of stroke. Lancet. 1998;352:1–4. doi: 10.1016/s0140-6736(98)90086-1. [DOI] [PubMed] [Google Scholar]
- 22.Ghandehari K, Pourzahed A, Taheri M, Abbasi M, Gorjestani S, Ahmadi AM, et al. Estimation of Iranian stroke patients eligible for intravenous thrombolysis with tPA. Int J Stroke. 2009;4:236. doi: 10.1111/j.1747-4949.2009.00273.x. [DOI] [PubMed] [Google Scholar]
- 23.Ghandehari K, Izadi Mood Z. Cardioembolic strokes in Eastern Iran and the importance of rheumatic valvular disease. Turkish J Med Sci. 2006;36:3614. [Google Scholar]
- 24.Komolafe MA, Ogunlade O, Komolafe EO. Stroke mortality in a teaching hospital in South Western Nigeria. Trop Doct. 2007;37:186–8. doi: 10.1258/004947507781524557. [DOI] [PubMed] [Google Scholar]
- 25.Kumral E, Ozkaya B, Sagduyu A, Sirin H, Vardarli E, Pehlivan M. The Ege Stroke Registry: Hospital-based study in Aegean region, Izmir, Turkey. Cerebrovasc Dis. 1998;8:278–88. doi: 10.1159/000015866. [DOI] [PubMed] [Google Scholar]
- 26.Bornstein NM, Aronovich BD, Karepov VG, Gur AY, Treves TA, Oved M, et al. The Tel-Aviv Stroke Registry: The consecutive 3600 patients. Stroke. 1996;27:1770–3. doi: 10.1161/01.str.27.10.1770. [DOI] [PubMed] [Google Scholar]
- 27.Moulin T, Tatu L, Crépin-Leblond T, Chavot D, Bergès S, Rumbach T. Besancom Stroke Registry: An acute stroke registry of 2,500 consecutive patients. Eur Neuro. 1997;38:10–20. doi: 10.1159/000112896. [DOI] [PubMed] [Google Scholar]
- 28.Bak S, Bak L, Sorense JS. Prevalence of risk factors in cerebral ischemia. Ugeskr Laeger. 1995;157:444–6. [PubMed] [Google Scholar]
- 29.Nwosu CM, Nwabueze AC, Ikeh VO. Stroke at the prime of life: A study of Nigerian Africans between the ages of 16 and 45 years. East Afr Med J. 1992;69:384–90. [PubMed] [Google Scholar]
- 30.Onwuchewa A, Bellgam H, Asekomeh G. Stroke at the university of port harcourt teaching hospital, rivers state, Nigeria. Trop Doct. 2009;39:150–2. doi: 10.1258/td.2008.080285. [DOI] [PubMed] [Google Scholar]
- 31.Ong TZ, Raymond AA. Risk factors for stroke and predictors of one-month mortality. Singapore Med J. 2002;43:517–21. [PubMed] [Google Scholar]
- 32.Kumral E, Ozkaya B, Sagduyu A, Sirin H, Vardarli E, Pehlivan M, et al. The Ege Stroke Registry: A hospital-based study in Aegean region, Izmir, Turkey. Cerebrovasc Dis. 1998;8:278–88. doi: 10.1159/000015866. [DOI] [PubMed] [Google Scholar]
- 33.Anderson CS, Jamrozik KD, Broadhurst RJ, Stewart-Wynne EG. Predicting survival for 1 year among different subtypes of stroke. Results from the Perth Community Stroke Study. Stroke. 1994;25:1935–44. doi: 10.1161/01.str.25.10.1935. [DOI] [PubMed] [Google Scholar]
- 34.Bamford J, Dennis MS, Sandercock P, Burn J, Warlow C. The frequency, cause and timing of death within 30 days of a first ever stroke: The Oxfordshire Community Stroke Project. J Neurol Neurosurg Psychiatr. 1990;53:824–9. doi: 10.1136/jnnp.53.10.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stegmayr B, Vinogradova T, Malyutina S, Peltonen M, Nikitin Y, Asplund K. Widening gap of stroke between East and West. Eight-year trends in occurrence and risk factors in Russia and Sweden. Stroke. 2000;31:2–8. doi: 10.1161/01.str.31.1.2. [DOI] [PubMed] [Google Scholar]
- 36.Jover-Saenz A, Porcel-Perez JM, Vives-Soto M, Rubio-Caballero M. Epidemiology of acute cerebrovascular disease in Lleida from 1996-1997. Predictive factors of mortality at short and medium term. Rev Neurol. 1999;28:941–8. [PubMed] [Google Scholar]
- 37.Mbala-Mukendi M, Tambwe MJ, Dikassa LN, M Buyamba-Kabangu JR. Initial arterial pressure and prognosis of cerebrovascular accidents. Arch Mal Coeur Vaiss. 1995;88:21–5. [PubMed] [Google Scholar]
- 38.Simon WR, Francis ALM, Robert BT. The Relation of Blood Pressure to Stroke Prognosis. Ann Intern Med. 1978;89:15–20. doi: 10.7326/0003-4819-89-1-15. [DOI] [PubMed] [Google Scholar]
- 39.Mazza A, Pessina AC, Gianluca P, Tikhonoff V, Pavei A. Casiglia E Pulse pressure: An independent predictor of coronary and stroke mortality in elderly females from the general population. Blood Press. 2001;10:205–11. doi: 10.1080/08037050152669710. [DOI] [PubMed] [Google Scholar]
- 40.Yang W, Lynette LY, Christopher L, Richard FH, Janet F. Influence of Hyperglycemia on Stroke Mortality. J Stroke Cerebrovasc Dis. 2001;10:11–8. doi: 10.1053/jscd.2001.20976. [DOI] [PubMed] [Google Scholar]
- 41.Moulin T, Tatu L, Crépin-Leblond T, Chavot D, Bergès S, Rumbach T. Besancom Stroke Registry: An acute stroke registry of 2,500 consecutive patients. Eur Neuro. 1997;38:10–20. doi: 10.1159/000112896. [DOI] [PubMed] [Google Scholar]
- 42.Thorsten S, Gabriel M, Michael De G, Peter S, Rolf H, Werner H. Prognosis of stroke patients requiring mechanical ventilation in a neurological critical care unit. Stroke. 1997;28:711–5. doi: 10.1161/01.str.28.4.711. [DOI] [PubMed] [Google Scholar]
- 43.Burtin P, Bollaert PE, Feldmann L, Lelarge P, Bauer P, Larcan A. Prognosis of patients with stroke undergoing mechanical ventilation. Intensive Care Med. 1994;20:32–6. doi: 10.1007/BF02425052. [DOI] [PubMed] [Google Scholar]
- 44.Chambers BR, Norris JW, Shurvell BL, Hachinski VC. Prognosis of acute stroke. Neurology. 1987;37:221–5. doi: 10.1212/wnl.37.2.221. [DOI] [PubMed] [Google Scholar]
- 45.Bonita R, Ford MA, Stewart AW. Predicting survival after stroke: A three-year follow-up. Stroke. 1988;19:669–73. doi: 10.1161/01.str.19.6.669. [DOI] [PubMed] [Google Scholar]
- 46.Sheikh K, Brennan PJ, Meade TW, Smith DS, Goldenberg E. Predictors of mortality and disability in stroke. J Epidemiol Community Health. 1983;37:70–4. doi: 10.1136/jech.37.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. “Malignant› middle cerebral artery territory infarction: Clinical course and prognostic signs. Arch Neurol. 1996;53:309–15. doi: 10.1001/archneur.1996.00550040037012. [DOI] [PubMed] [Google Scholar]
- 48.Smithard DG, O’Neill PA, Park C, Morris J. Complications and outcome after acute stroke – does dysphagia matter? Stroke. 1996;27:1200–4. doi: 10.1161/01.str.27.7.1200. [DOI] [PubMed] [Google Scholar]
- 49.Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. BMJ. 1987;295:411–4. doi: 10.1136/bmj.295.6595.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barer DH. The natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry. 1989;52:236–41. doi: 10.1136/jnnp.52.2.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999;30:744–8. doi: 10.1161/01.str.30.4.744. [DOI] [PubMed] [Google Scholar]
- 52.Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003;60:620–5. doi: 10.1212/01.wnl.0000046586.38284.60. [DOI] [PubMed] [Google Scholar]
- 53.Davenport RJ, Dennis MS, Wellwood I, Warlow CP. Complication after acute stroke. Stroke. 1996;27:415–20. doi: 10.1161/01.str.27.3.415. [DOI] [PubMed] [Google Scholar]


