Summary
The estrogen receptor (ER) and/or the human epidermal growth factor receptor 2 (HER2) signaling pathways are the dominant drivers of cell proliferation and survival in the majority of human breast cancers. As a result, targeting these pathways provides the most effective therapies in appropriately selected patients. Nevertheless, resistance to both endocrine and anti-HER2 therapies occurs frequently and represents a major clinical challenge. Compelling preclinical and clinical evidence relates this treatment resistance to the presence of a complex bidirectional molecular crosstalk between the ER and HER2 pathways. As a consequence, treatment strategies targeting either pathway are associated with up-regulation of the other one, ultimately resulting in resistance to therapy. Therefore, a more promising strategy to prevent or overcome either endocrine or anti-HER2 resistance at least in some tumors is to combine targeted treatments that simultaneously block both signaling pathways. Many clinical trials exploring this strategy have shown positive results, and many more are currently ongoing. Future clinical trials with appropriate patient selection, based on biomarker evaluation of primary tumors and possibly of recurrent lesions, are warranted for the optimization of individualized therapeutic strategies.
KeyWords: Estrogen Receptor, HER2, Crosstalk, Resistance
Zusammenfassung
Die Signalwege des Östrogenrezeptors (ER) und/oder des humanen epidermalen Wachstumsfaktorrezeptors 2 (HER2) sind bei der Mehrzahl der Brustkrebsarten des Menschen die ausschlaggebenden Faktoren für die Proliferation und das Überleben von Zellen. Eine Blockade dieser Signalwege ermöglicht deshalb die wirksamsten Therapien bei entsprechend ausgewählten Patientinnen. Dennoch kommt es oft zu einer Resistenz sowohl gegen endokrine als gegen auch Anti-HER2-Therapien, die in der klinischen Praxis eine große Herausforderung darstellt. Es gibt überzeugende präklinische und klinische Hinweise, dass diese Behandlungsresistenz mit der Existenz einer komplexen gegenseitigen Beeinflussung zwischen den ER- und HER2-Signalwegen zusammenhängt. Aus diesem Grund sind Behandlungsstrategien, die auf einen der Signalwege abzielen, mit der Hochregulation des anderen Signalwegs verknüpft, was letztendlich zur Therapieresistenz führt. Eine aussichtsreichere Strategie, um eine endokrine oder Anti-HER2-Resistenz zumindest bei einigen Tumoren zu verhindern oder zu überwinden, ist deshalb die Kombination von gezielten Therapien, die beide Signalwege gleichzeitig hemmen. Viele klinische Studien, die diese Strategie erforschen, haben positive Resultate gezeigt und viele weitere sind zurzeit noch nicht abgeschlossen. Zukünftige klinische Studien, die auf einer Evaluation der Primärtumoren und eventuell erneut auftretender Tumoren mithilfe von Biomarkern beruhen, sollten zur Optimierung von individualisierten Therapiestrategien durchgeführt werden.
Introduction
Despite the recent advances in the therapy and prevention of breast cancer, this malignancy remains the leading cause of cancer death among women, with approximately 425,000 deaths worldwide in 2010 [1]. In the last decades, many efforts have been made to understand the molecular mechanisms responsible for breast tumor initiation and progression and to develop effective treatment strategies. Breast cancer is a heterogeneous disease and various tumor characteristics can predict different treatment responses and patient outcomes. Traditionally, breast tumors are classified into distinct clinical subtypes by using histopathological features, such as the expression of the estrogen receptor (ER), the progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2). This histopathological classification identifies 3 major clinical subtypes, including the hormone receptor-positive (HR+; ER- and/or PR-positive), the HER2-positive (HER2+), and the triple-negative (TN; negative expression of ER, PR and HER2) subtypes, which are associated with different biological behaviors and treatment sensitivities. In addition, a novel molecular taxonomy based on gene expression profiling has recently been developed, with important therapeutic implications. This molecular classification describes 5 major subtypes, including the luminal A and B (corresponding to some extent to the ER+/PR+ and ER+/PR-/ HER2+ subtypes, respectively), the HER2 (corresponding to the HER2+/HR- subtype), the basal-like (partially overlapping with the TN subtype), and the normal breast-like subtype [2, 3]. Both the histopathological and the molecular classifications clearly indicate that ER and HER2 represent the dominant drivers of tumor growth, since they are present or overexpressed in the majority of tumors. Therefore, targeting these pathways provides the most effective therapies in appropriately selected patients. However, despite the overall success of ER- and HER2-targeting agents, treatment resistance remains a major clinical problem. Compelling preclinical and clinical evidence suggests the existence of a bidirectional crosstalk between the ER and HER2 pathways, which contributes to the development of endocrine resistance as well as resistance to HER2-targeted therapies [4]. The aim of this review is to summarize the current knowledge regarding the molecular mechanisms of this bidirectional crosstalk and to highlight its clinical implications.
ER and HER2 Pathways and Targeted Therapies
Two isoforms of the ER protein encoded by distinct genes have been identified: ERα, which mediates breast cancer cell proliferation and survival, and ERß, whose function in breast cancer is still unclear. Experimental evidence indicates that ERß may antagonize the ability of ERα to stimulate proliferation in response to estrogen (E2) [5]. For the purpose of this review, we will use ‘ER’ to indicate ‘ERα’, if not otherwise specified. ER acts predominantly as a hormone-activated nuclear transcription factor that binds to specific DNA sequences (estrogen response elements, EREs) localized in the enhancer/promoter regions of target genes mediating cell proliferation and survival (classical ER nuclear genomic pathway; fig. 1A) [5]. Importantly, this classical ER transcriptional activity can be modulated by different coregulators (coactivators and corepressors) [6]. ER can also induce gene expression by tethering to other transcription factors, such as the activator protein 1 (AP-1), the specificity protein 1 (SP-1), and the nuclear factor κB (NFκB) [7]. This alternative genomic signaling is also known as the non-classical ER nuclear genomic pathway (fig. 1B). Finally, ER is involved in non-nuclear/non-genomic pathways, where either the traditional ER protein or short spliced/translational variants, localized at the plasma membrane or in its vicinity, can interact with and activate several receptor tyrosine kinases (RTKs; e.g. HER2) and their downstream signaling intermediates (e.g. p42/44 mitogen-activated protein kinase (MAPK) and Akt) (fig. 1B) [8]. 3 main approaches have been successfully developed to block ER signaling in breast cancer: (1) competitive inhibition of estrogen action via ER antagonism by selective estrogen receptor modulators (SERMs; such as tamoxifen) or (2) by selective estrogen receptor down-regulators (SERDs; such as fulvestrant), which also degrade the ER protein (fig. 1A); and (3) reduction of estrogen levels by aromatase inhibitors (AIs; such as aromasin, anastrozole, letrozole; fig. 1A) or by ovarian suppression (e.g. gonadotropin-releasing hormone (GnRH) agonists, surgical ovariectomy), in postmenopausal and premenopausal patients, respectively [9, 10]. Despite the remarkable efficacy of the aforementioned endocrine treatments, more than 50% of patients with metastatic disease do not respond to first-line endocrine therapy, and the majority of responders eventually relapse [11, 12]. Also, the risk of disease recurrence in early breast cancer patients receiving adjuvant endocrine therapy remains a significant problem [13].
Fig. 1.
ER signaling, targeted therapies, and endocrine resistance. (A) ER signaling as dominant driver of cell proliferation and survival. The binding of estrogen to the ER protein results in its interaction with DNA, either directly at EREs of promoter/enhancer regions of target genes (classical nuclear genomic pathway) or indirectly by tethering to other transcription factors, including AP-1 and SP-1, at their DNA binding sites (non-classical nuclear genomic pathway). Estrogen-activated ER also interacts with coactivators (CoA) that facilitate its transcriptional activity. Ultimately, the transcription of ER target genes promotes cell proliferation, survival, and invasion. A small fraction of the cellular ER pool also resides at, or in proximity to, the plasma membrane, where it interacts with and promotes the activity of RTKs and other cellular kinases (non-nuclear/non-genomic pathway). Nuclear ER genomic activity is predominant in tumor cells with low growth factor receptor signaling and can be effectively inhibited by endocrine therapy with tamoxifen (T), fulvestrant (F), and Als. (B) Bidirectional crosstalk between the ER and HER pathways and resistance to endocrine therapy. In the presence of hyperactive HER signaling (such as in HER2+ tumors or in case of acquired overexpression of HER receptors during endocrine therapy), activated downstream kinases (e.g. Akt and MAPK) reduce ER expression at both the mRNA and protein levels. At the same time, these kinases phosphorylate ER and its coregulators, potentiating and modulating ER transcriptional activity and negating the effect of endocrine therapy. In addition, cytoplasmic/membrane ER non-genomic activity is increased, leading to further activation of the HER pathway by direct or indirect interaction with the HER receptors, G proteins, and other intracellular kinases. Non-nuclear/non-genomic ER activity can be stimulated rather than inhibited by tamoxifen. Collectively, these molecular events together contribute to intrinsic and acquired endocrine resistance.
Multiple lines of evidence suggest that endocrine resistance is associated with hyperactivity of RTK signaling pathways that circumvent hormonal treatment by modulating ER expression and/or its activity. Among these RTK pathways, the human epidermal growth factor receptor (HER) family seems to play a crucial role, and is the focus of this review [14]. Indeed, ER+ breast tumors that also overexpress HER2 show de novo (intrinsic) resistance to endocrine therapy [15, 16]. In addition, in both the preclinical and the clinical settings, increased HER signaling is associated with the development of acquired endocrine resistance [14, 17].
The HER family comprises 4 RTKs (HER1–4) and their several ligands (at least 11) [18]. Upon binding with the HER ligands, the receptors form homo- and heterodimers and activate downstream pathways (e.g. p42/44 MAPK and phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR)) mediating proliferation and survival stimuli (fig. 2A) [18]. In breast cancer, HER2 is the dominant RTK of the HER family, being overexpressed or gene-amplified in 20–25% of tumors, where it represents the dominant driver of cell growth. In these tumors, HER2, which does not have a ligand, is activated by heterodimerization with other ligand-bonded HER receptors, or by homodimerization. In the recent years, several drugs able to effectively block the HER pathway (primarily HER2) have been introduced in clinical practice. They are either monoclonal antibodies, such as trastuzumab, or small tyrosine kinase inhibitor molecules, such as the HER1/HER2 inhibitor lapatinib (fig. 2B) [19, 20]. More recently, 2 new agents have been approved by the Food and Drug Administration (FDA) for the treatment of advanced HER2+ breast cancer: the monoclonal antibody pertuzumab and the antibody-toxin conjugate trastuzumab emtansine (T-DM1; fig. 2B) [21, 22]. Despite the efficacy of these agents, HER2+ tumors can acquire treatment resistance either by reactivating the HER pathway or by activating alternative escape pathways that can bypass effective HER inhibition. One of these potential escape pathways is the ER signaling network itself. In support of this hypothesis, it has been shown that resistance to anti-HER2 treatments is associated with the reactivation of the ER pathway in HER2+/ER+ breast cancer preclinical models [23, 24]. In these models, ER inhibition determines cell growth arrest and apoptosis in lapatinib- and lapatinib + trastuzumab-resistant cells [23, 24]. Consistently, in clinical trials in patients with HER2+ breast tumors, ER positivity is associated with reduced response to HER2-targeting therapies [25]. This suggests the existence of a bidirectional crosstalk between the ER and HER pathways, potentially responsible for resistance not only to endocrine therapy but also to anti-HER2 treatments. In the next paragraphs, we will briefly describe the key molecular mechanisms of this crosstalk and highlight potential treatment strategies to overcome it.
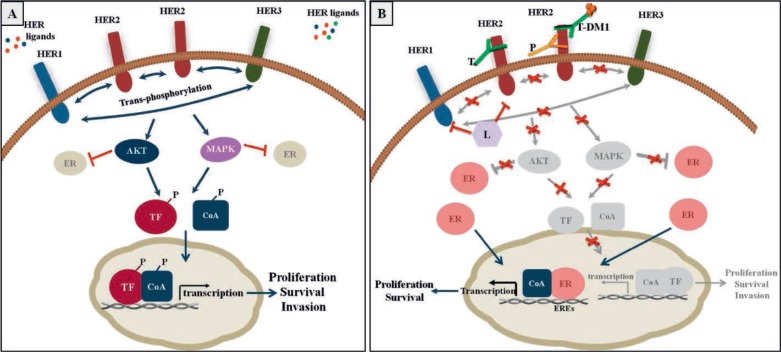
Fig. 2.
HER2 family pathways, targeted therapies, and treatment resistance. (A) HER signaling pathway as dominant driver of tumor cell growth and survival. Ligand-bound HER homo- and heterodimers, and HER2 homodimers in HER2+ tumors, activate downstream pathways (e.g. p42/44 MAPK and Akt), which in turn modulate the levels or activities of various transcription factors (TF) and their coregulators (such as coactivators, CoA). Activation of this core signaling process leads to changes in gene expression that ultimately mediate proliferation and survival stimuli. (B) ER signaling as mechanism of resistance to anti-HER2 therapy. Potent inhibition of the HER receptor layer by trastuzumab (T), lapatinib (L), pertuzumab (P), and trastuzumab-emtansine (T-DM1), as single agents or in combination, leads to effective blockade of downstream signaling, resulting in arrest of proliferation and induction of apoptosis. However, effective HER inhibition can lead to restoration/reactivation of ER signaling, which in turn provides alternative survival and proliferation stimuli leading to anti-HER2 resistance.
Molecular Mechanisms of the ER/HER Crosstalk
The deregulation of ER and HER pathways in breast cancer can occur by alteration of upstream signaling molecules (e.g. overexpression/amplification of HER receptors and/or their ligands) or as a result of genetic/epigenetic modifications of downstream signaling effectors (e.g. loss of heterozygosity or methylation of the tumor suppressor PTEN (phosphatase and tensin homolog) and activation of Akt) [26, 27]. The bidirectional ER/HER crosstalk can influence each of these pathways at the level of their expression and/or activity. Preclinical and clinical studies have shown an inverse correlation between ER and HER2 expression in breast cancer [28]. It has been proposed that HER signaling members can reduce ER expression both at the mRNA and protein levels. For instance, Akt inactivates the Forkhead box protein FOXO3a that represents a key regulator of ER gene transcription (fig. 1B) [29]. Also, activation of p44/42 MAPK is directly responsible for ER degradation (fig. 1B) [30]. In addition, it has recently been shown that RTK signaling members can interact with ERβ and impair its growth-inhibitory effects [31]. A potential consequence of this negative control exerted by the HER pathway on ER expression levels is a diminution of endocrine sensitivity. Importantly, for the same reason, effective blockade of the HER pathway results in increased/restored ER levels in HER2+ breast cancer preclinical models (fig. 2B). In these cell line models, the reactivated ER signaling can then become an escape survival pathway responsible for anti-HER2 resistance [23, 24].
In contrast to the negative effect of the HER signaling on ER levels, the activation of this pathway can also potentiate or modulate ER genomic and non-genomic signaling as well as its ligand dependency, resulting in impairment of endocrine sensitivity. In particular, the ER protein can be phosphorylated and activated in a ligand-independent manner by multiple RTK-dependent and stress-related kinases, including p44/42 MAPK, PI3K/Akt, and p38 MAPK (fig. 1B) [27, 32, 33]. These same kinases can also phosphorylate and activate ER coactivators, such as Src3 (also known as AIB1 (amplified in breast cancer 1); fig. 1B) [34]. This can determine a switch in the pharmacological action of SERMs such as tamoxifen from antagonistic to agonistic effects, leading to tamoxifen resistance [15]. Moreover, a recent study of ER genomic cistromes (genome-wide ER binding sites) has shown that, under estrogen deprivation and overactive RTK signaling conditions, ER can be recruited to different genomic binding sites in a ligand-independent manner [35]. This results in an alternative ER transcriptional program that is primarily dependent on AP-1 DNA sites. This AP-1-dependent switch in the ER transcriptional program has been observed also in a tamoxifen-resistant breast cancer preclinical model [36]. Importantly, many of the genes induced by the alternative ER transcriptional activity are overexpressed in HER2+ breast tumors [35]. In addition, our group developed a transcriptional and proteomic PI3K signature showing that hyperactive PI3K signaling in human breast tumors was associated with a reduction in expression of classic ER target genes, such as the PR gene. Consistently, PI3K signature scores were higher in luminal B (ER+/PR-) than in luminal A (ER+/PR+) tumors [37].
ER in turn, via both its membrane and nuclear activities, can interact with and activate the HER signaling members. As anticipated in the previous paragraph, upon estrogen binding, ER can activate the HER receptors either directly or indirectly via G protein interaction [8]. Also, ER can stimulate a signaling cascade involving the tyrosine kinase c-Src and other RTK downstream signaling members (fig. 1B) [38]. Estrogen signaling can also increase the expression of growth factors such as the transforming growth factor-α (TGFα) and the insulin-like growth factor 1 (IGF1) [39, 40]. On the other hand, it has been shown that ER signaling can down-regulate the expression of HER1 and HER2 and increase that of the IGF1 receptor [39, 41, 42]. This ER-induced hyperactivity of alternative growth factor receptor pathways can function as an escape from effective HER-targeting therapies.
All these complex bidirectional molecular circuits between the ER and HER2 signaling networks, if left uninhibited, can contribute in concert to the development of resistance to targeted therapies against these two key pathways.
Clinical Implications
As a direct consequence of the extensive crosstalk between the ER and HER2 signaling pathways, treatment strategies targeting only one of the pathways often result in the up-regulation of the other one, and ultimately in resistance to therapy. As an example, neoadjuvant treatment with AIs was associated with increased HER2 mRNA levels in tumors originally not overexpressing HER2 [43]. On the other hand, neoadjuvant anti-HER2 treatment increased ER expression and activity in HER2+ tumors [24, 44]. Thus, a more promising strategy to prevent or overcome endocrine and anti-HER2 resistance is to combine targeted treatments to simultaneously block both signaling pathways. In this attempt, several clinical trials have evaluated the effectiveness of combining endocrine therapy with anti-HER2 treatment in patients with ER+/HER2+ tumors. In the phase III TAnDEM trial, ER+/HER2+ metastatic breast cancer (MBC) patients receiving the combination of the AI anastrozole with trastuzumab had a longer progression-free survival (PFS) compared with those treated with the AI alone [45]. However, the overall response rate achieved in the combination arm was relatively low compared with the historical control of trastuzumab + chemotherapy, suggesting the need of an improved patient selection to identify those who can benefit from the combination of ER- and HER2-targeting therapies without chemotherapy. In a large phase III trial comparing another AI, letrozole, with and without lapatinib in patients with ER+ MBC, the combination treatment resulted in a clinical benefit that was primarily confined to the HER2+ subset [46]. In the neoadjuvant setting, potent anti-HER2 treatment with trastuzumab + lapatinib combined with letrozole in patients with locally advanced HER2+/ER+ breast tumors determined a pathologic complete response (pCR) rate of 21%, suggesting that a selected subset of patients with HER2+ tumors that are also highly responsive to endocrine therapy may greatly benefit from chemotherapy-free regimens that effectively block both the ER and the HER2 pathways [47]. Combinations of endocrine therapy with agents targeting either the HER receptors or downstream signaling intermediates have been tested in multiple trials also in ER+/HER2- MBC. As an example, the combination of tamoxifen with the epidermal growth factor receptor (EGFR) inhibitor gefitinib showed a numerical advantage in PFS compared with tamoxifen alone in a phase II trial randomizing HR+ MBC patients [48]. Consistent results were reported in a randomized phase II study evaluating the combination of anastrozole + gefitinib [49].
Despite their positive results, these trials showed only a small benefit from the addition of upstream HER signaling inhibitors to endocrine therapy. This suggests the need to test alternative strategies to more effectively block the HER pathways, such as the inhibition of downstream signaling molecules. Indeed, the randomized phase III trial BOLERO II that assessed the steroidal AI exemestane with or without the mTOR inhibitor everolimus showed a remarkable survival advantage in the combination arm [50]. As a consequence, this combination has become the standard treatment for ER+ MBC patients progressing on a previous treatment with non-steroidal AIs. In addition, many ongoing clinical trials are currently evaluating, in both the metastatic and the neoadjuvant settings, the effect of agents inhibiting different signaling molecules downstream from the HER tyrosine kinase receptors, including PI3K, Akt, mTOR, and MAP kinase kinases (MEK), in the context of endocrine resistance [51]. Importantly, emerging preclinical and clinical evidence suggests the presence of negative feedback loops among the RTK pathways that may limit the efficacy of targeted therapies (e.g. activation of the p44/42 MAPK pathway induced by mTOR inhibition) [52, 53]. Thus, a more extensive blockade of multiple up- and downstream pathways, obtained by combining different targeted agents, may be necessary to overcome treatment resistance. Also, since the molecular expression and signaling of tumor cells can change despite effective targeted treatment due to feedback loops and activation of escape pathways (e.g. ER restoration in tumors treated with anti-HER2 agents), re-biopsy of recurrent/progressing lesions, where feasible, should be considered in order to optimize individualized therapeutic strategies.
In conclusion, future clinical trials are warranted to optimize patient selection, improve biomarkers available to guide therapy and to identify novel targets, and test the efficacy and safety of new targeted therapies that can overcome endocrine and anti-HER2 resistance.
Disclosure Statement
None of the authors has conflicts of interests to disclose.
Acknowledgements
Supported in part by: National Cancer Institute grants P50 CA58183 (Breast Cancer SPORE) and P30CA125123 (Cancer Center); The Breast Cancer Research Foundation, Entertainment Industry Foundation/Lee Jeans Breast Cancer Program and Stand Up 2 Cancer; Cancer Prevention and Research Institute of Texas (CPRIT) program RP101499 – Baylor College of Medicine Comprehensive Cancer Training Program (to M.G.).
References
- 1.Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJ, Naghavi M. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378:1461–1484. doi: 10.1016/S0140-6736(11)61351-2. [DOI] [PubMed] [Google Scholar]
- 2.Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lonning PE, Borresen-Dale AL, Brown PO, Botstein D. Molecular portraits of human breast tumours. Nature. 2000;406:747–752. doi: 10.1038/35021093. [DOI] [PubMed] [Google Scholar]
- 3.Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M, Jeffrey SS, Thorsen T, Quist H, Matese JC, Brown PO, Botstein D, Lonning PE, Borresen-Dale AL. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98:10869–10874. doi: 10.1073/pnas.191367098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arpino G, Wiechmann L, Osborne CK, Schiff R. Crosstalk between the estrogen receptor and the HER tyrosine kinase receptor family: molecular mechanism and clinical implications for endocrine therapy resistance. Endocr Rev. 2008;29:217–233. doi: 10.1210/er.2006-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osborne CK, Schiff R, Fuqua SA, Shou J. Estrogen receptor: current understanding of its activation and modulation. Clin Cancer Res. 2001;7:4338s–4342s. discussion 4411s–4412s. [PubMed] [Google Scholar]
- 6.McKenna NJ, Lanz RB, O'Malley BW. Nuclear receptor coregulators: cellular and molecular biology. Endocr Rev. 1999;20:321–344. doi: 10.1210/edrv.20.3.0366. [DOI] [PubMed] [Google Scholar]
- 7.Kushner PJ, Agard DA, Greene GL, Scanlan TS, Shiau AK, Uht RM, Webb P. Estrogen receptor pathways to AP-1. J Steroid Biochem Mol Biol. 2000;74:311–317. doi: 10.1016/s0960-0760(00)00108-4. [DOI] [PubMed] [Google Scholar]
- 8.Nemere I, Pietras RJ, Blackmore PF. Membrane receptors for steroid hormones: signal transduction and physiological significance. J Cell Biochem. 2003;88:438–445. doi: 10.1002/jcb.10409. [DOI] [PubMed] [Google Scholar]
- 9.Lake DE, Hudis C. Aromatase inhibitors in breast cancer: an update. Cancer Control. 2002;9:490–498. doi: 10.1177/107327480200900606. [DOI] [PubMed] [Google Scholar]
- 10.Goel S, Sharma R, Hamilton A, Beith J. LHRH agonists for adjuvant therapy of early breast cancer in premenopausal women. Cochrane Database Syst Rev. 2009;4:CD004562. doi: 10.1002/14651858.CD004562.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ring A, Dowsett M. Mechanisms of tamoxifen resistance. Endocr Relat Cancer. 2004;11:643–658. doi: 10.1677/erc.1.00776. [DOI] [PubMed] [Google Scholar]
- 12.Brodie A, Sabnis G. Adaptive changes result in activation of alternate signaling pathways and acquisition of resistance to aromatase inhibitors. Clin Cancer Res. 2011;17:4208–4213. doi: 10.1158/1078-0432.CCR-10-2920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fisher B, Jeong JH, Bryant J, Anderson S, Dignam J, Fisher ER, Wolmark N. Treatment of lymph-node-negative, oestrogen-receptor-positive breast cancer: long-term findings from National Surgical Adjuvant Breast and Bowel Project randomised clinical trials. Lancet. 2004;364:858–868. doi: 10.1016/S0140-6736(04)16981-X. [DOI] [PubMed] [Google Scholar]
- 14.Osborne CK, Schiff R. Mechanisms of endocrine resistance in breast cancer. Annu Rev Med. 2011;62:233–247. doi: 10.1146/annurev-med-070909-182917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shou J, Massarweh S, Osborne CK, Wakeling AE, Ali S, Weiss H, Schiff R. Mechanisms of tamoxifen resistance: increased estrogen receptor-HER2/neu cross-talk in ER/HER2-positive breast cancer. J Natl Cancer Inst. 2004;96:926–935. doi: 10.1093/jnci/djh166. [DOI] [PubMed] [Google Scholar]
- 16.Chung YL, Sheu ML, Yang SC, Lin CH, Yen SH. Resistance to tamoxifen-induced apoptosis is associated with direct interaction between HER2/neu and cell membrane estrogen receptor in breast cancer. Int J Cancer. 2002;97:306–312. doi: 10.1002/ijc.1614. [DOI] [PubMed] [Google Scholar]
- 17.Nicholson RI, McClelland RA, Finlay P, Eaton CL, Gullick WJ, Dixon AR, Robertson JF, Ellis IO, Blamey RW. Relationship between EGF-R, c-erbB-2 protein expression and Ki67 immu-nostaining in breast cancer and hormone sensitivity. Eur J Cancer. 1993;29A:1018–1023. doi: 10.1016/s0959-8049(05)80215-1. [DOI] [PubMed] [Google Scholar]
- 18.Citri A, Yarden Y. EGF-erbB signalling: towards the systems level. Nat Rev Mol Cell Biol. 2006;7:505–516. doi: 10.1038/nrm1962. [DOI] [PubMed] [Google Scholar]
- 19.Lan KH, Lu CH, Yu D. Mechanisms of trastuzumab resistance and their clinical implications. Ann N Y Acad Sci. 2005;1059:70–75. doi: 10.1196/annals.1339.026. [DOI] [PubMed] [Google Scholar]
- 20.Spector NL, Xia W, Burris H, 3rd, Hurwitz H, Dees EC, Dowlati A, O'Neil B, Overmoyer B, Marcom PK, Blackwell KL, Smith DA, Koch KM, Stead A, Mangum S, Ellis MJ, Liu L, Man AK, Bremer TM, Harris J, Bacus S. Study of the biologic effects of lapatinib, a reversible inhibitor of erbB1 and erbB2 tyrosine kinases, on tumor growth and survival pathways in patients with advanced malignancies. J Clin Oncol. 2005;23:2502–2512. doi: 10.1200/JCO.2005.12.157. [DOI] [PubMed] [Google Scholar]
- 21.O'Sullivan CC, Swain SM. Pertuzumab: evolving therapeutic strategies in the management of HER2-overexpressing breast cancer. Expert Opin Biol Ther. 2013;13:779–790. doi: 10.1517/14712598.2013.783007. [DOI] [PubMed] [Google Scholar]
- 22.Barginear MF, John V, Budman DR. Trastuzu-mab-DM1: a clinical update of the novel antibody-drug conjugate for HER2-overexpressing breast cancer. Mol Med. 2013;18:1473–1479. doi: 10.2119/molmed.2012.00302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang YC, Morrison G, Gillihan R, Guo J, Ward RM, Fu X, Botero MF, Healy NA, Hilsenbeck SG, Phillips GL, Chamness GC, Rimawi MF, Osborne CK, Schiff R. Different mechanisms for resistance to trastuzumab versus lapatinib in HER2-positive breast cancers – role of estrogen receptor and HER2 reactivation. Breast Cancer Res. 2011;13:R121. doi: 10.1186/bcr3067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xia W, Bacus S, Hegde P, Husain I, Strum J, Liu L, Paulazzo G, Lyass L, Trusk P, Hill J, Harris J, Spector NL. A model of acquired autoresistance to a potent erbB2 tyrosine kinase inhibitor and a therapeutic strategy to prevent its onset in breast cancer. Proc Natl Acad Sci USA. 2006;103:7795–7800. doi: 10.1073/pnas.0602468103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nahta R, O'Regan RM. Therapeutic implications of estrogen receptor signaling in HER2-positive breast cancers. Breast Cancer Res Treat. 2012;135:39–48. doi: 10.1007/s10549-012-2067-8. [DOI] [PubMed] [Google Scholar]
- 26.Miller TW, Perez-Torres M, Narasanna A, Guix M, Stal O, Perez-Tenorio G, Gonzalez-Angulo AM, Hennessy BT, Mills GB, Kennedy JP, Lindsley CW, Arteaga CL. Loss of phosphatase and tensin homologue deleted on chromosome 10 engages erbB3 and insulin-like growth factor-I receptor signaling to promote antiestrogen resistance in breast cancer. Cancer Res. 2009;69:4192–4201. doi: 10.1158/0008-5472.CAN-09-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell RA, Bhat-Nakshatri P, Patel NM, Constantinidou D, Ali S, Nakshatri H. Phosphati-dylinositol 3-kinase/Akt-mediated activation of estrogen receptor alpha: A new model for anti-estrogen resistance. J Biol Chem. 2001;276:9817–9824. doi: 10.1074/jbc.M010840200. [DOI] [PubMed] [Google Scholar]
- 28.Konecny G, Pauletti G, Pegram M, Untch M, Dandekar S, Aguilar Z, Wilson C, Rong HM, Bauerfeind I, Felber M, Wang HJ, Beryt M, Seshadri R, Hepp H, Slamon DJ. Quantitative association between HER-2/neu and steroid hormone receptors in hormone receptor-positive primary breast cancer. J Natl Cancer Inst. 2003;95:142–153. doi: 10.1093/jnci/95.2.142. [DOI] [PubMed] [Google Scholar]
- 29.Guo S, Sonenshein GE. Forkhead box transcription factor FOXO3a regulates estrogen receptor alpha expression and is repressed by the HER-2/ neu/phosphatidylinositol 3-kinase/Akt signaling pathway. Mol Cell Biol. 2004;24:8681–8690. doi: 10.1128/MCB.24.19.8681-8690.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Creighton CJ, Hilger AM, Murthy S, Rae JM, Chinnaiyan AM, El-Ashry D. Activation of mitogen-activated protein kinase in estrogen receptor alpha-positive breast cancer cells in vitro induces an in vivo molecular phenotype of estrogen receptor alpha-negative human breast tumors. Cancer Res. 2006;66:3903–3911. doi: 10.1158/0008-5472.CAN-05-4363. [DOI] [PubMed] [Google Scholar]
- 31.Cotrim CZ, Fabris V, Doria ML, Lindberg K, Gustafsson JA, Amado F, Lanari C, Helguero LA. Estrogen receptor beta growth-inhibitory effects are repressed through activation of MAPK and PI3K signalling in mammary epithelial and breast cancer cells. Oncogene. 2013;32:2390–2402. doi: 10.1038/onc.2012.261. [DOI] [PubMed] [Google Scholar]
- 32.Kato S, Endoh H, Masuhiro Y, Kitamoto T, Uchiyama S, Sasaki H, Masushige S, Gotoh Y, Nishida E, Kawashima H, Metzger D, Chambon P. Activation of the estrogen receptor through phosphorylation by mitogen-activated protein kinase. Science. 1995;270:1491–1494. doi: 10.1126/science.270.5241.1491. [DOI] [PubMed] [Google Scholar]
- 33.Bunone G, Briand PA, Miksicek RJ, Picard D. Activation of the unliganded estrogen receptor by EGF involves the MAP kinase pathway and direct phosphorylation. EMBO J. 1996;15:2174–2183. [PMC free article] [PubMed] [Google Scholar]
- 34.Schiff R, Massarweh S, Shou J, Osborne CK. Breast cancer endocrine resistance: how growth factor signaling and estrogen receptor coregulators modulate response. Clin Cancer Res. 2003;9:447S–454S. [PubMed] [Google Scholar]
- 35.Lupien M, Meyer CA, Bailey ST, Eeckhoute J, Cook J, Westerling T, Zhang X, Carroll JS, Rhodes DR, Liu XS, Brown M. Growth factor stimulation induces a distinct ER(alpha) cistrome underlying breast cancer endocrine resistance. Genes Dev. 2010;24:2219–2227. doi: 10.1101/gad.1944810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Magnani L, Stoeck A, Zhang X, Lanczky A, Mirabella AC, Wang TL, Gyorffy B, Lupien M. Genome-wide reprogramming of the chromatin landscape underlies endocrine therapy resistance in breast cancer. Proc Natl Acad Sci USA. 2013;110:E1490–E1499. doi: 10.1073/pnas.1219992110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Creighton CJ, Fu X, Hennessy BT, Casa AJ, Zhang Y, Gonzalez-Angulo AM, Lluch A, Gray JW, Brown PH, Hilsenbeck SG, Osborne CK, Mills GB, Lee AV, Schiff R. Proteomic and transcriptomic profiling reveals a link between the PI3K pathway and lower estrogen-receptor (ER) levels and activity in ER+ breast cancer. Breast Cancer Res. 2010;12:R40. doi: 10.1186/bcr2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fox EM, Andrade J, Shupnik MA. Novel actions of estrogen to promote proliferation: integration of cytoplasmic and nuclear pathways. Steroids. 2009;74:622–627. doi: 10.1016/j.steroids.2008.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee AV, Cui X, Oesterreich S. Cross-talk among estrogen receptor, epidermal growth factor, and insulin-like growth factor signaling in breast cancer. Clin Cancer Res. 2001;7:4429s–4435s. discussion 4411s–4412s. [PubMed] [Google Scholar]
- 40.Vyhlidal C, Samudio I, Kladde MP, Safe S. Transcriptional activation of transforming growth factor alpha by estradiol: requirement for both a GC-rich site and an estrogen response element half-site. J Mol Endocrinol. 2000;24:329–338. doi: 10.1677/jme.0.0240329. [DOI] [PubMed] [Google Scholar]
- 41.Yarden RI, Wilson MA, Chrysogelos SA. Estrogen suppression of EGFR expression in breast cancer cells: a possible mechanism to modulate growth. J Cell Biochem Suppl. 2001;36(suppl):232–246. doi: 10.1002/jcb.1142. [DOI] [PubMed] [Google Scholar]
- 42.Newman SP, Bates NP, Vernimmen D, Parker MG, Hurst HC. Cofactor competition between the ligand-bound oestrogen receptor and an intron 1 enhancer leads to oestrogen repression of erbB2 expression in breast cancer. Oncogene. 2000;19:490–497. doi: 10.1038/sj.onc.1203416. [DOI] [PubMed] [Google Scholar]
- 43.Flageng MH, Moi LL, Dixon JM, Geisler J, Lien EA, Miller WR, Lonning PE, Mellgren G. Nuclear receptor co-activators and HER-2/neu are upregulated in breast cancer patients during neo-adjuvant treatment with aromatase inhibitors. Br J Cancer. 2009;101:1253–1260. doi: 10.1038/sj.bjc.6605324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rimawi MF, Gutierrez MC, Arpino G, Massarweh SA, Chang JC, Osborne CK, Schiff R: Inhibiting the growth factor receptor pathway preserves and enhances the expression of the estrogen receptor in HER-2/neu over-expressing human breast tumors and xenografts. Proceedings of the San Antonio Breast Cancer Symposium 2005.
- 45.Kaufman B, Mackey JR, Clemens MR, Bapsy PP, Vaid A, Wardley A, Tjulandin S, Jahn M, Lehle M, Feyereislova A, Revil C, Jones A. Trastuzumab plus anastrozole versus anastrozole alone for the treatment of postmenopausal women with human epidermal growth factor receptor 2-positive, hormone receptor-positive metastatic breast cancer: results from the randomized phase III tandem study. J Clin Oncol. 2009;27:5529–5537. doi: 10.1200/JCO.2008.20.6847. [DOI] [PubMed] [Google Scholar]
- 46.Johnston S, Pippen J, Jr, Pivot X, Lichinitser M, Sadeghi S, Dieras V, Gomez HL, Romieu G, Manikhas A, Kennedy MJ, Press MF, Maltzman J, Florance A, O'Rourke L, Oliva C, Stein S, Pegram M. Lapatinib combined with letrozole versus letrozole and placebo as first-line therapy for postmenopausal hormone receptor-positive metastatic breast cancer. J Clin Oncol. 2009;27:5538–5546. doi: 10.1200/JCO.2009.23.3734. [DOI] [PubMed] [Google Scholar]
- 47.Rimawi MF, Mayer IA, Forero A, Nanda R, Goetz MP, Rodriguez AA, Pavlick AC, Wang T, Hilsenbeck SG, Gutierrez C, Schiff R, Osborne CK, Chang JC. Multicenter phase II study of neoadjuvant lapatinib and trastuzumab with hormonal therapy and without chemotherapy in patients with human epidermal growth factor receptor 2-over-expressing breast cancer: TBCRC 006. J Clin Oncol. 2013;31:1726–1731. doi: 10.1200/JCO.2012.44.8027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Osborne CK, Neven P, Dirix LY, Mackey JR, Robert J, Underhill C, Schiff R, Gutierrez C, Migliaccio I, Anagnostou VK, Rimm DL, Magill P, Sellers M. Gefitinib or placebo in combination with tamoxifen in patients with hormone receptor-positive metastatic breast cancer: A randomized phase II study. Clin Cancer Res. 2011;17:1147–1159. doi: 10.1158/1078-0432.CCR-10-1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cristofanilli M, Valero V, Mangalik A, Royce M, Rabinowitz I, Arena FP, Kroener JF, Curcio E, Watkins C, Bacus S, Cora EM, Anderson E, Magill PJ. Phase II, randomized trial to compare anastrozole combined with gefitinib or placebo in postmenopausal women with hormone receptor-positive metastatic breast cancer. Clin Cancer Res. 2010;16:1904–1914. doi: 10.1158/1078-0432.CCR-09-2282. [DOI] [PubMed] [Google Scholar]
- 50.Baselga J, Campone M, Piccart M, Burris HA, 3rd, Rugo HS, Sahmoud T, Noguchi S, Gnant M, Pritchard KI, Lebrun F, Beck JT, Ito Y, Yardley D, Deleu I, Perez A, Bachelot T, Vittori L, Xu Z, Mukhopadhyay P, Lebwohl D, Hortobagyi GN. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366:520–529. doi: 10.1056/NEJMoa1109653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.National Cancer Institute at National Institutes of Health®, clinical trials search, www.Cancer.Gov/clinicaltrials/search
- 52.Legrier ME, Yang CP, Yan HG, Lopez-Barcons L, Keller SM, Perez-Soler R, Horwitz SB, McDaid HM. Targeting protein translation in human non small cell lung cancer via combined MEK and mammalian target of rapamycin suppression. Cancer Res. 2007;67:11300–11308. doi: 10.1158/0008-5472.CAN-07-0702. [DOI] [PubMed] [Google Scholar]
- 53.Carracedo A, Ma L, Teruya-Feldstein J, Rojo F, Salmena L, Alimonti A, Egia A, Sasaki AT, Thomas G, Kozma SC, Papa A, Nardella C, Cantley LC, Baselga J, Pandolfi PP. Inhibition of mTORC1 leads to MAPK pathway activation through a PI3K-dependent feedback loop in human cancer. J Clin Invest. 2008;118:3065–3074. doi: 10.1172/JCI34739. [DOI] [PMC free article] [PubMed] [Google Scholar]