Abstract
Background
The purpose of this study was to summarize published estimates for conversion from mild cognitive impairment or amnestic mild cognitive impairment to Alzheimer's dementia. We carried out a systematic review of English language publications to identify cohort studies published since January 2006 that reported the risk or rate of conversion.
Summary
Thirty-two cohort studies were identified, of which 14 reported annualized conversion rates (ACRs). Conversions over 1 year ranged from 10.2 to 33.6% (5 studies, median: 19.0%), and over 2 years from 9.8 to 36.3% (7 studies, median: 18.6%). ACRs ranged from 7.5 to 16.5% (7 studies, median: 11.0%) per person-year for studies recruiting from clinics, and from 5.4 to 11.5% (7 studies, median: 7.1%) for community samples.
Key Message
Extensive variation was observed in conversion rates due to the population sampled, diagnostic criteria, and duration, and because many studies did not account for loss to follow-up.
Key Words : Cognitive function, Alzheimer's dementia, Alzheimer's disease, Meta-analysis, Mild cognitive impairment
Introduction
Guidelines on defining preclinical Alzheimer's disease published by the National Institute on Aging (NIA) and the Alzheimer's Association in 2011 are based on decades of neuroimaging and pathological evidence indicating that neurobiological changes begin long before Alzheimer's dementia (AD) is diagnosed [1]. A reasonable expectation is that symptoms associated with these biological changes may present well before the onset of AD. However, potential indicators of early AD, such as memory loss and cognitive impairment, have proven to be difficult to distinguish from the decline associated with normal aging and cognitive impairment as a result of other etiologies [2].
Research to identify the clinical symptoms and risk factors for AD gave rise to the concept of mild cognitive impairment (MCI) to capture the predementia phase of cognitive impairment. More than a decade ago, Petersen et al. [3] published a definition of MCI which requires abnormal memory function relative to age and education, with preserved cognitive function and activities of daily living, in the absence of dementia. The term amnestic MCI (a-MCI) was recommended for individuals in the predementia phase prior to AD as a separate group from those with MCI preceding other forms of dementia [4]. However, these definitions are clinical, and no recommendations regarding which test and criteria were made. Therefore, other researchers have applied different diagnostic criteria to both MCI and a-MCI, and the standards for classifying patients as normal versus cognitively impaired have varied across studies [2,5,6,7,8,9].
Estimates of the risk for conversion to dementia from MCI or a-MCI have exhibited substantial variation; for example, a systematic review of cohort studies published before January 2002 estimated the annualized conversion rate (ACR) at approximately 10%, while a lower estimate of 7% was reported in a review of selected studies published before October 2008 with a mean duration of at least 3 years [8,9]. Although both reviews observed higher ACRs in the studies that recruited from memory clinics than from community-based samples, both the diagnostic criteria and the length of follow-up were noted to contribute to the substantial variation in the estimates. In 2003, a conference of international experts was convened which led to the publication of revised clinical criteria for categorizing cases diagnosed with MCI as a-MCI and non-a-MCI, and also for classification into two subtypes of single domain or multiple domains [10,11]. The purpose of this systematic review was to identify recent cohort studies (published since 2006) reporting on the risk or rate of conversion from MCI or a-MCI to AD.
Methods
A protocol was developed and followed for this review. Our methods adhered to the current practices for conducting systematic reviews of the literature. The data source was the literature published from January 1, 2006 to January 3, 2012. A literature search with both electronic and manual components was performed. MEDLINE (via PubMed) and Embase were searched to identify English language studies published within the last 6 years. The search strategies were developed and adapted for each database according to the appropriate index structures [e.g. Medical Subject Headings (MeSH) in MEDLINE and Emtree in Embase]. Combinations of search terms and key words for MCI, prodromal Alzheimer's disease, and disease progression were used in addition to terms related to the study design, including observational, longitudinal, retrospective, registry, population, cohort, and cross-sectional studies. Case reports, letters, commentaries, editorials, reviews, clinical trials, meta-analyses, practice guidelines, and in vitro studies were excluded from this review. The searches were limited to studies with human subjects published in the English language. A manual reference check of the bibliographies of the included studies was performed to supplement the electronic searches.
The citations and abstracts of all the studies identified in the searches were downloaded and the duplicates were removed. The studies selected for this review were based on two levels of screening. On the first level, the titles and abstracts of each citation were screened based on the inclusion and exclusion criteria outlined in the protocol. On the second level, the full text of each potentially relevant citation was screened by two independent reviewers to determine whether it met the criteria for inclusion in the review. Disagreements between the two reviewers were resolved by consensus.
Studies selected for this review met the following inclusion criteria: cohort or registry study, conversion to AD reported, a sample size of at least 100 patients with MCI or a-MCI at baseline, followed up for at least 12 months, and published in the English language between January 1, 2006 and January 3, 2012. Accepted studies describing the same patient population were identified by reviewing the method section, geographic location, sample size, author names, and institution name. The studies with the most complete data were used to avoid double counting.
Data were extracted to data forms developed for this review. Data extraction was performed by one researcher and reviewed by a second. Any discrepancies were resolved by consensus. Data extracted from each study included country, source of population (i.e. community, clinic, or other), cohort diagnosis criteria (i.e. MCI or a-MCI), demographics, and reported rate of conversion to AD.
The data extracted included (1) the proportion of patients with MCI or a-MCI that converted to AD over a specified follow-up period and (2) the ACRs to AD per 100 person-years or percent per person-year (%py). If the ACR was not reported by the authors, total person-time was estimated by multiplying the mean follow-up time by the number of patients with MCI or a-MCI at baseline. The number of cases of incident AD was divided by person-time to derive the ACR and reported as %py.
Results
Study Selection
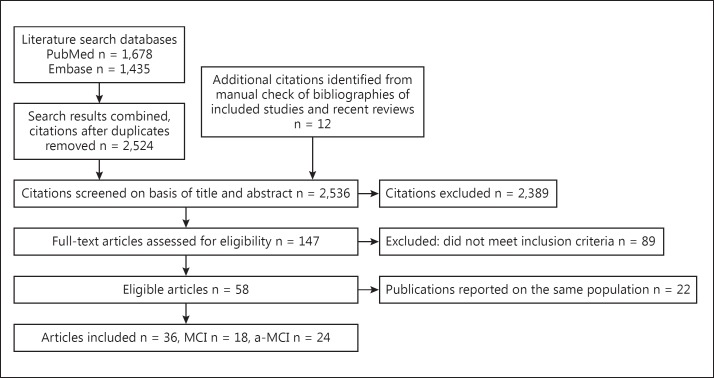
The titles and abstracts from 2,536 publications were screened, and the full texts of 135 studies were reviewed (fig. 1). Fifty-eight relevant publications met the eligibility criteria; however, 22 were determined to have reported on related study samples and were not included in the review. A total of 36 citations reporting data from 32 independent patient populations were identified for inclusion in this review [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. The data for two time intervals were obtained from separate publications on related populations from 4 studies that were conducted in France [35,39], Italy [37,42], the Netherlands [34,43], and the USA [22,33].
Fig. 1.
Selection of the relevant publications.
Study Characteristics
Data were reported on the conversion from MCI (18 studies) and a-MCI (24 studies). Studies were categorized as selecting a cohort with a-MCI at baseline when the authors indicated that memory impairment was part of the inclusion criteria. Nineteen cohort studies reported on AD conversion from MCI or a-MCI over a specified follow-up period (table 1), and 24 ACRs were obtained from 23 cohort studies (table 2). Fourteen ACRs were reported by the authors and an additional 10 were derived. Ten studies reported data over a fixed period as well as an ACR.
Table 1.
Cohort studies reporting conversion from MCI or a-MCI to AD over a specified follow-up period
| First author | Country | Age (mean ± SD)a, years | Sample size, n | AD conversion, % | Follow-up, years |
|---|---|---|---|---|---|
| MCI: clinic | |||||
| Rozzini [37] | Italy | N/R | 119 | 33.6 | 1 |
| Nordlund [30] | Sweden | 63.6 ± 7.7 | 205b | 9.8 | 2 |
| Vicini Chilovi [42] | Italy | 71 | 124b | 18.5 | 2 |
| Ramakers [34] | The Netherlands | 66.9 ± 7.7 | 263 | 18.6 | 2 |
| Devanand [18] | USA | N/R (41+) | 148 | 22.3 | 3 |
| Taragano [41] | Argentina | 72.3 ± 7.8 | 239c | 27.2 | 5 |
| MCI: community | |||||
| Fischer [19] | Austria | N/R (75) | 141 | 29.0 | 2.5 |
| Artero [12] | France | 74.6 ± 5.7 | 2,879b | 4.2 | 4 |
| Xu [46] | Sweden | N/R (75+) | 302 | 41.4 | 9 |
| a-MCI: clinic | |||||
| Babiloni [13] | Italy | 70.5 | 100 | 26.0 | 1 |
| Perri [32] | Italy | 70.3 | 269 | 19.0 | 1 |
| Robert [35] | France | 71.9 ± 5.4 | 216 | 10.2 | 1 |
| Petersen [33] | USA, Canada | 74.7 ± 7.4 | 398c | 16.1 | 1 |
| Xu [45] | China | N/R (45+) | 168 | 19.0 | 2 |
| Xu [44] | China | N/R (60+) | 176 | 17.6 | 2 |
| Perri [32] | Italy | 70.3 | 269 | 29.4 | 2 |
| Gomar [22] | USA, Canada | 75 | 320c | 36.3 | 2 |
| Sarazin [39] | France | 72 ± 5.4 | 223 | 26.5 | 3 |
| Gabryelewicz [21] | Poland | 69.3 | 105c | 18.1 | 3 |
| Palmer [31] | Italy | 70.8 ± 6.5 | 131c | 11.5 | 4 |
| Visser [43] | The Netherlands | 62.0 ± 11.5 | 119c | 37.8 | 5 |
| Ramakers [34] | The Netherlands | N/R (55+) | 110 | 55.5 | 10 |
| a-MCI: community | |||||
| Yu [47] | China | 74.2 | 216 | 16.2 | 3 |
| Li [26] | China | N/R (55+) | 837c | 35.6 | 5 |
| Ishikawa [24] | Japan | N/R (65+) | 104 | 10.6 | 5 |
| Xu [46] | Sweden | N/R (75+) | 120c | 47.5 | 9 |
Inclusion criteria provided when mean age was not reported.
Authors cross-reference to criteria published by Winblad et al. [10] for diagnostic criteria of MCI and a-MCI.
Table 2.
ACR from MCI or a-MCI to AD
| First author | Country | Age (mean ± SD)a, years | Sample size, n | AD conversion, % | Follow-up (mean), years | ACR, %pyb |
|---|---|---|---|---|---|---|
| MCI: clinic | ||||||
| Forti [20] | Italy | 75.7 ± 8.3 | 180c | 20.6 | 2.8 | 7.5d |
| Ramakers [34] | The Netherlands | 66.9 ± 7.7 | 263 | 18.6 | N/R | 11.0e |
| Devanand [18] | USA | N/R (41+) | 148 | 22.3 | N/R | 9.2d |
| Lopez [27] | USA | N/R | 136 | 41.9 | 4.3 | 9.7 |
| Rountree [36] | USA | N/R | 106f | 46.2 | 3.3 | 11.0e |
| MCI: community | ||||||
| Busse [16]g | Germany | N/R (75+) | 189f | 18.5 | 4.3 | 4.3 |
| Israeli-Korn [25] | Israel | 72.5 | 173 | 13.9 | 3.9 | 6.0e |
| Xu [46] | Sweden | N/R (75+) | 302 | 41.4 | 3.6 | 11.5d |
| Boyle [14] | USA | 82.8 ± 7.1 | 221 | 25.8 | 2.5 | 10.3 |
| Desikan [17] | USA | 72.4 | 129 | 34.1 | 6.2 | 5.5 |
| Manly [28] | USA | N/R (65+) | 564f | 21.8 | N/R | 5.4d |
| Smith [40] | USA | 72.3 ± 5.7 | 156 | 28.8 | 6.4 | 4.5 |
| a-MCI: clinic | ||||||
| Sarazin [39] | France | 72 ± 5.4 | 223 | 26.5 | 2.6 | 10.2 |
| Palmer [31] | Italy | 70.8 ± 6.5 | 131f | 11.5 | 1.4 | 8.2 |
| Mattsson [29] | Multinational (Europe) | N/Rh | 750 | 36.1 | N/R | 11.0e |
| Gabryelewicz [21] | Poland | 69.3 | 105f | 18.1 | 3.1 | 5.9 |
| Samaranch [38] | Spain | 73.8 ± 6.3 | 319f | 39.5 | 2.1 | 18.8 |
| Hertze [23] | Sweden | N/R | 166f | 33.1 | 4.7 | 7 |
| Buchhave [15] | Sweden | N/R | 147f | 42.9 | 5.2 | 11.6e |
| Petersen [33] | USA, Canada | 74.7 ± 7.4 | 398f | 16.1 | N/R | 16.5e |
| a-MCI: community | ||||||
| Li [26] | China | N/R (55+) | 837f | 35.6 | N/R | 7.1e |
| Yu [47] | China | 74.2 | 216 | 16.2 | N/R | 5.6d |
| Ishikawa [24] | Japan | N/R (65+) | 104 | 10.6 | N/R | 8.5d |
| Manly [28] | USA | N/R (65+) | 318f | 20.4 | N/R | 7.4d |
Inclusion criteria provided when mean age was not reported.
When not reported by authors, person-time and annual rate were calculated values using the reported mean follow-up period; values are derived unless otherwise specified.
Authors refer to Winblad et al. [10] for diagnostic criteria of MCI and a-MCI.
Reported by authors.
Reported by authors but not specified as n/person-years.
Different results reported according to different criteria among the same population; Petersen [11] criteria, SD 1.0 summarized in this table.
Age reported as median (range): 69 (43–89).
Most of the studies included in this review were conducted in the USA or in Europe, but there were also studies from China, Japan, Israel, and Argentina. The sample size was often less than 200 patients, and although the follow-up time varied from 1 to 10 years, most studies reported results of less than 5 years. The mean age reported ranged from 62 to 83 years. Some authors applied age restrictions (such as age ≥75 years); therefore, the inclusion criteria for the studies which did not report age are displayed in the tables.
The studies were categorized as recruiting a sample of participants from either a clinic-based or community population. In the clinic-based studies, the participants were recruited when they were referred for the evaluation of cognitive difficulties at a memory disorder clinic or to see a specialist. Community studies recruited volunteers living in the community by sampling electoral rolls or advertising.
AD Conversion over a Specified Follow-Up Period
Nineteen cohort studies reported on AD conversion from MCI or a-MCI over a specified follow-up period (table 1) [12,13,18,19,21,22,24,26,30,31,32,33,34,35,37,39,41,42,43,44,45,46,47]. A summary of these findings reported over each time period is provided for the clinic-based and community studies. The majority of these studies were conducted in a clinical setting. The sample size of half of the studies was under 190 cases, and most of the data were reported over a follow-up duration of 3 years or less. The mean age ranged from 62 to 75 years but was not always reported. The diagnostic criteria applied to select cases of MCI or a-MCI differed among researchers, but many referred to the criteria developed by Petersen et al. [3,4,5,11,33,48] or Winblad et al. [10] (table 1).
The AD conversion rate observed ranged from 10.2 to 33.6% over 1 year (5 studies, median: 19.0%) and from 9.8 to 36.3% over 2 years (7 studies, median: 18.6%). There were fewer studies over longer time horizons, and the AD conversion rate spanned 10.6-37.8% over 5 years. Most of the 7 studies reporting a time period of 5 or more years observed an AD conversion of over 33%. Over 10 years, the highest estimated conversion was 55.5% [34].
As follow-up times varied widely, additional comparisons are limited to where 3 or more studies conducted in the same setting report over comparable time frames. The incidence of AD observed in 4 studies recruiting patients with a-MCI from clinics ranged from 10.2% [35] to 26.0% [13] (median: 17.6%) over 1 year and from 17.6% [44] to 36.3% [22] (median: 24.2%) over 2 years. Three studies recruiting patients with MCI from clinics reported 9.8% [30] to 18.6% [34] over 2 years. These broad ranges illustrate how the estimates over comparable time intervals varied widely between studies. The estimates from community-based cohorts of MCI and a-MCI cases could not be compared given the small number of studies and differences in follow-up.
Three studies included in the review recruited patients with a-MCI from clinics and reported a conversion rate for two overlapping intervals. AD conversion in the Alzheimer's Disease Neuroimaging Initiative (ADNI) cohort was 16.1% [33] over 1 year and 36.3% over 2 years [22]. The ADNI study reported the highest 2-year conversion compared to other studies reporting over this specific time period. A cohort study in France recruited patients referred from memory clinics diagnosed with a-MCI at 14 centers and reported a conversion rate of 10.2% [35] over 1 year and of 26.5% [39] over 3 years. A study conducted at a single memory clinic in the Netherlands reported 37.8% converted over 5 years and 55.5% over 10 years.
AD ACR
A total of 23 cohort studies provided sufficient information to extract or derive an ACR (%py; table 2). The ACRs observed may have been impacted by the small sample size. The sample size of 4 of the studies was smaller than 147 cases, and half reported a mean follow-up time of less than approximately 3 years. The mean age (when reported) ranged from 67 to 76 years, but some studies used specific age inclusion criteria such as selecting patients 75 years and older. Although the diagnostic criteria developed by Petersen et al. [3,4,11,33,48,49] or Winblad et al. [10] for selecting cases of MCI or a-MCI were the most frequently cited, many studies did not refer to these criteria (table 2).
Table 3 provides an overview of these findings by showing the results of 14 ACRs reported by the authors alongside the data available when pooled with the estimates derived from the data reported. The rates in the 14 studies that reported an ACR ranged from 5.4%py [28] to 16.5%py [33] (median: 8.9%py). The lowest ACR (5.4%py) was reported in a community-based study conducted in the USA [28] and the highest (16.5%py) among participants recruited from clinics in the USA and Canada as part of the ADNI [33]. Six of these studies explicitly accounted for dropouts by calculating person-time [18,20,24,28,46,47], and these rates ranged from 5.4%py [28] to 11.5%py [46] (median: 8.0%py).
Table 3.
Summary of the ACRs (%py) from MCI or a-MCI to AD stratified by selected study characteristics
| Characteristic | ACR |
|||||
|---|---|---|---|---|---|---|
| author reported |
author reported or deriveda |
|||||
| k | range | median | k | range | median | |
| Population | ||||||
| Overall | 14 | 5.4–16.5 | 8.9 | 24 | 4.3–18.8 | 8.4 |
| MCI | 7 | 5.4–11.5 | 9.2 | 12 | 4.3–11.5 | 8.4 |
| a-MCI | 7 | 5.6–16.5 | 8.5 | 12 | 5.6–18.8 | 8.4 |
| Clinic | ||||||
| Overall | 7 | 7.5–16.5 | 11.0 | 13 | 5.9–18.8 | 10.2 |
| MCI | 4 | 7.5–11 | 10.1 | 5 | 7.5–11 | 9.7 |
| a-MCI | 3 | 11–16.5 | 11.6 | 8 | 5.9–18.8 | 10.6 |
| Community | ||||||
| Overall | 7 | 5.4–11.5 | 7.1 | 11 | 4.3–11.5 | 6.0 |
| MCI | 3 | 5.4–11.5 | 6.0 | 7 | 4.3–11.5 | 5.5 |
| a-MCI | 4 | 7.4–8.9 | 8.5 | 4 | 5.6–8.5 | 7.3 |
k = Number of studies.
Incident AD cases/person-time. If necessary estimated person-time = mean follow-up time × number of patients at baseline.
The ACR observed in 7 studies recruiting from clinics ranged from 7.5 to 16.5%py (median: 11.0%py) and in 7 cohorts of community samples from 5.4 to 11.5%py (median: 7.1%py; table 3). There was substantial variation in the ACR estimates observed in each setting. The ACR observed for participants diagnosed with MCI and a-MCI were compared within a single community-based study conducted by Manly et al. [28], and conversion rates were lower for MCI than a-MCI [5.4%py (95% CI: 4.7-6.3%py) vs. 7.4%py (95% CI: 5.7-9.2%py)]. The ranges overlap when the data reported across studies by MCI and a-MCI are stratified; however, once stratified by the sample source and diagnostic criteria, there was too much variation and too few studies in each category to determine whether the ACRs for the a-MCI clinic- and community-based studies were higher than for the respective MCI cohorts (table 3).
The published estimates were supplemented with values derived from the published data, thus increasing the number of studies; similar results were found after stratifying on the sample source and by MCI or a-MCI (table 3). Substantial differences were observed in the ACR estimates from each setting and cohort definition.
Discussion
This review summarizes the data available from 32 cohort studies reporting on conversion to AD. While a substantial number of studies have been published, a high degree of variation can be observed in the literature, which limits our ability to accurately summarize what may be the ‘true’ rate of conversion. The ACR ranged from 5.4 to 16.5%py (14 studies, median: 8.9%py). The estimates reported for AD conversion observed over 1 year ranged from approximately 10 to 33% (5 studies, range: 10.2-33.6%, median: 19.0%) and was similar over 2 years (7 studies, range: 9.8-36.3%, median: 18.6%) and 5 years (4 studies, range: 10.6-37.8%, median: 31.5%). Most of the 7 studies reporting over 5 or more years observed a conversion rate of over 33%.
Other researchers have observed that the conversion rate to AD from clinic-based populations may be higher than the conversion rates in the community [8,9,50]. After stratifying the studies included in this review by the sample source, the ACRs observed were often higher among participants recruited from memory clinics than from the community. The ACRs observed in studies which recruited from clinics ranged from 7.5 to 16.5%py (7 studies, median: 11.0%py) and from cohorts of community samples from 5.4 to 11.5%py (7 studies, median: 7.1%py). Patients attending memory clinics are assumed to be presenting due to a complaint by themselves or a family member and are thought to represent a later stage of cognitive impairment compared to individuals in community-based studies who volunteered to participate [9,50,51].
Overall, the wide ranges observed in the incidence of AD remain consistent with the findings of earlier literature reviews [8,9]. Bruscoli and Lovestone [9] included studies published between 1991 and 2001, and observed an ACR for dementia of 10.2%py (95% CI: 6.9-11.9%py) but ranged from a low of 2%py to slightly more than 30%py. Mitchell and Shiri-Feshki [8] selected a subset of studies published before October 2008 with a mean duration of at least 3 years, and reported an AD ACR of 6.5%py (95% CI: 4.8-8.5%py). They noted that higher rates of conversion were observed in the studies that recruited from clinics and also when studies applied the Petersen criteria for a-MCI [8,9]. In the current review, trends with a-MCI could not be evaluated across studies once the estimates were stratified by sample source and diagnostic criteria as there was too much variation in the ACR and either not enough studies in each category or too few studies reported over the same time period and setting.
Comparable challenges were highlighted when making comparisons between studies in the current review as in previous reviews. These challenges stem from variations in the sources of participants (clinic-based vs. community samples), diagnostic criteria employed, specific methods for implementation of the criteria, length of follow-up, and sample sizes. The impact of restriction of recruitment to subjects ≥65 or ≥75 years of age is also uncertain. Although some individual studies have observed lower ACRs among patients aged 65-69 years than among older subjects [28,47], this trend was not observed in the current or other reviews [9]. This extensive heterogeneity has been observed both in cohort studies and clinical trials, including, for example, 2 recent trials where the observed ACR was as low as 5% [52] and as high as 16% [8,53]. It was believed the lower rate may be due to (1) not applying age or education adjustments to memory test scores, and (2) using depression as an exclusion criterion, although this has since been recognized as common among patients with MCI. Many researchers have noted the difficulties created by the extensive heterogeneity across studies [8,9,10,54].
In longitudinal studies, the loss to follow-up for assessment may occur among individuals with cognitive impairment partially due to mortality, but also because the cognitive impairment often leads to them making changes in their living situations [8,55,56]. Studies of elderly populations with cognitive impairment are challenged by an increasingly high loss to follow-up over time. For example, in two 5-year studies included in this review, the study completion rates were 68.3 [24] and 77.1% [26]. While most patients diagnosed with MCI tend to remain stable (i.e. do not develop dementia) [57], some may revert to normal (2% [33] to 31% [28] depending on the MCI criteria used) or progress to AD. Patients with MCI who revert to normal should be excluded from the population at risk; however, although the studies based on the number enrolled at the study initiation would have included these in the estimation of conversion to AD, it is unclear how such cases were explicitly handled in the studies identified for this review. When studies report only the proportion of AD converters at the end of the specified follow-up periods based on the number initially enrolled, the conversion rate may be anticipated to be substantially different when at-risk time is considered. For these reasons, the argument can be made that the studies with AD incidence over 1 year, or 2 years at most, contained the most informative data for making summaries unless the studies were adjusted for loss to follow-up.
There was extensive variation in the follow-up periods from which results were reported. This was a major restriction in making cross-study comparisons of the studies that reported only the proportion of AD converters over specified follow-up periods. Other researchers have also noted that the proportion of patients diagnosed with MCI who convert to AD appears to decline with each passing year of follow-up, but this has not been confirmed in all studies [9,34]. An ACR was extracted for 14 studies included in this review, although only 6 studies had methods that explicitly reported that these estimates were based on cases of conversion to AD over total person-time. Where the ACR was not reported by the authors, mean follow-up was used to estimate total person-time, which allowed the derivation of an approximation for the rate of conversion from 10 additional studies. However, deriving these additional ACR estimates also introduced uncertainty into the values.
The variation in definitions of MCI or a-MCI and study inclusion and exclusion criteria may account for much of the variation in the reported rates of conversion [7,8,57]. Comparisons across studies ideally would take into consideration that the populations may be different; however, accounting for differences in diagnostic criteria is a challenge, as many studies have a unique operational definition. The differences are substantial; for example, while some studies diagnosed MCI based on assessment criteria such as the Clinical Dementia Rating (0.5 [17,25], or 0 or 0.5 [40]) or Global Deterioration Score (2 or 3 [34]), others diagnosed a-MCI after applying age or education adjustments to memory test scores. The lack of standardized research criteria for these diagnoses continues to create limitations for those attempting to review, summarize, and draw inferences from the body of published literature.
Another challenge exists when making comparisons among studies referencing similar criteria, as the investigators may have decided to use different tests or cutoff scores to make their diagnoses of MCI. Busse et al. [16] found that a wide range of conversion rates were being applied depending on which of 4 sets of criteria were used to diagnose MCI. For example, some investigators recommend applying the original Petersen criteria with a cutoff of 1.5 SD with cognitive test results from normal controls for high specificity and high positive predictive power of MCI progressing to AD, while others use modified criteria that do not require a subjective memory complaint and apply a cutoff of 1.0 SD with cognitive test results from normal controls for high sensitivity [16]. An essential element of the Petersen criteria is the requirement of memory impairment, which has been associated with increased rates of conversion [57] and may have a predictive value in progression to AD [16]. However, Lenehan et al. [6] noted that relying on a subjective memory complaint reduced the diagnostic accuracy of MCI progressing to AD. A discriminative, standardized definition of memory impairment may improve diagnostic accuracy. For example, a US clinic-based ADNI cohort (the design of the study protocol was led by Petersen) required age- and education-adjusted memory impairment for a diagnosis of a-MCI [58]. The studies of the ADNI cohort reported markedly high 1- and 2-year conversion rates compared with other studies in this review [22,33].
The AD diagnosis was confirmed in many studies by a small panel reviewing all the clinical diagnoses. Diagnostic misclassification of incident cases may have occurred as AD is still a clinical diagnosis; this has led to substantial differences in estimates of its incidence and prevalence [59,60,61], with the variation considered due to differences in the confirmation of an AD diagnosis [62,63]. The diagnosis of AD may be improved by including biomarkers as a diagnostic tool. This has shown promise and may improve the identification of individuals with minimal cognitive impairment who are likely to have AD and thus progress to frank AD. However, to date, biomarkers have not been accepted as diagnostic tools [54].
These relatively recently published studies continue to show extensive differences in the conversion rate from MCI or a-MCI to AD. Many factors may have contributed to the variation in conversion rates observed throughout the studies in this review, with a lack of standardization in diagnostic criteria and testing considered to be the factor with the most significant impact on the findings. The next important factor is the source of the patient population, i.e. whether they are from a clinic or the community. Though revised clinical criteria for categorizing cases diagnosed with MCI as amnestic were published in 2004, many of the studies did not refer to these criteria, and the implementation differed and was sometimes not described. The design of future studies could certainly be improved by taking into account loss to follow-up, consideration of any participants reverting to normal, and reporting the methods used to identify MCI or a-MCI cases in more detail. Researchers planning studies or forecasting the need for community-based services will have to continue to factor in the wide range of conversion rates observed.
Disclosure Statement
Alex Ward, Catherine Dye, and Sarah Tardiff were employees of United BioSource Corporation at the time of preparation of this article, and H. Michael Arrighi was an employee of Janssen Alzheimer Immunotherapy Research and Development LLC at the time this study was conducted.
Acknowledgements
This study was sponsored by Janssen Alzheimer Immunotherapy.
References
- 1.Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, Iwatsubo T, Jack CR, Jr, Kaye J, Montine TJ, Park DC, Reiman EM, Rowe CC, Siemers E, Stern Y, Yaffe K, Carrillo MC, Thies B, Morrison-Bogorad M, Wagster MV, Phelps CH. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alzheimer's Association 2012 Alzheimer's disease facts and figures. Alzheimers Dement. 2012;8:131–168. doi: 10.1016/j.jalz.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303–308. doi: 10.1001/archneur.56.3.303. [DOI] [PubMed] [Google Scholar]
- 4.Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV, Ritchie K, Rossor M, Thal L, Winblad B. Current concepts in mild cognitive impairment. Arch Neurol. 2001;58:1985–1992. doi: 10.1001/archneur.58.12.1985. [DOI] [PubMed] [Google Scholar]
- 5.Petersen RC, Morris JC. Mild cognitive impairment as a clinical entity and treatment target. Arch Neurol. 2005;62:1160–1163. doi: 10.1001/archneur.62.7.1160. discussion 1167. [DOI] [PubMed] [Google Scholar]
- 6.Lenehan ME, Klekociuk SZ, Summers MJ. Absence of a relationship between subjective memory complaint and objective memory impairment in mild cognitive impairment (MCI): is it time to abandon subjective memory complaint as an MCI diagnostic criterion? Int Psychogeriatr. 2012;24:1505–1514. doi: 10.1017/S1041610212000695. [DOI] [PubMed] [Google Scholar]
- 7.Trittschuh EH, Crane PK, Larson EB, Cholerton B, McCormick WC, McCurry SM, Bowen JD, Baker LD, Craft S. Effects of varying diagnostic criteria on prevalence of mild cognitive impairment in a community based sample. J Alzheimers Dis. 2011;25:163–173. doi: 10.3233/JAD-2011-101821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia – meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand. 2009;119:252–265. doi: 10.1111/j.1600-0447.2008.01326.x. [DOI] [PubMed] [Google Scholar]
- 9.Bruscoli M, Lovestone S. Is MCI really just early dementia? A systematic review of conversion studies. Int Psychogeriatr. 2004;16:129–140. doi: 10.1017/s1041610204000092. [DOI] [PubMed] [Google Scholar]
- 10.Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, Nordberg A, Backman L, Albert M, Almkvist O, Arai H, Basun H, Blennow K, de Leon M, DeCarli C, Erkinjuntti T, Giacobini E, Graff C, Hardy J, Jack C, Jorm A, Ritchie K, van Duijn C, Visser P, Petersen RC. Mild cognitive impairment – beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256:240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- 11.Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183–194. doi: 10.1111/j.1365-2796.2004.01388.x. [DOI] [PubMed] [Google Scholar]
- 12.Artero S, Ancelin ML, Portet F, Dupuy A, Berr C, Dartigues JF, Tzourio C, Rouaud O, Poncet M, Pasquier F, Auriacombe S, Touchon J, Ritchie K. Risk profiles for mild cognitive impairment and progression to dementia are gender specific. J Neurol Neurosurg Psychiatry. 2008;79:979–984. doi: 10.1136/jnnp.2007.136903. [DOI] [PubMed] [Google Scholar]
- 13.Babiloni C, Frisoni GB, Vecchio F, Lizio R, Pievani M, Cristina G, Fracassi C, Vernieri F, Rodriguez G, Nobili F, Ferri R, Rossini PM. Stability of clinical condition in mild cognitive impairment is related to cortical sources of alpha rhythms: an electroencephalographic study. Hum Brain Mapp. 2011;32:1916–1931. doi: 10.1002/hbm.21157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boyle PA, Wilson RS, Aggarwal NT, Tang Y, Bennett DA. Mild cognitive impairment: risk of Alzheimer disease and rate of cognitive decline. Neurology. 2006;67:441–445. doi: 10.1212/01.wnl.0000228244.10416.20. [DOI] [PubMed] [Google Scholar]
- 15.Buchhave P, Stomrud E, Warkentin S, Blennow K, Minthon L, Hansson O. Cube copying test in combination with rCBF or CSF A(beta)42 predicts development of Alzheimer's disease. Dement Geriatr Cogn Disord. 2008;25:544–552. doi: 10.1159/000137379. [DOI] [PubMed] [Google Scholar]
- 16.Busse A, Hensel A, Guhne U, Angermeyer MC, Riedel-Heller SG. Mild cognitive impairment: long-term course of four clinical subtypes. Neurology. 2006;67:2176–2185. doi: 10.1212/01.wnl.0000249117.23318.e1. [DOI] [PubMed] [Google Scholar]
- 17.Desikan RS, Cabral HJ, Fischl B, Guttmann CR, Blacker D, Hyman BT, Albert MS, Killiany RJ. Temporoparietal MR imaging measures of atrophy in subjects with mild cognitive impairment that predict subsequent diagnosis of Alzheimer disease. AJNR Am J Neuroradiol. 2009;30:532–538. doi: 10.3174/ajnr.A1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Devanand DP, Liu X, Tabert MH, Pradhaban G, Cuasay K, Bell K, de Leon MJ, Doty RL, Stern Y, Pelton GH. Combining early markers strongly predicts conversion from mild cognitive impairment to Alzheimer's disease. Biol Psychiatry. 2008;64:871–879. doi: 10.1016/j.biopsych.2008.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fischer P, Jungwirth S, Zehetmayer S, Weissgram S, Hoenigschnabl S, Gelpi E, Krampla W, Tragl KH. Conversion from subtypes of mild cognitive impairment to Alzheimer dementia. Neurology. 2007;68:288–291. doi: 10.1212/01.wnl.0000252358.03285.9d. [DOI] [PubMed] [Google Scholar]
- 20.Forti P, Maioli F, Pisacane N, Rietti E, Montesi F, Ravaglia G. Atrial fibrillation and risk of dementia in non-demented elderly subjects with and without mild cognitive impairment. Neurol Res. 2006;28:625–629. doi: 10.1179/016164106X130461. [DOI] [PubMed] [Google Scholar]
- 21.Gabryelewicz T, Styczynska M, Luczywek E, Barczak A, Pfeffer A, Androsiuk W, Chodakowska-Zebrowska M, Wasiak B, Peplonska B, Barcikowska M. The rate of conversion of mild cognitive impairment to dementia: predictive role of depression. Int J Geriatr Psychiatry. 2007;22:563–567. doi: 10.1002/gps.1716. [DOI] [PubMed] [Google Scholar]
- 22.Gomar JJ, Bobes-Bascaran MT, Conejero-Goldberg C, Davies P, Goldberg TE. Utility of combinations of biomarkers, cognitive markers, and risk factors to predict conversion from mild cognitive impairment to Alzheimer disease in patients in the Alzheimer's disease neuroimaging initiative. Arch Gen Psychiatry. 2011;68:961–969. doi: 10.1001/archgenpsychiatry.2011.96. [DOI] [PubMed] [Google Scholar]
- 23.Hertze J, Minthon L, Zetterberg H, Vanmechelen E, Blennow K, Hansson O. Evaluation of CSF biomarkers as predictors of Alzheimer's disease: a clinical follow-up study of 4.7 years. J Alzheimers Dis. 2010;21:1119–1128. doi: 10.3233/jad-2010-100207. [DOI] [PubMed] [Google Scholar]
- 24.Ishikawa T, Ikeda M. Mild cognitive impairment in a population-based epidemiological study. Psychogeriatrics. 2007;7:104–108. [Google Scholar]
- 25.Israeli-Korn SD, Massarwa M, Schechtman E, Strugatsky R, Avni S, Farrer LA, Friedland RP, Inzelberg R. Mild cognitive impairment is associated with mild parkinsonian signs in a door-to-door study. J Alzheimers Dis. 2010;22:1005–1013. doi: 10.3233/JAD-2010-101230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li J, Wang YJ, Zhang M, Xu ZQ, Gao CY, Fang CQ, Yan JC, Zhou HD. Vascular risk factors promote conversion from mild cognitive impairment to Alzheimer disease. Neurology. 2011;76:1485–1491. doi: 10.1212/WNL.0b013e318217e7a4. [DOI] [PubMed] [Google Scholar]
- 27.Lopez OL, Kuller LH, Becker JT, Dulberg C, Sweet RA, Gach HM, Dekosky ST. Incidence of dementia in mild cognitive impairment in the cardiovascular health study cognition study. Arch Neurol. 2007;64:416–420. doi: 10.1001/archneur.64.3.416. [DOI] [PubMed] [Google Scholar]
- 28.Manly JJ, Tang MX, Schupf N, Stern Y, Vonsattel JP, Mayeux R. Frequency and course of mild cognitive impairment in a multiethnic community. Ann Neurol. 2008;63:494–506. doi: 10.1002/ana.21326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mattsson N, Zetterberg H, Hansson O, Andreasen N, Parnetti L, Jonsson M, Herukka SK, van der Flier WM, Blankenstein MA, Ewers M, Rich K, Kaiser E, Verbeek M, Tsolaki M, Mulugeta E, Rosen E, Aarsland D, Jelle VP, Schröder J, Marcusson J, de Leon M, Hampel H, Scheltens P, Pirttila T, Wallin A, Jönhagin ME, Minthon L, Winblad B, Blennow K. CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA. 2009;302:385–393. doi: 10.1001/jama.2009.1064. [DOI] [PubMed] [Google Scholar]
- 30.Nordlund A, Rolstad S, Gothlin M, Edman A, Hansen S, Wallin A. Cognitive profiles of incipient dementia in the Goteborg MCI study. Dement Geriatr Cogn Disord. 2010;30:403–410. doi: 10.1159/000321352. [DOI] [PubMed] [Google Scholar]
- 31.Palmer K, Di Iulio F, Varsi AE, Gianni W, Sancesario G, Caltagirone C, Spalletta G. Neuropsychiatric predictors of progression from amnestic-mild cognitive impairment to Alzheimer's disease: the role of depression and apathy. J Alzheimers Dis. 2010;20:175–183. doi: 10.3233/JAD-2010-1352. [DOI] [PubMed] [Google Scholar]
- 32.Perri R, Serra L, Carlesimo GA, Caltagirone C. Preclinical dementia: an Italian multicentre study on amnestic mild cognitive impairment. Dement Geriatr Cogn Disord. 2007;23:289–300. doi: 10.1159/000100871. [DOI] [PubMed] [Google Scholar]
- 33.Petersen RC, Aisen PS, Beckett LA, Donohue MC, Gamst AC, Harvey DJ, Jack CR, Jr, Jagust WJ, Shaw LM, Toga AW, Trojanowski JQ, Weiner MW. Alzheimer's Disease Neuroimaging Initiative (ADNI): clinical characterization. Neurology. 2010;74:201–209. doi: 10.1212/WNL.0b013e3181cb3e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ramakers IH, Visser PJ, Aalten P, Kester A, Jolles J, Verhey FR. Affective symptoms as predictors of Alzheimer's disease in subjects with mild cognitive impairment: a 10-year follow-up study. Psychol Med. 2010;40:1193–1201. doi: 10.1017/S0033291709991577. [DOI] [PubMed] [Google Scholar]
- 35.Robert PH, Berr C, Volteau M, Bertogliati C, Benoit M, Sarazin M, Legrain S, Dubois B. Apathy in patients with mild cognitive impairment and the risk of developing dementia of Alzheimer's disease: a one-year follow-up study. Clin Neurol Neurosurg. 2006;108:733–736. doi: 10.1016/j.clineuro.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Rountree SD, Waring SC, Chan WC, Lupo PJ, Darby EJ, Doody RS. Importance of subtle amnestic and nonamnestic deficits in mild cognitive impairment: prognosis and conversion to dementia. Dement Geriatr Cogn Disord. 2007;24:476–482. doi: 10.1159/000110800. [DOI] [PubMed] [Google Scholar]
- 37.Rozzini L, Chilovi BV, Conti M, Bertoletti E, Delrio I, Trabucchi M, Padovani A. Conversion of amnestic mild cognitive impairment to dementia of Alzheimer type is independent to memory deterioration. Int J Geriatr Psychiatry. 2007;22:1217–1222. doi: 10.1002/gps.1816. [DOI] [PubMed] [Google Scholar]
- 38.Samaranch L, Cervantes S, Barabash A, Alonso A, Cabranes JA, Lamet I, Ancin I, Lorenzo E, Martinez-Lage P, Marcos A, Clarimon J, Alcolea D, Lleo A, Blesa R, Gomez-Isla T, Pastor P. The effect of MAPT H1 and APOE ε4 on transition from mild cognitive impairment to dementia. J Alzheimers Dis. 2010;22:1065–1071. doi: 10.3233/JAD-2010-101011. [DOI] [PubMed] [Google Scholar]
- 39.Sarazin M, Berr C, De Rotrou J, Fabrigoule C, Pasquier F, Legrain S, Michel B, Puel M, Volteau M, Touchon J, Verny M, Dubois B. Amnestic syndrome of the medial temporal type identifies prodromal AD: a longitudinal study. Neurology. 2007;69:1859–1867. doi: 10.1212/01.wnl.0000279336.36610.f7. [DOI] [PubMed] [Google Scholar]
- 40.Smith EE, Egorova S, Blacker D, Killiany RJ, Muzikansky A, Dickerson BC, Tanzi RE, Albert MS, Greenberg SM, Guttmann CR. Magnetic resonance imaging white matter hyperintensities and brain volume in the prediction of mild cognitive impairment and dementia. Arch Neurol. 2008;65:94–100. doi: 10.1001/archneurol.2007.23. [DOI] [PubMed] [Google Scholar]
- 41.Taragano FE, Allegri RF, Krupitzki H, Sarasola DR, Serrano CM, Lon L, Lyketsos CG. Mild behavioral impairment and risk of dementia: a prospective cohort study of 358 patients. J Clin Psychiatry. 2009;70:584–592. doi: 10.4088/jcp.08m04181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vicini Chilovi B, Conti M, Zanetti M, Mazzu I, Rozzini L, Padovani A. Differential impact of apathy and depression in the development of dementia in mild cognitive impairment patients. Dement Geriatr Cogn Disord. 2009;27:390–398. doi: 10.1159/000210045. [DOI] [PubMed] [Google Scholar]
- 43.Visser PJ, Verhey FR. Mild cognitive impairment as predictor for Alzheimer's disease in clinical practice: effect of age and diagnostic criteria. Psychol Med. 2008;38:113–122. doi: 10.1017/S0033291707000554. [DOI] [PubMed] [Google Scholar]
- 44.Xu G, Liu X, Yin Q, Zhu W, Zhang R, Fan X. Alcohol consumption and transition of mild cognitive impairment to dementia. Psychiatry Clin Neurosci. 2009;63:43–49. doi: 10.1111/j.1440-1819.2008.01904.x. [DOI] [PubMed] [Google Scholar]
- 45.Xu G, Zhou Z, Zhu W, Fan X, Liu X. Plasma C-reactive protein is related to cognitive deterioration and dementia in patients with mild cognitive impairment. J Neurol Sci. 2009;284:77–80. doi: 10.1016/j.jns.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 46.Xu W, Caracciolo B, Wang HX, Winblad B, Backman L, Qiu C, Fratiglioni L. Accelerated progression from mild cognitive impairment to dementia in people with diabetes. Diabetes. 2010;59:2928–2935. doi: 10.2337/db10-0539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yu BC, Tian JL, Ouyang LS, Wang YM, Wang CZ, Cui X, Wang XL, Qi LJ, Pan ZG, Wei SX, Gao Y. Incidence rate of mild cognitive impairment and the conversion rates into dementia or Alzheimer disease among elderly people: a population-based cohort study. Chin J Clin Rehabil. 2006;10:147–150. [Google Scholar]
- 48.Petersen RC, Smith GE, Waring SC, Ivnik RJ, Kokmen E, Tangelos EG. Aging, memory, and mild cognitive impairment. Int Psychogeriatr. 1997;9(suppl 1):65–69. doi: 10.1017/s1041610297004717. [DOI] [PubMed] [Google Scholar]
- 49.Petersen RC. Mild cognitive impairment clinical trials. Nat Rev Drug Discov. 2003;2:646–653. doi: 10.1038/nrd1155. [DOI] [PubMed] [Google Scholar]
- 50.Farias ST, Mungas D, Reed BR, Harvey D, DeCarli C. Progression of mild cognitive impairment to dementia in clinic- vs community-based cohorts. Arch Neurol. 2009;66:1151–1157. doi: 10.1001/archneurol.2009.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Petersen RC, Roberts RO, Knopman DS, Boeve BF, Geda YE, Ivnik RJ, Smith GE, Jack CR., Jr Mild cognitive impairment: ten years later. Arch Neurol. 2009;66:1447–1455. doi: 10.1001/archneurol.2009.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Feldman HH, Ferris S, Winblad B, Sfikas N, Mancione L, He Y, Tekin S, Burns A, Cummings J, del Ser T, Inzitari D, Orgogozo JM, Sauer H, Scheltens P, Scarpini E, Herrmann N, Farlow M, Potkin S, Charles HC, Fox NC, Lane R. Effect of rivastigmine on delay to diagnosis of Alzheimer's disease from mild cognitive impairment: the InDDEx study. Lancet Neurol. 2007;6:501–512. doi: 10.1016/S1474-4422(07)70109-6. [DOI] [PubMed] [Google Scholar]
- 53.Fleisher AS, Sowell BB, Taylor C, Gamst AC, Petersen RC, Thal LJ. Clinical predictors of progression to Alzheimer disease in amnestic mild cognitive impairment. Neurology. 2007;68:1588–1595. doi: 10.1212/01.wnl.0000258542.58725.4c. [DOI] [PubMed] [Google Scholar]
- 54.Weiner MW, Veitch DP, Aisen PS, Beckett LA, Cairns NJ, Green RC, Harvey D, Jack CR, Jagust W, Liu E, Morris JC, Petersen RC, Saykin AJ, Schmidt ME, Shaw L, Siuciak JA, Soares H, Toga AW, Trojanowski JQ, Alzheimer's Disease Neuroimaging Initiative The Alzheimer's Disease Neuroimaging Initiative: a review of papers published since its inception. Alzheimers Dement. 2012;8:S1–S68. doi: 10.1016/j.jalz.2011.09.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J Clin Epidemiol. 2005;58:13–19. doi: 10.1016/j.jclinepi.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 56.Matthews FE, Chatfield M, Freeman C, McCracken C, Brayne C, MRC CFAS. Attrition and bias in the MRC cognitive function and ageing study: an epidemiological investigation. BMC Public Health. 2004;4:12. doi: 10.1186/1471-2458-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ganguli M, Snitz BE, Saxton JA, Chang CC, Lee CW, Vander Bilt J, Hughes TF, Loewenstein DA, Unverzagt FW, Petersen RC. Outcomes of mild cognitive impairment by definition: a population study. Arch Neurol. 2011;68:761–767. doi: 10.1001/archneurol.2011.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Peterson RC.Alzheimer's Disease Neuroimaging (ADNI) protocol (protocol principal investigator: Ronald C. Peterson). Bethesda, National Institutes of Health, 2005, final protocol: March 2, 2005; amendment No. 1 – LP extension: October 30, 2007; amendment No. 2 – extended follow-up: September 19, 2008.
- 59.Brookmeyer R, Johnson E, Ziegler-Graham K, Arrighi HM. Forecasting the global burden of Alzheimer's disease. Alzheimers Dement. 2007;3:186–191. doi: 10.1016/j.jalz.2007.04.381. [DOI] [PubMed] [Google Scholar]
- 60.Jorm AF, Jolley D. The incidence of dementia: a meta-analysis. Neurology. 1998;51:728–733. doi: 10.1212/wnl.51.3.728. [DOI] [PubMed] [Google Scholar]
- 61.Ziegler-Graham K, Brookmeyer R, Johnson E, Arrighi HM. Worldwide variation in the doubling time of Alzheimer's disease incidence rates. Alzheimers Dement. 2008;4:316–323. doi: 10.1016/j.jalz.2008.05.2479. [DOI] [PubMed] [Google Scholar]
- 62.Brookmeyer R, Evans DA, Hebert L, Langa KM, Heeringa SG, Plassman BL, Kukull WA. National estimates of the prevalence of Alzheimer's disease in the United States. Alzheimers Dement. 2011;7:61–73. doi: 10.1016/j.jalz.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Corrada M, Brookmeyer R, Kawas C. Sources of variability in prevalence rates of Alzheimer's disease. Int J Epidemiol. 1995;24:1000–1005. doi: 10.1093/ije/24.5.1000. [DOI] [PubMed] [Google Scholar]
- 64.Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]