Abstract
Patient: Male, 20
Final Diagnosis: Sickle cell anemia
Symptoms: Bone marrow necrosis • bone pain • fever • hepatomegaly • icterus • splenomegaly • weakness
Medication: —
Clinical Procedure: —
Specialty: Hematology
Objective:
Unusual clinical course
Background:
In sickle cell disease, bone involvement is the commonest clinical presentation in the acute as well as chronic setting presenting as painful vaso-occlusive crisis and avascular necrosis, respectively. Other complications include bone marrow necrosis and infarction.
Case Report:
We report a case of a 20-year-old male who was referred for bone marrow evaluation due to symptoms of fever, weakness, and repeated episodes of bone pains. Bone trephine biopsy revealed multiple areas of central necrosis surrounded by fibroblasts.
Conclusions:
Recognition of necrosis through bone trephine biopsy is important for early initiation of therapy.
Keywords: sickle cell, necrosis, bone marrow
Background
Bone marrow necrosis resulting from impairment of blood supply is often seen in patients with leukemia, malignancy, and haemoglobinopathies (eg, sickle cell disease) in association with a hypercellular bone marrow. Causes such as malignancy comprise 90% of the cases of bone marrow necrosis. Necrosis due to sickle cell disease makes up 2% of all cases. Cases reported previously in literature are scarce because physicians do not routinely perform bone marrow procedure in sickle cell patients. We report a case of a 20-year-old male who was referred for bone marrow evaluation due to symptoms of fever, weakness, and bone pains.
Case Report
We received a request for evaluation of bone marrow and trephine biopsy of a 20-years-old male who was referred for evaluation of fever, weakness, and bone pains that began 3–4 months before. The referring physician’s clinical diagnosis was myelofibrosis. The patient had a history of repeated episodes of bone pains which subsided after taking Tramadol and Nuberol Forte. However, he was not investigated previously. Family history was not significant.
General physical examination revealed pallor and icterus. In systemic examination there was hepatosplenomegaly. Complete blood counts showed Hb: 6.7 G/DL, Hct: 20.5%, MCV: 99.3 FL, MCH: 32.2 PG, WBC: 5.8×109/L, and platelets: 114×109/L. Peripheral film review showed presence of numerous sickle cells, polychromasia, nucleated red blood cells, and target cells (Figure 1). On the basis of peripheral film findings, complimentary haemoglobin electrophoresis was done, which revealed: A2: 2.5%, F: 33.6% and S: 63.9%.
Figure 1.
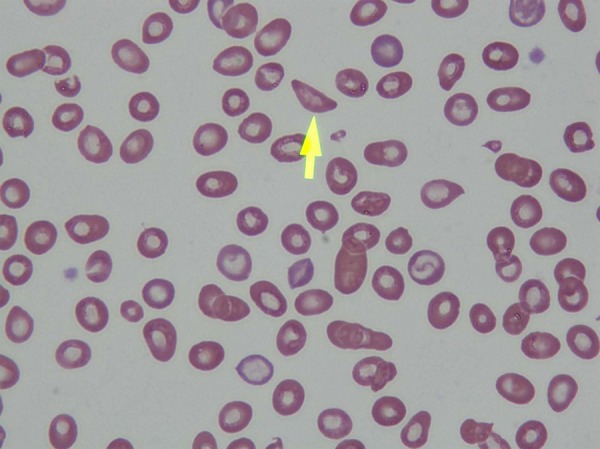
Peripheral Blood film showing sickle cells at 100×.
Subsequently, bone marrow was performed. There was presence of erythroid hyperplasia with dyserythropoietic changes and many sickle cells in the background (Figure 2). Bone trephine, however, revealed increased cellularity, mainly consisting of erythroid hyperplasia along with patch of haemopoietic tissue showing multiple areas of central necrosis surrounded by fibroblasts (Figures 3 and 4). Therefore, the repeated painful episodes were indicated a sickle cell crises eventually leading to bone marrow necrosis.
Figure 2.
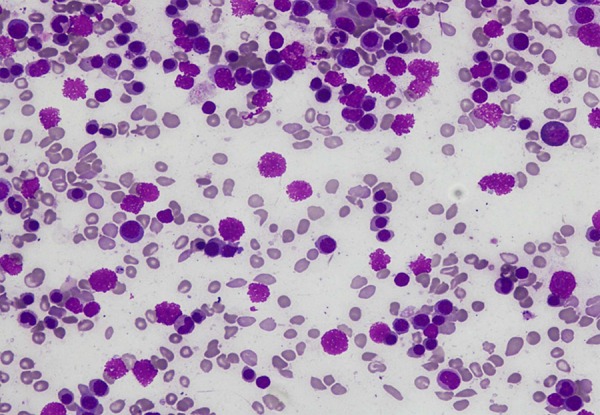
Bone marrow aspirate at 40× showing erythroid hyperplasia.
Figure 3.
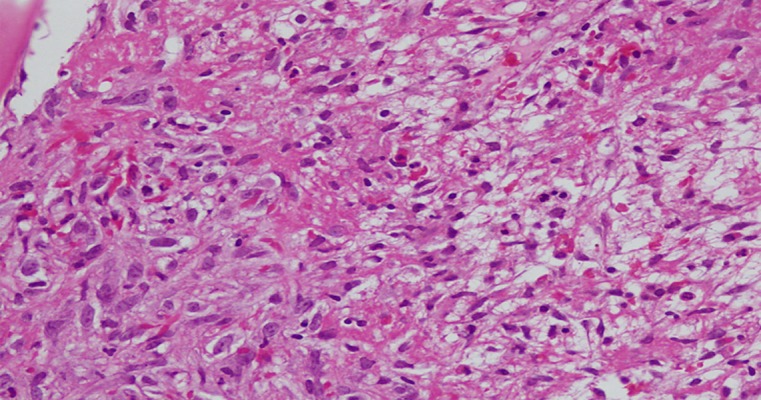
Area of central necrosis surrounded by fibroblasts at 40×.
Figure 4.
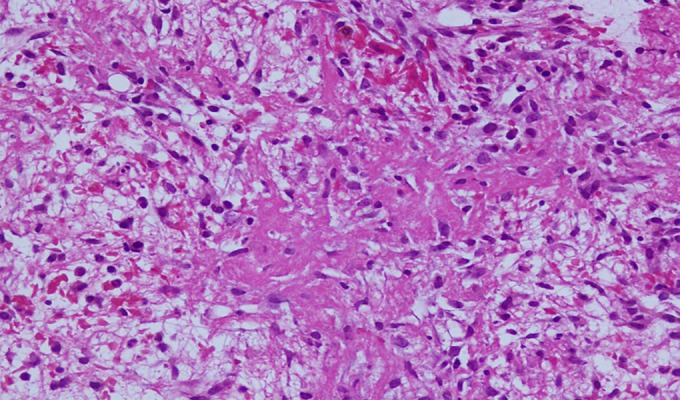
Bone trephine section showing necrosis at 20×.
Discussion
There are numerous consequences of sickle cell disease; the most characteristic is injury to the skeletal system. Bone marrow necrosis, infarction, osteomyelitis, and avascular necrosis are most frequent complications [1]. Descriptions of bone marrow necrosis in patients with sickle cell anemia are scarce since because physicians do not routinely perform bone marrow procedures in painful crisis. However, few cases with similar findings have been reported by Godeau B et al. [2]. A report by Ranaghan L et al. in 1994, mentioned that 133 cases of bone marrow necrosis had been reported, the most common causes being acute and chronic leukemia, carcinoma, malignant lymphoma, infections, and sickle cell disease [3].
Necrosis may range from localized, as seen in our patient, to widespread process. Recognition of the pathology is important, as early institution of transfusion therapy can be life-saving [4]. Bone marrow biopsy is necessary for the diagnosis of necrosis, as in our patient.
Conclusions
Bone marrow necrosis should be recognized through bone trephine biopsy for early institution of therapy.
References:
- 1.Smith JA. Bone disorders in sickle cell disease. Hematol Oncol Clin North Am. 1996;10:1345–56. doi: 10.1016/s0889-8588(05)70405-6. [DOI] [PubMed] [Google Scholar]
- 2.Godeau B, Bachir D, Randrianjohanny A, et al. Extensive bone marrow necrosis and major sickle cell syndromes. Rev Med Interne. 1994;15(1):25–29. doi: 10.1016/s0248-8663(05)82126-5. [DOI] [PubMed] [Google Scholar]
- 3.Ranaghan L, Morris TC, Desai ZR, Markey GM. Bone marrow necrosis. Am J Hematol. 1994;47(3):225–28. doi: 10.1002/ajh.2830470314. [DOI] [PubMed] [Google Scholar]
- 4.Ataga KI, Orringer EP. Bone marrow necrosis in sickle cell disease: a description of three cases and a review of the literature. Am J Med Sci. 2000;320(5):342–47. doi: 10.1097/00000441-200011000-00009. [DOI] [PubMed] [Google Scholar]


