Abstract
There is still controversy as to whether minimally invasive total hip arthroplasty enhances the postoperative outcome. The aim of this study was to compare the outcome of patients who underwent total hip replacement through an anterolateral minimally invasive (MIS) or a conventional lateral approach (CON). We performed a randomized, prospective study of 75 patients with primary hip arthritis, who underwent hip replacement through the MIS (n=36) or CON (n=39) approach. The Western Ontario and McMaster Universities Osteoarthritis Index and Harris Hip score (HHS) were evaluated at frequent intervals during the early postoperative follow-up period and then after 3.5 years. Pain sensations were recorded. Serological and radiological analyses were performed. In the MIS group the patients had smaller skin incisions and there was a significantly lower rate of patients with a positive Trendelenburg sign after six weeks postoperatively. After six weeks the HHS was 6.85 points higher in the MIS group (P=0.045). But calculating the mean difference between the baseline and the six weeks HHS we evaluated no significant differences. Blood loss was greater and the duration of surgery was longer in the MIS group. The other parameters, especially after the twelfth week, did not differ significantly. Radiographs showed the inclination of the acetabular component to be significantly higher in the MIS group, but on average it was within the same permitted tolerance range as in the CON group. Both approaches are adequate for hip replacement. Given the data, there appears to be no significant long term advantage to the MIS approach, as described in this study.
Key words: minimally invasive, hip arthroplasty, hip approach
Introduction
Minimally invasive total hip arthroplasty is claimed to be superior to the standard technique because it reduces operative, respectively soft tissue trauma. There is still controversy, however, as to whether minimally invasive total hip arthroplasty enhances the postoperative outcome. The benefits most often described in connection with minimally invasive hip surgery (MIS) are reduced perioperative pain and less blood loss and recovery time combined with shorter skin incisions.1-3 On the other hand, other groups report a higher complication rate and worse cosmetic results.4,5 In the light of current scientific knowledge it is not possible to decide if MIS is superior to the well established approaches.3
In 2004 Bertin and Röttinger described an anterolateral minimally invasive approach which comes close to the conventional Watson-Jones approach.1,6 In a prospective one-year follow-up study Martin et al. found that the anterolateral minimally invasive approach had no significant advantages in comparison to a conventional Hardinge approach, with the exception of reduced blood loss.7 Two further studies on the anterolateral minimally invasive approach with a short follow-up and small patient groups revealed better early functional hip scores.8,9
The aim of this prospective randomized study was to conduct a comprehensive comparison, based on a 3.5-year follow-up, of patients who underwent total hip replacement either by the anterolateral minimally invasive approach by Bertin or by a conventional lateral approach. We were particularly interested in differences with respect to the operative load of the patients and the postoperative rehabilitation. In the course of the investigation, various periand postoperative data were analyzed for detailed evaluation of the follow-up results achieved by the two approaches. This is of even greater interest, as some authors observed advantages of the MIS approach only in the early postoperative follow-up period.8,10
Materials and Methods
Patients
Approval was obtained from the local Ethics Committee (application number 06-3079). 250 consecutive patients who underwent total hip arthroplasty at the Department of Orthopaedics at the University of Duisburg-Essen between September 2006 and May 2008 were evaluated for inclusion in this study. Only patients aged between 65 and 75 years with unilateral osteoarthritis and an ASA (American Society of Anaesthesiologists) grade less than or equal to 3 were included. Exclusion criteria included a body-mass index (BMI) of over 30 kg/m2, secondary arthritis, replacement and osteoarthritis of other joints of the lower limbs, if patients had a special request for one of the two approaches and serious medical co-morbidities such as cancer. 76 met the inclusion criteria and agreed to participate in the study. Using computer-generated cards, patients were randomly allocated to either Bertin’s MIS anterolateral approach (MIS-group; n=36) or conventional lateral approach (CON-group; n=40). The observers were blinded and were not involved in the surgery. The medical history of all patients was documented, including age, gender and associated risk factors. Furthermore, the BMI and ASA grade were determined (Table 1).
Table 1.
Preoperative characteristics. The values are given as the mean ± the standard deviation.
| All patients | Patients with a complete set of data for early and long-term follow-up | |||||
|---|---|---|---|---|---|---|
| MIS | CON | P | MIS | CON | P | |
| Sex (F:M) | 24:12 | 26:14 | 1.000 | 18:1018:10 | 22:10 | 0.787 |
| Side (R:L) | 17:19 | 19:21 | 1.000 | 13:15 | 15:17 | 1.000 |
| Age (y) | 70.26±4.05 | 71.03±5.38 | 0.480 | 69.85±3.87 | 70.53±5.39 | 0.622 |
| Weight (kg) | 76.38±12.09 | 73.25±11.46 | 0.270 | 76.59±10.43 | 71.68±11.15 | 0.089 |
| Height (cm) | 167.74±7.88 | 165.50±8.18 | 0.248 | 168.00±7.00 | 165.71±8.91 | 0.278 |
| BMI (kg/m2) | 27.03±2.82 | 26.76±3.83 | 0.731 | 27.08±2.86 | 26.12±3.67 | 0.269 |
| ASA (1:2:3 %) | 2.77:91.67:5.56 | 0:90.0:10.0N | 0.451 | 3.79:92.42:3.79 | 0:93.75:6.25 | 0.507 |
MIS, minimally invasive hip surgery; CON, conventional lateral approach; BMI, body mas index; ASA, American Society of Anaesthesiologists.
Surgical techniques and evaluation of intraoperative data
All surgeries were performed by three experienced hip surgeons. A digitalized planning tool (mediCad®, HECTEC™ GmbH, Landshut, Germany) was used for preoperative planning. All patients underwent general anaesthesia and received a single-shot antibiotic prophylaxis (Cefazolin 2 g) before incision. The patients in the MIS group were positioned on the operating table in the lateral position and the surgical procedure was performed as described by Bertin and Röttinger.1 In the conventional approach group the patients were placed in the supine position and a modified Bauer respectively Hardinge approach was performed according to Thomine.11
All patients received a pressfit acetabular component. As the Trident® cup (Stryker™, 325 Corporate Drive, Mahwah, New Jersey 07430, United States), which was used for the first 64 patients, was temporarily taken off the market in January 2008, eight patients of the CON and three patients of the MIS group received a Duraloc® cup (DePuy Orthopaedics Inc.™, 700 Orthopaedic Drive, Warsaw, IN 46582, United States). A cemented Exeter® stem (Stryker™, 325 Corporate Drive, Mahwah, New Jersey 07430, United States) was implanted in all cases. The head diameter was 28 mm and the bearing surfaces were metal on highly cross-linked polyethylene. For auto-transfusion of blood we used the Cell Saver® (Haemonetics S.A. Signy Centre Rue des Flecheres P.O. Box 262, 1274 SIGNY Centre Switzerland) for all patients. We evaluated the blood volume returned to the patient after preparation both during surgery and for a further six hours after surgery by the Cell Saver® and, as appropriate, any administered allogenic blood products. Further data collected intraoperatively included the surgical procedure, the surgeon, the duration of the operation, the length of the incision, the prosthesis components implanted and their size, and any complications during surgery.
Postoperative treatment and follow-up
Appropriate prophylaxis for thromboembolism (enoxaparine) was administered for six weeks. Sensation of pain was recorded according to visual analogue scale ranging from 0-10 (0 = no pain and 10 = worst pain imaginable), before taking analgesics in the morning. Every patient received ibuprofen 600 mg three times daily for 14 days. The daily equianalgetic dose of the analgesics administered in addition to ibuprofen was calculated according to the pain-relieving efficacy equivalent to 10 mg of morphine.12
Standardized physical therapy was commenced on the first postoperative day. Patients were mobilized with two crutches and full weight-bearing was allowed, depending on the individual level of pain.
The recorded laboratory parameters included the haemoglobin level (Hb), hematocrit, the CK-NAC and C-reactive protein (CRP). The haemoglobin level was determined preoperatively, then 2, 4 and 6 hours after surgery and on the 1st, 2nd, 5th and 10th post-operative days. All other laboratory values were verified preoperatively, 6 hours postoperatively and on the 1st, 2nd, 5th, and 10th postoperative day.
A total of four physical examinations were performed on each patient, preoperatively and then on the 12th, 42nd and 84th postoperative days and 3.5 years after surgery. During each visit, the Trendelenburg sign, Harris hip score (HHS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) were determined.
Radiographs
We used preoperative and 12-day postoperative digitalized radiographs with an anteroposterior view of the pelvis centered over the pubic symphysis and ensured proper positioning of the pelvis.13 For the templating and measurements we used a digital image analysis system (mediCad II, HecTec GmbH, Niederviehbach, Germany). The limb length was then evaluated by measuring the perpendicular distance (mm) between the teardrop and the lesser trochanter (Figure 1). The position of the inserted total hip replacement was determined: Widmer’s and McLaren’s methods were used to evaluate the cup inclination respectively anteversion (Figure 1).14,15 To determine the precision of stem positioning we measured the angle between the axis of the bony femoral shaft and the implanted stem (Figure 1). The quality of the cement mantle was assessed by the method described by Mulroy et al. respectively Barrack et al.16,17
Figure 1.
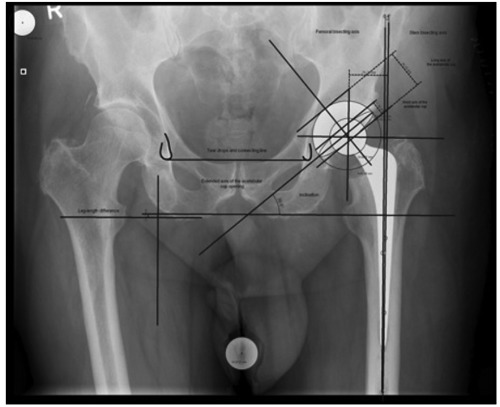
The limb length was evaluated by measuring the perpendicular distance (mm) between the teardrop and the lesser trochanter. The difference between the left and right side constituted the leg length difference. For evaluation of the cup inclination we measured the angle between the teardrop line and the long axis of the ellipse, which presents itself as the acetabular opening on the radiograph. The anteversion of the cup was calculated as inverse sine function of the ratio of short to the long axis of the acetabular cup. To determine the precision of stem positioning, the angle between the axis of the bony femoral shaft and the implanted stem was measured.
Statistical analysis
Summary statistics of the data were expressed as mean ± SD. The confirmatory Satterthwaite t-test for two independent samples was used, for evaluation of the primary endpoint, the change of the postoperative HHS in comparison to preoperative HHS. The confirmatory dichotomous Trendelenburg sign was evaluated with Fischer’s exact test between the two groups. In addition, the U-test (Wilcoxon-Mann-Whitney test) was applied for comparison of the secondary endpoints, depending on the type of scale. For large groups, the P-values according to Bonferroni-Holm were adjusted to keep the proportion of false-positive test results low. The exact Chi-Square-Test and the exact Cochrane-Armitage-Test were used for statistical evaluation of the cement mantle quality. Comparisons with Pvalues <0.05 were considered to be significant. The software SAS 9.2 TS1M0, (SAS Institute Inc., 100 SAS Campus Drive, Cary, NC 27513-2414, USA) was used to carry out the statistical computations.
Results
Patient demographics
The evaluated demographics were homogeneous in both groups (Table 1). The patients were in good general condition, but slightly overweight. One patient of the CON-group was excluded from the study after randomization, because of an unexpected preoperative serious illness and postponement of surgery. The other patients were available for evaluation of the cumulative dose and type of analgesic medications, pain sensation and intraoperative and early post-operative serological and radiographic data. The intraoperative and early post-operative complication rate refers to these patients. Five patients died during the first 3.5 years after surgery. The causes of death were not related to the hip replacement procedure. Ten further patients were not available for all clinical follow-up examinations. Overall, we obtained a complete set of clinical follow-up data for 60 patients. The demographics for these 60 patients were also homogeneous (Table 1).
Intraoperative results
Comparison of surgical data revealed that the MIS group had significantly shorter incisions (10.29±0.86 vs. 11.72±1.69 cm; P=0.0015). The blood loss, evaluated by measuring the red blood volume prepared by the cell-saver, was significantly higher in the MIS group (268.73±178.56 vs. 183.40±82.60; P=0.034) and the duration of surgery was longer (93.64±19.46 vs. 85.11±21.85; P=0.027). With the exception of one greater trochanter fracture in the MIS group, no complications were observed. Consequently, there were no significant differences between the two groups regarding complications (P=0.4853). The difference in risk was 3.03%. The mean acetabular cup size did not differ significantly (MIS 52.48±3.54 vs. CON 51.38±2.53; P=0.142). Furthermore, there were no significant differences regarding the stem size (P=0.129) and stem offset (P=0.181). The most frequently used Exeter stem was the 44 mm Offset option in both groups with a mean stem size of 1.31±1.09 (MIS) respectively 0.95±0.85 (CON).
Clinical outcome and follow-up
Postoperatively, we observed one non-surgery-related and two surgery-related complications in each group (MIS: 5.56% respectively 2.77% vs. CON 5.13% respectively 2.56%). Two patients in the MIS group and one patient in the CON group had prolonged wound-healing. The second patient in the CON group had a transient peroneal nerve palsy on the operated side for six months. The non-surgical complications were an idiopathic transient exanthema of the neck and an opticus neuropathy with scotoma. All complications disappeared after a short time of at most six months. In the further course of the long-term follow-up no further complications were observed.
The average daily analgesic consumption during the hospitalisation time, based on painrelieving efficacy equivalent to 10 mg of morphine, was nearly identical (MIS 5.113±1.283 mg/d vs. CON 4.554±1.327 mg/d; P=0.189) and the daily-evaluated pain sensations did not differ significantly between the groups at any time (Figure 2), nor did the mean (MIS 2.46±1.52 vs. CON 2.68±1.68; P=0.642) or median (MIS 2.17±1.64 vs. CON 2.30±1.96; P=0.823) values. Detailed results of the serological analyses are given in Table 2.
Figure 2.
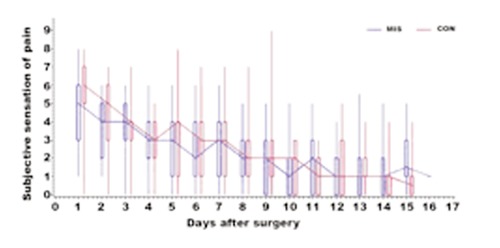
There were no significant differences between the groups at any time regarding the dai-ly or the mean values for pain sensation. The whiskers represent the 5% and 95% percentile. The con-necting lines pass through the medians.
Table 2.
The pre- and postoperative results of hemoglobin and hematocrit did not dif-fer significantly. Patients of both groups had a decrease in haemoglobin after surgery, starting from an almost equal basic level of 13.85 g/L (MIS) respectively 13.90 (CON). After the fifth postoperative day the level increased in both groups. The CK-NAC and CRP values showed significant differences on the 1st and 2nd postoperative days for CRP. However, the significance was lost after the results were adjusted for large groups. The mean CRP value reached its highest levels on the 2nd postoperative day and by the 10th postoperative day had fallen to the preoperative starting value. The mean values of CK-NAC reached their highest levels six hours postoperatively and fell by the 10th postoperative day to the preoperative starting value.
| Timing | MIS | CON Hemoglobin | P | MIS | CON Hematocrit | P |
|---|---|---|---|---|---|---|
| Preoperative | 13.85±1.16 | 13.93±1.34 | 0.9109 | 0.39±0.07 | 0.40±0.04 | 0.06485 |
| 2h postoperative | 12.45±1.53 | 11.90±1.58 | 0.3370 | |||
| 4h postoperative | 11.51±1.54 | 12.18±1.18 | 0.1491 | |||
| 6h postoperative | 12.11±1.34 | 12.07±1.34 | 0.9947 | 0.35±0.04 | 0.35±0.04 | 0.7107 |
| 1d postoperative | 11.38±1.48 | 11.33±1.46 | 0.5761 | 0.33±0.04 | 0.33±0.04 | 0.7128 |
| 2d postoperative | 11.25±1.35 | 10.80±1.47 | 0.1656 | 0.33±0.04 | 0.31±0.04 | 0.2358 |
| 5d postoperative | 10.76±1.07 | 10.35±1.44 | 0.2683 | 0.31±0.03 | 0.30±0.04 | 0.1758 |
| 10d postoperative | 11.13±1.19 | 10.67±1.33 | 0.0944 | 0.33±0.03 | 0.31±0.04 | 0.0592 |
| CK-NAC | CRP | |||||
| Preoperative | 94.84±49.81 | 120.46±115.66 | 0.4717 | 0.58±1.86 | 0.32±0.31 | 0.8522 |
| 6h postoperative | 625.10±263.96 | 561.45±319.85 | 0.2435 | 0.96±0.49 | 0.88±0.39 | 0.7286 |
| 1d postoperative | 521.93±211.02 | 469.64±217.60 | 0.1919 | 9.94±4.38 | 12.43±4.18 | 0.0231 |
| 2d postoperative | 381.29±183.14 | 359.61±152.24 | 0.7408 | 17.15±6.81 | 21.07±5.47 | 0.0224 |
| 5d postoperative | 178.16±103.70 | 161.35±85.50 | 0.6317 | 8.51±6.21 | 7.90±3.69 | 0.8951 |
| 10d postoperative | 81.20±47.38 | 79.49±47.65 | 0.8332 | 2.29±2.76 | 2.25±1.20 | 0.1129 |
| Preoperative | 94.84±49.81 | 120.46±115.66 | 0.4717 | 0.58±1.86 | 0.32±0.31 | 0.8522 |
MIS, minimally invasive hip surgery; CON, conventional lateral approach; CRP, C-reactive protein.
The clinical follow-up results (Table 3) concern the 60 patients with a complete data set. The results of all collected data were almost identical (data not shown). The preoperative HHS created the baseline for each group, which was 3.1 points higher in the MIS group (P=0.374). After six weeks this difference increased to 6.85 points and became significant (P=0.045). But calculating the mean difference between the baseline and the six weeks HHS (primary endpoint) we evaluated no significant differences between the MIS and CON group (P=0.478). After twelve weeks the HHS of both groups increased to a similar level (P=0.645) and did not become significant again after 3.5 years (P=0.457). There was also no significant difference between the baseline/twelve-week respectively baseline/3.5 year differences in the two groups (P=0.374 respectively 0.691). Statistical analysis of the WOMAC-Score also did not reveal any significant differences, either for the total score or for the diverse sub-scores (Table 3).
Table 3.
The HHS showed a similar increase in both groups in the early follow-up. Af-ter six weeks the difference became significant. But calculating the mean difference between the baseline and the six weeks HHS (primary endpoint) we evaluated no sig-nificant differences between the MIS and CON group. The WOMAC score showed no significant differences at any point in the early follow-up period, neither for the total score nor for pain, stiffness or activity.
| Timing | MIS | CON Hemoglobin | P | MIS | CON Hematocrit | P |
|---|---|---|---|---|---|---|
| Preoperative | 60.86±13.98 | 57.75±12.90 | 0.374 | |||
| 6w postoperative | 84.82±13.56 | 77.97±15.23 | 0.045 | 23.96±20.58 | 20.22±19.92 | 0.478 |
| 12w postoperative | 87.75±13.55 | 88.47±10.25 | 0.645 | 26.89±17.23 | 30.72±15.60 | 0.374 |
| 3y postoperative | 93.00±7.07 | 91.41±11.02 | 0.457 | 32.14±15.18 | 33.66±13.97 | 0.691 |
| WOMAC | WOMAC (difference to baseline) | |||||
| Preoperative | 52.00±7.18 | 55.13±12.42 | 0.476 | |||
| 6w postoperative | 19.93±14.25 | 23.94±15.45 | 0.235 | -32.07±15.29 | -31.19±15.19 | 0.823 |
| 12w postoperative | 16.32±9.77 | 19.28±13.29 | 0.578 | -35.68±10.41 | -35.84±14.99 | 0.960 |
| 3y postoperative | 13.07±11.47 | 16.19±18.56 | 0.859 | -38.93±12.81 | -38.94±15.40 | 0.998 |
| WOMAC – pain | WOMAC (difference to baseline) – pain | |||||
| Preoperative | 10.32±2.28 | 11.25±2.97 | 0.325 | |||
| 6w postoperative | 3.04±2.84 | 3.63±3.61 | 0.657 | -7.29±3.41 | -7.63±4.28 | 0.734 |
| 12w postoperative | 2.75±2.27 | 2.81±3.23 | 0.599 | -7.57±2.87 | -8.44±3.80 | 0.320 |
| 3y postoperative | 2.46±3.01 | 2.47±3.77 | 0.877 | -7.86±3.68 | -8.78±3.24 | 0.310 |
| WOMAC – stiffness | WOMAC (difference to baseline) – stiffness | |||||
| Preoperative | 4.71±1.15 | 5.22±1.36 | 0.295 | |||
| 6w postoperative | 2.14±1.43 | 2.41±1.90 | 0.709 | -2.61±1.60 | -2.81±1.98 | 0.658 |
| 12w postoperative | 2.44±1.68 | 2.04±1.29 | 0.237 | -2.71±1.36 | -2.78±1.79 | 0.870 |
| 3y postoperative | 1.50±1.55 | 1.56±1.54 | 0.860 | -3.25±1.43 | -3.66±1.34 | 0.262 |
| WOMAC – activity | WOMAC (difference to baseline) – activity | |||||
| Preoperative | 36.93±6.38 | 38.66±9.01 | 0.630 | |||
| 6w postoperative | 14.75±10.67 | 17.91±11.04 | 0.187 | -22.18±12.40 | -20.75±10.19 | 0.631 |
| 12w postoperative | 11.54±6.93 | 14.03±9.51 | 0.357 | -25.39±8.77 | -24.63±10.70 | 0.761 |
| 3y postoperative | 9.11±8.14 | 12.16±14.19 | 0.688 | -27.82±9.90 | -26.50±12.26 | 0.646 |
MIS, minimally invasive hip surgery; CON, conventional lateral approach; HHS, Harris Hip score.
Preoperatively, we evaluated a lower percentage of Trendelenburg sign (TS) in the MIS group (17.9% vs. 21.9%; P=0.756). After six weeks the MIS showed a decrease of TS positive patients (7.1%) whereas the CON group showed an increase (28.1%) and so the difference between the two groups became significant (P=0.048). At the 12-week followup also the proportion of TS positive patients in the CON group fell below the baseline (12.5%) and in the MIS group only one patient was left with a positive TS (3.6%). So the difference between the two groups was no longer significant (P=0.359). After 3.5 years none of the patients in the MIS group and only three patients (9.4%) in the CON group had a positive TS (P=0.241). All patients with a positive TS 12 weeks respectively 3.5 years after total hip replacement had had the TS before surgery.
Radiographs
The recommendations for inclination and anteversion of the acetabular cup differ in literature, but a range of 30° to 50° inclination and 5° to 30° anteversion is approved by most authors.18-23 Radiological evaluation of the acetabular cup positioning showed two cups with an inclination only just out of the recommended range in the CON group. In the MIS group all patients were within the normal range. Statistical calculations revealed that this difference was not significant (P=0.494). The difference in the acetabular cups outside the recommended range for anteversion was also not significant (MIS 7 vs. CON 5; P=0.532). However, the inclination of the acetabular cup in the MIS group was significantly higher (42.18±5.04 vs. 38.96±5.31; P=0.011), whereas the anteversion did not significantly differ (MIS 19.71±6.15 vs. 19.19±4.96; P=0.697). The mean leg-length difference in both groups was almost identical (MIS 6.45±4.19 vs. CON 6.69±3.74; P=0.795).
When implanting the stem, surgeons aim for an anatomical position in accordance with the femoral axis. In both groups the mean stem position differed only marginally from the ideal position (MIS 1.24±0.86 vs. CON 1.06±0.84; P=0.379). The quality of cementation according to Mulroy was level A in 11 cases (30.56%) of the MIS group and 15 (40.54%) of the CON group, level B in 23 (63.89%) cases, respectively 20 (52.63%) cases and level C1 in 2 (5.88%) cases, respectively 3 (8.11%) cases. Poorer results were not observed. Statistical analysis using the exact Chi-Square-Test (P=0.562) and the exact Cochrane-Armitage-Test (P=0.5519) revealed no significant differences.
Discussion
Several studies have been performed to evaluate the possible benefits of different kinds of minimally invasive approaches for total hip replacement. A meta-analysis of 28 randomised and non-randomised controlled trials comparing the clinical and radiological outcomes of minimally invasive and conventional THA procedures by Smith et al. revealed that the MIS procedure did not result in a better outcome.24 As most of these studies focused their interest only on some individual aspects, for example clinical outcome or radiological outcome, we performed an extensive comparison of the anterolateral minimally invasive approach by Bertin and a conventional lateral approach. Moreover, great importance was attached to continuous monitoring of both the early postoperative follow-up and the longterm follow-up. Despite this, and despite the fact that we compared two large and homogeneous groups of patients we detected only a few significant differences, most of which were related to intraoperative characteristics. Thus, the intraoperative blood loss, for instance, was significantly higher in the MIS group, but by using the Cell-Saver® the blood loss was compensated and the postoperative haemoglobin index did not differ between the groups. Our results differ from those of Martin et al., who observed a lower blood loss in patients who underwent surgery by Bertin’s MIS approach.7 The contradictory results may be explained by the fact that we did not only evaluate the postoperative haemoglobin but also the real blood loss during the surgery. Furthermore, the use of the cell-saver may influence the results. In accordance with Martin et al. and other authors we evaluated a significantly shorter skin incision but longer surgical time for the MIS group. Both are of subordinate importance, especially as minimally invasive should not address the length of the skin incision, but minimise surgical trauma.8,10 For this purpose we measured CRP and CK-NAC as markers for muscle damage. But we found significant differences only for CRP at first and second day after surgery. Bergin et al. performed the same analysis for the minimally invasive direct anterior approach.25 In comparison to the conventional posterior approach they observed significant differences only immediately after surgery for CK-NAC, but not on the first and second postoperative days.
As early functional recovery is of particular interest and attractive to both patients and surgeons, determination of the HHS was declared as the primary endpoint of the study. Evaluation of the differences between the preoperative HHS and the 6-week result revealed a slightly faster, but non-significant, increase in the HHS in the MIS group during the first six weeks after surgery, even if the difference at six weeks regarding the HHS was significant. However, the 12-week results were equal. Examination of the Trendelenburg sign showed significantly better results in the MIS group after six weeks. But already 12 weeks after surgery both groups were on the same level. This corresponds to the results of Inaba et al., who also evaluated a better, but non-significant, recovery during the first six weeks after surgery.26 However, this only applied to the first six weeks, not to the longer follow-up. One explanation for this apparent advantage in the immediate postoperative phase may be delivered by the study of Muller et al. Using MRI imaging to compare a minimally invasive anterolateral with a direct lateral approach they observed no degeneration of muscles in the MIS group, but atrophy of the gluteus medius in a large number of patients who underwent hip replacement with the direct lateral approach. The loss of gluteus medius function was compensated by a hypertrophy of the m. tensor fasciae latae. However, after 12 weeks and also after 3.5 years the HHS was at a very high level in both groups. The WOMAC score, as a further indicator for functional outcome and the pain level, respectively analgesic intake, was equal for both groups at all times.
A further important factor for successful hip replacement is the correct positioning of the implants. It is often maintained that the reduced visibility during MIS approaches provokes poorer cup and stem positioning in comparison to conventional approaches, which in turn results in a reduced survival time of the arthroplasties.27,28 However, this was not substantiated by our study, as postoperative radiographs did not show any significant differences, and the rate of malpositioning was almost equal in the two groups. Other authors, for example Wohlrab et al. and Martin et al., also found similar results regarding implant position in patients who underwent hip replacement by an anterolateral minimally invasive approach.7,8
Conclusions
In conclusion, both approaches are adequate for hip replacement. The experience and preferences of the individual surgeon seem to be more important factors when it comes to the choice of surgical technique. The only advantages of the MIS approach are the smaller skin incision and possible faster rehabilitation in the first six weeks after surgery. Regarding a minimization of the surgical trauma we observed significant differences only for CRP at first and second day after surgery
Acknowledgments
we thank Christian Lösch from the Institute of Medical Informatics, Biometry and Epidemiology for supporting statistical analysis. The study was sponsored by Stryker™, 325 Corporate Drive, Mahwah, New Jersey 07430, United States and HECTEC™ GmbH, Ottostr. 16, 84030 Landshut, Germany.
References
- 1.Bertin KC, Rottinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res 2004:248-55 [PubMed] [Google Scholar]
- 2.Dorr LD, Maheshwari AV, Long WT, et al. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty. A prospective, randomized, blinded study. J Bone Joint Surg Am. 2007;89:1153-60 [DOI] [PubMed] [Google Scholar]
- 3.Gravius S, Wirtz DC, Maus U, et al. [Minimally invasive approaches to the hip joint for total hip arthroplasty: state of the art within the scope of the OrthoMIT project for the development of an integrated platform for smart interventional orthopaedic surgery and traumatology]. Z Orthop Unfall 2007;145:608-14 [Article in German] [DOI] [PubMed] [Google Scholar]
- 4.Mow CS, Woolson ST, Ngarmukos SG, et al. Comparison of scars from total hip replacements done with a standard or a mini-incision. Clin Orthop Relat Res 2005;441:80-5 [DOI] [PubMed] [Google Scholar]
- 5.Woolson ST, Mow CS, Syquia JF, et al. Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg Am 2004;86A:1353-8 [DOI] [PubMed] [Google Scholar]
- 6.Watson-Jones R. The classic: Fractures and Joint Injuries by Sir Reginald Watson-Jones, taken from Fractures and Joint Injuries, by R. Watson-Jones, Vol. II, 4th ed., Baltimore, Williams and Wilkins Company, 1955. Clin Orthop Relat Res 1974:4-10 [PubMed] [Google Scholar]
- 7.Martin R, Clayson PE, Troussel S, et al. Anterolateral minimally invasive total hip arthroplasty: a prospective randomized controlled study with a follow-up of 1 year. J Arthroplasty 2011;26:1362-72 [DOI] [PubMed] [Google Scholar]
- 8.Wohlrab D, Droege JW, Mendel T, et al. [Minimally invasive vs. transgluteal total hip replacement. A 3-month follow-up of a prospective randomized clinical study] Orthopade. 2008;37:1121-6 [Article in German] [DOI] [PubMed] [Google Scholar]
- 9.D’Arrigo C, Speranza A, Monaco E, et al. Learning curve in tissue sparing total hip replacement: comparison between different approaches. J Orthop Traumatol 2009;10:47-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leuchte S, Luchs A, Wohlrab D. [Measurement of ground reaction forces after total hip arthroplasty using different surgical approaches]. Z Orthop Ihre Grenzgeb 2007;145:74-80 [DOI] [PubMed] [Google Scholar]
- 11.Thomine JM, Duparc F, Dujardin F, Biga N. [Transgluteal approach to the hip by anterior hemimyotomy of the gluteus medius]. Rev Chir Orthop Reparatrice Appar Mot 1999;85:520-5 [Article in German] [PubMed] [Google Scholar]
- 12.Gordon DB, Stevenson KK, Griffie J, et al. Opioid equianalgesic calculations. J Palliat Med 1999;2:209-18 [DOI] [PubMed] [Google Scholar]
- 13.Tannast M, Zheng G, Anderegg C, et al. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res 2005;438:182-90 [DOI] [PubMed] [Google Scholar]
- 14.Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty 2004;19:387-90 [DOI] [PubMed] [Google Scholar]
- 15.McLaren RH. Prosthetic hip angulation. Radiology 1973;107:705-6 [DOI] [PubMed] [Google Scholar]
- 16.Barrack RL, Mulroy RD, Jr., Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review J Bone Joint Surg Br 1992;74:385-9 [DOI] [PubMed] [Google Scholar]
- 17.Mulroy WF, Estok DM, Harris WH. Total hip arthroplasty with use of so-called secondgeneration cementing techniques. A fifteen-year-average follow-up study J Bone Joint Surg Am. 1995;77:1845-52 [DOI] [PubMed] [Google Scholar]
- 18.Charnley J. Total hip replacement by lowfriction arthroplasty. Clin Orthop Relat Res 1970;72:7-21 [PubMed] [Google Scholar]
- 19.Coventry MB. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am 1985;67:832-41 [PubMed] [Google Scholar]
- 20.D’Lima DD, Urquhart AG, Buehler KO, et al. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am 2000;82:315-21 [DOI] [PubMed] [Google Scholar]
- 21.Harris WH. Advances in surgical technique for total hip replacement: without and with osteotomy of the greater trochanter. Clin Orthop Relat Res 1980:188-204 [PubMed] [Google Scholar]
- 22.Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978;60:217-20 [PubMed] [Google Scholar]
- 23.Seki M, Yuasa N, Ohkuni K. Analysis of optimal range of socket orientations in total hip arthroplasty with use of computer-aided design simulation. J Orthop Res 1998;16:513-7 [DOI] [PubMed] [Google Scholar]
- 24.Smith TO, Blake V, Hing CB. Minimally invasive versus conventional exposure for total hip arthroplasty: a systematic review and meta-analysis of clinical and radiological outcomes. Int Orthop 2011;35:173-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bergin PF, Doppelt JD, Kephart CJ, et al. Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers. J Bone Joint Surg Am 2011;93:1392-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Inaba Y, Kobayashi N, Yukizawa Y, et al. Little clinical advantage of modified watson-jones approach over modified miniincision direct lateral approach in primary total hip arthroplasty. J Arthroplasty 2011;26:1117-22 [DOI] [PubMed] [Google Scholar]
- 27.Cheng T, Feng JG, Liu T, Zhang XL. Minimally invasive total hip arthroplasty: a systematic review. Int Orthop 2009;33:1473-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Szendroi M, Sztrinkai G, Vass R, Kiss J. The impact of minimally invasive total hip arthroplasty on the standard procedure. Int Orthop 2006;30:167-71 [DOI] [PMC free article] [PubMed] [Google Scholar]


