Abstract
From the first shoulder arthroscopy performed on a cadaver in 1931, shoulder arthroscopy has grown tremendously in its ability to diagnose and treat pathologic conditions about the shoulder. Despite improvements in arthroscopic techniques and instrumentation, it is only recently that arthroscopists have begun to explore precise anatomical structures within the subdeltoid space. By way of a thorough bursectomy of the subdeltoid region, meticulous hemostasis, and the reciprocal use of posterior and lateral viewing portals, one can identify a myriad of pertinent ligamentous, musculotendinous, osseous, and neurovascular structures. For the purposes of this review, the subdeltoid space has been compartmentalized into lateral, medial, anterior, and posterior regions. Being able to identify pertinent structures in the subdeltoid space will provide shoulder arthroscopists with the requisite foundation in core anatomy that will be required for challenging procedures such as arthroscopic subscapularis mobilization and repair, biceps tenodesis, subcoracoid decompression, suprascapular nerve decompression, quadrangular space decompression and repair of massive rotator cuff tears.
Key words: subdeltoid space, arthroscopy, anatomy
Introduction
Through the evolution in arthroscopic techniques, instrumentation, and implants, the shoulder anatomy has remained constant, but only recently have shoulder arthroscopists begun to explore precise anatomical structures within the subdeltoid space. An appreciation of the anatomy begins with proper entry and extensive bursectomy. In the present article, the authors have described the arthroscopic anatomy of the lateral, medial, anterior, and posterior regions of subdeltoid space.
Arthroscopic anatomy by location
Lateral
Greater tuberosity
The greater tuberosity is the insertion site of the supraspinatus, infraspinatus, and teres minor (Figure 1A and B). Of particular interest to the arthroscopist is the footprint of the supraspinatus insertion on the greater tuberosity. An anatomic dissection study of the supraspinatus footprint found that the mean anterior to posterior dimension of the supraspinatus tendon was 25 mm, with a mean medial to lateral thickness of the footprint of 12 mm - the mean distance from the cartilage to the supraspinatus footprint was 1.5 mm at midtendon.1
Figure 1.
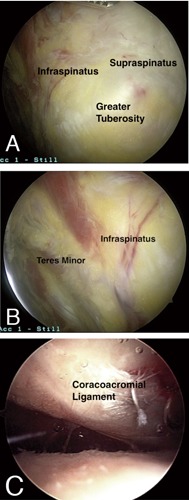
A) Insertion of the supraspinatus and Infraspinatus tendons is visualized on the rotator cuff fooprint on the greater tuberosity (lateral viewing portal). B) Insertion of the Infraspinatus and teres minor is visualized (lateral viewing portal). C) Visualization of the coracoacromial ligament from posterolateral viewing portal.
The greater tuberosity can be seen from either a posterior viewing portal or lateral viewing portal. It is important to perform at least a partial resection of the sub-acromial bursa to improve visualization of this structure. With the use of a mechanical shaver or electrocautery device the lateral sub-deltoid region can be visualized and the most lateral insertion of the greater tuberosity is well visualized.
Supraspinatus tendon
The supraspinatus originates from the supraspinatus fossa and the superior surface of the spine of the scapula, and runs laterally to insert on the anteromedial area of the highest impression of the greater tuberosity.2 The anterior margin of the supraspinatus is defined by the posterior edge of the rotator interval that separates the supraspinatus from the rolled superior border of the subscapularis. The posterior margin of the supraspinatus is marked by the extension of the raphe between supraspinatus and infraspinatus around the scapular spine. The anterior portion of the supraspinatus is composed of a long and thick tendinous component whereas the posterior portion has been shown to be short and thin. The supraspinatus derives its innervation from the suprascapular nerve.
Arthroscopic evaluation of the supraspinatus tendon has been well described from the subdeltoid space. The key to its evaluation is appropriate resection of the sub-deltoid bursa. This must be accomplished with some alacrity as the bursa may become distended with arthroscopic fluid and swell, impeding visualization. Optimal viewing of the supraspinatus insertion is via 2 portals - by viewing the insertion from at least 2 vantage points the surgeon can more easily identify the anatomic insertion.
Infraspinatus tendon
The infraspinatus originates from both the infraspinatus fossa and the inferior surface of the spine of the scapula, running from this medial origin in a superior and lateral direction to insert on the middle impression of the greater tuberosity. The innervation to the infraspinatus is also derived from the suprascapular nerve. Much like the supraspinatus the infraspinatus is comprised of a thick tendinous portion and a thinner component, although the thicker portion is oriented more inferiorly.
The footprint of the infraspinatus resembles a trapezoid that is wider laterally than medially, with an average maximum length of 10.2±1.6 mm and an average width of 32.7±3.4 on the lateral margin.2 Arthroscopically the insertion of the infraspinatus can be difficult to truly delineate, as there is often some connective tissue including the coracohumeral ligament overlying the border between the infraspinatus footprint and the footprint of the supraspinatus. By following the muscle tendon unit from its more medial aspect the arthroscopist can better appreciate the demarcation.
Acromion
The acromion has been implicated by several authors in the pathology of rotator cuff dysfunction and injury.3 The classic study by Aoki et al. described three types of acromial morphology.4 A type I acromion is one with a flat undersurface, a type II Acromion is defined as having a curved undersurface, and a Type III has a hooked undersurface that carried the highest risk of impingement.
Nicholson et al. reported the mean acromial dimensions in men to be length = 48.5 mm, width = 19.5 mm, and anterior thickness = 7.7 mm. The mean dimensions in women were significantly different and reported to be length = 40.6 mm, width = 18.4 mm, and thickness = 6.7 mm.3
The acromion serves as the attachment of the coracoacromial ligament, is the origin of the deltoid muscle, and forms the acromioclavicular joint via an articulation with the clavicle. The arthroscopist can choose to evaluate the acromion via a lateral, posterior, or anterior portal position, though the posterior and lateral portals are most common. It is important to remove the soft tissue from the undersurface to delineate the anatomy.
Coracoacromial ligament
The coracoacromial ligament (CAL) is part of the coracoacromial arch, serving as a connection between the coracoid and the acromion. Holt et al. described 3 main anatomic variants of the CAL: quadrangular, Y-shaped, and a broadband variant.5 In 2008 Kesmezacar et al. added a V-shaped variant and multiple band variant to the existing classification.6 They determined that the Y-shaped variant was the most common type occurring at a frequency of 41.3% while the multi-band type was least common occurring in 11.2% of specimens, with a significantly increased incidence of rotator cuff pathology in those specimens with CALs that had more than one bundle.
Flatow et al. reported that the CAL is an important superior stabilizer of the shoulder.7 Lee et al. demonstrated that with release of the CAL increased translation was observed in the inferior and anterior directions at multiple degrees of abduction.8 For this reason, release of this structure may lead to anterior and superior instability when the primary stabilizers (i.e. rotator cuff) of the humerus are absent.
Optimal viewing of the CAL can be achieved from a postero-lateral portal in the subacromial space (Figure 1C). By viewing from this area subtle extensions of the ligament that may contribute to an impingement-like condition can be appreciated. The CAL also serves as the anterior boundary of a triangle formed by the undersurface of the AC joint and the anterior border of the supraspinatus that is the initial interval for suprascapular nerve decompression at the suprascapular notch.
Medial
Distal clavicle/AC Joint
Distal clavicle resection was first described by Mumford in 1941.9 Disease processes including AC joint arthritis, distal clavicle osteolysis, and fractures of the distal end of the clavicle have all been treated arthroscopically.10
This anatomy is also of particular interest in the arthroscopically assisted reconstruction of the coraco-coracoid ligaments. Rios et al. determined the mean distances from the lateral clavicle to the conoid tuberosity (Male: 47.2 mm, Female: 42.8 mm) and the distance from the lateral edge of the clavicle to the center of the trapezoid tuberosity (M: 25.4 mm, F: 22.9 mm).11
For simple evaluation of the AC joint a lateral or posterior viewing portal is sufficient in the subacromial space (Figure 2A). The AC joint can be arthroscopically excised via the indirect subacromial approach through a lateral viewing portal with the working portal being anterior, or via direct superior approach with the arthroscope placed posterior to the AC joint and directed intra-articularly.10,12
Figure 2.
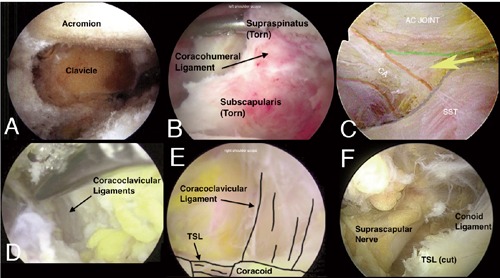
A) Undersurface of the acromion and resected distal clavicle as viewed from a lateral portal. B) The coracohumeral ligament is identified in an anterosuperior rotator cuff tear (lateral viewing portal). Notice how it attaches to both the leading rolled border of the subscapularis and the leading edge of the supraspinatus. C) The triangular interval formed by the anterior border of the supraspinatus, the medial border of the coracoacromial (CA) ligament, and the undersurface of the acromioclavicular (AC) joint is entered (from lateral viewing portal) to gain access to the coracoclavicular ligaments. D) The posterior aspect of the coracoclavicular ligaments is identified from a posterior viewing portal anterior to the supraspinatus plane. E) With the arthroscope advanced more medial compared with figure 2d, the posterior aspect of the coracoacromial ligaments is identified from a lateral viewing portal anterior to the supraspinatus plane. The schematic on the right demonstrates the conoid ligament, the transverse scapular ligament (TSL) and the base of the coracoid. F) The resected transverse scapular ligament (TSL) along with the decompressed suprascapular nerves are identified from a lateral viewing portal.
Rotator interval
First described by Neer in 1970, the RI defines the anterosuperior space in the rotator cuff between the supraspinatus and subscapularis tendons.13 This triangular space, whose base is located medially at the coracoid process and whose apex is lateral at the intertubercular groove, contains the long head of the biceps tendon, the superior glenohumeral ligament (SGHL), the glenohumeral joint capsule and coracohumeral ligament (CHL).14,15 While debate still remains in the orthopaedic surgery literature as to its exact function, recent studies have demonstrated that the rotator interval plays a role in the stability of the glenohumeral joint.16-21 The interval and its structures can be visualized from a lateral viewing portal or from an anterior viewing portal.
Coracohumeral ligament
Neer who implicated shortening and thickening of the CHL in the pathology of adhesive capsulitis, particularly loss of external rotation.22 Yang et al. dissected 26 fresh frozen shoulders, and identified that the CHL is shaped like an irregular trapezoid.23 The CHL lies below the subacromial bursa and above the subcoracoid bursa. The origin of this structure is constant, taking rise from the lateral aspect of the coracoid. The insertion is more variable, with the termination seen on the supraspinatus, rotator interval, or subscapularis.23
This structure can be visualized from the lateral portal when the rotator interval is opened or has been injured (Figure 2B). Alternatively the anterior portal can be used to optimize the visualization of the CHL.
Coracoid
Several procedures, including arthroscopic transfer of the coracoid and conjoint tendon, and release of the transverse scapular ligament (TSL) require visualization of the coracoid as a landmark.24,25 The coracoid serves as the origin of the short head of the biceps and coracobrachialis tendons as well as the insertion of the pectoralis minor, coracoacromial, coracohumeral, coraco-clavicular ligaments. From the subdeltoid space the coracoid can be located reliably by dissecting initially with a blunt instrument into the triangle formed by the undersurface of the AC joint, the anterior border of the supraspinatus, and the edge of the CA ligament. By viewing from a lateral portal the arthroscopist can look over the top of the supraspinatus and follow the conoid ligament to find the base of the coracoid (Figure 2C). The TSL extends laterally from the coracoid base (Figure 2D).
Sub-coracoid space
The area between the lesser tuberosity and the coracoid process has recently been implicated by some authors as a potential location for impingement of the subscapularis.26-30 There have been several studies that have determined the normal coracohumeral distance with measurements ranging between 8.7-11 mm.29,31 In a study by Nove-Josserand et al. using CT-arthrograms performed in patients with full thickness rotator cuff tears, patients with tears involving the subscapularis had a significantly decreased coracohumeral distance, with 26% having less than 6 mm of space.32
The coracohumeral space can be seen by viewing from either a standard posterior viewing portal or from a lateral portal. An arthroscopic probe can be used to measure the distance between the subscapularis tendon and the coracoid.
Coracoclavicular ligaments
The CCLs are two distinct structures connecting the clavicle to the coracoid, with the primary function of providing stability of the clavicle in the superior and inferior plane. The more medial of the two is the conoid ligament and is seen to originate on average 47 mm from the lateral edge of the clavicle in males and 42.8 mm from the lateral edge in females. The more lateral structure is the trapezoid ligament, with an average distance from the lateral clavicle to the footprint of the trapezoid of 25.4 mm in men and 22.9 mm in women.11 The conoid footprint (25.3 mm) on the clavicle is more than 2 times the size of the trapezoid origin (11.8).
The CC ligaments can be identified from either a lateral or posterior viewing portal, but we prefer a lateral viewing position in the subacromial space. A triangle defined by the undersurface of the AC joint, the medial edge of the CAL and the anterior border of the supraspinatus muscle belly is the first interval that must be developed when attempting to define these structures (Figure 2C). A Wissenger rod may be helpful to retract the anterior border of the supraspinatus to better define these structures as described by Ghodadra et al.25 The posterior aspect of both ligaments can be seen from this approach and by following the conoid ligament distally the arthroscopist can easily and reproducibly identify the coracoid (Figure 2D and E).
Suprascapular notch/transverse scapular ligament
The TSL serves as the roof of the suprascapular notch (Figure 2F), and has been classified by Rengachary et al. into 6 different types.33 The suprascapular artery passes over the TSL and the suprascapular nerve passes beneath it. There are many reports of suprascapular nerve entrapment occurring at this site and recently arthroscopic techniques of TSL release have been described.25
With the patient in the beach chair position the surgeon can place the arthroscope in the lateral portal for viewing while working initially from an anterior portal. Again the triangle formed by the supraspinatus anterior border, the posterior aspect of the CAL ligament, and the undersurface of the AC joint is developed by blunt dissection (Figure 2C). The CC ligaments are identified and followed to the base of the coracoid. The TSL inserts here on the base of the coracoid and can be more clearly defined by blunt dissection. Once identified the ligament can be released with an arthroscopic device.
Anterior
Lesser tuberosity
The lesser tuberosity is the insertion site for the subscapularis tendon. The biceps groove is located directly lateral to the lesser tuberosity, with the articular cartilage of the humeral head being medial. The insertion of the subscapularis muscle was described by Curtis et al. to take place in a comma-shaped pattern from 7 to 11 o’clock around the tuberosity (with the right shoulder used as a point of reference). 34 In this cadaveric study, the average maximum length of the tendon insertion was 40 mm (range: 35-55 mm), and the average maximum width was 20 mm (range: 15-25 mm), with the superior portion of the footprint the widest part of the subscapularis insertion. The mean width at the most superior aspect of the insertion site was 1.8 cm (range: 1.5 to 2.6 cm). The most inferior aspect of the footprint was much narrower with a mean width of 0.3 cm (range: 0.1 to 0.7 cm).
Subscapularis tendon
The subscapularis muscle is the largest and most powerful rotator cuff muscle, arising from the anterior surface of the scapula. This muscle is innervated by the upper and lower subscapular nerves, and Its major role is internal rotation of the humerus. The subscapularis has between four and six tendon slips that arise from deep within the muscle and converge superiorly and laterally to form the main tendon that inserts along the superior aspect of the lesser tuberosity.17
At the upper aspect of the subscapularis tendon, the fibers interdigitate with the anterior fibers of the supraspinatus to contribute to the structure of the rotator cuff interval as well as the transverse humeral ligament. Glenohumeral arthroscopy can be used to visualize the subscapularis tendon by positioning the arthroscope in the posterior portal and then elevating the shoulder to greater than 45 degrees while providing internal rotation.35 This position also allows visualization of the biceps tendon, coracohumeral, and superior glenohumeral ligaments.
A study by Pearsall et al.36 found that the intra-articular portion of the subscapularis constituted approximately 25% of the entire cephalocaudal dimension of the subscapularis tendon. Burkhart and Tehrany were the first to report on arthroscopic repair of the subscapularis tendon.37 An extra-articular view of the subscapularis tendon can also be achieved by use of a lateral viewing portal (Figure 3A).
Figure 3.
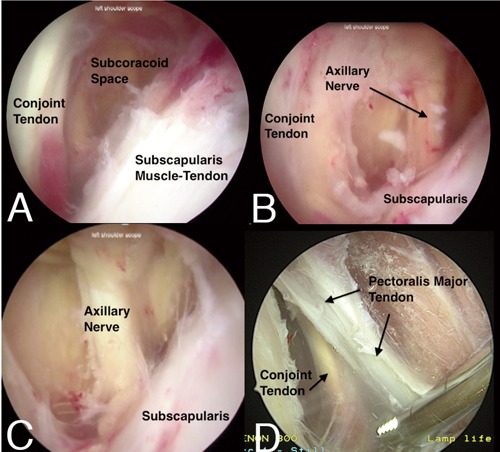
A) The conjoint tendon and the subscapularis muscle tendon units define the anterior and posterior boundaries of the subcoracoid space, respectively, and can be visualized from a lateral viewing portal. B) With the arthroscope advanced more medially compared with Figure 3a, the deep aspect of the conjoint tendon and medial subscapularis muscle tendon unit can be seen. After a careful bursectomy in this area, the axillary nerve can also been seen along the lower border of the subscapularis. C) The axillary nerve visualized in the subcoracoid space from a lateral viewing portal. D) The conjoint tendon and the deep portion of the pectoralis major tendon can be visualized during the dissection required for an arthroscopic biceps tenodesis. This view is appreciated from a lateral viewing portal at the junction of the anterior and middle thirds of the acromion with the arm in a forward flexed and slightly abducted position.
Pectoralis major tendon
The pectoralis major muscle is a powerful internal rotator, flexor, and adductor of the arm. This muscle has a superior half, which forms the clavicular head, and an inferior half, which forms the sternal head. The lateral pectoral nerve is responsible for innervating the clavicular head and the medial portion of the sternal head. The medial pectoral nerve innervates the lateral portion of the sternal head.
The pectoralis tendon is approximately 5 cm wide, 1 cm long on the anterior surface, and 2.5 cm long on the posterior surface.38,39 The tendon has been described as having three laminae.40 The investing fascia of the pectoralis muscle is continuous with the fascia of the brachium as well as the medial antebrachial septum, making it challenging to visual the true tendon arthroscopically. However, the deep and superior surface of the pectoralis major can be visualized during an arthroscopic suprapectoral biceps tenodesis (Figure 3B).
Long head of biceps tendon
The LHB is normally found within the glenohumeral joint, within a synovial sheath. It passes anterior and superior to the humeral head, emerging from the joint in the bicipital groove. In the bicipital groove the tendon is bound by the subscapularis, supraspinatus, the transverse humeral ligament, and an extension from pectoralis major.41 The long head of biceps tendon has been described as originating at the supraglenoid tubercle, however several studies have demonstrated significant anatomic variance. Pal et al. found in 70% of shoulder the posterior-superior glenoid labrum was deficient and the long head of the biceps replaced it, resulting in only a small portion of the tendon attaching to the supraglenoid tubercle.42 Similarly, Vangsness et al. studied 105 cadaveric shoulders and found only 40-60% of LHB tendons originated at the supraglenoid tubercle, with the rest originating at the superior glenoid labrum.43
The bicipital groove is located between the greater and lesser tubercles at the proximal extremity of the humerus and extends inferiorly. A recent study by Wafae et al. found the average length of the groove to be 8.1 cm, with a width of 10.1 mm, and an average depth of 4 mm.44 Direct arthroscopy of the bicipital groove can be performed, by placing a 4.5 mm cannula through a superior-medial (Neviaser) portal and into the glenohumeral joint.45 The arm is then positioned in abduction, external rotation, and forward flexion, to align the groove with the arthroscope, allowing direct visualization.
Neurovascular structures
The main neurovascular structures in the anterior aspect of the subdeltoid space are the axillary nerve and the musculocutaneous nerve. The axillary nerve runs obliquely across the inferolateral border of the subscapularis, crossing 3 to 5 mm from its musculotendinous junction (Figure 3C and D). Bryan and colleagues found that it averaged 0.32 cm inferior to the capsule of the shoulder.46 Eakin et al. delineated a safe zone for the placement of casulolabral sutures, finding that as long as the sutures entered the capsule 1 cm from the glenoid, all were farther than 7 mm from the axillary nerve at any position around the capsule.47,48 The musculocutaneous nerve can be predictable found as it courses through the conjoined tendon about 1 to 5 cm distal to the coracoid process - by following the conjoined tendon inferiorly from the coracoid, it can be visualized arthroscopically.
Posterior
Posterior interval
The posterior rotator interval lies between the supraspinatus and the infraspinatus in the space created by the separation of these muscles by the scapular spine (Figure 4A). Miller et al. defined the interval to be an average of 49.4 mm (scapular spine to the confluence of the tendons) which is devoid of any muscle or tendon.49 The interval is technically triangular, and the histologic makeup of the interval is fibroadipose tissue with a synovial lining analogous to the shoulder capsule.
Figure 4.
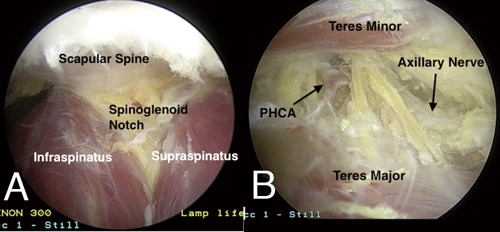
A) The scapular spine (as viewed from a lateral portal) can be used to delineate the border between the supraspinatus and Infraspinatus. By following the scapular spine medially, dissection to the spinoglenoid notch can also be performed. B) Identification of the axillary nerve and posterior humeral circumflex artery (PHCA) in the quadrangular space from a posterior viewing portal.
Scapular spine
The scapular spine serves as a boundary between the supraspinatus and Infraspinatus (Figure 4B). Tubbs et al. described that the length of the spine ranged from 7 to 15 cm (mean 11.5 cm), and that the mean thickness was 1 cm at the most medial segment (1 cm), 2.2 cm at the segment adjacent to the spinoglenoid notch, and 2.5 cm near the acromion (2.5 cm).50
Spinoglenoid notch
The reported prevalence of the spinoglenoid ligament varies between 3-80%, however a recent study by Plancher et al. demonstrated 100% prevalence of the spinoglenoid ligament in a cadaveric study of fifty-eight shoulders.51
Arthroscopic decompression of the spinoglenoid notch has been described in the literature and may be done via the glenohumeral or subacromical space. Our preferred method is to use an anterior high rotator interval portal for viewing, and a create a posterior working portal 3 cm inferior to and in line with the posterolateral acromion.25 Any labral pathology is addressed. The posterior-superior capsule is released with a mechanical shaver between the 9-o’clock and 12-o’clock positions, preserving the posterior band of the inferior glenohumeral ligament complex. The raphe between the supraspinatus and infraspinatus is identified and followed medially (Figure 4A). If a cyst is present it can be seen directly on the scapula and decompressed with a shaver.
If inspection of the glenohumeral joint does not show a capsule or labral tear, the spinoglenoid notch cyst can be decompressed from the subacromial space, using a posterior and lateral portal. All soft tissue is removed from the undersurface of the acromion and the bursal surface of the rotator cuff. The arthroscope is directed posteriorly and medially to identify the separate muscle bellies of the supraspinatus and the infraspinatus, and to visualize the scapular spine. A probe can be used to palpate the posterior aspect of the glenoid, which defines the anterior boundary, and the cyst can sometimes be localized between the scapular spine and the posterior glenoid. The mechanical shaver is used to debride the soft tissue and further expose the spinoglenoid notch cyst is carefully advanced from anterior to posterior, to avoid injury to the SSN. The SSN is located at the base of the scapular spine, and therefore the mechanical shaver should not be used near the spine. If the cyst is not palpable, the mechanical shaver can be carefully advanced until cyst fluid is visible.
Quadrangular space
The quadrangular space is created by the teres minor superiorly, the surgical neck of the humerus laterally, the long head of triceps medially, and the upper border of teres major inferiorly. It contains the axillary nerve and the posterior circumflex humeral artery (Figure 4B). Fibrous bands of tissue can result in compression of the quadrangular space and the axillay nerve, necessitating arthroscopic evaluation and decompression.
Discussion and Conclusisions
Through a thorough bursectomy of the subdeltoid space, meticulous hemostasis, and the reciprocal use of posterior and lateral viewing portals, one can identify a myriad of pertinent ligamentous, musculotendinous, osseous, and neurovascular structures. Being able to identify pertinent structures in the subdeltoid space will provide shoulder arthroscopists with the requisite foundation in core anatomy that will be required for challenging procedures such as arthroscopic subscapularis mobilization and repair, biceps tenodesis, subcoracoid decompression, suprascapular nerve decompression, quadrangular space decompression and repair of massive rotator cuff tears.
References
- 1.Ruotolo C, Fow JE, Nottage WM. The supraspinatus footprint: an anatomic study of the supraspinatus insertion. Arthroscopy 2004;20:246-9 [DOI] [PubMed] [Google Scholar]
- 2.Mochizuki T, Sugaya H, Uomizu M, et al. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff J Bone Joint Surg Am 2008;90:962-9 [DOI] [PubMed] [Google Scholar]
- 3.Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: morphologic condition and age-related changes. A study of 420 scapulas J Shoulder Elbow Surg 1996;5:1-11 [DOI] [PubMed] [Google Scholar]
- 4.Aoki M IS, Usui M. The slope of the acromion in the rotator cuff impingement. Orthop Trans 1986;10:228 [Google Scholar]
- 5.Holt EM, Allibone RO. Anatomic variants of the coracoacromial ligament. J Shoulder Elbow Surg 1995;4:370-5 [DOI] [PubMed] [Google Scholar]
- 6.Kesmezacar H, Akgun I, Ogut T, Gokay S, Uzun I. The coracoacromial ligament: the morphology and relation to rotator cuff pathology. J Shoulder Elbow Surg 2008;17:182-8 [DOI] [PubMed] [Google Scholar]
- 7.Flatow EL WV, Kelkar R, Raimondo RA, et al. The coracoacromial ligament passively restrains anterosuperior humeral subluxation in the rotator cuff deficient shoulder. Trans ORS 1996;21:229 [Google Scholar]
- 8.Lee TQ BA, Tibone JE, McMahon PJ. Release of the coracoacromial ligament can lead to glenohumeral laxity: a biomechanical study. J Shoulder Elbow Surg 2001;10:68-72 [DOI] [PubMed] [Google Scholar]
- 9.Mumford E. Acromioclavicular dislocation. J Bone Joint Surg 1941;23:799-802 [Google Scholar]
- 10.Freedman BA, Javernick MA, O’Brien FP, et al. Arthroscopic versus open distal clavicle excision: comparative results at six months and one year from a randomized, prospective clinical trial. J Shoulder Elbow Surg 2007;16:413-8 [DOI] [PubMed] [Google Scholar]
- 11.Rios CG, Arciero RA, Mazzocca AD. Anatomy of the clavicle and coracoid process for reconstruction of the coracoclavicular ligaments. Am J Sports Med 2007;35:811-7 [DOI] [PubMed] [Google Scholar]
- 12.Charron KM, Schepsis AA, Voloshin I. Arthroscopic distal clavicle resection in athletes: a prospective comparison of the direct and indirect approach. Am J Sports Med 2007;35:53-8 [DOI] [PubMed] [Google Scholar]
- 13.Neer CS., 2nd Displaced proximal humeral fractures. I. Classification and evaluation J Bone Joint Surg Am 1970;52:1077-89 [PubMed] [Google Scholar]
- 14.Hunt SA, Kwon YW, Zuckerman JD. The rotator interval: anatomy, pathology, and strategies for treatment. J Am Acad Orthop Surg 2007;15:218-27 [DOI] [PubMed] [Google Scholar]
- 15.Fitzpatrick MJ, Powell SE, Tibone JE, Warren RF. The anatomy, pathology, and definitive treatment of rotator interval lesions: current concepts. Arthroscopy 2003;19:70-9 [DOI] [PubMed] [Google Scholar]
- 16.Provencher MT, Mologne TS, Hongo M, et al. Arthroscopic versus open rotator interval closure: biomechanical evaluation of stability and motion. Arthroscopy 2007;23:583-92 [DOI] [PubMed] [Google Scholar]
- 17.Clark JM, Harryman DT., 2nd Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy J Bone Joint Surg Am 1992;74:713-25 [PubMed] [Google Scholar]
- 18.Itoi E, Berglund LJ, Grabowski JJ, Naggar L, et al. Superior-inferior stability of the shoulder: role of the coracohumeral ligament and the rotator interval capsule. Mayo Clin Proc 1998;73:508-15 [DOI] [PubMed] [Google Scholar]
- 19.Selecky MT, Tibone JE, Yang BY, et al. Glenohumeral joint translation after arthroscopic thermal capsuloplasty of the rotator interval. J Shoulder Elbow Surg 2003;12:139-43 [DOI] [PubMed] [Google Scholar]
- 20.Tetro AM, Bauer G, Hollstien SB, Yamaguchi K. Arthroscopic release of the rotator interval and coracohumeral ligament: an anatomic study in cadavers. Arthroscopy 2002;18:145-50 [DOI] [PubMed] [Google Scholar]
- 21.Mologne TS, Zhao K, Hongo M, et al. The addition of rotator interval closure after arthroscopic repair of either anterior or posterior shoulder instability: effect on glenohumeral translation and range of motion. Am J Sports Med 2008;36:1123-31 [DOI] [PubMed] [Google Scholar]
- 22.Neer CS, 2nd, Satterlee CC, Dalsey RM, Flatow EL. The anatomy and potential effects of contracture of the coracohumeral ligament. Clin Orthop Relat Res 1992:182-5 [PubMed] [Google Scholar]
- 23.Yang HF, Tang KL, Chen W, et al. An anatomic and histologic study of the coracohumeral ligament. J Shoulder Elbow Surg 2009;18:305-10 [DOI] [PubMed] [Google Scholar]
- 24.Lafosse L, Lejeune E, Bouchard A, et al. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy 2007;23:1242 e1-5 [DOI] [PubMed] [Google Scholar]
- 25.Ghodadra N, Nho SJ, Verma NN, et al. Arthroscopic decompression of the suprascapular nerve at the spinoglenoid notch and suprascapular notch through the subacromial space. Arthroscopy 2009;25:439-45 [DOI] [PubMed] [Google Scholar]
- 26.Dines DM, Warren RF, Inglis AE, Pavlov H. The coracoid impingement syndrome. J Bone Joint Surg Br 1990;72:314-6 [DOI] [PubMed] [Google Scholar]
- 27.Ferrick MR. Coracoid impingement. A case report and review of the literature Am J Sports Med 2000;28:117-9 [DOI] [PubMed] [Google Scholar]
- 28.Gerber C, Terrier F, Ganz R. The role of the coracoid process in the chronic impingement syndrome. J Bone Joint Surg Br 1985;67:703-8 [DOI] [PubMed] [Google Scholar]
- 29.Gerber C, Terrier F, Zehnder R, Ganz R. The subcoracoid space. An anatomic study Clin Orthop Relat Res 1987:132-8 [PubMed] [Google Scholar]
- 30.Patte D. The subcoracoid impingement. Clin Orthop Relat Res 1990:55-9 [PubMed] [Google Scholar]
- 31.Friedman RJ, Bonutti PM, Genez B. Cine magnetic resonance imaging of the subcoracoid region. Orthopedics 1998;21:545-8 [PubMed] [Google Scholar]
- 32.Nove-Josserand L BA, Levigne C. Coracohumeral space and rotator cuff tears. Rev Chir Orthop Reparatrice Appar Mot 1999;85:677-83 [PubMed] [Google Scholar]
- 33.Rengachary SS, Burr D, Lucas S, Brackett CE. Suprascapular entrapment neuropathy: a clinical, anatomical, and comparative study. Part 3: comparative study Neurosurgery 1979;5:452-5 [DOI] [PubMed] [Google Scholar]
- 34.Curtis AS, Burbank KM, Tierney JJ, et al. The insertional footprint of the rotator cuff: an anatomic study. Arthroscopy 2006;22:609 e1. [DOI] [PubMed] [Google Scholar]
- 35.Bennett WF. Subscapularis, medial, and lateral head coracohumeral ligament insertion anatomy. Arthroscopic appearance and incidence of hidden rotator interval lesions Arthroscopy 2001;17:173-80 [DOI] [PubMed] [Google Scholar]
- 36.Pearsall AWt, Holovacs TF, Speer KP. The intra-articular component of the subscapularis tendon: anatomic and histological correlation in reference to surgical release in patients with frozen-shoulder syndrome. Arthroscopy 2000;16:236-42 [DOI] [PubMed] [Google Scholar]
- 37.Burkhart SS, Tehrany AM. Arthroscopic subscapularis tendon repair: technique and preliminary results. Arthroscopy 2002;18:454-63 [DOI] [PubMed] [Google Scholar]
- 38.Wolfe SW, Wickiewicz TL, Cavanaugh JT. Ruptures of the pectoralis major muscle. An anatomic and clinical analysis Am J Sports Med 1992;20:587-93 [DOI] [PubMed] [Google Scholar]
- 39.Petilon J, Carr DR, Sekiya JK, Unger DV. Pectoralis major muscle injuries: evaluation and management. J Am Acad Orthop Surg 2005;13:59-68 [DOI] [PubMed] [Google Scholar]
- 40.Dodds SD, Wolfe SW. Injuries to the pectoralis major. Sports Med 2002;32:945-52 [DOI] [PubMed] [Google Scholar]
- 41.Ghalayini SR, Board TN, Srinivasan MS. Anatomic variations in the long head of biceps: contribution to shoulder dysfunction. Arthroscopy 2007;23:1012-8 [DOI] [PubMed] [Google Scholar]
- 42.Pal GP, Bhatt RH, Patel VS. Relationship between the tendon of the long head of biceps brachii and the glenoidal labrum in humans. Anat Rec 1991;229:278-80 [DOI] [PubMed] [Google Scholar]
- 43.Vangsness CT, Jr., Jorgenson SS, Watson T, Johnson DL. The origin of the long head of the biceps from the scapula and glenoid labrum. An anatomical study of 100 shoulders J Bone Joint Surg Br 1994;76:951-4 [PubMed] [Google Scholar]
- 44.Wafae N, Atencio Santamaria LE, Vitor L, et al. Morphometry of the human bicipital groove (sulcus intertubercularis). J Shoulder Elbow Surg 2010;19:65-8 [DOI] [PubMed] [Google Scholar]
- 45.Bhatia DN, van Rooyen KS, de Beer JF. Direct arthroscopy of the bicipital groove: a new approach to evaluation and treatment of bicipital groove and biceps tendon pathology. Arthroscopy 2008;24:368 e1-6 [DOI] [PubMed] [Google Scholar]
- 46.Bryan WJ, Schauder K, Tullos HS. The axillary nerve and its relationship to common sports medicine shoulder procedures. Am J Sports Med 1986;14:113-6 [DOI] [PubMed] [Google Scholar]
- 47.Eakin CL, Dvirnak P, Miller CM, Hawkins RJ. The relationship of the axillary nerve to arthroscopically placed capsulolabral sutures. An anatomic study Am J Sports Med. 1998;26:505-9 [DOI] [PubMed] [Google Scholar]
- 48.Boardman ND, 3rd, Cofield RH. Neurologic complications of shoulder surgery. Clin Orthop Relat Res 1999:44-53 [PubMed] [Google Scholar]
- 49.Miller SL, Gladstone JN, Cleeman E, et al. Anatomy of the posterior rotator interval: implications for cuff mobilization. Clin Orthop Relat Res 2003:152-6 [DOI] [PubMed] [Google Scholar]
- 50.Tubbs RS WC, Louis RG, Jr, Shoja MM, et al. Use of the scapular spine in lumbar fusion procedures: cadaveric feasibility study. Laboratory investigation J Neurosurg Spine 2007:554-7 [DOI] [PubMed] [Google Scholar]
- 51.Plancher KD, Peterson RK, Johnston JC, Luke TA. The spinoglenoid ligament. Anatomy, morphology, and histological findings J Bone Joint Surg Am 2005;87:361-5 [DOI] [PubMed] [Google Scholar]


